Abstract
Purpose
To define important elements of a structured radiology report of a CT or MRI performed to evaluate an indeterminate renal mass.
Methods
IRB approval was waived for this multi-site prospective quality improvement study. A 35-question survey investigating elements of a CT or MRI report describing a renal mass was created through an iterative process by the Society of Abdominal Radiology Disease-Focused Panel on renal cell carcinoma. Surveys were distributed to consenting abdominal radiologists and urologists at nine academic institutions. Consensus within and between specialties was defined as ≥70% agreement. Respondent rates were compared with Chi Square test.
Results
The response rate was 68% (117/171; 55% [39/71] urologists, 78% [78/100] radiologists). Inter-specialty consensus was that the following were essential: mass size with comparison to prior imaging, mass type (cystic vs. solid), presence of fat, presence of enhancement, and radiologic stage. Urologists were more likely to prefer the Nephrometry score (75% [27/36] vs. 22% [17/76], p < 0.0001), quantitative reporting of enhancement on CT (85% [32/38] vs. 46% [36/77], p < 0.0001), and mass position with respect to the renal polar lines (67% [24/36] vs. 36% [27/76], p = 0.002). There was inter-specialty consensus that the Bosniak classification for cystic masses was preferred. Most urologists (60% [21/35]) preferred management recommendations be omitted for solid masses or Bosniak III–IV cystic masses.
Conclusions
Important elements to include in a CT or MRI report of an indeterminate renal mass are critical diagnostic features, the Bosniak classification if relevant, and the most likely specific diagnosis when feasible; including management recommendations is controversial.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
The incidence of renal masses detected incidentally on imaging is increasing [1–5]. Most renal cancers are now detected with imaging performed for a non-renal complaint [5]. When a confident diagnosis cannot be rendered, incidental renal masses are considered indeterminate and typically are evaluated further with a CT or MRI using a protocol that is specifically designed to evaluate them [5–7]. Of the renal masses that are not treated, many undergo active surveillance with the same or similar imaging protocol [8–10]. These factors have led to a substantial increase in the number of radiology reports that describe renal masses. However, in our experience, the content of these radiology reports is inconsistent, perhaps due to a lack of guidance as to what are the most important elements to include in the report.
Although there is general understanding that some imaging features of a renal mass are essential to report (e.g., presence of fat [5, 7, 11]), the necessity of other radiologic findings (e.g., Nephrometry score [12, 13]) and the way findings are reported (e.g., methods of size measurement [14]) are less clear. Various studies have attempted to use imaging to better characterize renal masses and help select which need to be treated. Imaging findings such as presence of intracellular lipid [15–18], homogeneous hyperattenuation on non-contrast CT [19], enhancement patterns on CT and MRI [20, 21], and hypointensity on T2-weighted MR imaging [18, 19] have all been suggested (among others) as indicators of whether a renal mass is benign or malignant, what type of cancer is likely if the mass is malignant, or how aggressive a possible cancer might be. However, because the meaning of many of these features is not fully known [18, 19], there is no standard as to how or whether this information should be included in a CT or MRI report.
Additionally, some elements of a radiology report of a renal mass that have broad consensus in the literature (e.g., use of the Bosniak classification for cystic renal masses [5–7]) may not be used consistently due to incomplete knowledge or experience, or variable physician opinion (e.g., use of “complicated cyst” rather than “Bosniak II cyst” to describe a benign complicated cyst). Assessing the preferences of urologists—the principal group of referring non-radiologist physicians who manage indeterminate renal masses—and radiologists could help derive the essential elements of what could be included in a structured template when reporting a renal mass. Therefore, this survey was conducted to define the most important elements of a structured radiology report of a CT or MRI performed to evaluate an indeterminate renal mass.
Materials and methods
The requirement for informed consent was waived by the host institutional review board for this HIPAA-compliant prospective multi-center quality improvement survey.
Survey design and delivery
A 35-question survey investigating elements of a CT or MRI report describing an indeterminate renal mass was created through an iterative process by the Society of Abdominal Radiology Disease-Focused Panel on renal cell carcinoma. This panel is composed of 11 academic abdominal radiologists with an interest in renal cell carcinoma convened by the Society of Abdominal Radiology from nine tertiary care institutions in the United States: Brigham and Women’s Hospital, Cleveland Clinic, MD Anderson Cancer Center, New York University Langone Medical Center, University of California San Francisco Medical Center, University of Michigan Health System, University of Mississippi Medical Center, University of Texas Southwestern Medical Center, and Yale New Haven Hospital. The mission of the panel is to advance the radiologic contributions to the detection, diagnosis, and management of renal cell carcinoma.
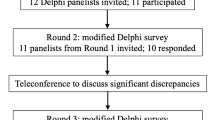
The survey was designed for dissemination to urologists and radiologists and included a variety of topics relevant to renal mass reporting. It was designed and implemented using an online web-based survey tool (Qualtrics, https://www.qualtrics.com/). There were no related pre-existing surveys to our knowledge. Therefore, content was created de novo from expert opinion and the literature. The development phase included five rounds of brainstorming, response compiling, and editing using a modified Delphi method. The following individuals participated: four expert radiologist members of the Disease-Focused Panel (rounds 1, 2, 4, 5); one multidisciplinary genitourinary oncology working group comprised of urologists, oncologists, and radiation oncologists (round 3); one expert urologist (round 4); two expert radiologists (round 4) who were not members of the Disease-Focused Panel; and one radiology resident (rounds 1, 2, 4, 5). Content was modified throughout the development phase using informal consensus.
The frame of the survey was for respondents to “indicate [their] preferences on what should be included in a structured report of a CT or MRI exam designed to evaluate an indeterminate renal mass.” The introductory email text accompanying the survey stated:
“The Society of Abdominal Radiology’s Disease-Focused Panel (DFP) on Renal Cell Carcinoma is developing a recommendation for a structured MRI/CT report of an indeterminate renal mass. We would like your opinion on what should be included, and how the information should be presented. The survey can be accessed from the link below, and should take less than 20 min to complete. You may leave and return to the survey as needed. Simply click on the link each time you wish to return to the survey and the program will track your progress.”
Therefore, the survey investigated the desired contents of a structured report of a CT or MRI performed to evaluate a renal mass and not the report of an incidental renal mass seen on a monophasic CT, for example. Survey questions specific to the radiology report body were grouped into the following categories: (1) basic imaging features of a renal mass, (2) methods of reporting renal mass size and growth, (3) methods of reporting details relevant to nephron-sparing treatment planning (i.e., surgery or percutaneous ablation), and (4) methods of reporting renal cancer stage. Survey questions specific to the radiology report impression were grouped into the following categories: (1) methods of reporting renal mass prognostic features, (2) methods of summarizing imaging features of a renal mass stratified by mass type, and (3) methods of reporting management recommendations. Respondent background and respondent clinical and research experience with renal masses were recorded, as were additional details not summarized above (report body and impression). A copy of the survey is shown in Appendix 1.
Surveys were distributed electronically from 9/10/2015 to 11/10/2015 to consenting academic abdominal radiologists (n = 95) and urologists (n = 59) at nine tertiary care academic institutions. One reminder was sent approximately 14 days after initial email.
Data analysis
Rates were summarized with counts and percentages and compared with Chi Square test. The response rate was calculated by dividing the number of respondents by the number of subjects offered to participate prior to consent [radiologists n = 100 (of which 95 consented to participate), urologists n = 71 (of which 59 consented to participate)]. Not all subjects who consented to participate actually completed the survey.
Intra- and inter-specialty consensus was defined as ≥70% agreement. This threshold was chosen so that with an alpha of 0.05 and a power 80%, the lower bound on the exact 95% binomial confidence interval (CI) for a sample of 37 subjects would remain a majority (i.e., >50%; [95% CI 53–84%]). Assuming an alpha of 0.05, a power of 80%, and a 2:1 response rate of radiologists to urologists, the number of respondents needed to observe a difference in proportions between specialties of 0.30 is 34 urologists and 68 radiologists. Statistical tests were performed in SPSS v.22 (IBM Corporation).
Results
Respondents
The response rate was 68% (117/171; 55% [39/71] urologists, 78% [78/100] radiologists). The response rate by institution ranged from 57% (8/14) to 91% (10/11) for radiologists and 33% (1/3) to 100% (10/10) for urologists. At least one radiologist (range 4–12) and one urologist (range 1–10) responded from every institution; median respondents per institution were nine radiologists and three urologists. Not all respondents answered every question; individual question response rates ranged from 92% (108/117) to 100% (117/117). Surveys required a median of 15 min to complete. Details of the survey population are provided in Table 1.
Basic imaging features of a renal mass
There was inter-specialty consensus that the following elements are essential in the reporting of a renal mass (Table 2): mass size (radiology 94% [72/77], urology 95% [36/38]), whether the mass is cystic or solid (radiology 88% [68/77], urology 97% [37/38]), presence or absence of fat (radiology 77% [59/77], urology 87% [33/38]), and presence or absence of enhancement (radiology 92% [71/77], urology 97% [37/38]). There was inter-specialty consensus that the following elements were either preferred or essential to include (Table 2): whether a solid mass has regions of necrosis (radiology 81% [62/77], urology 87% [33/38]), a description of the mass margins (e.g., infiltrative or circumscribed, radiology 88% [68/77], urology 92% [35/38]), a listing of the individual applicable criteria justifying the assigned Bosniak classification when reporting a cystic mass (radiology 71% [55/77], urology 95% [36/38]), and whether a portion or all of the mass enhances (radiology 78% [60/77], urology 74% [28/38]). Urologists were more likely to want enhancement on CT to be reported quantitatively rather than qualitatively, regardless of the method used (i.e., enhancement with or without calculations; 85% [32/38] vs. 46% [36/77], p < 0.0001) (Table 3).
Renal mass size comparisons to prior examinations
There was inter-specialty consensus that size comparisons were essential for solid masses (radiology 93% [71/76], urology 95% [35/37]), Bosniak IV cystic masses (radiology 87% [66/76], urology 81% [30/37]), and Bosniak III cystic masses (radiology 83% [63/76], urology 81% [30/37]) (Table 2). If only one method is used to report renal mass size, a larger proportion of radiologists and urologists preferred either the single largest diameter in any plane (radiology 30% [23/76], urology 24% [9/37]) or three orthogonal measurements (radiology 33% [25/76], urology 46% [17/37]) (Table 3). Among renal masses undergoing active surveillance, radiologists and urologists preferred (among the options given) that size comparisons be made to both the oldest and most recent comparison exams (radiology 62% [47/76], urology 49% [18/37]) (Table 3).
Renal mass imaging features related to nephron-sparing therapies
For renal masses in patients who might benefit from a nephron-sparing therapy, there was inter-specialty consensus that the following are preferred or essential to include (Table 2): axial location of the mass (e.g., anterior, radiology 93% [71/76], urology 84% [31/37]), capsular location of the mass (e.g., endophytic, radiology 91% [69/76], urology 84% [31/37]), distance of the mass to the sinus fat (radiology 70% [53/76], urology 70% [26/37]), and distance of the mass to the collecting system (radiology 71% [54/76], urology 76% [28/37]).
Urologists were more likely to consider the Nephrometry score to be preferred or essential to include (75% [27/36] vs. 22% [17/76], p < 0.0001), but there was no preference as to how the score should be reported (Table 3). Urologists were also significantly more likely to consider the relationship to the polar lines preferred or essential to include (67% [24/36] vs. 36% [27/76], p = 0.002).
Renal mass staging
There was inter-specialty consensus that radiologic staging details should always be reported for solid masses (radiology 95% [71/75], urology 94% [34/36]) and Bosniak IV cystic masses (radiology 91% [68/75], urology 92% [33/36]) (Table 4). Urologists were less likely to prefer that lymph node size be reported using only the short-axis diameter (36% [13/36] vs. 67% [50/75], p = 0.004). The largest proportion of urologists preferred bi-directional measurements (47% [17/36]) (Table 3).
There was consensus among urologists that tumor thrombus be reported with both anatomic descriptions of tumor thrombus extent and distances of the tumor thrombus to important structures (83% [30/36]); radiologists also preferred this combined qualitative and quantitative method of reporting tumor thrombus but did not reach consensus (64% [48/75]) (Table 3). Preferred measurements in the setting of tumor thrombus are shown by specialty in Table 3. There was inter-specialty consensus that it is preferred or essential to report whether there is bland thrombus peripheral to tumor thrombus (radiology 96% [72/75], urology 100% [36/36]) (Table 2).
Describing a renal mass in the impression
There was inter-specialty consensus that it was essential to report mass size in the impression for solid, Bosniak IV, Bosniak III, and Bosniak IIF renal masses (Table 5). When a Bosniak II mass was diagnosed, urologists were more likely to prefer that the mass be summarized in the impression as a “Bosniak II cyst” (urology 97% [34/35] vs. radiology 59% [43/73], p < 0.001), rather than with alternative nomenclature (e.g., “complicated cyst”) (Table 6). Including the Bosniak classification was considered preferred or essential by both specialties for Bosniak IV, Bosniak III, and Bosniak IIF renal masses (Table 5).
Radiologists were more likely than urologists to consider a differential diagnosis essential (solid 48% [35/78] vs. 14% [5/35], p = 0.002; Bosniak IV 34% [25/78] vs. 9% [3/35], p = 0.009; Bosniak III 33% [24/78] vs. 9% [3/35], p = 0.02; Bosniak IIF 32% [23/78] vs. 9% [3/35], p = 0.02), while urologists were more likely to consider the Nephrometry score [19, 20] preferred or essential (solid 17% [13/78] vs. 60% [21/35], p < 0.001; Bosniak IV 17% [13/78] vs. 63% [22/35], p < 0.001; Bosniak III 14% [11/78] vs. 57% [20/35], p < 0.001; Bosniak IIF 4% [3/78] vs. 31% [11/35], p < 0.001) (Table 5). Radiologists and urologists were more likely to prefer inclusion of the TNM stage as the probability of a mass being malignant increased (Table 6).
Predicting renal mass histology and biologic behavior
There was consensus among radiologists that it was preferred or essential to include in the impression the probability of malignancy for solid masses, and a majority of urologists and radiologists considered it preferred or essential to report the probability of malignancy for solid masses, Bosniak IV masses, and Bosniak III masses (Table 5). In this context, ‘probability of malignancy’ indicated a qualitative or quantitative expression of the likelihood that a mass was malignant. A majority of urologists (but not radiologists) thought it was preferred or essential to report the probability of malignancy for Bosniak IIF masses (Table 5). There was consensus among radiologists (81% [59/76]) that the probability of malignancy should be stated qualitatively (e.g., “likely malignant”) rather than quantitatively (e.g., “70% likely to be malignant”); urologists had no clear preference (Table 6). When there are imaging features present (e.g., T2w signal intensity) that might impart information about the biologic behavior of a renal mass, there was inter-specialty consensus that these findings should be reported, but the specialties disagreed on how that information should be summarized in the impression (Table 6).
If the imaging features of an indeterminate renal mass suggest but do not confirm a particular histology (e.g., fat-poor angiomyolipoma, papillary RCC), a majority of radiologists (86% [63/73]) and urologists (66% [23/35]) thought that this information should be reported and expressed qualitatively (e.g., “likely papillary RCC”), rather than stating a percentage likelihood.
Follow-up and management recommendations
Radiologists were more likely to consider management recommendations preferred or essential to include for solid masses (52% [38/73] vs. 23% [8/35], p = 0.006), Bosniak IV masses (48% [35/73] vs. 23% [8/35], p = 0.02), Bosniak III masses (53% [39/73] vs. 26% [9/35], p = 0.008) and Bosniak IIF masses (73% [53/73] vs. 31% [11/35], p < 0.001). Most urologists did not want management recommendations included in the report other than a specification of the best type and interval of imaging to use in follow-up (Table 7).
Discussion
Our survey has shown that radiologists and urologists have different expectations regarding what should be included in a CT or MRI report of an indeterminate renal mass. In general, for elements related to the description of a renal mass (i.e., elements not related to differential diagnosis or management), we found that consensus between specialties was more likely to be achieved when considering what features should be reported rather than how those features should be reported. Interestingly, some, albeit a small minority of academic radiologists and urologists, did not consider it essential to report certain features that are well documented to be critical in renal mass evaluation (e.g., presence of fat, presence of enhancement [5, 7, 11]). These findings demonstrate the need for improved education.
Urologists were more likely to prefer the Nephrometry score (75% [27/36] vs. 22% [17/76], p < 0.0001) [12, 13], more likely to prefer that enhancement on CT be reported quantitatively (85% [32/38] vs. 46% [36/77], p < 0.0001), more likely to prefer reporting of the relationship of a renal mass to the renal polar lines (67% [24/36] vs. 36% [27/76], p = 0.002) [12, 13], and less likely to want lymph node size reported using only the short-axis diameter (36% [13/36] vs. 67% [50/75], p = 0.004). The reasons for these disagreements were not investigated directly in the survey, but it is probable that they reflect specialty-specific practice patterns. For example, the Nephrometry score and the relationship of a mass to the renal polar lines are both factors that may influence nephron-sparing treatment decisions [12, 13], while reporting of quantitative enhancement on CT may be preferred by urologists, so they can be reassured about the degree of enhancement being reported by the radiologist. Additionally, the observed radiologist preference to report lymph nodes using a single short-axis diameter likely relates to radiologist experience with Response Evaluation Criteria in Solid Tumors (RECIST) and tumor measurements in general [24] and their familiarity with the weaker positive predictive value and weaker reproducibility of long-axis measurements relative to short-axis measurements for lymph nodes [24, 25]. The preference among urologists for bi-directional lymph node measurements does eliminate any confusion on which axis is being reported when only one measurement is provided.
Mass size was considered essential to report in the impression by both specialties, likely because it governs a variety of management steps. Specifically, when describing a suspected solid RCC, mass size is an important predictor of malignancy, is fundamental to the TNM staging system [26, 27], is used to monitor growth [10, 14, 28], affects the feasibility of nephron-sparing treatment options [29], and helps prognosticate and predict the probability of metastasis [30, 31]. Size comparisons were considered essential by both specialties for most renal mass types but the preferred method of reporting size was controversial. In general, both specialties preferred including a comparison to both the most recent examination and the oldest examination, likely because it is a better indicator of growth rate than a single proximate comparison.
Use of the Bosniak classification was considered preferred or essential by both specialties for Bosniak IIF, III, and IV cystic masses. There was consensus among urologists that use of this system was essential, even for Bosniak II masses, while radiologists were more likely to use the phrase “complicated cyst” in lieu of a Bosniak II designation. Neither specialty preferred the term “Bosniak I cyst”—both considered “simple cyst” to be a better option. One of the interesting results of the survey was that urologists in consensus thought radiologists should reiterate in the impression the supportive morphologic details of the Bosniak classification already listed in the report body. For example, when assigning a Bosniak IV designation, urologists would prefer the impression include “Bosniak IV cystic mass with an enhancing mural nodule” rather than simply “Bosniak IV cystic mass.” The reasons for this are unclear, though perhaps it might allow a urologist to verify or better understand the basis for the Bosniak classification assignment.
Although providing a differential diagnosis is a common practice by radiologists, urologists were significantly less likely to consider this essential when reporting an indeterminate renal mass. This may be because current management algorithms for small indeterminate solid masses [5, 7, 10, 27, 32, 33] and Bosniak IIF–IV masses [6, 7] typically base the recommended management strategies largely on size. However, current management algorithms do not dictate a strategy for all patients. A differential diagnosis that includes and expresses the probability of RCC relative to benign masses such as oncocytoma and fat-poor angiomyolipoma may still help determine whether treatment, biopsy, or active surveillance is appropriate. In addition, current management algorithms generally were conceived at a time in which radiologists were more limited in their ability to differentiate different types of solid masses (e.g., clear cell RCC vs. papillary RCC) or to predict biologic behavior. As imaging improves and management evolves, provision of a differential diagnosis—or a listing of imaging phenotypes from the point-of-view of mass aggressiveness (e.g., hypointensity on T2-weighted imaging [18, 19, 22, 23])—may prove increasingly helpful when selecting among various treatment options [9, 34]. Both specialties preferred that when possible the most likely histology be stated and expressed qualitatively (e.g., “likely papillary RCC,” “possible fat-poor angiomyolipoma”). Both specialties thought that having an imaging test that reliably could differentiate papillary RCC or clear cell RCC from other renal cancers would be helpful. This information highlights the potential impact of recent efforts to expand the ability of MRI and CT to predict histology [15–21].
However, the practice of translating predictive imaging information into management recommendations is controversial. For example, although certain imaging features might indicate a substantial benefit of percutaneous biopsy due to the higher likelihood of benignity and potential avoidance of unneeded surgery, only 37% [13/35] of urologists preferred such an explicit recommendation for biopsy to be made. In fact, a majority of urologists (60% [21/35]) preferred management recommendations be omitted for solid masses, Bosniak IV masses, or Bosniak III masses. Based on free-text responses by the urologists, common explanations for this opinion were that management decisions should be made “in person between the ordering physician and the patient depending on patient age, comorbidity, other malignancies, patient wishes, etc.” One urologist stated that management “suggestions [may] lead to anxiety and defensive medicine,” and another wrote that “management should…not be suggested unless you are seeing the patient directly.” Urologists preferred that radiologists only offer management recommendations that pertain directly to imaging, with a majority of urologists considering it preferred or essential to include information about the recommended interval and type of imaging follow-up. However, the provision of management options beyond imaging (e.g., percutaneous biopsy) could be helpful in certain situations because radiology reports may be received primarily by non-urologist physicians caring for the patient. Additionally, the survey did not capture the range of verbiage that can be used to suggest a management option; urologists may have welcomed management recommendations, if the wording was not ‘binding.’ For example, the following sentence, “possible options for management could include a percutaneous biopsy” may have engendered a more favorable response.
There are several limitations of our study. The survey was delivered only to academic abdominal radiologists and urologists in the United States; some of those institutions were represented by individual members of the survey design team. Other potential stakeholders are not represented, including international, non-academic (e.g., private practice), and non-specialized (e.g., general practitioners) physicians who may have different levels of knowledge and different opinions, raising the possibility of selection bias. General practitioners may be more interested in explanatory diagnostic terms (e.g., “benign complicated cyst” rather than “Bosniak II cyst”) or specific management recommendations than urologists. Our survey did not include a question-by-question opportunity for free-text entry—only a single general opportunity at survey conclusion; therefore, in some instances, we were unable to discern in retrospect why a particular answer was chosen. Provider preferences are only one component of a decision framework regarding what should be included in a hypothetical report. For example, some providers may not believe that a particular item is necessary to include even if it is grounded in evidence (e.g., use of the Bosniak classification [6, 7]). Lastly, this survey investigates a hypothetical future state in which these data are incorporated into a structured template describing a renal mass. It is possible that respondents’ opinions may change when faced with creating or consuming a more or less detailed report.
In conclusion, important elements to include in a CT or MRI report of an indeterminate renal mass are critical diagnostic features, the Bosniak classification if relevant, and the most likely specific diagnosis when feasible; including management recommendations is controversial. The information obtained from this survey can be used to derive a structured template for the reporting of a renal mass, inform radiologists about what is desired when describing a renal mass, and hopefully help standardize related dictations received by referring physicians.
References
Hollingsworth JM, Miller DC, Daignault S, et al. (2006) Rising incidence of small real masses: a need to reassess treatment effect. J Natl Cancer Inst 98:1331–1334
Lipworth L, Tarone RE, McLaughlin JK (2006) The epidemiology of renal cell carcinoma. J Urol 176:2353–2358
Ljungberg B, Campbell SC, Choi HY, et al. (2011) The epidemiology of renal cell carcinoma. Eur Urol 60:615–621
Bjorge T, Tretli S, Engeland A (2004) Relation of height and body mass index to renal cell carcinoma in two million Norwegian men and women. Am J Epidemiol 160:1168–1176
Silverman SG, Israel GM, Herts BR, et al. (2008) Management of the incidental renal mass. Radiology 249:16–31
Bosniak MA (2011) The Bosniak renal cyst classification: 25 years later. Radiology 262:781–785
Israel GM, Bosniak MA (2005) How I do it: evaluating renal masses. Radiology 236:441–450
Donat SM, Diaz M, Bishoff JT, et al. Follow-up for clinically localized renal neoplasms: AUA guideline. American Urological Association 2013. https://www.auanet.org/common/pdf/education/clinical-guidance/Renal-Cancer-Followup.pdf. Accessed: Jan 7, 2016.
Halverson SJ, Kunju LP, Bhalla R, et al. (2013) Accuracy of determining small renal mass management with risk stratified biopsies: confirmation by final pathology. J Urol 189:441–446
Silverman SG, Israel GM, Trinh QD (2015) Incompletely characterized incidental renal masses: emerging data support conservative management. Radiology 275:28–42
Bosniak MA, Megibow AJ, Hulnick DH, et al. (1988) CT diagnosis of renal angiomyolipoma: the importance of detecting small amounts of fat. AJR Am J Roentgenol 151:497–501
Kutikov A, Uzzo RG (2009) The RENAL nephrometry score: a comprehensive standardized system for quantitating renal tumor size, location and depth. J Urol 182:844–853
Parsons RB, Canter D, Kutikov A, et al. (2012) RENAL nephrometry scoring system: the radiologist’s perspective. AJR Am J Roentgenol 199:W355–W359
Orton LP, Cohan RH, Davenport MS, et al. (2014) Variability in computed tomography diameter measurements of solid renal masses. Abdominal Imaging 39:533–542
Outwater EK, Bhatia M, Siegelman ES, et al. (1997) Lipid in renal clear cell carcinoma: detection on opposed-phase gradient-echo MR images. Radiology 205:103–107
Pedrosa I, Sun MR, Spencer M, et al. (2008) MR imaging of renal masses: correlation with findings at surgery and pathologic analysis. RadioGraphics 28:985–1003
Jhaveri KS, Elmi A, Hosseini-Nik H, et al. (2015) Predictive value of chemical-shift MRI in distinguishing clear cell renal cell carcinoma from non-clear cell renal cell carcinoma and minimal-fat angiomyolipoma. AJR Am J Roentgenol 205:W79–W86
Hindman N, Ngo L, Genega EM, et al. (2012) Angiomyolipoma with minimal fat: can it be differentiated from clear cell renal cell carcinoma by using standard MR techniques? Radiology 265:468–477
Silverman SG, Mortele KJ, Tuncali K, et al. (2007) Hyperattenuating renal masses: etiologies, pathogenesis, and imaging evaluation. RadioGraphics 27:1131–1143
Kim JK, Park SY, Shon JH, et al. (2004) Angiomyolipoma with minimal fat: differentiation from renal cell carcinoma at biphasic helical CT. Radiology 230:677–684
Sun MR, Ngo L, Genega EM, et al. (2009) Renal cell carcinoma: dynamic contrast-enhanced MR imaging for differentiation of tumor subtypes—correlation with pathologic findings. Radiology 250:793–802
Oliva MR, Glickman JN, Zou KH, et al. (2009) Renal cell carcinoma: t1 and t2 signal intensity characteristics of papillary and clear cell types correlated with pathology. AJR Am J Roentgenol 192:1524–1530
Sasiwimonphan K, Takahashi N, Leibovich BC, et al. (2012) Small (<4 cm) renal mass: differentiation of angiomyolipoma without visible fat from renal cell carcinoma utilizing MR imaging. Radiology 263:160–168
Eisenhauer EA, Therasse P, Bogaerts J, et al. (2009) New response evaluation criteria in solid tumours: revised RECIST guideline (version 1.1). Eur J Cancer 45:228–247
Schwartz LH, Bogaerts J, Ford R, et al. (2009) Evaluation of lymph nodes with RECIST 1.1. Eur J Cancer 45:261–267
Edge SB, Byrd DR, Compton CC, et al. (2010) AJCC Cancer Staging Manual, 7th edn. New York: Springer-Verlag
NCCN Clinical Practice Guidelines in Oncology: Kidney Cancer V 2.2014 http://www.nccn.org/professionals/physician_gls/pdf/kidney.pdf. Accessed: Mar 5, 2016.
Jacobs BL, Tan HJ, Montgomery JS, et al. (2012) Understanding criteria for surveillance of patients with a small renal mass. Urology 79:1027–1032
Uzzo RG, Novick AC (2011) Nephron sparing surgery for renal tumors: indications, techniques, and outcomes. J Urol 166:6–18
Umbreit EC, Shimko MS, Childs MA, et al. (2012) Metastatic potential of a renal mass according to original tumour size at presentation. BJU Int 109:190–194
Chawla SN, Crispen PL, Hanlon AL, et al. (2006) The natural history of observed enhancing renal masses: meta-analysis and review of the world literature. J Urol 175:425–431
Umbreit EC, Thompson RH (2011) Metastatic potential of the small renal mass: why can’t we agree? Eur Urol 60:983–986
Novick AC, Campbell SC, Belldegrun A, et al. Guideline for management of the clinical stage 1 renal mass: AUA guideline. American Urological Association 2009. https://www.auanet.org/education/guidelines/renal-mass.cfm. Accessed: Jan 7, 2016.
Silverman SG, Gan YU, Mortele KJ, et al. (2006) Renal masses in the adult patient: the role of percutaneous biopsy. Radiology 240:6–22
Acknowledgements
Members of the SAR Disease-Focused Panel on Renal Cell Carcinoma: Matthew Davenport MD (Project Lead), University of Michigan Health System; Hersh Chandarana MD (DFP Co-Chair), NYU Langone Medical Center; Stuart Silverman MD (DFP Co-Chair), Brigham and Women's Hospital; Gary Israel MD, Yale New Haven Hospital; John Leyendecker MD, UT Southwestern Medical Center; Ivan Pedrosa MD, UT Southwestern Medical Center; Raghu Vikram MD, MD Anderson Cancer Center; Steve Raman MD, UCLA Medical Center; Erick Remer MD, Cleveland Clinic; Andrew Smith MD PhD, University of Mississippi Medical Center; Jane Wang MD, UCSF Medical Center.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Funding
No funding was received for this study.
Conflict of interest
Stuart G. Silverman received royalties from Wolters-Kluwer. J. Stuart Wolf, Jr is a member of the Urology Times Editorial Council. Matthew S. Davenport is a consultant to FDA and NCI, and received royalties from Elsevier and Wolters Kluwer. The other authors declare that they have no conflict of interest.
Ethical approval
Institutional review board approval was obtained and subjects consented to participate in the survey. All study procedures performed were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki declaration and its later amendments.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Davenport, M.S., Hu, E.M., Smith, A.D. et al. Reporting standards for the imaging-based diagnosis of renal masses on CT and MRI: a national survey of academic abdominal radiologists and urologists. Abdom Radiol 42, 1229–1240 (2017). https://doi.org/10.1007/s00261-016-0962-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00261-016-0962-x