Abstract
Purpose
To standardize workflow for dual-energy computed tomography (DECT) involving common abdominopelvic exam protocols.
Materials and methods
9 institutions (4 rsDECT, 1 dsDECT, 4 both) with 32 participants [average # years (range) in practice and DECT experience, 12.3 (1–35) and 4.6 (1–14), respectively] filled out a single survey (n = 9). A five-point agreement scale (0, 1, 2, 3, 4—contra-, not, mildly, moderately, strongly indicated, respectively) and utilization scale (0—not performing and shouldn’t; 1—performing but not clinically useful; 2—performing but not sure if clinically useful; 3—not performing it but would like to; 4—performing and clinically useful) were used. Consensus was considered with a score of ≥2.5. Survey results were discussed over three separate live webinar sessions.
Results
5/9 (56%) institutions exclude large patients from DECT. 2 (40%) use weight, 2 (40%) use transverse dimension, and 1 (20%) uses both. 7/9 (78%) use 50 keV for low and 70 keV for medium monochromatic reconstructed images. DECT is indicated for dual liver [agreement score (AS) 3.78; utilization score (US) 3.22] and dual pancreas in the arterial phase (AS 3.78; US 3.11), mesenteric ischemia/gastrointestinal bleeding in both the arterial and venous phases (AS 2.89; US 2.79), RCC exams in the arterial phase (AS 3.33; US 2.78), and CT urography in the nephrographic phase (AS 3.11; US 2.89). DECT for renal stone and certain single-phase exams is indicated (AS 3.00).
Conclusions
DECT is indicated during the arterial phase for multiphasic abdominal exams, nephrographic phase for CTU, and for certain single-phase and renal stone exams.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Dual-energy computed tomography (DECT) involves acquisition of two simultaneous datasets through the use of two different X-ray energy spectra, which in turn allows material decomposition analysis [1, 2]. Decomposition analysis is achieved through spectral separation and by exploiting the differences in CT number or attenuation ratios of two materials at low and high tube potentials (e.g., 80 and 140 kVp) [1, 3]. Tissue characterization through spectral separation was first reported in the late 1970s and early 1980s showing potential use [1, 4]. However, momentum of rapid spread and clinical adoption of early dual-energy technology was stifled by inherent technical limitations, such as noise from low tube potentials and spatial misregistrations between low- and high-energy datasets due to prolonged and separate data acquisitions [1, 3, 4]. However, these limitations were largely mitigated with the subsequent advent of newer CT technologies allowing more rapid data acquisition. Availability of simultaneous (e.g., dual-layer detector DECTs) and near simultaneous (e.g., single source, rapid kilovoltage-switching DECT and dual-source DECT) acquisition technology sparked renewed interest in DECT applications with resultant increase in reports of clinical applications in the literature [1, 3–15].
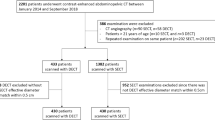
DECT applications in abdominal imaging have been widely reported, including use in liver, pancreas, renal, and adrenal imaging [1, 3–17]. Despite this and continued advances in the technology, widespread adoption and integration into routine clinical practice has not occurred [1]. This is despite well-reported benefits of increased lesion conspicuity, reduction in iodinated contrast media use, and lower overall exam radiation dose [16, 18–21]. Historically, higher radiation dose and poorer image quality of DECT compared with conventional single-energy CT (SECT) were cited for lack of widespread use. However, recent advances have allowed DECT to have equivalent or reduced radiation dose [through improvements in scan acquisition technology and replacement of true unenhanced (TUE) images with virtual unenhanced (VUE) images] and comparable image quality to SECT (through the use of noise reduction algorithms) [22–28]. Currently, the fee-for-service payment model in some ways disincentivizes the use of DECT. DECT studies with VUE images replacing TUE images cannot be charged as CT examinations requested for without and with intravenous contrast even though the patient receives less total radiation by virtue of eliminating an acquisition (i.e., the TUE). On the contrary, in future value-based alternative payment models, DECT can show tremendous value through reduced total radiation dose and the ability to lower volumes of iodinated contrast due to increased tissue contrast gained from lower energy monochromatic images. Additional barriers for adoption include multiple decision points that exist when considering incorporating DECT in clinical practice ranging from patient and exam type selection for dual-energy scanning as well as questions regarding image reconstruction, routing, and interpretation (Fig. 1). Moreover, contribution of dual-energy scanning on increased CT technologists’ workload must also be considered. Although there are reports of prior experience with successful clinical implementation of DECT into practice, universally accepted workflow standardization does not exist [2]. Moreover, a roadmap is needed to serve as initial reference points for those practices considering adopting DECT into their practice.
Decision tree flowchart showing examples of points of decisions that must be made when considering DECT implementation. CT computed tomography, DECT dual-energy computed tomography, SECT single-energy computed tomography, VMI virtual monochromatic images, PACS picture archiving and communication system
The purpose of this study was to therefore standardize patient selection and exam protocol workflow for DECT involving single and multiphasic abdominopelvic exams via a multi-institutional consensus.
Materials and methods
Conference participants and preparation
Twenty-two abdominal radiologists representing nine major academic institutions with expertise in and experience with DECT formed a working group. The purpose of this group was to discuss clinical and research applications of DECT as well as provide a forum for discussions related to DECT optimization and troubleshoot any challenges that may be encountered. The working group met regularly over live webinar sessions (GoToWebinar, Citrix Systems, LLC; Fort Lauderdale, FL). Prior to consensus gathering, two of the authors (B.P. and D.M.) presented a PowerPoint over a single live webinar session to the working group that included background material, including current DECT workflow and potential areas needing standardization. These authors also developed a standardized questionnaire (Qualtrics LLC, Provo, UT) with general questions on patient selection for DECT as well as specific questions on gastrointestinal and genitourinary CT protocol-specific questions (Fig. 2). The survey was reviewed and discussed by the working group over webinar sessions and subsequently revised based on those discussions. The final survey was then emailed to nine individuals (average number of years of DECT experience, 6.1 years; range 1–14 years) who were voluntarily selected to serve as faculty leads responsible for filling out the survey based on local consensus from discussions at their respective institutions.
Consensus scoring
For questions specific to CT examination protocols, two scoring systems were utilized with five-point ordinal scales (Table 1). Survey participants rendered a score for each protocol question using an agreement scale (AS) and a utilization scale (US) (both out of 4 points). The agreement scoring system was chosen to confer the degree of indication or contraindication of dual-energy CT for a particular protocol. The utilization score was chosen to provide information on current practice standards and experience with dual energy for a particular exam protocol. A consensus for the use of DECT was considered when a score of ≥2.5 was achieved for a scale. A 2.5 threshold was chosen as it would represent a majority score (i.e., 2.5 out of 4 total points or 62.5%).
Data collection and discussions
Survey responses from the nine institutions were collected and the data were analyzed. Collective responses from the nine institutions were tabulated and anonymized and presented to the working group over two live webinar sessions. Comments and discussions with salient points for each question and their results were captured.
Results
Demographics
A total of 32 abdominal radiologists from nine major academic institutions participated in formulating survey responses. This included 22 members of the working group and additional abdominal radiologists at each local institution chosen at the discretion of the faculty lead at each institution. The average number of years in practice among the participants was 12.3 years (range 1–35) with an average number of years of experience with DECT of 4.6 years (range 1–14). Four institutions are equipped with rapid kV-switching single-source DECT (rsDECT) scanners, one institution with a dual-source DECT (dsDECT), and four institutions have both platforms.
Patient selection
Seven (78%) institutions perform DECT based on the examination protocol type. Five (56%) institutions exclude large patients either by total body weight (n = 2), transverse dimension based on the frontal scout radiograph (n = 2), or both (n = 1). Weight cutoffs used include 260 lbs (118 kg) (n = 2) and 280 lbs (127 kg) (n = 1). Transverse diameter cutoffs used include 38 cm (n = 1), 42 cm (n = 1), and 46 cm (n = 1).
Image reconstruction and general preferences
For reconstruction of virtual monochromatic images from the acquired DECT datasets, 7 (78%) institutions prefer and send to picture archiving and communication system 50 keV for the low energy level (i.e., high contrast) and 70 keV for medium energy level (i.e., low noise). Few institutions reconstruct high keV virtual monochromatic images (i.e., metal artifact reduction), with energies of 120 keV (n = 1) or 140 keV (n = 3). Other institutions either do not reconstruct high keV virtual monochromatic images, or use metal artifact reduction algorithms or iodine material density images.
Eight (89%) institutions send iodine material density and virtual unenhanced images to the picture archiving and communication system (PACS). Eight (89%) use independent, vendor-specific thin-client software for selective cases depending on the need for advanced visualization and/or quantification of materials. Common examples of use for the thin-client platforms include material quantification (e.g., iodine) (n = 8), image optimization (e.g., select keV for optimal CNR) (n = 6), and image color overlays (n = 6). For DECT examination interpretation, 5 (56%) institutions stated their radiologists prefer using the same approach/order in viewing different series independent of the type of examination. The most common approach was viewing DECT datasets in the following order: high keV images, low keV images, virtual unenhanced images, and iodine material density images.
Examination-specific protocols
Multiphasic liver examination
DECT for multiphasic (i.e., arterial, portal venous, and delayed venous phases) liver CT examinations is indicated (AS 3.67; US 3.44) in the arterial phase (AS 3.78; US 3.22) and participants are performing it (Fig. 3). DECT during both arterial and venous phases is not indicated nor being performed (AS 2.22; US 2.33). Although there was interest in performing DECT during the portal venous or delayed phases for better detection of washout of hepatocellular carcinomas (HCC), most centers are not performing it (AS 2.67; US 2.22). DECT during the venous phases only is not indicated and not performed (AS 1.67; US 0.78). Additionally, participants agreed that a true unenhanced examination in addition to the multiphasic liver DECT dataset was not indicated (AS 1.56; US 0.44) as the VUE images usually suffice.
Dual pancreas examination
Surveyed participants agreed that DECT for dual pancreas is indicated with institutions currently performing it (AS 3.78; US 3.44) during the arterial phase (AS 3.78; US 3.11) (Fig. 4). DECT during both phases, even for certain indications, is not indicated nor are centers performing it (AS 2.44; US 2.33). Additionally, DECT during the venous phase only is not indicated and surveyed institutions do not perform it (AS 2.00; US 1.78). A true unenhanced examination in addition to DECT datasets is not indicated nor performed (AS 1.56; US 1.44).
Renal cell carcinoma (RCC) examination
DECT for RCC examinations is indicated and being performed (AS 3.44; US 3.33) in the arterial phase (AS 3.33; US 2.78) (Fig. 5). Participants agreed that DECT is not indicated and is not being performed during both arterial and venous phases (AS 1.89; US 1.78) or during the venous phase only (AS 2.44; US 2.22). DECT plus a true unenhanced examination is indicated and being performed (AS 2.67; US 2.89) as VUE images were not felt to adequately replace TUE images.
CT urogram
DECT for CT urography is indicated and performed (AS 3.33; US 3.22) during the nephrographic phase (AS 3.11; US 2.89) (Fig. 6). Additionally, DECT plus a true unenhanced exam is indicated and being performed (AS 2.78; US 2.78). During live discussion, participants agreed that VUE cannot currently completely replace TUE due to limitations of VUE images for renal application (see Discussion section “DECT for Multiphasic GU Exams”). DECT during both the nephrographic and excretory phases is not indicated nor is it being performed (AS 1.78; US 1.78).
Mesenteric ischemia/gastrointestinal bleeding exams
DECT for mesenteric ischemia and gastrointestinal bleeding is indicated (AS 3.33; US 3.00), particularly during the arterial phase (AS 3.11; US 3.11) (Fig. 7). Additionally, participants agreed that there would be value in performing DECT during both the arterial and venous phases (AS 2.89; US 2.79). Despite high utilization scores, most centers do not have much experience with performing DECT for this examination protocol. Surveyed participants agreed that VUE datasets can replace TUE examinations and that a TUE acquisition in addition to VUE dataset was not indicated (AS 1.78; 2.44).
Single-phase exams
DECT for routine single-phase (i.e., portal venous phase) exams for common indications such as abdominal pain or oncology follow-up is indicated (AS 3.00). Only 4 centers perform this while the remainder do not but would like to (US 3.11). During live webinar discussion, barriers that were cited for lack of adoption at respective institutions included the time required for image reconstruction and lack of uniform awareness of utility of DECT for single routine portal venous exams. For renal stone protocol, participants agreed that DECT is indicated (AS 3.00) for stone composition analysis depending on referring urologist preferences at particular institutions. Most centers would like to perform it (US 3.00) but do not based on their discussion with local urology referral practice who do not express desire for routine compositional analysis of stones.
Discussion
Although dual-energy CT applications in abdominal imaging have been well reported, widespread adoption into routine clinical practice has not occurred. Moreover, there continues to be significant variation in practice patterns and applications of the technology, which in turn can add to the challenge to a practice considering implementation of DECT. The results of this study could ease implementation of DECT in practice by providing basic guidelines that are based on common current practice patterns among large academic centers with experience. A summary of consensus statements derived from the results of our survey is listed in Table 2.
Patient and protocol selection
One of the challenges of DECT implementation is to determine which patients are appropriate for scanning. Lower energy monochromatic energy datasets provide higher contrast; however, there is a trade-off with associated higher noise as compared to the higher energy datasets [11, 15, 29, 30]. Larger body size can further degrade image quality due to associated increase in noise and likelihood of photon starvation [29, 31]. Studies have shown the impact of body sizes on the diagnostic performance of dual energy for various clinical applications [32–35]. dsDECT platforms have a limited reconstruction field of view associated with the high-voltage tube, with a maximum diameter of 26 cm for first generation and 33 cm for second-generation systems. Although central organs such as kidneys and pancreas may not be as affected with this system, it is critical to center the patient properly so that portions of the peripheral organs (such as, liver, small bowel, or colon) are not excluded from the reconstruction field of view [1, 2, 5, 11]. Large body sizes could make this positioning difficult. While the rsDECT has a full field of view (50 cm), the rapid switching between the high- and low-energy acquisition times results in relatively decreased X-ray flux making this system susceptible to noise with larger body sizes. Moreover, the lower tube potential cannot be altered and is limited to 80 kVp thereby limiting the ability to scan larger patients with acceptable image quality due to noise. The higher noise associated with the lower energy tube potential can be reduced through slowing the gantry rotation (increasing rotation time from 0.5 to 0.8 s) as well as through the use of iterative reconstruction techniques [1, 2, 5]. Because of the aforementioned effects of body size on image quality, many centers use a cutoff to exclude patients from dual-energy CT scanning. Our results showed that the practice patterns vary in terms of which parameters for cutoff (i.e., weight vs. transverse diameter from the initial scout image) are used. While the weight cutoffs were relatively similar among institutions that use a cutoff (260–280 lbs.), the lateral dimensions varied widely (38, 42, and 46 cm). This likely reflects the patient demographic makeup for each institution and the acceptable image noise level within the practice. There is a paucity of literature on which cutoff method is better to use (weight vs. lateral dimensions for dual energy) as well as what the optimal cutoff value should be. Guimarães et al reported that the optimal patient size cutoff to generate acceptable image quality with the low tube potential (80-kVp) ranged from 34.9 to 35.8 cm depending on the organ of interest being imaged using 14 × 1.2-mm detector configuration on a dual-source platform [31].
Another initial challenge for a practice considering DECT adoption is deciding how to determine which protocols will be performed with dual energy and which ones will not. A majority of the surveyed institutions incorporate DECT for specific exam protocols (i.e., dual pancreas CT) rather than incorporating it based on exam indication (e.g., pre-operative pancreatic cancer staging). This likely reflects the ease of implementation into workflow if protocols are designated for DECT scanning rather than sorting through indications to determine whether or not DECT scanning is appropriate for the clinical indication [2].
DECT for multiphasic GI exams
Our results showed that a majority of centers are performing dual-energy CT in the arterial phase for multiphasic liver exams. This practice pattern is well supported by studies showing increased lesion conspicuity of hypervascular tumors, such as HCC and hypervascular metastases, on lower energy virtual monochromatic energy datasets [17, 30]. In addition to HCC lesion detection, other DECT applications have been reported and include distinguishing bland from tumor thrombus with iodine quantification and detection of recurrence after trans-arterial chemoembolization using iodine material density images [36, 37]. Interestingly, our results also demonstrated growing interest in using dual-energy CT during the portal venous and/or delayed venous phases, in addition to the arterial phase, allowing potential improved detection of lesion washout in cases of HCC. Despite the interest, this was not routinely practiced at most centers, namely due to slight incremental increase in radiation dose on the single source platform as well as the lack of supporting data in the literature. At this time, the use of dual-energy CT during the venous phases for multiphasic liver exams is not a well-established practice pattern.
There was also a consensus among participants that dual-energy CT should be performed during the arterial phase for multiphasic pancreas examinations. Pancreatic parenchymal attenuation increases with lower tube potential, as expected, and this can improve lesion conspicuity of hypoattenuating tumors such as adenocarcinomas. Detecting small, less than 2 cm, pancreatic adenocarcinomas and isoattenuating pancreatic tumors, which occur in up to 11%–27% of cases, can pose a diagnostic challenge [3, 38]. Improved detection of small and isoattenuating pancreatic adenocarcinomas has been shown using lower energy monochromatic images which provide higher contrast between the tumor and normal parenchyma [3, 16]. Similarly, high-contrast lower energy monochromatic images can also aid in detecting small hypervascular pancreatic tumors, such as neuroendocrine [39] or renal cell carcinoma metastasis.
As one would expect, dual-energy CT could prove useful for the detection of gastrointestinal bleeding source or the detection of bowel ischemia. Our results showed most participants agreed that current dual-energy CT applications for bowel imaging could be useful in these scenarios. Despite this intuitive application, most centers that were surveyed do not have experience with implementing dual-energy CT scanning in these two clinical settings. To date, only two studies have demonstrated the role of dual-energy CT in detecting active gastrointestinal bleeding, both using a dual-source platform showing sensitivity for detection of active bleeding between 89%–94%. Both studies showed potential radiation dose savings of approximately 30% compared with conventional triple-phase scans (i.e., true unenhanced, arterial, and portal venous) and one study interestingly showed better image quality of the virtual unenhanced images as compared with true unenhanced images with no difference in CT numbers [21, 40]. Similarly, lower energy monochromatic images and iodine maps could be used to detect lack of bowel wall enhancement in cases of bowel ischemia. Animal models using rsDECT showed higher contrast-to-noise (CNR) ratios for ischemic bowel segments on reconstructed virtual monochromatic images as compared to the conventional polychromatic 120-kVp images, with 51-keV and iodine material density images having the highest CNRs [41]. Despite demonstration of maximum attenuation of bowel wall at low (i.e., 40-keV) energy monochromatic images and feasibility of dual-energy datasets to allow more confident detection of small bowel enhancement in one study, subjective noise was reported to be higher with monochromatic 70-keV images as compared with polychromatic images [42].
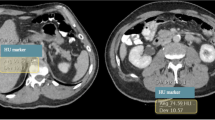
DECT for multiphasic GU examinations
As for the multiphasic GI exams, low-energy virtual monochromatic images reconstructed from the dual-energy dataset can, by way of increases contrast, increase the conspicuity of arterially enhancing renal masses, such as RCC. Low-energy virtual monochromatic images can also allow accurate pre-operative assessment of RCC and renal vasculature through increased iodine contrast. Our results reflect these applications with surveyed participants indicating dual-energy CT scanning commonly being performed for RCC protocols [43]. Iodine quantification can also be used to determine which subtype of renal cell carcinoma is present as well as confer the grade of the tumor [44].
For patients undergoing hematuria workup, a split-bolus technique with simultaneous acquisition of the nephrographic and excretory phases has been reported to carry a sensitivity for detection of upper tract urothelial carcinomas up to 99%–100%. Additionally, split-bolus dual-energy technique has the potential to reduce radiation dose by eliminating the TUE dataset and replacing it with the VUE dataset [45, 46]. Several studies have confirmed that VUE images can be comparable to TUE images in terms of renal lesion characterization and detection of contrast enhancement when comparing post-contrast images with VUE images [47–50]. However, VUE images remain limited in their use to due their susceptibility to noise artifacts as well as limitations in detecting small, less than 4-mm renal stones [51, 52]. Practice patterns across surveyed institutions support these data as there was a consensus that VUE cannot replace TUE for hematuria work-up at this time.
Renal lesion characterization can pose a diagnostic dilemma as often it can be difficult to distinguish benign hyperdense cysts from low-grade solid renal lesions due to high attenuation. Because of this, multiphasic renal studies are often subsequently obtained with a true unenhanced and nephrographic phase to determine if there is enhancement, defined as a change in attenuation between TUE images and nephrographic phase as an increase in attenuation of 10–20 Hounsfield Units (HU) [43, 53]. Additionally, small, less than 2 cm, simple cysts can show a spurious increase in attenuation, or pseudoenhancement, between the unenhanced and enhanced images largely attributed to beam hardening. Dual-energy reconstructed monoenergetic datasets simulate an ideal X-ray beam and are therefore not susceptible to beam hardening artifacts. Thus, DECT virtual monochromatic images can and have been shown to overcome pseudoenhancement and provide a solution to the aforementioned clinical dilemma when encountering pseudoenhancement on conventional multidetector CT [35]. Moreover, iodine material density images can allow easier detection of enhancement as voxels with iodine will be bright or color coded on iodine overlay images [11]. A quantitative approach using iodine material density images to determine enhancement may also be performed, with a threshold of 2 and 0.5 mg/mL for rsDECT and dsDECT, respectively [53].
DECT single phase
Our study showed that DECT for single-phase examinations, such as evaluation of acute abdominal pain or oncology follow-up is indicated though many were not performing it at their institution. Oncologic applications include lesion response to therapy, detection of recurrent or metastatic disease, and treatment planning [5]. Similarly, participants agreed that DECT for renal stone protocols can allow stone composition analysis. However, centers were only performing it based on the perceived value of composition analysis by their referring urologists. DECT can play a significant role in stratifying patient management through stone composition analysis. For example, DECT can allow discrimination of uric from non-uric acid stones as well as characterize those stones that may be resistant to extracorporeal shock wave lithotripsy [54, 55].
Limitations
Our study has several limitations that merit attention. First, the survey was limited to major academic institutions, and thus results and perceived issues with DECT adoption are biased toward those encountered in academic settings. Second, we also had a small sample size of nine institutions though individuals from each institution amounted to 32 total participants. Finally, our study was subject to inherent biases associated with survey-based works.
Conclusions
Although dual-energy CT applications in abdominal imaging have been well reported, there is a lag in widespread adoption. Despite the availability of literature, there is variability in DECT use and practice patterns across departments and imaging centers. This variability further adds to the challenge of those practices considering implementing DECT into their workflow. We herein provide a basic roadmap and guidance to those practices considering either adopting DECT or changing their current DECT workflow.
References
Marin D, Boll DT, Mileto A, Nelson RC (2014) State of the art: dual-energy CT of the abdomen. Radiology 271:327–342
Megibow AJ, Sahani D (2012) Best practice: implementation and use of abdominal dual-energy CT in routine patient care. AJR Am J Roentgenol 199:S71–77
Coursey CA, Nelson RC, Boll DT, et al. (2010) Dual-energy multidetector CT: how does it work, what can it tell us, and when can we use it in abdominopelvic imaging? Radiographics 30:1037–1055
Heye T, Nelson RC, Ho LM, Marin D, Boll DT (2012) Dual-energy CT applications in the abdomen. AJR Am J Roentgenol 199:S64–70
Agrawal MD, Pinho DF, Kulkarni NM, et al. (2014) Oncologic applications of dual-energy CT in the abdomen. Radiographics 34:589–612
Chandarana H, Megibow AJ, Cohen BA, et al. (2011) Iodine quantification with dual-energy CT: phantom study and preliminary experience with renal masses. AJR Am J Roentgenol 196:W693–700
De Cecco CN, Darnell A, Rengo M, et al. (2012) Dual-energy CT: oncologic applications. AJR Am J Roentgenol 199:S98–S105
Graser A, Johnson TR, Chandarana H, Macari M (2009) Dual energy CT: preliminary observations and potential clinical applications in the abdomen. Eur Radiol 19:13–23
Gupta RT, Ho LM, Marin D, et al. (2010) Dual-energy CT for characterization of adrenal nodules: initial experience. AJR Am J Roentgenol 194:1479–1483
Johnson TR, Krauss B, Sedlmair M, et al. (2007) Material differentiation by dual energy CT: initial experience. Eur Radiol 17:1510–1517
Kaza RK, Platt JF, Cohan RH, et al. (2012) Dual-energy CT with single- and dual-source scanners: current applications in evaluating the genitourinary tract. Radiographics 32:353–369
Silva AC, Morse BG, Hara AK, et al. (2011) Dual-energy (spectral) CT: applications in abdominal imaging. Radiographics 31:1031–1046 ((discussion 1047–1050))
Vrtiska TJ, Takahashi N, Fletcher JG, et al. (2010) Genitourinary applications of dual-energy CT. AJR Am J Roentgenol 194:1434–1442
Yeh BM, Shepherd JA, Wang ZJ, et al. (2009) Dual-energy and low-kVp CT in the abdomen. AJR Am J Roentgenol 193:47–54
Yu L, Leng S, McCollough CH (2012) Dual-energy CT-based monochromatic imaging. AJR Am J Roentgenol 199:S9–S15
Patel BN, Thomas JV, Lockhart ME, Berland LL, Morgan DE (2013) Single-source dual-energy spectral multidetector CT of pancreatic adenocarcinoma: optimization of energy level viewing significantly increases lesion contrast. Clin Radiol 68:148–154
Shuman WP, Green DE, Busey JM, et al. (2014) Dual-energy liver CT: effect of monochromatic imaging on lesion detection, conspicuity, and contrast-to-noise ratio of hypervascular lesions on late arterial phase. AJR Am J Roentgenol 203:601–606
Macari M, Spieler B, Kim D, et al. (2010) Dual-source dual-energy MDCT of pancreatic adenocarcinoma: initial observations with data generated at 80 kVp and at simulated weighted-average 120 kVp. AJR Am J Roentgenol 194:W27–32
Carrascosa P, Leipsic JA, Capunay C, et al. (2015) Monochromatic image reconstruction by dual energy imaging allows half iodine load computed tomography coronary angiography. Eur J Radiol 84:1915–1920
Chai Y, Xing J, Gao J, et al. (2016) Feasibility of virtual nonenhanced images derived from single-source fast kVp-switching dual-energy CT in evaluating gastric tumors. Eur J Radiol 85:366–372
Sun H, Hou XY, Xue HD, et al. (2015) Dual-source dual-energy CT angiography with virtual non-enhanced images and iodine map for active gastrointestinal bleeding: image quality, radiation dose and diagnostic performance. Eur J Radiol 84:884–891
Yamada Y, Jinzaki M, Hosokawa T, et al. (2014) Abdominal CT: an intra-individual comparison between virtual monochromatic spectral and polychromatic 120-kVp images obtained during the same examination. Eur J Radiol 83:1715–1722
Tawfik AM, Kerl JM, Razek AA, et al. (2011) Image quality and radiation dose of dual-energy CT of the head and neck compared with a standard 120-kVp acquisition. AJNR Am J Neuroradiol 32:1994–1999
Stiller W, Schwarzwaelder CB, Sommer CM, et al. (2012) Dual-energy, standard and low-kVp contrast-enhanced CT-cholangiography: a comparative analysis of image quality and radiation exposure. Eur J Radiol 81:1405–1412
Sommer CM, Schwarzwaelder CB, Stiller W, et al. (2012) Iodine removal in intravenous dual-energy CT-cholangiography: is virtual non-enhanced imaging effective to replace true non-enhanced imaging? Eur J Radiol 81:692–699
Ho LM, Yoshizumi TT, Hurwitz LM, et al. (2009) Dual energy versus single energy MDCT: measurement of radiation dose using adult abdominal imaging protocols. Acad Radiol 16:1400–1407
Pinho DF, Kulkarni NM, Krishnaraj A, Kalva SP, Sahani DV (2013) Initial experience with single-source dual-energy CT abdominal angiography and comparison with single-energy CT angiography: image quality, enhancement, diagnosis and radiation dose. Eur Radiol 23:351–359
Ma CL, Chen XX, Lei YX, et al. (2016) Clinical value of dual-energy spectral imaging with adaptive statistical iterative reconstruction for reducing contrast medium dose in CT portal venography: in comparison with standard 120-kVp imaging protocol. Br J Radiol 89:20151022
Yu L, Christner JA, Leng S, et al. (2011) Virtual monochromatic imaging in dual-source dual-energy CT: radiation dose and image quality. Med Phys 38:6371–6379
Marin D, Ramirez-Giraldo JC, Gupta S, et al. (2016) Effect of a noise-optimized second-generation monoenergetic algorithm on image noise and conspicuity of hypervascular liver tumors: an in vitro and in vivo study. AJR Am J Roentgenol 206:1222–1232
Guimaraes LS, Fletcher JG, Harmsen WS, et al. (2010) Appropriate patient selection at abdominal dual-energy CT using 80 kV: relationship between patient size, image noise, and image quality. Radiology 257:732–742
Mileto A, Nelson RC, Samei E, et al. (2014) Dual-energy MDCT in hypervascular liver tumors: effect of body size on selection of the optimal monochromatic energy level. AJR Am J Roentgenol 203:1257–1264
Leng S, Huang A, Cardona JM, Duan X, Williams JC, McCollough CH (2016) Dual-energy CT for quantification of urinary stone composition in mixed stones: a phantom study. AJR Am J Roentgenol: 1–9
Marin D, Pratts-Emanuelli JJ, Mileto A, et al. (2015) Interdependencies of acquisition, detection, and reconstruction techniques on the accuracy of iodine quantification in varying patient sizes employing dual-energy CT. Eur Radiol 25:679–686
Mileto A, Nelson RC, Samei E, et al. (2014) Impact of dual-energy multi-detector row CT with virtual monochromatic imaging on renal cyst pseudoenhancement: in vitro and in vivo study. Radiology 272:767–776
Ascenti G, Sofia C, Mazziotti S, et al. (2016) Dual-energy CT with iodine quantification in distinguishing between bland and neoplastic portal vein thrombosis in patients with hepatocellular carcinoma. Clin Radiol
Lee JA, Jeong WK, Kim Y, et al. (2013) Dual-energy CT to detect recurrent HCC after TACE: initial experience of color-coded iodine CT imaging. Eur J Radiol 82:569–576
Pietryga JA, Morgan DE (2015) Imaging preoperatively for pancreatic adenocarcinoma. J Gastrointest Oncol 6:343–357
Lin XZ, Wu ZY, Tao R, et al. (2012) Dual energy spectral CT imaging of insulinoma-value in preoperative diagnosis compared with conventional multi-detector CT. Eur J Radiol 81:2487–2494
Sun H, Xue HD, Wang YN, et al. (2013) Dual-source dual-energy computed tomography angiography for active gastrointestinal bleeding: a preliminary study. Clin Radiol 68:139–147
Potretzke TA, Brace CL, Lubner MG, et al. (2015) Early small-bowel ischemia: dual-energy CT improves conspicuity compared with conventional CT in a swine model. Radiology 275:119–126
Darras KE, McLaughlin PD, Kang H, et al. (2016) Virtual monoenergetic reconstruction of contrast-enhanced dual energy CT at 70 keV maximizes mural enhancement in acute small bowel obstruction. Eur J Radiol 85:950–956
Mileto A, Sofue K, Marin D (2016) Imaging the renal lesion with dual-energy multidetector CT and multi-energy applications in clinical practice: what can it truly do for you? Eur Radiol 26:3677
Mileto A, Marin D, Alfaro-Cordoba M, et al. (2014) Iodine quantification to distinguish clear cell from papillary renal cell carcinoma at dual-energy multidetector CT: a multireader diagnostic performance study. Radiology 273:813–820
Chow LC, Kwan SW, Olcott EW, Sommer G (2007) Split-bolus MDCT urography with synchronous nephrographic and excretory phase enhancement. AJR Am J Roentgenol 189:314–322
Maheshwari E, O’Malley ME, Ghai S, Staunton M, Massey C (2010) Split-bolus MDCT urography: upper tract opacification and performance for upper tract tumors in patients with hematuria. AJR Am J Roentgenol 194:453–458
Brown CL, Hartman RP, Dzyubak OP, et al. (2009) Dual-energy CT iodine overlay technique for characterization of renal masses as cyst or solid: a phantom feasibility study. Eur Radiol 19:1289–1295
Graser A, Johnson TR, Hecht EM, et al. (2009) Dual-energy CT in patients suspected of having renal masses: can virtual nonenhanced images replace true nonenhanced images? Radiology 252:433–440
Neville AM, Gupta RT, Miller CM, et al. (2011) Detection of renal lesion enhancement with dual-energy multidetector CT. Radiology 259:173–183
Song KD, Kim CK, Park BK, Kim B (2011) Utility of iodine overlay technique and virtual unenhanced images for the characterization of renal masses by dual-energy CT. AJR Am J Roentgenol 197:W1076–1082
Karlo CA, Gnannt R, Winklehner A, et al. (2013) Split-bolus dual-energy CT urography: protocol optimization and diagnostic performance for the detection of urinary stones. Abdom Imaging 38:1136–1143
Moon JW, Park BK, Kim CK, Park SY (2012) Evaluation of virtual unenhanced CT obtained from dual-energy CT urography for detecting urinary stones. Br J Radiol 85:e176–181
Kaza RK, Platt JF (2016) Renal applications of dual-energy CT. Abdom Radiol (NY) 41:1122–1132
Graser A, Johnson TR, Bader M, et al. (2008) Dual energy CT characterization of urinary calculi: initial in vitro and clinical experience. Investig Radiol 43:112–119
Bres-Niewada E, Dybowski B, Radziszewski P (2014) Predicting stone composition before treatment: can it really drive clinical decisions? Cent Eur J Urol 67:392–396
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
No funding was received for this study.
Conflict of interest
Bhavik N. Patel, Lauren Alexander, Brian Allen, Lincoln Berland, Amir Borhani, Courtney Moreno, Mitchell Tublin: no relevant financial disclosures; D. Morgan: research support, General Electric Healthcare; Dushyant Sahani: medical consultant and research support, General Electric Healthcare; royalties from Elsevier; William Shuman: research support, General Electric Healthcare; Eric Tamm: research support, General Electric Healthcare; Benjamin Yeh: research support from General Electric Healthcare; shareholder for Nextrast, Inc; royalties from Oxford University Press. D. Marin: research support, Siemens Healthcare. One of the authors (B.P.), who is neither an employee or consultant to industry, had control of the data and the information submitted for publication.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Informed consent
Statement of informed consent was not applicable since the manuscript does not contain any patient data.
Rights and permissions
About this article
Cite this article
Patel, B.N., Alexander, L., Allen, B. et al. Dual-energy CT workflow: multi-institutional consensus on standardization of abdominopelvic MDCT protocols. Abdom Radiol 42, 676–687 (2017). https://doi.org/10.1007/s00261-016-0966-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00261-016-0966-6