Abstract
Purpose
To evaluate the role of virtual monoenergetic imaging (VMI) in the detection of peritoneal metastatic disease in contrast-enhanced computed tomography (CT) of the abdomen and pelvis and to compare this technique to the conventional 120 kV mixed dataset.
Materials and methods
Institutional review board approval was obtained with no informed consent required for this retrospective analysis. 43 consecutive patients with histopathologically confirmed peritoneal disease were scanned using a standard protocol on a 128-section dual-source, dual-energy CT system (100/140 keV). Scans were retrospectively reconstructed at VMI energy levels from 40–110 keV in 10 keV increments and were analyzed both quantitatively and qualitatively. CNR values for peritoneal metastatic deposits were recorded using region of interest (ROI) analysis at each energy level for all VMI datasets. Subjective analysis was performed by two independent fellowship-trained readers with combined experience of greater than 15 years. Qualitative parameters included diagnostic acceptability, subjective noise, and contrast resolution and confidence.
Results
The contrast-to-noise ratios (CNRs) for peritoneal metastatic deposits at the different VMI energy levels were compared using a one-way ANOVA with Tukey Post Test, and the optimal CNR was observed at 40 keV (p < 0.0001). Qualitative parameters were compared using a Paired T Test. Subjective noise, diagnostic acceptability, and contrast resolution was significantly better on the conventional images, but readers reported increased confidence on VMI at 40 keV (p < 0.001).
Conclusion
VMI reconstruction of contrast-enhanced dual-energy CT scans of the abdomen and pelvis at 40 keV maximizes the conspicuity of metastatic peritoneal deposits and improves radiologists’ diagnostic confidence compared with conventional CT images. We recommend using virtual monoenergetic datasets at 40 keV as a tool for improving the detection of these lesions in routine clinical practice.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Peritoneal carcinomatosis is often a subtle finding in patients with advanced abdominopelvic malignancy. Cancers which have a propensity to spread to the peritoneum include colorectal, ovarian, gastric, pancreatic, and adrenocortical carcinomas [1]. Patients diagnosed with peritoneal spread of disease have a very poor life expectancy. However, with early recognition, advanced chemotherapy regimens and surgery, such as hyperthermic intraperitoneal therapy (HIPEC), can be initiated to improve patient survival [2,3,4,5,6]. It is extremely important for radiologists to identify peritoneal disease, when possible, to ensure that the disease is managed appropriately.
The comparative effectiveness of the various imaging modalities for detecting peritoneal disease is debated. Magnetic resonance imaging (MRI), specifically diffusion-weighted imaging (DWI), has been shown to be more sensitive for detecting early peritoneal disease in ovarian cancer [7]. However, a recent study demonstrated that CT was equivalent to MRI for most sites of peritoneal metastases from ovarian cancer including the omentum, liver surface, bowel mesentery, and cul de sac [8]. The study reported that DWI remained superior for the detection of right-sided diaphragmatic deposits [8]. In another recent study, MRI and CT were found to be equivalent for the detection of peritoneal disease in presurgical pancreatic cancer [9]. Although MRI and positron-emission tomography (PET) have roles in the work up of abdominopelvic malignancy, computed tomography remains the imaging modality of choice due to its widespread availability, excellent spatial resolution and rapid acquisition time [10].
VMI uses a complex post-processing algorithm (both interpolation and extrapolation) on dual-energy data sets to produce computed images at a single chosen “monoenergetic” energy level [11, 12]. Reconstructions at low keV levels have been shown to maximize contrast from intravenous contrast agents as they more closely approximate the k edge of iodine 33 keV [13, 14]. VMI at low keV has been shown to provide more reliable attenuation values and to detect more subtle contrast enhancement than conventional single energy polychromatic imaging (PCI) in abdominal and chest CT angiography [13, 14]. VMI has shown initial promise in evaluating abdominal, thoracic, vertebral, and head and neck malignancies [15,16,17,18,19]. In the liver, virtual monoenergetic imaging has been shown to not only improve the conspicuity of lesions but also to facilitate the differentiation between benign and malignant neoplasms [16, 17].
VMI has yet to be evaluated in malignant peritoneal disease. The goal of this study was to quantitatively assess contrast-to-noise (CNR) of abdominopelvic peritoneal deposits across the spectrum of virtual monoenergetic levels to identify the optimal keV for detecting these deposits. In addition, we wanted to qualitatively assess reader whether there was increased reader confidence in detecting peritoneal disease on the virtual monoenergetic images compared to conventional mixed CT images.
Materials and methods
Study population
Institutional ethical review board approved this retrospective study. 72 consecutive patients with peritoneal metastases were scanned between February and October 2014 using a standardized protocol on a single dual-source dual-energy CT system (Somatom Definition Flash, Siemens Healthcare, Forchheim Germany) situated in the Emergency Department of an academic teaching hospital. Patients who did not receive iodinated intravenous contrast, who received enteric contrast, or who did not have pathology-proven peritoneal disease within 2 months of the CT scan were excluded. This led to a total of 43 patients for inclusion in this study.
Reference standard
For each patient, we retrospectively reviewed the operative and pathology reports within a 2-month window of the CT scan. The histopathologic diagnosis of peritoneal metastases served as the reference standard for the diagnosis of metastatic peritoneal disease.
CT acquisition
All CT images were acquired using a second-generation dual-source 128-slice multirow detector CT system (Somatom Definition Flash, Siemens Healthcare, Forchheim Germany). After obtaining anteroposterior and mediolateral scout views, 90 cc of intravenous contrast was administered (Omnipaque 350 mg I/mL; GE Healthcare, USA) at a rate of 2.5 cc per second followed by 30 cc of 0.9% NaCl at the same rate. At our institution, all routine CT scans of the abdomen and pelvis are performed with 90 cc of IV contrast. The datasets were acquired in the portal venous phase (70 s postinjection) using a dual-source, dual-energy, low-pitch (pitch = 0.6) helical acquisition with tube voltages of 100 kV and 140 kV with Tin filter (mAs 115 and 89, respectively) with a rotation time of 0.5 s.
CT image reconstruction
Images were acquired using a 32 × 0.6-mm collimation and were subsequently reconstructed to a 3-mm slice thickness, 2-mm slice increment using a field of view appropriate to the patient’s size. Axial source data was reconstructed with sinogram affirmed iterative reconstruction algorithm (SAFIRE, Siemens Healthcare, Forchheim, Germany) at a strength of 2. Images were reconstructed using the I30 “soft tissue” deconvolution kernel. Scans were transferred through the institutional picture archiving computer system (PACS) to the Multi-Modality Workstation (Syngo mmWP VE36A, Siemens Healthcare, Forchheim, Germany). Using the dual-energy advanced monoenergetic reconstruction application (Mono+), scans were reconstructed at VMI energy levels from 40 to 110 in 10 keV increments.
Effective dose measurements
Dose length product (DLP) was recorded from the dose report for each patient. The effective dose was estimated by multiplying the DLP by 0.015 mSv/mGy.cm [20, 21].
Quantitative image analysis
For each patient, a circular regions of interest (ROI) (area, 0.5 cm2) was placed within the peritoneal deposits. In some patients with numerous lesions, more than one ROI was placed. ROIs were placed in areas of conglomerate/gross metastatic disease with a maximum of five ROIs over patient. An additional ROI (area, 0.5 cm2) was placed within the gluteal muscle groups with efforts made to place the ROI in as homogenous an area as possible, away from tissue planes, calcification, and intramuscular fat. Mean attenuation in Hounsfield units (HU) and standard deviation of the mean attenuation in the ROI were recorded for all. The standard deviation of the mean attenuation in the ROI served as an objective measure of noise [11]. The contrast-to-noise ratios (CNR) were calculated for each dataset at each keV. CNR was defined as the HU difference between the peritoneal deposit and the average muscle divided by the mean noise of the muscle. In total, 72 peritoneal lesions were included for analysis.
Qualitative image analysis
Based on these results, datasets were reconstructed using the dual-energy monoenergetic application (Siemens Healthcare, Forchheim, Germany) at 40 keV (VMI-40). All VMI-40 images were independently assessed for image quality by two radiologists with 15 years of experience on the institutional PACS. The scoring system was adapted from the European Guidelines on Quality Criteria for CT [22]. Subjective parameters included diagnostic acceptability, subjective noise, contrast resolution, and confidence. Image acceptability was scored out of 3 where 1 = standard and diagnostic, 2 = acceptable and diagnostic only after windowing, and 3 = perceptible change that affects interpretation. Subjective noise was graded out of 3 where 1 = standard and diagnostic, 2 = noisy but diagnostic, and 3 = noisy and nondiagnostic. Spatial resolution was also scored out of 3 where 1 = standard and diagnostic, 2 = acceptable and diagnostic only after windowing, and 3 = perceptible change that affects interpretation. Contrast resolution was graded out of 3 where 1 = excellent, 2 = acceptable, and 3 = poor. Radiologists were permitted to adjust the window level and width of the images based on their own search pattern and preference. Although the original European Guidelines on Quality Criteria for CT do not take into account windowing, it has been shown that windowing significantly improves the perception of virtual monoenergetic images by improving the actual display CNR, as a result of the different HU values [23]. Finally, diagnostic confidence was graded out of 3 where 3 = confident, 2 = somewhat confident, and 1 = not confident.
Statistical analysis
Statistical tests were performed with a commercial medical statistical package [24]. The CNRs for peritoneal metastatic deposits at the different VMI energy levels (40–110 keV) were compared using a one-way ANOVA with Tukey Post Test. A Paired T Test was used to compare the qualitative parameters used to assess image quality. A difference with a p value of < 0.05 was considered statistically significant. All data are presented as mean ± standard deviation.
Results
Study patients
We included 43 consecutive patients including 11 males and 32 females, with an age range between 18 and 93 years (mean age, 59.8 years; median age, 69 years). Of the 43 patients included, nine primary malignancies were represented: 16 (37.2%) had ovarian cancer; 15 (34.9%) had colon cancer; 4 (9.3%) had uterine cancer; 2 (4.7%) had gastric cancer or had breast cancer; and 1 (2.3%) had pancreas, appendix, gallbladder, or lung cancer (Fig. 1). From these 43 patients, 72 peritoneal lesions were included for analysis.
Effective dose measurements
The average DLP was 285.9 mGy.cm (± 89.1 mGy.cm), and the effective dose was 4.3 mSv (± 1.3 mSv).
Reference standard
29 patients underwent surgery, and 14 patients underwent biopsy for confirmation of their peritoneal metastatic disease.
Quantitative image analysis
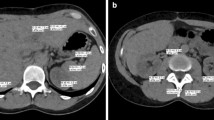
The mean peritoneal deposit attenuation and noise was significantly higher at 40 keV compared to the other sampled virtual monoenergetic levels (p < 0.0001) (Fig. 2A, B). Using the peritoneal deposit and gluteal muscle attenuation values obtained with 10 keV increments from 110 to 40 keV, the contrast-to-noise ratios were calculated (Fig. 2C). The contrast-to-noise ratio for the peritoneal deposits was the highest at 40 keV (p < 0.0001). Figure 3 shows an example of the VMI reconstructions performed.
Quantitative quality indexes across the range of virtual monoenergetic energy levels (40–110 keV) reconstructed from contrast-enhanced dual-energy abdomen CT data. For peritoneal metastases ROIs, maximal attenuation, and noise occurred at 40 keV (A, B), optimal CNR occurred at 40 keV (C). Error bars = standard deviation of the mean
Qualitative image analysis
On qualitative image assessment, the conventional CT images demonstrated significantly higher diagnostic acceptability, subjective noise, and contrast resolution (Table 1). However, readers reported improved confidence when detecting peritoneal deposits on the VMI-40 images compared to the conventional CT images. Example cases are shown in Figs. 4 and 5.
Discussion
Although peritoneal carcinomatosis can be a subtle finding on CT, its presence or absence has a dramatic role on patient management and prognosis. Accurate identification and characterization of peritoneal metastatic deposits is also essential as some lesions are more amenable to surgical resection than others [1]. As more sophisticated treatment options for metastatic peritoneal disease emerge, it will even more important to be able to confidently identify lesions, even when subtle.
Despite the overall superior sensitivity of DWI MRI sequences, MRI is expensive and not always practical in these patients. Our study demonstrates that virtual monoenergetic levels of 40 keV provide optimal CNR for detecting peritoneal deposits—a technique which may serve as an adjunct to currently available modalities. The value of 40 keV, where maximum attenuation and CNR of the peritoneal depositions was observed, is the same maximum attenuation value that has been identified for head and neck malignancy [15]. It is likely that this value, which is close to the k-edge of iodine (33 keV) is due to the increased vascularity of these lesions compared to the surrounding soft tissues. Other studies have also demonstrated that malignant tissue is more likely to concentrate iodine on DECT images and is therefore more vascular than other etiologies. Hou et al. demonstrated that high iodine concentration within lung masses on DECT scans performed in the venous phase were suggestive of malignant rather than inflammatory tissue [18].
Despite the advantages of the VMI-40 images, these images should be used with caution for routine interpretation due to the high subjective noise and poor contrast resolution, as reflected by the lower diagnostic acceptability score for the VMI-40 images. Although the VMI-40 images were less diagnostically acceptable than the conventional CT images, they were still within the diagnostically acceptable range (with windowing). It is important that radiologists using these VMI-40 images to adjust their window level and width to provide high lesion to background contrast to increase the conspicuity of lesions. Fu et al. demonstrated that virtual monoenergetic images require windowing beyond the usual window level and width used for the interpretation of the conventional CT images due to the significant increase in CNR [23]. Since the VMI-40 images are accompanied by a significant increase in image noise, we do not recommend that sole interpretation of a study be performed on a VMI-40 reconstructed dataset. Instead, we posit its application to be similar to the use of DWI sequences in abdominal MRI, where lesion detection is significantly improved, however, anatomy and image details are lost. With appropriate windowing, we found that the VMI-40 images improved radiologists’ diagnostic confidence for peritoneal deposits compared to the conventional CT images.
There is growing evidence of support the use of VMI in the detection and characterization of abdominopelvic malignancy [25]. Although our study is the first to report on the advantages of DECT for detecting peritoneal metastatic disease, our findings are in keeping with what has been reported in the literature for primary tumors and hepatic metastases. Similar to our results, these studies demonstrate that lower keV virtual monoenergetic images improve lesion detection by increasing the CNRs [25]. Spectral imaging with 50 keV monoenergetic images has been shown to aid in the detection of primary pancreatic neoplasms and hepatic metastases [25, 26]. In addition, hypervascular liver lesions had the greatest CNR and conspicuity on arterial phase 50 keV monoenergetic images [16]. Iodine maps have also been shown to be helpful in qualitatively improving detection and characterization of malignant tissue, and although we did not investigate this technique, it may also prove to be useful in the diagnosis of peritoneal metastases [25].
This study has limitations in that it is a retrospective study, which included patients admitted through the emergency department in a large academic hospital and that outpatients receiving scans for staging were not included. In addition, the time to post-process each dual-energy scan (approximately 3 min) may be seen as a drawback to using this technique in very busy clinical practice. However, the added information provided from both the monoenergetic imaging modes without additional patient exposure to radiation or contrast material, is invaluable. Also, due to recent advances, integrating DECT image analysis into clinical workflow has become much less cumbersome. For example, production of excellent multiplanar reconstructions can be produced automatically enabling these reconstructions to happen in the background with no intervention from the radiologist/technologist thus reducing the time and effort required to interpret dual-energy images [27]. In addition, a single second-generation dual-source DECT platform was used in this study and other dual-energy platforms, such as rapid kVp switching, were not examined.
We conclude that virtual monoenergetic reconstruction of contrast-enhanced dual-energy CT scans of the abdomen and pelvis at 40 keV allows for the optimal CNR and conspicuity of metastatic peritoneal deposits. At 40 keV, radiologists reported increased confidence in detecting peritoneal deposits, compared with conventional single energy CT. We recommend using virtual monoenergetic datasets at 40 keV as a tool for improving the detection of peritoneal metastases in routine clinical practice. Improved detection of these lesions will enable surgeons and oncologists to make more informed decisions regarding operative intervention and chemotherapeutic regimens.
References
Levy AD, Shaw JC, Sobin LH (2009) Secondary tumors and tumorlike lesions of the peritoneal cavity: imaging features with pathologic correlation. Radiographics 29(2):347–373
O’Dwyer S, Verwaal VJ, Sugarbaker PH (2015) Evolution of treatments for peritoneal metastases from colorectal cancer. J Clin Oncol 33(18):2122–2123
Klaver CEL, et al. (2015) Adjuvant hyperthermic intraperitoneal chemotherapy (HIPEC) in patients with colon cancer at high risk of peritoneal carcinomatosis; the COLOPEC randomized multicentre trial. BMC Cancer 15:428
Naffouje SA, Salti GI (2018) Cytoreductive surgery and hyperthermic intraperitoneal chemotherapy in elderly patients: complete cytoreduction is feasible and crucial for improved survival despite high carcinomatosis index. Anticancer Res 38(1):441–448
Huang Y, Alzahrani NA, Liauw W, et al. (2017) Early postoperative intraperitoneal chemotherapy is associated with survival benefit for appendiceal adenocarcinoma with peritoneal dissemination. Eur J Surg Oncol 43(12):2292–2298
Magge D, et al. (2017) Hyperthermic intraperitoneal chemoperfusion as a component of multimodality therapy for ovarian and primary peritoneal cancer. J Surg Oncol 116(3):320–328
Grabowska-Derlatka L, Derlatka P, Szeszkowski W, Cieszanowski A (2016) Diffusion-weighted imaging of small peritoneal implants in ‘potentially’ early-stage ovarian cancer. Biomed Res Int 2016:9254742
Fehniger J, et al. (2016) A prospective study evaluating diffusion weighted magnetic resonance imaging (DW-MRI) in the detection of peritoneal carcinomatosis in suspected gynecologic malignancies. Gynecol Oncol 142(1):169–175
Chen F-M, Ni J-M, Zhang Z-Y, et al. (2016) Presurgical evaluation of pancreatic cancer: a comprehensive imaging comparison of CT versus MRI. AJR Am J Roentgenol 206(3):526–535
Schmidt S, Meuli RA, Achtari C, Prior JO (2015) Peritoneal carcinomatosis in primary ovarian cancer staging: comparison between MDCT, MRI, and 18F-FDG PET/CT. Clin Nucl Med 40(5):371–377
Marin D, et al. (2010) Low-tube-voltage, high-tube-current multidetector abdominal CT: improved image quality and decreased radiation dose with adaptive statistical iterative reconstruction algorithm–initial clinical experience. Radiology 254(1):145–153
Silva AC, Morse BG, Hara AK, et al. (2011) Dual-energy (spectral) CT: applications in abdominal imaging. Radiographics 31(4):1031–1050
Yu L, Christner JA, Leng S, et al. (2011) Virtual monochromatic imaging in dual-source dual-energy CT: radiation dose and image quality. Med Phys 38(12):6371–6379
Yu L, Leng S, McCollough CH (2012) Dual-energy CT-based monochromatic imaging. AJR Am J Roentgenol 199(5 Suppl):S9–S15
Srinivasan A, Parker RA, Manjunathan A, et al. (2013) Differentiation of benign and malignant neck pathologies: preliminary experience using spectral computed tomography. J Comput Assist Tomogr 37(5):666–672
Shuman WP, et al. (2014) Dual-energy liver CT: effect of monochromatic imaging on lesion detection, conspicuity, and contrast-to-noise ratio of hypervascular lesions on late arterial phase. AJR Am J Roentgenol 203(3):601–606
Wang Q, Shi G, Qi X, Fan X, Wang L (2014) Quantitative analysis of the dual-energy CT virtual spectral curve for focal liver lesions characterization. Eur J Radiol 83(10):1759–1764
Hou WS, Wu HW, Yin Y, et al. (2015) Differentiation of lung cancers from inflammatory masses with dual-energy spectral CT imaging. Acad Radiol 22(3):337–344
Yuan Y, Zhang Y, Lang N, Li J, Yuan H (2015) Differentiating malignant vertebral tumours from non-malignancies with CT spectral imaging: a preliminary study. Eur Radiol 25(10):2945–2950
Huda W, Ogden KM, Khorasani MR (2008) Converting dose-length product to effective dose at CT. Radiology 248(3):995–1003
Christner JA, Kofler JM, McCollough CH (2010) Estimating effective dose for CT using dose-length product compared with using organ doses: consequences of adopting international commission on radiological protection publication 103 or dual-energy scanning. Am J Roentgenol 194(4):881–889
Bongartz G et al. (1999) European guidelines on quality criteria for computed tomography. Eur Comm.
Fu W, et al. (2017) Optimizing window settings for improved presentation of virtual monoenergetic images in dual-energy computed tomography. Med Phys 44(11):5686–5696
GraphPad Prism. https://www.graphpad.com/scientific-software/prism/. Accessed 29 July 2018.
Morgan DE (2018) The role of dual-energy computed tomography in assessment of abdominal oncology and beyond. Radiol Clin North Am 56(4):565–585
McNamara MM, Little MD, Alexander LF, et al. (2015) Multireader evaluation of lesion conspicuity in small pancreatic adenocarcinomas: complimentary value of iodine material density and low keV simulated monoenergetic images using multiphasic rapid kVp-switching dual energy CT. Abdom Imaging 40(5):1230–1240
Sodickson A, Primak A, Keraliya A. Workflow evaluation of a new fully automated dual-energy CT post-processing configuration. In: Radiological Society of North America (RSNA) Scientific Assembly and Annual Meeting
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This study was funded by a 2015 Research Grant from the Canadian Radiological Foundation (CRF).
Conflict of interest
Savvas Nicolaou: Institutional research agreement, Siemens AG. All the other authors have declared that they have no competing interests.
Human ethics
Institutional review board approval (University of British Columbia) was obtained for this study.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent from individual participants was not required for this retrospective study as per Institutional Review Board approvals.
Rights and permissions
About this article
Cite this article
Darras, K.E., Clark, S.J., Kang, H. et al. Virtual monoenergetic reconstruction of contrast-enhanced CT scans of the abdomen and pelvis at 40 keV improves the detection of peritoneal metastatic deposits. Abdom Radiol 44, 422–428 (2019). https://doi.org/10.1007/s00261-018-1733-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00261-018-1733-7