Abstract
Purpose
The purpose of the study was to evaluate diagnostic yield and the added value of culture results on the clinical management of patients empirically treated with antibiotics prior to CT-guided drainage.
Methods
This retrospective, HIPAA-compliant, IRB-approved study reviewed records of 300 consecutive patients who underwent CT-guided aspiration or drainage for suspected infected fluid collection while on empiric antibiotics (11/2011 to 9/2013) at a single institution. Patient imaging and clinical characteristics were evaluated by an abdominal imaging fellow and culture results, and patient management were evaluated by an infectious diseases fellow.
Results
After exclusion of 14/300 (4.6%) patients who were not on empiric antibiotics and 8/300 (2.6%) patients in which no culture was acquired, 278 patients (average age 55 ± 16 years; M:F ratio 54:46) constituted the final study cohort. Leukocytosis was present in 163/278 (59%), and fever in 65/278 (24%). The average collection size was 8.5 ± 4.2 cm with gas present in 140/278 (50%) of collections; median amount drained was 35 mL, and visibly purulent material was obtained in 172/278 (63%). 236/278 (85%) received drains and the remainder were aspirated only. Average time between initiation of antibiotics and start of the drainage procedure was 4.1 ± 6.4 days (median 1.7 days). Cultures were positive in 205/278 (74%) patients with a resulting change in management in 181/278 (65%) cases. The change in management included change of antibiotics in 71/278 (26%), narrowing the antibiotic regimen in 94/278 (34%), and cessation of antibiotics in 16/278 (6%). Multidrug-resistant bacteria were cultured in 53/278 (19%). Several factors were found to be statistically significant predictors of positive cultures: patient leukocytosis (sens 62%, spec 53%), gas in the collection on CT (sens 59%, spec 77%), purulent material aspiration (sens 76%, spec 76%), and presence of polymorphonuclear cells in the specimen.
Conclusions
Despite predrainage antibiotic therapy, CT-guided drainage demonstrates a high yield of positive cultures and influences clinical management in the majority of patients.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Hospitalized patients with infectious symptoms are often placed on empiric antibiotic therapy in accordance with accepted clinical guidelines, particularly at-risk populations such as those who are postoperative, neutropenic, or who have presumed hospital-acquired infections [1–3]. Fluid collections later discovered in patients who have been empirically treated with antibiotics for other clinically diagnosed infections present a diagnostic dilemma as to whether the fluid collection was a source of the patient’s infectious symptoms or was an incidental finding such as seroma, loculated ascites, or other sterile fluid collection. Where fluid collections are infectious, percutaneous drainage offers direct therapeutic benefit [4], and diagnostic sampling can also help to improve the antibiotic regimen. Note that in cases of sterile fluid collections, drainage may be an unwarranted intervention, adding unnecessary risk for the patient and cost for the health care system [5, 6].
In several retrospective studies [7–9], the imaging characteristics alone of fluid collections have not proven to reliably predict the presence of infection, with variable rates of sterility found in clinically suspected infected collections in the liver (15%) [10], during fine needle lung aspiration (18%) [11], in cholecystectomy tubes (56%) [9], and hip aspirations (83%) [7]. Thus, although percutaneous drainage has low morbidity and mortality [8, 12, 13], some clinicians may be hesitant to submit patients who are on empiric antibiotics to a semi-invasive procedure as the collection could be presumed to have been sterilized by the antibiotics, therefore neither therapeutic drainage nor diagnostic specimen gathering would be required.
In cases with an elevated procedural risk due to the small size or location of the collection, the benefit of tailoring antibiotic therapy must be incorporated into the risk to benefit assessment.
At present, only two studies [5, 14] have evaluated the diagnostic yield of CT-guided drainage in patients with previous antibiotic treatment and reported a positivity rate of 63% [5] and 85% [14]. However, only 38 and 33 patients, respectively, were included and the added value of acquiring cultures from fluid collections in patients pretreated with antibiotics on changes to the antibiotic regime remains unknown.
The goal of our study was to quantify the diagnostic yield of microbiologic cultures obtained during CT-guided drainage in patients on empiric antibiotics and subsequently the clinical impact on patient antibiotic management.
Materials and methods
Study inclusion criteria
In this retrospective, HIPAA-compliant, IRB-approved study with a waiver of informed consent, we reviewed the records of 300 consecutive adult patients who underwent successful CT-guided aspiration or drainage for clinically suspected infection from November 1, 2011 through September 9, 2013 at a single tertiary care center. Inclusion criteria were as follows: CT-guided aspiration or drainage of a fluid collection in the chest, abdomen, or pelvis performed on both inpatients and outpatients. Aspirations that yielded no fluid, cholecystectomy tubes, superficial fluid collections (defined as external to the abdominal or pelvic fascia or outside of the chest pleural cavity), and joint aspirations were not included. Superficial collections were excluded as it was thought that these caused less diagnostic dilemma to their etiology (overlying cellulitis, known postoperative seroma from a superficial surgery, etc.), were relatively low risk, and routinely collected under ultrasound guidance. All patients without preinterventional antibiotic treatment were excluded from the study. Antibiotic treatment was initiated based on clinical presentation, as the patients presented with suspected infection.
Data collection
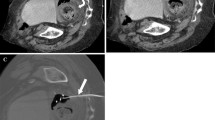
The patient’s imaging, CT reports, clinical characteristics, and culture results were reviewed by an abdominal imaging fellow (KLM), while the antibiotic treatments and patient management were evaluated by an infectious diseases fellow (RN). The images reviewed for data collection included the diagnostic CT leading to the identification of the targeted fluid collection, if performed within 24 h of the procedure; otherwise, the preprocedural, noncontrast, limited CT scan that was performed immediately prior to the procedure was evaluated.
Collected data from the CT images included measurement of the largest diameter of the targeted collection, whether the collection contained gas, the collection location (abdomen, pelvis, gallbladder fossa, liver, or pleura), as well as the date and time of the procedure. The differentiation of abdomen versus pelvis for the purposes of data collection was defined by the level of the iliac crests—below the crests was considered to be in the pelvis. By standard interventional radiology protocol in our institution, fluid collections smaller than 3 cm in size or those that contain clear serous fluid are aspirated, while drain is placed in the collections larger than 3 cm or in the collection with nonclear contents.
The following features were collected from the CT report: volume of aspirate, presence of visibly purulent-appearing fluid in the aspirate, and whether a drain was placed in addition to aspiration. Several dictations were incomplete and did not document the amount of fluid aspirated (n = 20) or the presence or absence of purulent material in the aspirate (n = 5). However, as the rest of the data were available, these patients were otherwise included in the analysis.
The following data were collected from the medical records: patient’s gender, age at the time of procedure, white blood cell count (WBC) prior to and during the 3 days following the procedure, and temperature. WBC trends were defined as an increase or decrease of 2 thousand white blood cells. If the patient was febrile, the following day’s temperature was also recorded. Leukocytosis was defined as greater than 11,000 cells per microliter, while fever was defined as body temperature greater than 100.4 degrees Fahrenheit. Defervescence was defined as a decrease in previously reported fever to below 100.4 degrees Fahrenheit on the day after the procedure. Additional culture data collected included the number of polymorphonuclear cells seen on Gram stain and the presence and type of organism growth.
Clinical data included the time and date of antibiotic coverage initiation, relevant patient comorbidities, and the reason, if known, for the fluid collection occurrence. The patient’s discharge date, whether the patient required further drainage procedures during the hospitalization, and subsequent ICU transfers for further treatment were also noted. To provide additional information in regards to patients that underwent aspiration only, additional detailed analysis was performed in this subgroup.
The infectious diseases fellow (yy) reviewed the medical record for culture results, including evaluation for the presence of multidrug-resistant organisms (defined as microorganisms nonsusceptible to at least 1 agent in 3 or more antimicrobial categories [15]), antibiotics that the patient was taking in the 24 h prior to the procedure, and for a change in antibiotic management based on the culture results. “Management change” was defined as a change in therapy (specifically, the addition of or a change to a different antibiotic), narrowing of the therapy (change from broad spectrum antibiotic to a specific narrow spectrum antibiotic, tailored for treatment of the specific detected pathogen), or the cessation of antibiotic therapy. “No change” to prior antibiotic therapy was also recorded.
Comorbidities such as malignancy, diabetes, immunocompromised status, intravenous drug abuse, or no known comorbidity (Table 1) were obtained. Etiology was determined by the location of the collection, patient’s diagnosis, and the recent surgical history and included gastrointestinal (all bowel-related etiologies such as postsurgical, inflammatory bowel disease, and diverticulitis), pancreas (pancreatic surgery and pancreatitis) and vascular (postendovascular interventions, encompassing both surgical and interventional radiology). Additional categories were postcholecystectomy, trauma, urologic, pleural, bacteremia, gynecologic, spinal surgery, miscellaneous, and unknown. Complications during the procedure and complications related to the procedure during the week after the intervention (such as bleeding, infection, and clogging of the drain) were reviewed in all patients that were admitted to the intensive care unit.
Statistical analysis
Statistical analysis was performed on Matlab (Mathworks, Natick, MA). Descriptive statistics were used to describe the study group. Kruskal–Wallis and ANOVA tests were used to evaluate the differences for medians and averages of the continuous variables such as age, collection size, and time interval between the initiation of antibiotic treatment and procedure. Difference in categorical variables such as gender, presence of visibly purulent material, presence of polymorphonuclear cells on Gram stain, presence of gas, fever, leukocytosis, and multidrug-resistant organisms were evaluated with Chi-square test. The statistical significance level was set at alpha = 0.05.
Results
Patient characteristics
300 consecutive patients underwent CT-guided aspiration or drainage for a suspected infectious collection during the study period. Twenty-two patients were subsequently excluded as they were either not on preprocedure antibiotics (14/300, 5%), or samples for culture were not sent from the procedure (8/300, 3%). A total of 278 patients constituted the final study cohort, with a mean age of 55 ± 16 years (range 18–92 years of age), all of which were on preprocedure antibiotics. There were 150 male and 128 female patients with a male to female ratio of 54–46 (Table 2). Leukocytosis was present in 163/278 (59%) and fever in 65/278 patients (24%) (Table 2). The average time between the initiation of antibiotics and the start of the drainage procedure was 4.1 ± 6.4 days (median of 1.7 days with a range of 0.01 days to 52.9 days) (Table 2). In 236/278 (85%) patients, a drainage catheter was placed whereas the remainder 42/278 (15%) were aspirated only. Clinical follow-up was available for 277/278 (99.6%) patients. One 83-year-old female patient with multiple comorbidities (celiac stenosis with chronic mesenteric ischemia, Crohn’s disease, and high blood pressure) and complicated postsurgical clinical course with ileus and admission to intensive care unit presented 30 days after bypass surgery with abdominal fluid collection of 9.9 cm. The procedure was uneventful; however, during transfer to the bed after the procedure, the patient became unresponsive and code was called. Pulseless electrical activity was recorded during the resuscitation efforts; however, no specific cause for death was identified. Despite full code, the patient expired.
Indication for CT guided intervention
A gastrointestinal cause was the most common etiology 135/278 (49%), followed by pancreatic etiology 47/278 (17%) (Table 3). Most of the patients (160/278 [58%]) had not known comorbidity at the time of the procedure (Table 1). The most common comorbidity present was malignancy 56/278 (20%), followed by diabetes 44/278 (16%). 161/278 (57.9%) of the patients had prior surgery including 90/278 (32.3%) gastrointestinal surgeries, 26/278 (9.4%) pancreatic surgeries, 18/278 (6.5%) cholecystectomies, 5/278 (1.8%) of gynecological, vascular, liver, and trauma surgeries, respectively, 2/278 (0.7%) urologic and spinal surgeries, respectively, and 3/278 (1.1%) surgeries for other indications.
Fluid collection characteristics
121/278 (44%) of the collections were located in the pelvis, 115/278 (41%) in the abdomen, 18/278 (7%) in the iliopsoas musculature, 12/278 (5%) in the liver, 9/278 (3%) within the pleura, and 3/278 (1%) in the gallbladder fossa. The average greatest dimension of the targeted fluid collection was 8.5 ± 4.2 cm (range 2.1–24.8 cm), with gas present in the collection in 140/278 patients (50%). The average amount of fluid removed per collection was 109 ± 211 mL (range of 1–1700 mL; median of 35 mL). Purulent material was obtained in the aspirated fluid in 172/278 patients (63%) (Table 2). 236/278 (85%) received drains, and the remaining fluid collections (42/278, 15%) were aspirated only.
Results of the cultures
Cultures were positive for growth (bacterial or yeast) in 205/278 (74%). The most frequent culture outcome was polymicrobial growth 81/278 (29%), followed by E. coli 53/278 (19%), and B. fragilis 50/278 (18%). Multidrug-resistant organisms were cultured in 53 patients, representing 19% of the entire cohort of 278 patients, and 26% of the 205 positive cultures.
Positive cultures were related to polymorphonuclear cells on the Gram stain of the fluid collection material (0 = 37/69, 54% positive cultures and 7/37, 19% MDRO; 1 = 43/59, 73% of positive cultures and 16/43, 37% of MDRO; 2 = 32/46, 70% of positive cultures and 8/32, 25% of MDRO; 3 = 32/40, 80 of positive cultures and 9/32, 28% of MDRO; 4 = 58/61, 95% of positive cultures and 12/58, 21% of MDRO).
Impact on clinical management
One patient died soon after the intervention. In the remaining patients, a change in antibiotic management due to the culture results occurred in 181/277 patients (65%, 95% CI 59–71%). A change in management was defined as either a change in antibiotics in 71/277 patients (26%, 95% CI 21–31%), narrowing the regimen in 94/277 (34%, 95% CI 28–40%), or a cessation of antibiotics in 16/277 (6%, 95% CI 3–9%).
Predictors of positive cultures
Statistically significant predictors of positive cultures (Table 2) were leukocytosis (sensitivity 62%, specificity 52%), gas in the collection (sensitivity 60%, specificity 78%), purulent material (sensitivity 77%, specificity 75%), the number of polymorphonuclear cells on the Gram stain specimen, and a shorter time interval between initiation of antibiotics and the start of the procedure (Table 2). Size of the fluid collection was also statistically significant, with a smaller collection associated with positive cultures. The presence of fever had high specificity (78%), but low sensitivity (24%), for culture positivity (Table 2).
The only statistically significant predictors for change in management were the presence of purulent material in the fluid collection (sensitivity 57%, specificity 30%) and the median time difference between the initiation of antibiotics and the start of the procedure (median 1.5 days for no change in management versus 2.1 days for change in management) (Table 4).
Patients with aspiration only
In the 42/278 patients (15.1%, 19 male, 23 female, 58.5 ± 15.2 years) that only underwent aspiration, median size of the fluid collection was 5.7 cm (interquartile range, IQR 3.8–7.7 cm) and amount of drained fluid was 10 mL (IQR 5–30 mL). Purulent material was aspirated in 17/42 (40.5%) of the patients, and air within the collection was found in 7/42 (16.7%) patients.
14/42 (33.3%) of the patients had positive cultures including 6/42 (14.3%) of the patients with MDROs. Antibiotic regimen was changed in 8/42 (19.0%), unchanged in 18/42 (42.9%), narrowed in 12/42 (28.6%), and stopped in 4/42 (9.5%).
Repeated procedure was necessary in 5/42 (11.9%) of the patients with a median fluid collection size of 5.7 cm (IQR 2.9–9.2 cm). 0/5 (0%) patients had gas in the collection, 3/5 (60%) had purulent material, 5/5 (100%) had leukocytosis, and 2/5 (40%) had fever.
Clinical follow-up of patients
Data for WBC levels were available in 249/278 (90%) patients. After the procedure, WBC levels decreased over a 3-day trend in 136/249 (54%) patients, while WBC levels increased in 33/249 patients (13%). No change in WBC levels occurred in 80/249 patients (32%). There was a significant correlation between decrease in WBC levels and positive culture (p = 0.01) as well as with change in management (p = 0.03).
Data for fever were available in 272/278 (98%) patients. Only 63/272 (23%) patients had fever within the 24 h prior to the procedure. Of those with fever, 30/63 (48%) patients remained febrile, while 33/63 patients (52%) defervesced. One patient who did not have a fever preprocedure developed a fever postprocedure (0.4%). There was no statistically significant correlation of fever with positive cultures, change in management, or postprocedure WBC trend. Infectious diseases consultation occurred in just under half of the patients (115/287, 40%), but statistically correlated with change in management (p = 0.0006) and was most often associated with changing or narrowing therapy (41/115 [36%] and 36/115 [31%], respectively).
Discussion
The diagnostic yield of microbiologic cultures acquired with CT-guided drainage in patients with previous empiric antibiotic treatment was 74% with a detection rate of 19% for multidrug-resistant organisms. The culture results changed antibiotic management in 65% of the patients and helped to narrow antibiotic treatment in 34% of the cases. Several significant predictors of positive cultures were found, including gas in the collection, smaller collection size, purulent material, and polymorphonuclear cells on Gram stain.
Prior studies recommended obtaining a sample from a fluid collection suspected of infection prior to antibiotics treatment due to decreased culture yield when performed afterwards [16–18]. We found that CT-guided aspiration of fluid collections has a very high yield of positive cultures of 74% despite varying durations of antibiotic therapy administered prior to the procedure. Our findings are in the range of previously reported values for abdominal fluid collections in patients without previous antibiotic treatment. Several studies evaluated diagnostic yield of fluid collection drainage and reported an infection rate of 60% [5], 62% [19], and 81% [14] for intraabdominal fluid collections and 85% for fluid collections in the liver [10]. The difference between reported values may be the result of the large variety of indications and locations for CT-guided drainage with diagnostic sampling. This is reflected by the variation of positivity rates for the different locations found in our study. Our results are also in accordance with a previous study [5, 14] showing a high diagnostic yield of 65% to 85% of cultures from CT-guided drainage in postsurgical patients on empiric antibiotics. However, only 38 patients were included in the Gnannt study [5] which reported a diagnostic yield of 65%. Postsurgical fluid collections may have a lower rate of infection than fluid collections in nonsurgical patients as patients are more likely to have seromas or loculated ascites. The added value for patient antibiotic treatment was not evaluated, which limits comparability to our study. Asai et al. [14] reported a diagnostic yield of 85% in patients on empiric antibiotics; however, only 33 patients with prior antibiotics were included, and the time of antibiotic treatment before drainage remains unclear.
Our findings support previous studies [16, 18] that found a decreased likelihood of obtaining positive cultures in patients with a longer duration on antibiotic therapy prior to sampling. However, we found that a longer time interval between antibiotic initiation and the procedure was associated with a higher likelihood for clinical management change regarding the patients’ antibiotic therapy. Therefore, our results indicate that although the likelihood for positive culture may be lower, the possible impact on clinical management justifies diagnostic sampling in patients despite a long duration of previous antibiotic treatment. Nevertheless, early diagnostic sampling of probable abscesses in patients on empiric antibiotics seems favorable.
We found that antibiotic regimen was changed due to culture results from CT-guided drainage in 65% of patients. This is higher than Asai’s previously reported 30% [14] however, which, only accounted for 14 patients. Additionally, Asai et al. [14] did not report how many of these patients were on empiric antibiotics prior to CT-guided drainage. Our high value of 65% for change in antibiotic management may be the result of consultation with an infectious diseases specialist. Interestingly, consulting an infectious disease specialist also significantly correlated with change in antibiotic management substantiating the established and important role of the infectious diseases specialist in the complicated treatment of patients with infections. This is especially important for the 34% of cases in which a positive culture led to narrowing of the antibiotic regime. Widespread use of antibiotics has led to a high number of multidrug-resistant organisms, which are a common problem in the clinical management of patients with suspected infection [20–22]. While just over a quarter of our patients grew multidrug-resistant organisms, the rate was significantly higher in immunocompromised patients. This is an important fact to consider when evaluating immunocompromised patients with fluid collections—the microbiologic yield of a drainage procedure may have a greater clinical impact in this patient population, since the presence of multidrug-resistant organisms increases the likelihood of a change in antibiotic management. The greater potential benefit should be considered when evaluating small or difficult to access fluid collections in immunocompromised patients. Additionally, a high rate of targeted antibiotic therapies can help to reduce the increase of multidrug-resistant organisms in the future.
We found that several imaging and clinical characteristics were associated with positive cultures. Gas within the fluid collection was associated with positive culture in our study. This is in accordance with previous studies [5, 23–25] which also reported gas within a fluid collection to be predictive of positive culture. The high diagnostic yield of entrapped gas is reflected within the scoring system invented by Gnannt et al. [5], in which gas is the second most important factor. Interestingly, a smaller collection size was also associated with positive cultures. This could be because collections that are infected may clinically present earlier, whereas a sterile collection may grow to a larger size before becoming clinically apparent or possibly superinfected. Not surprisingly, procedure-related positive culture and change in management predictors included the aspiration of purulent material and a higher number of polymorphonuclear cells on Gram stain. However, based on our findings, we would not recommend that nonpurulent aspirates be discarded. Of note, fever showed no correlation with positive blood cultures or change in management in our study. Fever has been described to be an unreliable predictor of infection in patients with fluid collections due to its low specificity and many possible biases such as fever-reducing drugs [5, 26].
Several limitations were present in our retrospective study. Our study included only CT-guided aspirations and drainages; therefore, the data regarding liver and gallbladder fossa locations are limited, as most of these procedures are performed under ultrasound. In most of the patients (85%) in our study, drainage of the fluid collection was performed; however, some fluid collections were only aspirated, as the collection was small or contents were clear serous fluid. This may have affected our results. To provide additional information, patients with aspiration were analyzed separately. Additional bias includes results acquired from a single tertiary institution in which early empiric treatment with broad spectrum antibiotics is frequent. Conclusions regarding specific predictors are limited by the exploratory nature of the study. Previously evaluated imaging features such as attenuation and wall delineation [5, 24] were not part of our study, and we did not perform logistic regression analysis to implement a model of prediction. While this has been done previously [5], the focus of our study was the added value of diagnostic sampling via CT-guided drainage for antibiotic treatment. Additionally, we imply that administering a culture-appropriate antibiotics regimen would benefit patients but did not provide proof of this matter in the paper, as this issue is beyond the scope of this study. We found that changes in antibiotic management were significantly correlated to an overall trend of decreasing WBC count. Although this may demonstrate the effectiveness of therapy tailoring, it can also be the result of the removal of the offending infected collection, which would coincide, but not be causally related to, the change in antibiotic management.
In conclusion, microbiological cultures from CT-guided drainage in patients already on antibiotics were positive in 74% and led to a change in management in 65%. Infectious diseases consultation and multidrug-resistant organisms, which were more commonly seen in immunocompromised patients, were significantly correlated with changes in therapy. Our results indicate that a high diagnostic yield and an impact on patient treatment in the majority of cases justify diagnostic sampling via CT-guided drainage in patients with fluid collections, irrespective of their previous antibiotic treatment.
References
American Thoracic Society, Infectious Diseases Society of America (2005) Guidelines for the management of adults with hospital-acquired, ventilator-associated, and healthcare-associated pneumonia. Am J Respir Crit Care Med. 171:388–416
Freifeld AG, Bow EJ, Sepkowitz KA, et al. (2011) Clinical practice guideline for the use of antimicrobial agents in neutropenic patients with cancer: 2010 update by the infectious diseases society of america. Clin Infect Dis Off Publ Infect Dis Soc Am. 52:e56–e93
Kendrick JE, Numnum TM, Estes JM, et al. (2008) Conservative management of postoperative Fever in gynecologic patients undergoing major abdominal or vaginal operations. J Am Coll Surg. 207:393–397
To J, Aldape D, Frost A, et al. (2014) Image-guided drainage versus antibiotic-only treatment of pelvic abscesses: short-term and long-term outcomes. Fertil Steril. 102:1155–1159
Gnannt R, Fischer MA, Baechler T, et al. (2015) Distinguishing infected from noninfected abdominal fluid collections after surgery: an imaging, clinical, and laboratory-based scoring system. Invest Radiol. 50:17–23
Gee MS, Kim JY, Gervais DA, Hahn PF, Mueller PR (2010) Management of abdominal and pelvic abscesses that persist despite satisfactory percutaneous drainage catheter placement. Am J Roentgenol 194:815–820
Kung JW, Yablon C, Huang ES, Hennessey H, Wu JS (2012) Clinical and radiologic predictive factors of septic hip arthritis. Am J Roentgenol. 199:868–872
Mehendiratta V, McCarty BC, Gomez L, Graviss EA, Musher DM (2007) Computerized tomography (CT)-guided aspiration of abscesses: outcome of therapy at a tertiary care hospital. J Infect. 54:122–128
Sosna J, Kruskal JB, Copel L, Goldberg SN, Kane RA (2004) US-guided percutaneous cholecystostomy: features predicting culture-positive bile and clinical outcome. Radiology 230:785–791
Zibari GB, Maguire S, Aultman DF, McMillan RW, McDonald JC (2000) Pyogenic liver abscess. Surg Infect. 1:15–21
Peña GN, Muñoz LF, Vargas RJ, et al. (1990) Yield of percutaneous needle lung aspiration in lung abscess. Chest. 97:69–74
Schechter S, Eisenstat TE, Oliver GC, Rubin RJ, Salvati EP (1994) Computerized tomographic scan-guided drainage of intra-abdominal abscesses. Preoperative and postoperative modalities in colon and rectal surgery. Dis Colon Rectum. 37:984–988
Schurawitzki H, Karnel F, Stiglbauer R, Schimmerl S, Salomonowitz E (1987) CT-guided percutaneous drainage and fluid aspiration in intensive care patients. Acta Radiol Stockh Swed 1992(33):131–136
Asai N, Ohkuni Y, Yamazaki I, et al. (2013) Therapeutic impact of CT-guided percutaneous catheter drainage in treatment of deep tissue abscesses. Braz J Infect Dis Off Publ Braz Soc Infect Dis. 17:483–486
Magiorakos A-P, Srinivasan A, Carey RB, et al. (2012) Multidrug-resistant, extensively drug-resistant and pandrug-resistant bacteria: an international expert proposal for interim standard definitions for acquired resistance. Clin Microbiol Infect. 18:268–281
Grace CJ, Lieberman J, Pierce K, Littenberg B (2001) Usefulness of blood culture for hospitalized patients who are receiving antibiotic therapy. Clin Infect Dis Off Publ Infect Dis Soc Am. 32:1651–1655
Chahoud J, Kanafani Z, Kanj SS (2014) Surgical site infections following spine surgery: eliminating the controversies in the diagnosis. Front Med. 1:7
Ghanem E, Richman J, Barrack R, et al. (2009) Do preoperative antibiotics decrease intraoperative culture yield? Orthop Proc. 91B:175
van Sonnenberg E, Mueller PR, Ferrucci JT (1984) Percutaneous drainage of 250 abdominal abscesses and fluid collections. Part I: Results, failures, and complications. Radiology 151:337–341
Lutz P, Nischalke HD, Strassburg CP, Spengler U (2015) Spontaneous bacterial peritonitis: the clinical challenge of a leaky gut and a cirrhotic liver. World J Hepatol. 7:304–314
Chakupurakal R, Ahmed M, Sobithadevi DN, Chinnappan S, Reynolds T (2010) Urinary tract pathogens and resistance pattern. J Clin Pathol. 63:652–654
Division of Healthcare Quality Promotion, National Center for Emerging and Zoonotic Infectious Diseases, Centers for Disease Control, and Prevention,. ANTIBIOTIC RESISTANCE THREATS in the United States, 2013, http://www.cdc.gov/drugresistance/pdf/ar-threats-2013-508.pdf. Accessed 5 May 2016.
Haaga JR, Alfidi RJ, Havrilla TR, et al. (1977) CT detection and aspiration of abdominal abscesses. Am J Roentgenol. 128:465–474
Jaques P, Mauro M, Safrit H, Yankaskas B, Piggott B (1986) CT features of intraabdominal abscesses: prediction of successful percutaneous drainage. Am J Roentgenol. 146:1041–1045
Liao W-I, Tsai S-H, Yu C-Y, et al. (2012) Pyogenic liver abscess treated by percutaneous catheter drainage: MDCT measurement for treatment outcome. Eur J Radiol. 81:609–615
Circiumaru B, Baldock G, Cohen J (1999) A prospective study of fever in the intensive care unit. Intensive Care Med. 25:668–673
Funding
No funding was received for this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Rights and permissions
About this article
Cite this article
McGillen, K.L., Boos, J., Nathavitharana, R. et al. Diagnostic yield and clinical impact of microbiologic diagnosis from CT-guided drainage in patients previously treated with empiric antibiotics. Abdom Radiol 42, 298–305 (2017). https://doi.org/10.1007/s00261-016-0833-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00261-016-0833-5