Abstract
Purpose
The prognostic value of 18F-deoxyglucose positron emission tomography (18F-FDG PET) on hepatocellular carcinoma (HCC) remains inconclusive. This study aims to investigate the prognostic role of pretreatment 18F-FDG PET on HCC patients by meta-analysis.
Methods
PubMed, Embase, Cochrane library, and Wanfang databases were searched until June 2015. Hazard ratios (HRs) with corresponding 95% confidence intervals (CIs) were synthesized by Stata 10.0, and the combined results were used as effective values.
Results
Twenty-two studies containing a total of 1721 patients were identified. According to random-effect model, meta-analysis results showed that high Tumor SUV/Liver SUV (Tsuv/Lsuv) ratio was significantly associated with poorer overall survival (OS) (HR = 2.04; 95% CI 1.50–2.79; P = 0.000) and poorer disease-free survival (HR = 7.17; 95% CI 3.58–14.36; P = 0.000); and high Tumor SUV (Tsuv) value was also correlated with poor OS (HR = 1.53; 95% CI 1.26–1.87; P = 0.000). Meanwhile, subgroup analysis results showed that the significant association above was not altered by study sample size, parameter cutoff value, analytic method, and follow-up period, but there was no significant association between Tsuv/Lsuv ratio and OS in patients who underwent resection (HR = 1.71; 95% CI 1.00–2.92; P = 0.052).
Conclusions
Both high Tsuv/Lsuv ratio and high Tsuv value are associated with poor prognosis in HCC patients. Therefore, pretreatment 18F-FDG PET is a useful tool in predicting the prognosis of HCC patients. More studies with explicit treatment modalities are required to investigate the prognostic value of pretreatment 18F-FDG PET on HCC patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Hepatocellular carcinoma (HCC) accounting for most of primary liver cancer (70%–90%) is the fifth most common cancer diagnosed in male and ninth in female worldwide [1]. According to the GLOBOCAN 2012, an estimated 782,500 new liver cancer cases and 745,500 deaths occurred worldwide during 2012, making it the second most common cause of cancer-related deaths (after lung cancer) [1]. Although advancements have been achieved in the treatments of HCC, the prognosis of HCC patients remains poor with 5-year survival rate ranging from 12% to 23% [2]. Serving as a curative and predominant treatment for HCC, the recurrence rate after resection is approximately 50% at 2 years and 75% at 5 years [3]. Therefore, accurate prediction of survival and early detection of recurrence will be critical for HCC management.
[18F] Fluorodeoxyglucose (FDG) PET is a functional imaging tool by providing metabolic information, which is widely used in the detection of gastrointestinal malignancies, such as gastric cancer, pancreatic cancer, and hepatobiliary cancers [4, 5]. Meanwhile, 18F-FDG PET also plays an important role in gastrointestinal malignancies managements, e.g., staging in pancreatic cancer, evaluation of response to treatments in colorectal cancer, and detection of recurrence and metastases in HCC [6–10]. However, the prognostic value of pretreatment 18F-FDG PET on HCC remains inconclusive, though many studies have investigated its role on HCC patients.
This meta-analysis aims to investigate the prognostic role of pretreatment 18F-FDG PET on HCC patients, in which Tumor SUV/Liver SUV (Tsuv/Lsuv) ratio and Tumor SUV (Tsuv) were used as parameters of 18F-FDG PET, and overall survival (OS) and disease-free survival (DFS) were used as outcomes of HCC patients.
Materials and methods
Search strategy
A systemic search of PubMed, Embase, Cochrane library, and Wanfang databases was performed up to June 2015. The following keywords were used: (“hepatocellular carcinoma” or “liver cancer” or “HCC”) and (“PET” or “18F-fluorodeoxyglucose PET/CT” or “18F-FDG PET”). The search strategy used in PubMed is as follows: “((((hepatocellular carcinoma[Title/Abstract]) OR liver cancer[Title/Abstract]) OR HCC[Title/Abstract])) AND (((18F-fluorodeoxyglucose PET/CT[Title/Abstract]) OR 18F-FDG PET[Title/Abstract]) OR PET[Title/Abstract]).” The references list of retrieved articles was manually screened, in order to gain potential eligible studies.
Selection and exclusion criteria
Studies were included if they fulfill the following criteria: (1) studies investigating the prognostic role of 18F-FDG PET on HCC patients; (2) 18F-FDG PET results were obtained before any treatments; (3) survival results were provided in the original article, such as OS or/and DFS; and (4) relative hazard ratios (HRs) with corresponding 95% confidence intervals (CIs) were available.
Studies were excluded if they met any of the following items: (1) case reports, comment letters, reviews, and duplicates; (2) 18F-FDG PET results were obtained after treatments; (3) the tracer used for PET was not 18F-FDG; (4) other parameters were used rather than common indicators (Tsuv/Lsuv ratio, Tsuv value), such as Tumor SUV/Mediastinum SUV ratio; (5) without survival results, such as OS/DFS; (6) HRs with corresponding CIs were not available; (7) the HRs provided in article were paradoxical obviously; and (8) HRs calculated from available data or Kaplan–Meier were significantly different from the original statistical significance, in terms of P value. If the studies were based on the same origin of population, only the most complete ones were enrolled. Besides, we did not set limitations for language or study sample size during this process.
Data extraction
Two investigators performed data extraction from each potentially included study independently. The extracted data are as follows: the first author, year of publication, origin of population, study sample size, cancer stage, treatments, parameters (Tsuv/Lsuv ratio or Tsuv value), cutoff values for parameters, study endpoints (OS, DFS), HRs with corresponding 95% CIs, HR sources (direct, available data, and Kaplan–Meier curve), and follow-up period. If both univariate and multivariate analyzing results were provided in the same study, then we selected the latter one. When HRs were not provided directly in the article, the total numbers of observed deaths/cancer recurrences and the numbers of samples in each group were extracted to calculate HRs [11]. Besides, we also used Engauge Digitizer version 4.1 (http://sourceforge.net) to read the Kaplan–Meier curves when the data above were not available either; then we calculated the HRs with their corresponding CIs as before [11]. However, we excluded articles which provided paradoxical survival results, and articles in which survival results calculated from Kaplan–Meier curve were significantly different from the original statistical significance, in terms of P value. During this process, discrepancies were resolved by consensus in the meeting organized by a senior investigator.
Statistical analysis
This meta-analysis was performed using Stata 10.0. Pooled HRs with corresponding 95% CIs were used to assess the impact of parameters (Tsuv/Lsuv ratio, Tsuv value) on HCC patients. A combined HR > 1 indicated poor prognosis for patients with high Tsuv/Lsuv ratio or high Tsuv value. The heterogeneity among studies was measured using Cochrane Q test (assessing the P value) and I 2 statistic [12]. If I 2 > 50% or/and P < 0.1, the random-effect model was used; otherwise, the fixed-effect model was used. Both Begg’s and Egger’s tests were used to examine the potential publication biases [13, 14]. All P values were two sided, and P < 0.05 indicates statistical significance.
Methodological assessment
In this meta-analysis, we did not perform methodological assessment, because there is no widely agreed quality for assessing prognostic studies [15]. However, we strictly carried out the inclusion and exclusion criteria during the literature search. Besides, we made sure there was no duplication of data during the data extraction, especially those studies conducted in the same center.
Results
Literature search information
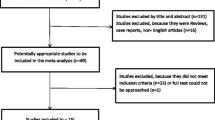
Initially, we identified 766 studies by using the key words provided before in the available databases. Next, we excluded 715 studies by reading the title and abstract, because these studies were not related with our research purpose. Of the remained 51 studies, 29 studies were excluded due to duplicates (n = 10), without enough or correct survival data (n = 7), research purpose unrelated (n = 10), and full-text unavailable (n = 2). Finally, there were 22 studies included in this meta-analysis (nineteen in English, two in Chinese, and one in Korean) [16–37]. Details of the search process are given in Fig. 1.
Characteristics of included studies
The baseline of included studies is shown in Table 1. Totally, there were twenty-two studies with 1721 patients included in this meta-analysis. The study sample size ranged from 25 to 298 (median number 61). Nineteen of the included studies were conducted in Asia (11 in Korea, 5 in Japan, and 3 in China), and the other three were conducted in Germany, Canada, and Belgium. Regarding treatments, transplantation was used in six studies, transarterial chemoembolization (TACE) was used in four studies, resection was used in five studies, multiple treatment was used in six studies, and no treatment modality was reported in the remained one. There were two kinds of parameters from pretreatment 18F-FDG PET results extracted in this meta-analysis. One parameter was Tsuv/Lsuv ratio, which was used in fourteen studies. The other parameter was Tsuv value, which was used in ten studies. In terms of study endpoints, OS was provided in eighteen studies and DFS was provided in seven studies. The follow-up period was available in twenty-one studies, of which thirteen had the longest follow-up period more than 60 months.
Meta-analysis for the prognostic value of 18F-FDG PET on OS
In this meta-analysis, OS was analyzed by using both Tsuv/Lsuv ratio and Tsuv value from pretreatment 18F-FDG PET. According to Tsuv/Lsuv ratio, ten studies with 836 patients were included during this analysis. Since heterogeneity was found among these studies (I 2 = 51.4%, P = 0.030), a random-effect model was used to calculate the pooled HR (HR = 2.04; 95% CI 1.50–2.79; P = 0.000) (Fig. 2A). In addition, there were ten studies with 937 patients investigating the prognostic role of Tsuv value on HCC patients. There was heterogeneity among these studies (I 2 = 73.1%, P = 0.000), so a random-effect model was used to calculate the pooled HR (HR = 1.53; 95% CI 1.26–1.87; P = 0.000) (Fig. 2B). These results above suggested that both high Tsuv/Lsuv ratio and high Tsuv value were significantly associated with poor OS, indicating that HCC patients with high Tsuv/Lsuv ratio or high Tsuv value suffered from decreased survival rate.
Meta-analysis for the prognostic value of 18F-FDG PET on DFS
Totally, there were seven studies with 532 patients investigating the prognostic impact of pretreatment 18F-FDG PET on DFS, by parameter of Tsuv/Lsuv ratio. There was heterogeneity among these studies, so a random-effect model was used to calculate the pooled HR (HR = 7.17; 95% CI 3.58–14.36; P = 0.000). The results above suggested high Tsuv/Lsuv ratio were significantly associated with poor DFS, indicating that HCC patients with high Tsuv/Lsuv ratio suffered from high tumor recurrence rate. Besides, we also identified only one study investigating the association between Tsuv value and prognosis of HCC patients, in which the HR was 2.03 (95% CI 1.05–3.92; P = 0.036).
Subgroup analysis
Since heterogeneity was found in the meta-analysis with OS and DFS, we therefore conducted subgroup analysis for each of them. According to the median number, the cutoff values for Tsuv/Lsuv ratio and Tsuv value in OS were 1.83 and 4.9, respectively. Despite cutoff values, both high Tsuv/Lsuv ratio and high Tsuv value were associated with poor OS (Fig. 2A, B), and high Tsuv/Lsuv ratio was also associated with poor DFS in HCC patients (Fig. 3). Meanwhile, we found that high Tsuv/Lsuv ratio was associated with poor OS in patients who underwent TACE (HR = 2.08; 95% CI 1.45–2.99; P = 0.000) and transplantation (HR = 4.47; 95% CI 2.23–8.96; P = 0.000), but this association was not found in patients who underwent resection (HR = 1.71; 95% CI 1.00–2.92; P = 0.052) (Table 2). Besides, high Tsuv value was also significantly associated with poor OS in patients who underwent TACE (HR = 5.24; 95% CI 1.54–17.81; P = 0.008) and resection (HR = 2.75; 95% CI 1.10–6.87; P = 0.001) (Table 3). Moreover, high Tsuv/Lsuv ratio was correlated with poor DFS in patients who underwent transplantation (HR = 8.67; 95% CI 3.73–20.19; P = 0.000) and resection (HR = 3.81; 95% CI 1.17–12.41; P = 0.026) (Table 4). However, other subgroup analysis factors, such as study sample size, analysis method, and follow-up period, did not affect the statistical significance from meta-analysis results (Tables 2, 3, 4).
Generally, subgroup analysis showed that both high Tsuv/Lsuv ratio and high Tsuv value were significantly associated with poorer prognosis in HCC patients, and this association was not altered by subgroup analysis factors except treatments.
Publication bias
In this meta-analysis, both Begg’s and Egger’s tests were used to examine the potential publication bias. Publication bias was found in the meta-analysis with OS by parameters of Tsuv/Lsuv (P = 0.007, 0.003) and Tsuv (P = 0.004, 0.000), and DFS by parameter of Tsuv (P = 0.072, 0.009).
Discussion
HCC is a lethal malignancy, and its incidence is increasing in the United States [38]. Only 30% of HCC patients are diagnosed at localized stage [38], which are suitable for curative resection or radiofrequency (RFA). However, the survival rate after these treatments remains poor due to high tumor recurrence rate [2, 3]. Till now, the prognostic factors for HCC after treatments are alpha-fetoprotein (AFP) level, immunohistochemical makers (P53, Ki67, CD105, etc.), and pathological features including tumor stage and differentiation [39–41]. However, only part of HCC patients have a significant elevation of AFP level, these biomarkers above are not commonly used in our clinical work, and the pathological features are individual rather than universal. Therefore, searching for practical indicators that can predict survival and detect recurrence after treatments is imperative, which will not only guide the life quality of patients but also allow therapies to be more aggressive.
To the best of our knowledge, this is the first meta-analysis investigating the prognostic value of pretreatment 18F-FDG PET on HCC patients. In the present meta-analysis, we included 22 studies with 1721HCC patients and assessed the prognostic value of parameters from 18F-FDG PET on OS and DFS. Meta-analysis results showed that high Tsuv/Lsuv ratio was significantly associated with both poor survival rate (HR = 2.04; 95% CI 1.50–2.79) and early tumor recurrence rate (HR = 1.53; 95% CI 1.26–1.87), and high Tsuv/Lsuv ratio was also correlated with early tumor recurrence rate (HR = 7.17; 95% CI 3.58–14.36; P = 0.000) in HCC patients. These results suggested that both high Tsuv/Lsuv ratio and high Tsuv value can serve as an indicator of poor survival rate, and high Tsuv/Lsuv ratio can serve as an indicator of early tumor recurrence rate in HCC patients. Meanwhile, subgroup analysis showed that the association above was stable despite study sample size, parameter cutoff value, analytic method, and follow-up period changes, but the association above was unsuitable for patients who underwent resection, in which high Tsuv/Lsuv ratio was not significantly associated with poorer OS (HR = 1.71; 95% CI 1.00–2.92; P = 0.052).
However, this meta-analysis does have some potential limitations. The primary concern is publication biases. Some studies did not provide survival results or provided paradoxical results (not included), some articles were unavailable (published in other databases or could not be downloaded), and some studies achieving negative results were not reported, all these may account for the publication biases in our study. The secondary issue is that the number of included studies for each treatment modality is too small when subgroup analyzed by treatments (e.g., two studies about resection in the analysis with OS and one study about resection in the analysis with DFS by parameter of Tsuv/Lsuv ratio, one study in the analysis with OS by parameter of Tsuv, and some studies did not provide explicit modalities). This issue may make the subgroup analysis results by treatments segmentary. As we all know, publication bias and included studies’ number are vey important factors, which may impact the final meta-analysis results. Therefore, the results from our meta-analysis may be estimation, and more well-designed and prospective studies with large population are required to investigate the prognostic value of pretreatment 18F-FDG PET on HCC patients, especially those with explicit treatment modalities.
In conclusion, we showed that both high Tsuv/Lsuv ratio and high Tsuv value from pretreatment 18F-FDG PET were significantly associated with poor survival rate, and high Tsuv/Lsuv ratio was significantly associated with early tumor recurrence rate in HCC patients. Therefore, pretreatment 18F-FDG PET is a useful tool in predicting the prognosis of HCC patients. As our study has some limitations, more prospectively well-designed and large-scale studies are required to investigate the prognostic value of pretreatment 18F-FDG PET on HCC patients, especially those with explicit treatment modalities.
References
Torre LA, Bray F, Siegel RL, et al. (2015) Global cancer statistics, 2012. CA Cancer J Clin 65(2):87–108
Altekruse SF, McGlynn KA, Dickie LA, et al. (2012) Hepatocellular carcinoma confirmation, treatment, and survival in surveillance, epidemiology, and end results registries, 1992–2008. Hepatology 55(2):476–482
Maluccio M, Covey A (2012) Recent progress in understanding, diagnosing, and treating hepatocellular carcinoma. CA Cancer J Clin 62(6):394–399
Donswijk ML, Hess S, Mulders T, et al. (2014) [18F]Fluorodeoxyglucose PET/computed tomography in gastrointestinal malignancies. PET Clin 9(4):421–441
Gauthé M, Richard-Molard M, Cacheux W, et al. (2015) Role of fluorine 18 fluorodeoxyglucose positron emission tomography/computed tomography in gastrointestinal cancers. Dig Liver Dis 47(6):443–454
Wang Z, Chen JQ, Liu JL, et al. (2013) FDG-PET in diagnosis, staging and prognosis of pancreatic carcinoma: a meta-analysis. World J Gastroenterol 19(29):4808–4817
Maffione AM, Marzola MC, Capirci C, et al. (2015) Value of (18)F-FDG PET for predicting response to neoadjuvant therapy in rectal cancer: systematic review and meta-analysis. AJR Am J Roentgenol 204(6):1261–1268
Li C, Lan X, Yuan H, et al. (2014) 18F-FDG PET predicts pathological response to preoperative chemoradiotherapy in patients with primary rectal cancer: a meta-analysis. Ann Nucl Med 28(5):436–446
Jones M, Hruby G, Solomon M, et al. (2015) Diagnostic Value of <sup> 18 </sup> F-FDG PET/CT in detecting local recurrent colorectal cancer: a pooled analysis of 26 individual studies. Cell Biochem Biophys. [Epub ahead of print]
Lin CY, Chen JH, Liang JA, et al. (2011) 18F-FDG PET or PET/CT for detecting extrahepatic metastases or recurrent hepatocellular carcinoma: a systematic review and meta-analysis. Eur J Radiol 81(9):2417–2422
Parmar MK, Torri V, Stewart L (1988) Extracting summary statistics to perform meta-analyses of the published literature for survival endpoints. Stat Med 17(24):2815–2834
Higgins JP, Thompson SG (2002) Quantifying heterogeneity in a meta-analysis. Stat Med 21(11):1539–1558
Begg CB, Mazumdar M (1994) Operating characteristics of a rank correlation test for publication bias. Biometrics 50(4):1088–1101
Egger M, Davey Smith G, Schneider M, et al. (1997) Bias in meta-analysis detected by a simple, graphical test. Br Med J 315(7109):629–634
Altman DG (2001) Systematic reviews of evaluations of prognostic variables. BMJ 323(7306):224–228
Song HJ, Cheng JY, Hu SL, et al. (2015) Value of 18F-FDG PET/CT in detecting viable tumour and predicting prognosis of hepatocellular carcinoma after TACE. Clin Radiol 70(2):128–137
Kim YK, Kim SH, Lee SD, et al. (2015) Pretransplant serum levels of C-reactive protein predict prognoses in patients undergoing liver transplantation for hepatocellular carcinoma. Transplant Proc 47(3):686–693
Kim MJ, Kim YS, Cho YH, et al. (2015) Use of (18)F-FDG PET to predict tumor progression and survival in patients with intermediate hepatocellular carcinoma treated by transarterial chemoembolization. Korean J Intern Med 30(3):308–315
Chang ZF, Song P, Wang MQ, et al. (2014) Value of 18F-FDG PET in preoperative TACE of hepatocellular carcinoma. Chin J Oncol 36(5):377–380
Xu ZQ, Zhang XS, Zhang LQ, et al. (2014) 18F-FDG PET/CT in predicting tumor recurrence for hepatocellular carcinoma after liver transplantation. Chin J Organ Transplant 35(6):341–344
Han JH, Kim DG, Na GH, et al. (2014) Evaluation of prognostic factors on recurrence after curative resections for hepatocellular carcinoma. World J Gastroenterol 20(45):17132–17140
Simoneau E, Hassanain M, Madkhali A, et al. (2014) (18)F-Fluorodeoxyglucose positron-emission tomography could have a prognostic role in patients with advanced hepatocellular carcinoma. Curr Oncol 21(4):e551–e556
Kawamura E, Shiomi S, Kotani K, et al. (2014) Positioning of 18F-fluorodeoxyglucose-positron emission tomography imaging in the management algorithm of hepatocellular carcinoma. J Gastroenterol Hepatol 29(9):1722–1727
Ahn SG, Jeon TJ, Lee SD, et al. (2013) A survival benefit of major hepatectomy for hepatocellular carcinoma identified by preoperative [18F] fluorodeoxyglucose positron emission tomography in patients with well-preserved hepatic function. Eur J Surg Oncol 39(9):964–973
Detry O, Govaerts L, Deroover A, et al. (2015) Prognostic value of (18)F-FDG PET/CT in liver transplantation for hepatocarcinoma. World J Gastroenterol 21(10):3049–3054
Kim JW, Seong J, Yun M, et al. (2012) Usefulness of positron emission tomography with fluorine-18-fluorodeoxyglucose in predicting treatment response in unresectable hepatocellular carcinoma patients treated with external beam radiotherapy. Int J Radiat Oncol Biol Phys 82(3):1172–1178
Song MJ, Bae SH, IeR Yoo, et al. (2012) Predictive value of 18F-fluorodeoxyglucose PET/CT for transarterial chemolipiodolization of hepatocellular carcinoma. World J Gastroenterol 18(25):3215–3222
Kitamura K, Hatano E, Higashi T, et al. (2012) Preoperative FDG-PET predicts recurrence patterns in hepatocellular carcinoma. Ann Surg Oncol 19(1):156–162
Kornberg A, Küpper B, Tannapfel A, et al. (2012) Patients with non-[18 F]fludeoxyglucose-avid advanced hepatocellular carcinoma on clinical staging may achieve long-term recurrence-free survival after liver transplantation. Liver Transpl 18(1):53–61
Shin DY, Han SW, Oh DY, et al. (2011) Prognostic implication of (18)F FDG-PET in patients with extrahepatic metastatic hepatocellular carcinoma undergoing systemic treatment, a retrospective cohort study. Cancer Chemother Pharmacol 68(1):165–175
Kim BK, Kang WJ, Kim JK, et al. (2011) 18F-fluorodeoxyglucose uptake on positron emission tomography as a prognostic predictor in locally advanced hepatocellular carcinoma. Cancer 117(20):4779–4787
Lee JW, Paeng JC, Kang KW, et al. (2009) Prediction of tumor recurrence by 18F-FDG PET in liver transplantation for hepatocellular carcinoma. J Nucl Med 50(5):682–687
Paudyal B, Paudyal P, Oriuchi N, et al. (2008) Clinical implication of glucose transport and metabolism evaluated by 18F-FDG PET in hepatocellular carcinoma. Int J Oncol 33(5):1047–1054
Yang SH, Suh KS, Lee HW, et al. (2006) The role of (18)F-FDG-PET imaging for the selection of liver transplantation candidates among hepatocellular carcinoma patients. Liver Transpl 12(11):1655–1660
Hatano E, Ikai I, Higashi T, et al. (2006) Preoperative positron emission tomography with fluorine-18-fluorodeoxyglucose is predictive of prognosis in patients with hepatocellular carcinoma after resection. World J Surg 30(9):1736–1741
Kong YH, Han CJ, Lee SD, et al. (2004) Positron emission tomography with fluorine-18-fluorodeoxyglucose is useful for predicting the prognosis of patients with hepatocellular carcinoma. Korean J Hepatol 10(4):279–287
Shiomi S, Nishiguchi S, Ishizu H, et al. (2001) Usefulness of positron emission tomography with fluorine-18-fluorodeoxyglucose for predicting outcome in patients with hepatocellular carcinoma. Am J Gastroenterol 96(6):1877–1880
Siegel RL, Miller KD, Jemal A (2015) Cancer statistics, 2015. CA Cancer J Clin 65(1):5–29
Ma WJ, Wang HY, Teng LS (2013) Correlation analysis of preoperative serum alpha-fetoprotein (AFP) level and prognosis of hepatocellular carcinoma (HCC) after hepatectomy. World J Surg Oncol 11:212. doi:10.1186/1477-7819-11-212
Niu ZS, Niu XJ, Wang M (2015) Management of hepatocellular carcinoma: predictive value of immunohistochemical markers for postoperative survival. World J Hepatol 7(1):7–27
Zhou L, Rui JA, Wang SB, et al. (2014) Early recurrence in large hepatocellular carcinoma after curative hepatic resection: prognostic significance and risk factors. Hepatogastroenterology 61(135):2035–2041
Acknowledgments
This work was supported by research funding from Jilin Provincial Science & Technology Department (No. 20130413021GH).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of Interest
None.
Additional information
Da-wei Sun and Lin An have contributed equally to this work.
Rights and permissions
About this article
Cite this article
Sun, DW., An, L., Wei, F. et al. Prognostic significance of parameters from pretreatment 18F-FDG PET in hepatocellular carcinoma: a meta-analysis. Abdom Radiol 41, 33–41 (2016). https://doi.org/10.1007/s00261-015-0603-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00261-015-0603-9