Abstract
Over the past 16 years, several scientific organizations have proposed systems that incorporate imaging for surveillance, diagnosis, staging, treatment, and monitoring of treatment response of hepatocellular carcinoma (HCC). These systems are needed to standardize the acquisition, interpretation, and reporting of liver imaging examinations; help differentiate benign from malignant observations; improve consistency between radiologists; and provide guidance for management of HCC. This review article discusses the historical evolution of HCC imaging systems. We indicate the features differentiating these systems, including target population, screening and surveillance algorithm, diagnostic imaging modalities, diagnostic scope, expertise and technical requirements, terminology, major and ancillary imaging features, staging and transplant eligibility, and assessment of treatment response. We highlight the potential benefits of unifying the systems, which we anticipate will enable sharing, pooling, and meta-analysis of data; facilitate multi-center trials; and accelerate dissemination of knowledge.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Hepatocellular carcinoma (HCC) has high incidence and high mortality. It is the sixth most common malignancy worldwide and the second most common cause of mortality from cancer [1]. Prior to the widespread adoption of systematic screening and surveillance in patients at risk for HCC, the mortality attributed to HCC was similar to its incidence [2]. In 1990, the age-adjusted mortality rate of liver cancer was 3.6 per 100,000 people and the incidence was 3.9 per 100,000 people [3]. Unscreened patients present with symptomatic advanced disease for which there are no effective options; with a dismal prognosis, such patients usually die within one year of presentation. By comparison, diagnosis of HCC at an early stage, accompanied by potentially effective and sometimes even curative therapy, can markedly improve patient survival [4]. The 5-year survival markedly improved after the mid-1990s with the introduction of systematic screening and surveillance for HCC [3]. Formal surveillance was advocated in a seminal paper on clinical management of HCC written after the European Association for the Study of the Liver (EASL) Barcelona conference [5]. The committee of experts on HCC was composed of hepatologists, oncologists, hepatobiliary surgeons, and radiologists [5].
Improvements in HCC mortality have in part been attributed to the critical role that imaging now plays in the screening, surveillance, diagnosis, staging, management (treatment selection, eligibility, and priority for liver transplantation) [6, 7], and monitoring (assessment of treatment response) of HCC. In parallel to the growing role of liver imaging in patients at risk for developing HCC, several international scientific organizations and societies have proposed systems for the interpretation of imaging examinations performed for HCC surveillance and diagnosis, staging and treatment planning, and assessment of treatment response [8,9,10,11,12,13,14,15,16,17,18,19,20,21,22,23,24]. Reflecting the state of radiology knowledge and technical state of the art, these systems have been developed to standardize the acquisition, interpretation, and reporting of liver imaging examinations, improve consistency between radiologists, and provide guidance for HCC management.
Over the past 16 years, 14 scientific organizations and societies (three from Europe, six from Asia, four from North America, and one by a global organization) have published systems that include imaging-based criteria for diagnosis of HCC. Nine of these systems have been updated over time to reflect the evolution in imaging technique and advances in understanding of HCC imaging. Except for LI-RADS which has been designed primarily by radiologists, other systems have been developed by hepatologists, gastroenterologists, oncologists, and hepatobiliary transplant surgeons. However, radiologists who interpret liver imaging examinations should be familiar with the diagnostic systems used in their geographical area because surveillance recommendations, diagnostic criteria, and transplant eligibility criteria very between different geographical areas. By understanding the differences between HCC imaging systems, radiologists will appreciate the potential benefit of a unified HCC system.
The purpose of this study is to review the historical evolution of HCC imaging systems by explaining why they exist, how they differ, and what they contain. We also highlight the potential benefits of unifying the various systems.
Why do HCC imaging systems exist?
More than 50% of patients with HCC present with an intermediate or advanced tumor stage [25]. While therapeutic options are limited for those who present with advanced disease at presentation, several options including curative therapy exist for those presenting with very early or early stage disease [8, 9]. The 1-year survival rate of HCC was 25% in 1992 and has improved to 47% in 2004, an improvement attributed to diagnosis of HCC at an early stage [2]. Further, the combination of early detection of HCC and curative therapy has improved the 5-year survival from 40% to 70% [26, 27].
The ability to diagnose HCC early depends on screening for detection of existing cases, and enrollment into a surveillance program to detect new cases. HCC screening and surveillance includes blood tests (typically alpha-fetoprotein), imaging tests, or combination of both. The use of blood tests for screening and surveillance of HCC remains controversial [8, 9]. Although alpha-fetoprotein appears to be the single most useful biomarker for detection of HCC, current Western guidelines have excluded alpha-fetoprotein because of its limited accuracy [8, 13]. At a threshold of 20 ng/mL, the per-patient sensitivity of 59% is too low for screening purpose despite a specificity of 90% [28]. At a lower threshold of 10.3 ng/mL, the sensitivity is slightly improved to 70% but at the expense of lower specificity at 82% [28]. According to a comprehensive meta-analysis on imaging modalities for detection of HCC, ultrasound without contrast had a per-patient pooled sensitivity of 78% and pooled specificity of 89%, whereas CT had a pooled per-patient sensitivity of 84% and specificity of 99% [29]. Because of their higher sensitivities, imaging tests are preferred over blood tests for screening and surveillance in at-risk patients [8, 9, 13].
In turn, patients with positive screening test results must undergo more comprehensive imaging to confirm the diagnosis. Liver biopsy was previously the historical reference standard for diagnosis of HCC. However, unlike tissue sampling of superficial organs (e.g., breast or thyroid) or fine needle aspiration of deeper organs reachable by endoscopic approaches (e.g., pancreas), biopsy of focal liver lesions is associated with additional risks and complications. This includes a 2.5% risk of significant bleeding attributable to the hypervascular nature of HCCs [30] and a 0.06% risk of mortality [31], a 10%–30% risk of false-negative biopsies in patients with HCC [32,33,34], a 1.6% to 5.1% risk of tumor seeding along the biopsy tract [35,36,37,38], and the risk of upstaging disease in liver transplant candidates [39]. Because of these concerns, the majority of HCCs are now diagnosed by imaging alone, a trend that has progressed over the last two decades [40]. Nowadays, biopsy of focal liver lesions is reserved for equivocal cases, including those where malignancy other than HCC is part of the differential diagnosis, and research protocols that require histological proof of cancer.
In a diagnostic (i.e., non-surveillance) setting, contrast-enhanced ultrasound has a per-lesion sensitivity of 75% and specificity of 97%, CT a sensitivity of 76% and specificity of 89%, and MRI a sensitivity of 83% and specificity of 87% according to the meta-analysis cited above [29]. While these numbers represent pooled estimates of diagnostic performance from studies performed over a period covering almost two decades, more recent literature indicates that stringent imaging-based diagnostic criteria are able to achieve near-100% specificity for non-invasive diagnosis of HCC [41].
To achieve consistent imaging-based diagnosis of HCC, formal systems have been introduced to standardize the acquisition, interpretation, and reporting of liver imaging examinations (Table 1 ). As discussed in the next section, there are regional variations in the various imaging systems which might be attributed to geographic variation in the distribution of risk factors, patient population, and incidence of HCC. These diagnostic systems have become increasingly sophisticated over time, and many have been updated in parallel with advances in radiological knowledge, better understanding of HCC pathophysiology, and technological capabilities (Fig. 1). For example, the earliest systems emphasized only arterial phase hyperenhancement for the diagnosis of HCC [5], whereas subsequent updates and newer systems [8, 13, 42] have incorporated washout appearance and other imaging features observable with multiphasic acquisitions, higher spatial resolution, and new contrast agents. In addition, HCC imaging systems provide management guidance at different steps of the clinical care continuum—screening, surveillance, diagnosis, staging, treatment selection, treatment guidance, and treatment response monitoring. Further, these diagnostic systems have helped formalize a central role for radiologists in HCC management by assigning them the responsibility to detect suspected HCC on screening or surveillance examinations and to verify the diagnosis of HCC on call-back examinations. Lesions that meet diagnostic criteria for HCC qualify for tumor staging and are discussed in the setting of multidisciplinary tumor boards to identify the most appropriate treatment for individual patients.
How do HCC imaging systems differ?
Designs of the imaging systems vary in several ways. HCC imaging systems differ in their target population, clinical context (screening, surveillance, diagnosis, staging, assessment of treatment response), technical requirements and specifications, intended users, terminology, clinical, cultural and socioeconomic context, breadth, and level of complexity. Differences are summarized in Table 2 and discussed below.
Patient population
Although all current diagnostic systems apply to patients with cirrhosis or other risk factors for developing HCC, they differ in how patients are selected. For example, with the exception of cirrhosis due to a vascular disorder (e.g., Budd–Chiari, hereditary hemorrhagic telangiectasia, nodular regenerative hyperplasia or cardiac cirrhosis), cirrhosis due to congenital hepatic fibrosis, or in pediatric patients [43], the CT/MRI diagnostic system advocated by LI-RADS applies to all cirrhotic and other high-risk patients, regardless of whether they previously underwent ultrasound screening. By comparison, most other systems (European Association for the Study of the Liver-European Organization for Research and Treatment of Cancer [EASL-EORTC] [13], American Association for the Study of Liver Diseases [AASLD] [9], Japan Society of Hepatology [JSH] [18], and Asian Pacific Association for the Study of the Liver [APASL] [11]) apply only to patients with positive screening or surveillance tests subsequently called back for diagnostic imaging tests. One system, United Network for Organ Sharing and Organ Procurement and Transplantation Network (UNOS-OPTN), applies only to liver transplant candidates with HCC [23]. The differences in patient selection are pertinent because they affect the pre-test probability of disease and so the positive predictive value of a test. Hence, the diagnostic performance reported for one system’s imaging criteria may not apply to another system intended for a different patient population [44, 45].
Screening and surveillance algorithm
Several systems (EASL-EORTC, AASLD, National Comprehensive Cancer Network [NCCN], and LI-RADS) provide screening and surveillance algorithms. These describe the frequency of periodic ultrasound, sometimes in combination with serum tumor biomarkers [9, 13, 20, 21], as well as the recommended management based on test results. Some systems embed the surveillance algorithm within a larger diagnostic algorithm [8, 13, 18], whereas others have separate surveillance algorithms [20, 21].
For example, AASLD recommends ultrasound every 6 months in at-risk patients [8]; EASL-EORTC recommends ultrasound every 6 months in at-risk patients, ultrasound every 3–4 months when a nodule smaller than 1 cm has been detected and in the follow-up after resection or locoregional therapies, and CT or MRI for patients on waiting list for liver transplantation and when technical factors prevent adequate ultrasound assessment [13].
Diagnostic imaging modalities and techniques
All current systems recommend multiphase computed tomography (CT) or magnetic resonance imaging (MRI) as first-line diagnostic imaging modalities. Some systems recommend specific modalities for second-line imaging: CEUS [11, 18], SPIO-enhanced MRI [11], hepatobiliary phase MRI with gadoxetate [18,19,20], and CT during hepatic arteriography (CTHA) and CT during arterial portography (CTAP) [18]. LI-RADS does not differentiate between first-line and second-line modalities, providing diagnostic imaging algorithms for all major modalities and agents available in the United States for HCC imaging, as there is insufficient evidence, especially in the community setting, to preferentially recommend particular modalities or agents.
Diagnostic scope
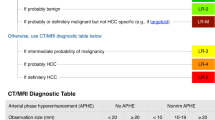
Diagnostic imaging systems vary in their diagnostic scope. LI-RADS primarily targets radiologists who encounter the whole spectrum of observations seen in the liver, including pseudolesions and lesions (non-tumoral lesions and masses). Other systems, which were designed as practice guidelines for clinicians, focus instead on the distinction between definitely HCC and not definitely HCC.
All Western systems currently address only HCCs with arterial phase hyperenhancement [8, 9, 13, 20, 21, 23] and do not permit the diagnosis of HCC for lesions without this feature, although LI-RADS does allow arterial phase iso- or hypoenhancing observations to qualify as probable HCC [20]. In contrast, Asian systems provide criteria for hypo, iso, or hyperenhancing HCCs [11, 18, 19]. The differences in diagnostic scope and design of criteria are motivated by different priorities in treatment practices between geographic areas (discussed below).
Contrast agents
All current systems recommend extracellular agents for multiphase contrast-enhanced CT or MRI. JSH, KLCSG, and LI-RADS provide guidance for hepatobiliary contrast agents [18,19,20], whereas APASL provides guidance for superparamagnetic iron oxides (SPIO) and Kupffer cell agents [11]. These variations reflect regional differences in the availability of contrast agents. These alternative contrast agents reveal different aspects of the underlying tumor biology: decrease uptake of the hepatobiliary contrast agents or decrease uptake of SPIO and Kupffer cell agents by reticulo-endothelial system during hepatocarcinogenesis.
Diagnostic and technical expertise
Systems vary in the level of diagnostic and technical requirements. LI-RADS is intended for both “community and academic radiologists” [20]. Other systems either do not mention their target audience or are designed specifically for specialists. AASLD is intended for “radiologists with extensive expertise in liver imaging” [8], OPTN for “approved transplant centers” [23], and EASL-EORTC for “centers of excellence with high-end radiological equipment” [13].
Terminology
Systems vary widely in their terminology, reflecting the inconsistent and imprecisely defined language encountered in the radiology literature.
LI-RADS introduced a standardized lexicon of precisely defined terms supported by diagrams and an imaging atlas [20]. Different from most other HCC diagnostic systems, LI-RADS codifies the confidence of benign versus malignant into 5 levels, ranging from definitely benign to definitely HCC. Uniquely, LI-RADS also provides other categories for suspected non-HCC malignancy and for designating an observation uninterpretable due to image omission or degradation. Other systems, by comparison, provide a binary approach in which lesions are either definitely HCC or not definitely HCC.
Major imaging features of HCC
Systems vary in their imaging requirements for the diagnosis of definite HCC. Although all systems recognize that the combination of arterial phase hyperenhancement and washout appearance constitutes a hallmark feature of definite HCC, they differ in their specific requirements. Unlike Western systems, for example, Asian systems do not mandate arterial phase hyperenhancement for the definite diagnosis of HCC [11, 18, 19], as discussed above.
Except for guidelines by the JSH and APASL, which permit the diagnosis of definite HCC regardless of size [11, 18], all guidelines impose a minimal observation diameter of 10 mm as a requirement for definite HCC diagnosis. In addition, EASL-EORTC, LI-RADS, and OPTN systems stratify the risk of HCC with an additional size threshold for observations equal or larger than 20 mm [13, 20, 23] or 50 mm [23].
Capsule appearance constitutes a major imaging feature of HCC in two systems (LI-RADS and OPTN) [20, 23].
Threshold growth also constitutes a major imaging feature of HCC in LI-RADS and OPTN [20, 23]. However, the definitions differ. LI-RADS defines threshold growth as a “diameter increase of a mass by a minimum of 5 mm and by at least 50% if time interval is 6 months or less or by at least 100% diameter increase if more than 6 months.” In addition, a new mass that measures at least 10 mm also represents threshold growth if previously not seen within 24 months. In contrast, OPTN recognizes threshold growth only as ≥50% increase in size in ≤6 months. This has implication for OPTN staging and conversion of LI-RADS to OPTN classes as discussed by Tang et al. in this special issue [46].
Ancillary imaging features of HCC
LI-RADS is the only system that integrates ancillary features that modulate the probability of HCC [20]. Some of these ancillary features favor malignancy in general, some favor HCC in particular, and others favor benign entities.
Staging and transplant eligibility
Systems vary in their approach to tumor staging, recommended treatment approaches for each stage, and transplant eligibility criteria. The radiologic T-staging system is advocated by OPTN and LI-RADS [20, 23], the Barcelona Clinic Liver Cancer (BCLC) staging system by EASL-EORTC and AASLD [8, 9, 13], and the Modified Union for International Cancer Control (mUICC) by KLCSG [19].
HCC tumor stages eligible for liver transplantation are further discussed by Tang et al. [46].
Treatment response
Systems vary in their approach to treatment response assessment. The new treatment response algorithm [20] advocated by LI-RADS v2017 is further discussed by Do et al. in this special issue. AASLD advocates RECIST and references mRECIST, EASL-EORTC advocates the use of mRECIST, and KLCSG advocates both RECIST and mRECIST [8, 9, 13, 19, 47, 48]. Hence, systems reference RECIST, mRECIST, or both. Such references imply tacit endorsement of RECIST and/or mRECIST, but the endorsement is not made explicit and therefore subject to interpretation. Moreover, since KLCSG references both RECIST and mRECIST, there is ambiguity regarding which particular system to use.
Advances in knowledge and technology
Newer systems tend to integrate advances in radiology knowledge from the scientific literature, including from other diagnostic systems, into their own diagnostic criteria. Further, regularly updated systems are more likely to reflect the current state of the art in imaging interpretation, and to integrate new imaging modalities, sequences, and contrast agents into their diagnostic algorithms. This is reflected in the technical requirements specified by LI-RADS and OPTN [20, 23].
From a historical perspective, different regions worldwide have adapted guidelines that best suit their local practices given geographic differences in patient population, etiology of liver disease, policies on organ transplantation, imaging resources, and technology. The guidelines have been updated and modified over time as new data and evidence accrue, and as the aforementioned factors change and evolve.
For example, in 2001, given the rising incidence of HCC as well as existing controversies regarding its diagnosis and management, the EASL organized a Monothematic Conference on Clinical Management of Hepatocellular Carcinoma in 2001. It was at this conference that the first non-invasive criteria for HCC diagnosis based on imaging were developed, and the concept of arterial phase hyperenhancement (APHE) introduced, in the EASL 2001 guidelines [5].
By 2005, imaging technology had evolved to include contrast-enhanced ultrasound, multidetector computed tomography (CT), and dynamic magnetic resonance imaging (MRI). Emerging evidence demonstrated that the dynamic vascular pattern of HCC could be assessed using these imaging modalities, in particular APHE followed by washout appearance. Recognizing these advances in technology and new evidence, the AASLD amended the EASL 2001 imaging criteria, and introduced the concept of APHE and washout appearance as a hallmark feature of HCC, in the AASLD 2005 guidelines [42].
As of 2010, the AASLD 2005 concept of APHE and washout appearance being a hallmark feature of HCC had been validated. New evidence, however, demonstrated that at contrast ultrasound, intrahepatic cholangiocarcinoma (ICC) in cirrhosis might show a similar enhancement pattern as HCC, i.e., APHE followed by washout appearance. The AASLD amended its guidelines accordingly, and the AASLD 2010 guidelines no longer recommended contrast ultrasound for the diagnosis of HCC [8].
UNOS-OPTN is the network in the United States that develops policies that determine eligibility and priority for organ transplantation. Because there are not enough livers for all patients that require liver transplant, in 2011 UNOS-OPTN developed stringent diagnostic criteria for liver transplant candidates with HCC. The criteria aimed at high specificity of HCC diagnosis so as to prevent high-risk liver transplantation procedures in patients with false-positive diagnoses of HCC [49].
Recognizing the need for an imaging system that addresses the entire spectrum of liver findings in patients at risk for HCC, and the need for standardized terminology with a lexicon and an illustrative atlas, the LI-RADS system was developed in 2011 and has undergone regular updates (2013, 2014, and 2017) that take into account new evidence and technological advances. For example, unlike the initial LI-RADS 2011 version, the current LI-RADS 2017 version incorporates imaging criteria for hepatobiliary agents and contrast-enhanced ultrasound [20].
Treatment practices
The design of imaging systems is influenced by treatment practices which vary between geographic areas. In North America, the diagnostic criteria are intentionally designed to achieve high specificity (rather than high sensitivity) for the diagnosis of definite HCC [20, 23, 50]. Since patients with definite HCC may undergo liver transplantation for curative therapy based on imaging alone, stringent diagnostic criteria are used to avoid false-positive HCC diagnoses [51].
In Asia, diagnostic criteria favor high sensitivity for detection of early HCC [11, 18, 19]. This is justified by the larger use of locoregional ablative therapies such as percutaneous ethanol injection, radiofrequency ablation, and transarterial chemoembolization [52].
What do HCC imaging systems contain?
As summarized in Table 3, these systems may have several components: description of the patient population, inclusion of surveillance algorithm, diagnostic criteria, diagnostic algorithm, diagnostic table, ancillary features, tumor staging (either in the form of table or diagrams), assessment of treatment response, management guidelines, reporting guidelines, standardized lexicon, imaging atlas, and technical requirements.
LI-RADS v2017 integrates many components found in other systems as well as unique components (e.g., levels of confidence that correspond to management options, ancillary features, reporting guidelines, standardized lexicon, and imaging atlas).
Potential benefits of unification and standardization of HCC imaging systems
There are several potential benefits of unification and standardization of HCC imaging systems. Adoption of standard terminology would facilitate communication between radiologists and with other stakeholders: pathologists, hepatologists, and hepatobiliary surgeons. This would also facilitate dissemination of knowledge and adoption of research findings from other institutions adopting the same terminology. A standard terminology has the potential to reduce variability between radiologists, as inter-reader agreement has already been shown to be moderate to excellent for major imaging features [53,54,55,56].
System unification also will facilitate development of common data registries; data sharing, pooling, and meta-analysis; multi-center observational studies and clinical trials; trials; and scientific knowledge dissemination.
Based on this historical perspective, we anticipate that the future will see the development of a single unified system for international use. Developing such a system will require international feedback and leverage the pool of international talent, expertise, and perspective on HCC imaging and patient care. For reasons discussed above, we anticipate that standardized terminology should be adopted first, both in research and clinical care. Standardization of technical requirements, diagnostic criteria and algorithm, treatment response assessment criteria and algorithm, and management guidelines would then follow. The unification and standardization of HCC imaging systems will require identification of potential barriers to adoption of the unified system in different geographic areas. Ultimately, such a unified system will share core components with appropriate adjustments to optimize local healthcare systems, clinical practices, and resources.
Conclusion
Over the past 16 years, several scientific organizations have proposed systems that incorporate imaging for surveillance, diagnosis, staging, treatment, and monitoring of treatment response of HCC. These systems have been developed to standardize the acquisition, interpretation, and reporting of liver imaging examinations; help differentiate benign from malignant observations; improve consistency between radiologists; and provide guidance for management of HCC. The designs of these systems vary between geographic areas to address different target populations, resources, and treatment practices. These systems contain many components and have evolved to incorporate advances in radiological knowledge and technological capabilities.
Abbreviations
- AASLD:
-
American Association for the Study of Liver Diseases
- AOS:
-
Asian Oncology Summit
- APASL:
-
Asian Pacific Association for the Study of the Liver
- BASL:
-
Belgian Association for the Study of the Liver
- BCLC:
-
Barcelona Clinic Liver Cancer staging system
- CEUS:
-
Contrast-enhanced ultrasound
- CT:
-
Computed tomography
- CTHA:
-
CT during hepatic arteriography
- EASL:
-
European Association for the Study of the Liver
- EORTC:
-
European Organization for Research and Treatment of Cancer
- ESMO:
-
European Society for Medical Oncology
- HCC:
-
Hepatocellular carcinoma
- J-HCC:
-
Japanese HCC guidelines
- JSH:
-
Japan Society of Hepatology
- LI-RADS:
-
Liver Imaging Reporting and Data System
- MRI:
-
Magnetic resonance imaging
- NCCN:
-
National Comprehensive Cancer Network
- mUICC:
-
Modified Union for International Cancer Control
- SGA:
-
Saudi Gastroenterology Association
- SPIO:
-
Superparamagnetic iron oxide
- UNOS-OPTN:
-
United Network for Organ Sharing and Organ Procurement and Transplantation Network
- WGO:
-
World Gastroenterology Organisation
References
Ferenci P, Fried M, Labrecque D, et al. (2010) Hepatocellular carcinoma (HCC): a global perspective. J Clin Gastroenterol 44:239–245
Altekruse SF, McGlynn KA, Reichman ME (2009) Hepatocellular carcinoma incidence, mortality, and survival trends in the United States from 1975 to 2005. J Clin Oncol 27:1485–1491
Lingvay I, Raskin P, Szczepaniak LS (2007) Effect of insulin-metformin combination on hepatic steatosis in patients with type 2 diabetes. J Diabetes Complicat 21:137–142
Llovet JM, Di Bisceglie AM, Bruix J, et al. (2008) Design and endpoints of clinical trials in hepatocellular carcinoma. J Natl Cancer Inst 100:698–711
Bruix J, Sherman M, Llovet JM, et al. (2001) Clinical management of hepatocellular carcinoma. Conclusions of the Barcelona-2000 EASL conference. European Association for the Study of the Liver. J Hepatol 35:421–430
Cruite I, Tang A, Sirlin CB (2013) Imaging-based diagnostic systems for hepatocellular carcinoma. AJR Am J Roentgenol 201:41–55
Tang A, Cruite I, Sirlin CB (2013) Toward a standardized system for hepatocellular carcinoma diagnosis using computed tomography and MRI. Expert Rev Gastroenterol Hepatol 7:269–279
Bruix J, Sherman M (2011) Management of hepatocellular carcinoma: an update. Hepatology 53:1020–1022
Heimbach J, Kulik LM, Finn R, et al. (2017) Aasld guidelines for the treatment of hepatocellular carcinoma. Hepatology. doi:10.1002/hep.29086
Poon D, Anderson BO, Chen LT, et al. (2009) Management of hepatocellular carcinoma in Asia: consensus statement from the Asian Oncology Summit 2009. Lancet Oncol 10:1111–1118
Omata M, Lesmana LA, Tateishi R, et al. (2010) Asian Pacific Association for the Study of the Liver consensus recommendations on hepatocellular carcinoma. Hepatol Int 4:439–474
Van Vlierberghe H, Borbath I, Delwaide J, et al. (2004) BASL guidelines for the surveillance, diagnosis and treatment of hepatocellular carcinoma. Acta Gastroenterol Belg 67:14–25
European Association for the Study of the Liver, European Organisation for Research and Treatment of Cancer (2012) EASL-EORTC clinical practice guidelines: management of hepatocellular carcinoma. J Hepatol 56:908–943
Jelic S (2009) Hepatocellular carcinoma: ESMO clinical recommendations for diagnosis, treatment and follow-up. Ann Oncol 20(Suppl 4):41–45
Parikh P, Malhotra H, Jelic S (2008) Hepatocellular carcinoma: ESMO clinical recommendations for diagnosis, treatment and follow-up. Ann Oncol 19(Suppl 2):ii27–ii28
Makuuchi M, Kokudo N (2006) Clinical practice guidelines for hepatocellular carcinoma: the first evidence based guidelines from Japan. World J Gastroenterol 12:828–829
Makuuchi M, Kokudo N, Arii S, et al. (2008) Development of evidence-based clinical guidelines for the diagnosis and treatment of hepatocellular carcinoma in Japan. Hepatol Res 38:37–51
Kudo M, Matsui O, Izumi N, et al. (2014) JSH consensus-based clinical practice guidelines for the management of hepatocellular carcinoma: 2014 update by the Liver Cancer Study Group of Japan. Liver Cancer 3:458–468
Korean Liver Cancer Study Group, National Cancer Center (2015) 2014 Korean Liver Cancer Study Group-National Cancer Center Korea practice guideline for the management of hepatocellular carcinoma. Korean J Radiol 16:465–522
American College of Radiology (ACR) (2017) Liver imaging reporting and data system version 2017. Retrieved from http://www.acr.org/quality-safety/resources/LIRADS. Accessed 14 Aug 2017
Benson AB 3rd, D’Angelica MI, Abrams TA, et al. (2016) NCCN clinical practice guidelines in oncology: hepatobiliary cancers. J Natl Compr Cancer Netw 2:2016
Abdo AA, Al Abdul Karim H, Al Fuhaid T, et al. (2007) Saudi gastroenterology association guidelines for the diagnosis and management of hepatocellular carcinoma: summary of recommendations. Saudi J Gastroenterol 13:45–48
Organ Procurement and Transplantation Network (OPTN) (2017) OPTN/UNOS policy 9: allocation of livers and liver-intestines. http://optn.transplant.hrsa.gov/ContentDocuments/OPTN_Policies.pdf-nameddest=Policy_09. Accessed 4 March 2017
Ferenci P, Fried M, Labrecque D, et al. (2010) World Gastroenterology Organisation Guideline. Hepatocellular carcinoma (HCC): a global perspective. J Gastrointest Liver Dis 19:311–317
Pinter M, Hucke F, Graziadei I, et al. (2012) Advanced-stage hepatocellular carcinoma: transarterial chemoembolization versus sorafenib. Radiology 263:590–599
Lopez PM, Villanueva A, Llovet JM (2006) Systematic review: evidence-based management of hepatocellular carcinoma—an updated analysis of randomized controlled trials. Aliment Pharmacol Ther 23:1535–1547
Sutherland LM, Williams JA, Padbury RT, et al. (2006) Radiofrequency ablation of liver tumors: a systematic review. Arch Surg 141:181–190
Marrero JA, Feng Z, Wang Y, et al. (2009) Alpha-fetoprotein, des-gamma carboxyprothrombin, and lectin-bound alpha-fetoprotein in early hepatocellular carcinoma. Gastroenterology 137:110–118
Chou R, Cuevas C, Fu R, et al. (2015) Imaging techniques for the diagnosis of hepatocellular carcinoma: a systematic review and meta-analysis. Ann Intern Med 162:697–711
Bret PM, Labadie M, Bretagnolle M, et al. (1988) Hepatocellular carcinoma: diagnosis by percutaneous fine needle biopsy. Gastrointest Radiol 13:253–255
Giorgio A, Tarantino L, de Stefano G, et al. (2003) Complications after interventional sonography of focal liver lesions: a 22-year single-center experience. J Ultrasound Med 22:193–205
Caturelli E, Solmi L, Anti M, et al. (2004) Ultrasound guided fine needle biopsy of early hepatocellular carcinoma complicating liver cirrhosis: a multicentre study. Gut 53:1356–1362
Scholmerich J, Schacherer D (2004) Diagnostic biopsy for hepatocellular carcinoma in cirrhosis: useful, necessary, dangerous, or academic sport? Gut 53:1224–1226
Forner A, Vilana R, Ayuso C, et al. (2008) Diagnosis of hepatic nodules 20 mm or smaller in cirrhosis: prospective validation of the noninvasive diagnostic criteria for hepatocellular carcinoma. Hepatology 47:97–104
Durand F, Regimbeau JM, Belghiti J, et al. (2001) Assessment of the benefits and risks of percutaneous biopsy before surgical resection of hepatocellular carcinoma. J Hepatol 35:254–258
Takamori R, Wong LL, Dang C, Wong L (2000) Needle-tract implantation from hepatocellular cancer: is needle biopsy of the liver always necessary? Liver Transpl 6:67–72
Silva MA, Hegab B, Hyde C, et al. (2008) Needle track seeding following biopsy of liver lesions in the diagnosis of hepatocellular cancer: a systematic review and meta-analysis. Gut 57:1592–1596
Stigliano R, Marelli L, Yu D, et al. (2007) Seeding following percutaneous diagnostic and therapeutic approaches for hepatocellular carcinoma. What is the risk and the outcome? Seeding risk for percutaneous approach of HCC. Cancer Treat Rev 33:437–447
Rockey DC, Caldwell SH, Goodman ZD, et al. (2009) Liver Biopsy. Hepatology 49:1017–1044
Wald C (2014) A prospective, multicenter comparison of multiphase contrast-enhanced CT and multiphase contrast-enhanced MRI for diagnosis of hepatocellular carcinoma and liver transplant allocation https://www.acrin.org/Portals/0/Protocols/6690/ACRIN6690_Amend4_v022414-ForOnline.pdf
Santillan C, Fowler K, Kono Y, Chernyak V (2017) LI-RADS major features: CT, MRI with extracellular agents, and MRI with hepatobiliary agents. Abdom Radiol. doi:10.1007/s00261-017-1291-4
Bruix J, Sherman M (2005) Management of hepatocellular carcinoma. Hepatology 42:1208–1236
Tang A, Hallouch O, Chernyak V, Kamaya A, Sirlin CB (2017) Epidemiology of hepatocellular carcinoma: target population for surveillance and diagnosis. Abdom Radiol. doi:10.1007/s00261-017-1209-1
Darnell A, Forner A, Rimola J, et al. (2015) Liver imaging reporting and data system with MR imaging: evaluation in nodules 20 mm or smaller detected in cirrhosis at screening US. Radiology 275:698–707
Tanabe M, Kanki A, Wolfson T, et al. (2016) Imaging outcomes of liver imaging reporting and data system version 2014 category 2, 3, and 4 observations detected at CT and MR imaging. Radiology 281:129–139
Tang A, Fowler KJ, Chernyak V, Chapman WC, Sirlin CB (2017) LI-RADS and transplantation for hepatocellular carcinoma. Abdom Radiol. doi:10.1007/s00261-017-1210-8
Eisenhauer EA, Therasse P, Bogaerts J, et al. (2009) New response evaluation criteria in solid tumours: revised RECIST guideline (version 1.1). Eur J Cancer 45:228–247
Lencioni R, Llovet JM (2010) Modified RECIST (mRECIST) assessment for hepatocellular carcinoma. Semin Liver Dis 30:52–60
OPTN/UNOS policy 3.6.4.4. http://optn.transplant.hrsa.gov/policiesAndBylaws/policies.asp.
Wald C, Russo MW, Heimbach JK, et al. (2013) New OPTN/UNOS policy for liver transplant allocation: standardization of liver imaging, diagnosis, classification, and reporting of hepatocellular carcinoma. Radiology 266:376–382
Hayashi PH, Trotter JF, Forman L, et al. (2004) Impact of pretransplant diagnosis of hepatocellular carcinoma on cadveric liver allocation in the era of MELD. Liver Transpl 10:42–48
Park JW, Chen M, Colombo M, et al. (2015) Global patterns of hepatocellular carcinoma management from diagnosis to death: the BRIDGE Study. Liver Int 35:2155–2166
Bashir MR, Huang R, Mayes N, et al. (2015) Concordance of hypervascular liver nodule characterization between the organ procurement and transplant network and liver imaging reporting and data system classifications. J Magn Reson Imaging 42:305–314
Davenport MS, Khalatbari S, Liu PS, et al. (2014) Repeatability of diagnostic features and scoring systems for hepatocellular carcinoma by using MR imaging. Radiology 272:132–142
Joo I, Lee JM, Lee DH, et al. (2016) Liver imaging reporting and data system v2014 categorization of hepatocellular carcinoma on gadoxetic acid-enhanced MRI: comparison with multiphasic multidetector computed tomography. J Magn Reson Imaging. doi:10.1002/jmri.25406
Sofue K, Sirlin CB, Allen BC, et al. (2015) How reader perception of capsule affects interpretation of washout in hypervascular liver nodules in patients at risk for hepatocellular carcinoma. J Magn Reson Imaging. doi:10.1002/jmri.25094
Acknowledgements
This work was supported by the Fonds de recherche du Québec—Santé (Career Award #26993).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This study was funded by a clinical research scholarship by the Fonds de recherche du Québec—Santé and Fondation de l’association des radiologistes du Québec (Career Award #26993) to An Tang.
Conflict of interest
An Tang, Donald G. Mitchell and Claude B. Sirlin are members of the LI-RADS Steering Committee. Irene Cruite declares that she has no conflict of interest. Claude B. Sirlin has industry research grants from Bayer, Guerbet, Siemens, GE, Philips, Supersonic, and Arterys and consulting and service agreeements with Alexion, AstraZeneca, Bioclinica, BMS, Bracco, Celgene, Fibrogen, Galmed, Genentech, Genzyme, Gilead, Icon, Intercept, Isis, Janssen, NuSirt, Perspectum, Pfizer, Profil, Sanofi, Shire, Synageva, Tobira, Takeda, and Virtual Scopics.
Ethical approval
This article does not contain any studies with human participants performed by any of the authors.
Rights and permissions
About this article
Cite this article
Tang, A., Cruite, I., Mitchell, D.G. et al. Hepatocellular carcinoma imaging systems: why they exist, how they have evolved, and how they differ. Abdom Radiol 43, 3–12 (2018). https://doi.org/10.1007/s00261-017-1292-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00261-017-1292-3