Abstract
Purpose
For digestive tract cancers, the bilirubin threshold for administration of systemic chemotherapy can be 5 or 2 mg/dL (85.5 or 34.2 μmol/L) depending upon the regimen. We examined the ability of percutaneous biliary drainage (PBD) in patients with malignant biliary obstruction to achieve these clinically relevant endpoints.
Methods
106 consecutive patients with malignant biliary obstruction and a baseline serum bilirubin >2 mg/dL underwent PBD. Time to achieve a bilirubin of 5 mg/dL (85.5 μmol/L), 2 mg/dL (34.2 μmol/L), and survival was estimated by Kaplan–Meier analysis. Potential technical and clinical prognostic factors were subjected to univariate and multivariate analysis. Categorical variables were analyzed by the log rank test. Hazard ratios were calculated for continuous variables.
Results
Median survival was 100 days (range 1–3771 days). Among 88 patients with a pre-drainage bilirubin >5 mg/dL, 62% achieved a serum bilirubin ≤5 mg/dL within 30 days and 84% within 60 days, median 21 days. Among 106 patients with a pre-drainage bilirubin >2 mg/dL, 37% achieved a serum bilirubin ≤2 mg/dL by 30 days and 70% within 60 days, median 43 days. None of the technical or clinical factors evaluated, including pre-drainage bilirubin, were significant predictors of time to achieve a bilirubin ≤2 mg/dL (p = 0.51). Size and type of biliary device were the only technical variables found to affect time to bilirubin of 5 mg/dL (p = 0.016).
Conclusion
PBD of malignant obstruction achieves clinically relevant reduction in serum bilirubin in the majority of patients within 1–2 months, irrespective of the pre-drainage serum bilirubin, sufficient to allow administration of systemic chemotherapy. However, the decision to undergo this procedure for this indication alone must be considered in the context of patients’ prognosis and treatment goals.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Many chemotherapeutic agents used for gastrointestinal malignancies are contraindicated in patients with elevated serum bilirubin levels because diminished hepatic clearance may lead to increased toxicity [1–5]. For this reason, patients with malignant biliary obstruction may undergo biliary drainage to lower serum bilirubin to allow initiation of chemotherapy.
A previous study reported that only 31% of patients undergoing percutaneous biliary drainage (PBD) to decrease serum bilirubin for administration of chemotherapy reached a level of 1 mg/dL (17.1 μmol/L) by 100 days [6]. However, chemotherapeutic agents commonly used to treat GI cancers and other malignancies causing biliary obstruction do not require normalization of serum bilirubin levels. Serum bilirubin levels of 2 or 5 mg/dL (34.2 or 85.5 μmol/L) are often sufficient, depending on the regimen [3]. This study evaluates the ability of PBD to achieve these clinically relevant endpoints and identifies patient characteristics and technical variables that are predictive of success.
Methods
This retrospective study was approved by the Institutional Review Board and requirement for informed consent was waived. We searched our Quality Assurance Database (HI-IQ, Conexys, Lincoln, RI) and identified all patients who underwent percutaneous biliary drainage at our institution between July 2004 and May 2013. 106 consecutive patients drained for a malignant biliary obstruction, defined by the presence of one or multiple biliary strictures or occlusions with an elevated serum bilirubin, a diagnosis of cancer, and no other documented reason for the obstruction.
The clinical variables examined included cancer diagnosis; presence of liver metastases (none, focal, diffuse); location of the stricture or occlusion; prior biliary surgery; pre-drainage total serum bilirubin, creatinine, international normalized ratio (INR), and platelet count; presence of cholangitis or pruritus; whether the patient received chemotherapy; and survival. Demographic information obtained included sex, age, and race.
Pre-drainage bilirubin levels, creatinine, INR, and platelet count were recorded on the day of the procedure or no more than 3 days prior to the drainage. The location of the stricture was recorded as documented on the exam report or by review of the procedural cholangiogram. The technical variables examined included fraction of the liver drained by quartiles, size of drain, and type of drain. The percentage of liver drained was estimated by reviewing the procedural cholangiograms in combination with concurrent cross-sectional imaging (CT or MRI scan). The number of lobes drained was divided by the total number of lobes present, in order to account for patients with partial hepatectomy. All images were reviewed by a senior attending with >20 years experience. Selection of the initial size and type of drain was at the discretion of the interventional radiologist based on the patient’s anatomy and features of the obstruction. Patients in whom the biliary obstruction could be traversed who had suitable anatomy underwent metal stent placement, either primarily or after initial tube decompression. If it was not possible for the guidewire to cross the obstruction, an external drain was placed. Drains were changed for preventative maintenance every 3 months, with replacement or upsizing in cases of pericatheter leakage or drain dislodgment.
The time to achieve a total serum bilirubin of 2 and 5 mg/dL were the primary study endpoints because these are the levels required by most chemotherapy protocols before initiation of chemotherapy for digestive tract cancers. Postdrainage serum bilirubin levels were recorded at variable intervals until achieving ≤2 mg/dL, patient death, or loss to follow-up.
The time to bilirubin level endpoints was counted from the date of successful completion of biliary drainage. For example, if a drain needed to be upsized a few days after initial placement, or an additional drain was placed due to inadequate drainage after the first procedure, time to normalization was counted from the date of the second drain placement. Survival was calculated from the date of the initial biliary drainage.
Statistical analysis
Time to achieve a bilirubin of 5 mg/dL, 2 mg/dL and survival were estimated by the method of Kaplan and Meier (Medcalc v12, MedCalc Software, Ostend, Belgium).
Time to achieve a bilirubin of 5 mg/dL, 2 mg/dL and overall survival were compared for categorically defined groups using the log rank test. Associations with continuous laboratory variables were evaluated by Cox regression analysis. Continuous variables were also categorized by quartiles and compared by the log rank test. All analyses were performed in SPSS v21 (SPSS, Inc, Chicago, IL). Significance was defined as p < 0.05.
Results
The median follow-up time for all patients was 90 days. For 86 patients, surveillance of bilirubin levels continued until death or endpoints were reached. For 18 patients who were still alive at the time of data collection, surveillance ended on the expiration date of the IRB waiver. Two patients were lost to follow-up.
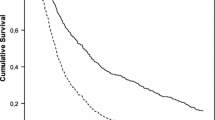
The median age at time of percutaneous biliary drainage was 64 years (range 21–99 years). Median survival for the study population was 100 days (range 1–3771 days), with 75% alive at 30 days, 60% at 60 days, and 52% at 90 days. Survival data were not available for two patients who were lost to follow-up Fig. 1.
37 patients had a diagnosis of pancreatic cancer, 24 patients had cholangiocarcinoma, six patients had gastric cancer, four patients had gall bladder cancer, and 35 patients had another cancer diagnosis, including duodenal, colon, cervical, and lung cancer, among others. Demographic and clinical data are displayed in Table 1.
Pre-drainage serum bilirubin levels ranged from 2.0 to 37.4 mg/dL (mean ± SD, 12.3 ± 8.3 mg/dL) [34.2–639.5 μmol/L (mean ± SD, 210.3 ± 141.9 μmol/L)]. For all 106 patients with a pre-drainage bilirubin level >2 mg/dL, the median time to achieve a bilirubin level of 2 mg/dL was 43 days, with 37% achieving this level by 30 days, 70% by 60 days, and 88% by 90 days, Fig. 2. 88 of these patients had a pre-drainage bilirubin level >5 mg/dL. The median time to achieve a bilirubin level of 5 mg/dL was 21 days, with 62% achieving this level by 30 days, 84% by 60 days, and 92% by 90 days, Fig. 3.
Results of univariate analysis to assess the association of bilirubin endpoints with clinical and technical variables are presented in Tables 2 and 3. No clinical variables (cancer type, liver metastases, prior hepatobiliary surgery, level of obstruction, or obstructive symptoms) were associated with time to achieve a bilirubin of 2 or 5 mg/dL. Size and type of biliary device were the only technical variables found to affect time to bilirubin of 5 mg/dL (p = 0.016). Patients requiring multiple percutaneous drains had a median time to reach a bilirubin of 5 mg/dL of 70 days; those with a single 8F or 10F drain had a median time of 24 days; those with a single 12F or 14F drain had a median time of 15 days; and patients with a single metal stent had a median time of 7 days. No technical variables (drain or stent type/size, drain or stent location, percent liver drained) were associated with time to reach a bilirubin of 2 mg/dL.
Pre-drainage bilirubin categorized by quartiles was a significant predictor of time to achieve a bilirubin ≤5 mg/dL (p < 0.001). Patients with pre-drainage bilirubin levels in the lowest quartile, between 5.1 and 8.6 mg/dL, achieved a bilirubin of 5 mg/dL in a median time of 3 days; patients with a pre-drainage bilirubin from 8.7 to 13.7 mg/dL took an average of 7 days; patients with levels of 13.7 to 19.7 mg/dL took 32 days; and patients with pre-drainage levels from 19.8 to 37.4 mg/dL had a median time to reach 5 mg/dL of 40 days. Time to achieve a bilirubin of 2 mg/dL increased with pre-drainage quartiles but the trend did not reach statistical significance (p = 0.51) Table 4.
The high rates of success reaching target bilirubin must be considered in the context of overall survival. Patients in the higher quartiles for baseline bilirubin had shorter survival, although the difference did not reach statistical significance by the log rank test, Table 5. Using Cox regression analysis of pre-drainage bilirubin as a continuous variable, there was a small but statistically significant association with survival, with a hazard ratio of 1.04 [95% CI 1.01–1.07], p = 0.009. This is equivalent to a 4% increased risk of death for every unit increase in the baseline bilirubin.
Table 6 displays the results of Cox regression analysis of time to bilirubin endpoints for the continuous variables of pre-drainage bilirubin, creatinine, INR, and platelet count. Pre-drainage bilirubin (HR 0.91, p < 0.001), INR (HR 0.23, p = 0.036), and platelets (HR 1.003, p = 0.012) were significant predictors of time to achieve bilirubin <5 mg/dL. Pre-drainage creatinine was not associated with time to achieve bilirubin of 5 mg/dL (p = 0.288). Pre-drainage bilirubin (p = 0.083), creatinine (p = 0.675), INR (p = 0.809), and platelets (p = 0.085) were not significant predictors of time to achieve a bilirubin <2 mg/dL.
Major complications occurred in 3.5% of patients with a single mortality. The most common complications were sepsis (1.9%) and bleeding (1.1%).
Discussion
Biliary obstruction is a common complication of GI malignancies. Patients with biliary obstruction may experience jaundice and pruritus, as well as an increased risk of cholangitis, malabsorption, and progressive hepatocellular and renal dysfunction. While placement of an endoscopic biliary stent is often preferred due to its lower acute major complication rate relative to PBD [7–10], patient anatomy or high bile duct obstruction may preclude endoscopic drainage. In these cases, percutaneous biliary drainage is performed [6].
Biliary drainage may be requested solely to lower serum bilirubin to allow administration of chemotherapy. Elevated serum bilirubin is a contraindication to certain chemotherapeutic agents because diminished hepatic clearance may alter drug metabolism and increase risk of toxicity [1–5]. For example, 5-fluorouracil, which is commonly used to treat bowel, stomach, and pancreatic cancers, should not be administered to patients with serum bilirubin levels greater than 5 mg/dL [3]. Irinotecan is contraindicated in patients with serum bilirubin levels greater than 2 mg/dL [6]. Other agents requiring dose modifications include gemcitabine and taxanes. For example, the dose of paclitaxel must be reduced by 75% in patients with bilirubin levels greater than or equal to 3 mg/dL [3]. Importantly, most clinical trials require a normal serum bilirubin for enrollment.
Endoscopic stenting is often the initial approach to manage biliary obstruction. A series from MD Anderson Cancer Center, which included patients with both plastic and metal endoscopic stents, reported that 93/156 (60%) successfully stented patients achieved a serum bilirubin <2 mg/dL, with 80% of responding patients reaching this endpoint within 2–6 weeks [8]. In contrast, a recent study of patients at Memorial Sloan-Kettering Cancer Center undergoing PBD to decrease serum bilirubin for administration of chemotherapy found that patients had a probability of reaching a level of 1 mg/dL by 100 days of only 31% [6]. The endpoint for this study was chosen because some chemotherapeutic agents require a bilirubin level of 1 mg/dL for administration at full dose. Since most commonly used agents can be administered at bilirubin levels greater than 1 mg/dL, this is not a practical endpoint in the general oncologic population.
The goal of this study was to evaluate the ability of percutaneous biliary drainage to lower serum bilirubin in patients with malignant biliary obstruction. Serum bilirubin levels of 2 and 5 mg/dL were chosen as the endpoints because these are the levels above which commonly used chemotherapeutic agents are contraindicated. This study revealed that the median times to achieve bilirubin levels of 2 and 5 mg/dL (43 days and 21 days, respectively) were considerably shorter than the median survival of the study population (100 days). This result suggests that most patients undergoing this procedure will reach bilirubin levels adequate to permit systemic chemotherapy.
Pre-drainage bilirubin level was a predictor of time required to achieve a bilirubin level of 5 mg/dL. This result was consistent with the findings of the Memorial study which showed that the pre-drainage serum bilirubin level was associated with the probability of achieving a serum bilirubin level of 1 mg/dL within 100 days [6]. However, in our study, even those patients with pre-drainage bilirubin levels in the highest quartile (19.8–37.4 mg/dL) had a median time to bilirubin of 5 mg/dL of only 40 days. This result indicates that even patients with the highest pre-drainage levels can achieve clinically relevant bilirubin reduction.
In contrast, pre-drainage bilirubin was not a statistically significant predictor of time to achieve a bilirubin of 2 mg/dL. This result likely differs from that for the 5 mg/dL endpoint because patients with modest bilirubin elevations (lowest two quartiles) got to 5 mg/dL in a few days, while the time needed to get down to 2 mg/dL was longer for all quartiles. While there is a clear trend of longer time to reach 2 mg/dL as baseline bilirubin increases, the magnitude of difference among quartiles did not reach statistical significance by the log rank test.
Pre-drainage INR and platelets were predictive of the time to achieve a bilirubin level of 5 mg/dL but not 2 mg/dL. Because these values are markers of liver synthetic function and portal hypertension, it would be reasonable to conclude that patients with worse liver function require more time to achieve bilirubin reduction. The finding that INR is predictive of time to achieve bilirubin reduction is consistent with previous studies [6, 8].
It is important to recognize important differences between this cohort and the Memorial series which may have contributed to the differences in outcomes [6]. Sixty-five percent of patients in our cohort had common duct obstruction, making drainage of the entire liver possible with a single catheter or stent, versus only 48.5% in the Memorial series. Seventy-eight percent in our series had >75% of the liver drained, versus only 48% of the Memorial patients. The higher prevalence of hilar and intrahepatic obstruction likely contributed to the inability to drain the majority of the liver in the majority of patients in the Memorial series, which may account for the lesser reported efficacy in correcting hyperbilirubinemia.
The MD Anderson endoscopic stent series found that pre-drainage bilirubin level was predictive of rate of bilirubin reduction to 2 mg/dL [8]. Eighty percent of patients with a pre-drainage bilirubin <10 mg/dL achieved a bilirubin of 2 mg/dL by 2.7 weeks, while for those with an initial bilirubin >10 mg/dL it took 5.6 weeks for 80% to reach that endpoint. This study also found that patients with multiple biliary strictures and those with strictures proximal to the CBD treated endoscopically were less likely to achieve the endpoint than those with distal strictures. Because neither pre-drainage bilirubin level nor stricture location were significant predictors of success among our patients undergoing PBD, it may be reasonable to consider PBD over ERCP in patients with obstructions proximal to the CBD or high pre-drainage bilirubin levels, even if ERCP can technically be performed. Studies comparing PBD to endoscopic stenting in patients with Klatskin tumors also suggest higher technical and clinical success rates for PBD in a population with proximal obstructions [11, 12].
In contrast to the Memorial series, this study did not find that percent of liver drained was associated with time to bilirubin endpoints, which was unexpected. However, given that the majority of patients undergoing PBD at our institution have 100% liver drainage, any difference in outcomes based on drainage level may not be clinically apparent.
Our study found that metallic stents resulted in quicker bilirubin reduction to 5 mg/dL than drains. Because stent or drain selection was influenced by characteristics of the patient’s obstruction, and the radiologist’s selection of a stent reflected the fact that an obstruction was distal and could be easily traversed, we do not feel these results necessarily reflect improved drainage with stents than with drains. However, it is important to note that metal stents have longer patency than internal/external biliary drainage catheters [13], and a greater number of catheter exchanges are associated with increased probability of bile spillage and cancer dissemination [14]. Therefore, we generally favor stent placement over drain insertion in patients who are appropriate candidates.
Although this study demonstrates that PBD can successfully lower bilirubin in patients with malignant biliary obstruction, it is important to note that for only 35% of patients was administration of chemotherapy the indication for PBD. Most patients underwent the procedure for indications such as pruritus, nausea-associated jaundice, or suspected cholangitis. Among these patients for whom chemotherapy was not the primary indication for PBD, 38% were eventually treated with chemotherapy. In those patients for whom the indication was chemotherapy administration, 27% ultimately received chemotherapy. The decision to undergo chemotherapy for incurable malignancies is clearly a personalized one and depends upon many factors including performance status, age, co-morbidities, and cultural influences. It would be interesting to know why patients who undergo PBD do not ultimately receive chemotherapy despite reaching an acceptable bilirubin level. Such a study would be difficult because most systemic therapy is administered in the outpatient setting in the patient’s home community. Inpatient medical records from the time of biliary drainage do not indicate future chemotherapeutic agents or any changes made to a treatment plan based on PBD outcomes.
Although PBD is successful in most patients, it is important to note that the procedure has a significant complication rate. The SIR Clinical Practice Guidelines suggest a threshold for all major complications (sepsis, hemorrhage, inflammatory/infection, pleural complication, and death) of 10% for all patients undergoing PBD [15]. A previous study found that PBD in patients with malignant obstruction had a 3.4% rate of major complications, very similar to the 3.5% rate observed in our study [6]. This value is well within the range of acceptable major complication rates. Of course, each individual patient must be evaluated for risk factors (such as coagulopathy) that could increase the complication rate. Patients with deranged clotting would not only be at higher risk for complications as a result of PBD, but also less likely to achieve adequate bilirubin reduction and less suitable candidates for chemotherapy should they achieve the desired serum bilirubin level. The risk:benefit ratio should be considered in the context of expected survival. While patients in the highest quartile may achieve a low enough bilirubin to receive chemotherapy, the majority succumb to their disease before this occurs.
Our study found a statistically significant association between pre-drainage bilirubin level and survival. This result may simply reflect the fact that patients with higher pre-drainage bilirubin levels have more advanced cancer and therefore have shorter life expectancies. However, another explanation is that liver impairment caused by the obstruction (and measured by serum bilirubin) hastens death. It is likely that both of these explanations are at play. The latter underscores the importance of treating obstructive biliary disease as soon as possible to prevent further liver damage.
Limitations of this study include the retrospective design and the limited sample size relative to the heterogeneity of the study population, reflecting multiple cancer types, levels of obstruction, and drainage devices. Nonetheless, the results overall demonstrate that PBD of malignant obstruction achieves clinically relevant reduction in serum bilirubin in the majority of patients within 1–2 months, irrespective of the pre-drainage serum bilirubin. PBD can be employed effectively for reduction of bilirubin to allow administration of systemic chemotherapy.
References
King PD (2001) Hepatotoxicity of chemotherapy. Oncologist 6:162–176
Floyd J, Mirza I, Sachs B, Perry MC (2006) Hepatotoxicity of chemotherapy. Semin Oncol 33:50–67
Eklund JW, Trifilio S, Mulcahy MF (2005) Chemotherapy dosing in the setting of liver dysfunction. Oncology (Williston Park) 19:1057–1063
Donelli MG, Zucchetti M, Munzone E, et al. (1998) Pharmacokinetics of anticancer agents in patients with impaired liver function. Eur J Cancer 34:33–46
Venook AP, Egorin MJ, Rosner GL, et al. (2000) Phase 1 and pharmacokinetic trial of gemcitabine in patients with hepatic and renal dysfunction: Cancer and Leukemia Group B 9565. J Clin Oncol 18:2780–2787
Thornton RH, Ulrich R, Hsu M, et al. (2012) Outcomes of patients undergoing percutaneous biliary drainage to reduce bilirubin for administration of chemotherapy. J Vasc Interv Radiol 23:89–95
Adler DG, Baron TH, Davila RE, et al. (2005) ASGE guideline: the role of ERCP in diseases of the biliary tract and the pancreas. Gastrointest Endosc 62:1–8
Weston BR, Ross WA, Wolff RA, et al. (2008) Rate of bilirubin regression after stenting in malignant biliary obstruction for the initiation of chemotherapy. Cancer 112(11):2417–2423
Speer AR, Russell CG, Hatfield AW, et al. (1987) Randomised trial of endoscopic versus percutaneous stent insertion in malignant obstructive jaundice. Lancet 330:57–62
Pinol V, Castellis A, Bordas JM, et al. (2002) Percutaneous self-expanding metal stents versus endoscopic polyethylene endoprostheses for treating malignant biliary obstruction: randomized clinical trial. Radiology 225:27–34
Walter T, Ho CS, Horgan AM, et al. (2013) Endoscopic or percutaneous biliary drainage for Klatskin tumors? J Vasc Interv Radiol 24:113–121
Guidi MA, Curvale C, Viscardi J, et al. (2015) Hilar bile duct tumors: endoscopic or percutaneous drainage? A prospective analysis. Rev Esp Enferm Dig 107:488–494
Mahgerefteh S, Hubert A, Klimov A, Bloom AI (2015) Clinical impact of percutaneous transhepatic insertion of metal biliary endoprostheses for palliation of jaundice and facilitation of chemotherapy. Am J Clin Oncol 38:489–494
Kwang MK, Park JW, Lee JK, et al. (2015) A comparison of preoperative biliary drainage methods for perihilar cholangiocarcinoma: endoscopic versus percutaneous transhepatic biliary drainage. Gut Liver 9(6):791
Saad W, Wallace MJ, Wojak JC, Kundu S, Cardella JF (2010) Quality improvement guidelines for percutaneous transhepatic cholangiography, biliary drainage, and percutaneous cholecystostomy. J Vasc Interv Radiol 21:789–795
Acknowledgments
Supported in part (RM) by Abramson Cancer Center Support Grant (P30-CA016520).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interests
All authors declare no conflicts of interest related to the content of this work.
Rights and permissions
About this article
Cite this article
Levy, J.L., Sudheendra, D., Dagli, M. et al. Percutaneous biliary drainage effectively lowers serum bilirubin to permit chemotherapy treatment. Abdom Radiol 41, 317–323 (2016). https://doi.org/10.1007/s00261-015-0580-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00261-015-0580-z