Abstract
Sarcoidosis is mainly a disease of the respiratory system; however, several other organ systems may be affected in the course of the disease. Liver is one of the most frequently affected organs in the setting of sarcoidosis after lungs and lymph nodes. Microscopic hepatic involvement is common in these patients but is mostly clinically silent. However, in a significant portion of these patients, macroscopic findings can be detected in the course of the disease, and these findings may easily be confused with other benign and malignant conditions of the liver. The purposes of this article are to briefly summarize the clinical findings and the underlying pathophysiology of sarcoidosis and detailed presentation of the radiologic findings of hepatic involvement in this disease. We subgrouped the imaging findings based on the location and the radiologic appearance of the hepatic involvement. We tried to provide images that would enable the readers to link the imaging findings with the underlying pathology and clinical symptoms.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Sarcoidosis is a multisystemic granulomatous disease characterized typically by the development and accumulation of non-caseating granulomas [1–4]. Sarcoidosis was first described by a Norwegian dermatologist, Boeck, in 1899, as nodules observed in the skin characterized by sharply defined ‘epitheloid cells’ with large pale nuclei and also a few ‘giant cells’ [3, 5]. In his original description [5], Boeck likened the nodules to sarcoma, and therefore, he coined the term ‘multiple benign sarcoid of the skin’ to this newly diagnosed entity. The prevalence of systemic sarcoidosis is highest among the northern European countries and is around 5–40 cases per 100,000 people [6]. The adjusted annual incidence among African Americans is about three times higher than white Americans (35.5 cases per 100,000, as compared with 10.9 per 100,000) [7]. The disease can occur in both men and women, with 70% of the patients aged 25–45 years. The exact underlying cause of sarcoidosis is still not very well understood. Genetic susceptibility and environmental factors are proposed as the underlying causes of sarcoidosis [8–11]. With the environmental risk factors reported in the literature, it might be possible that the development of sarcoidosis is secondary to the exaggerated immune responses to several environmental agents such as insecticides, agricultural employment, bioaerosol exposure, inorganic dusts, molds, and solvents or oils [3, 8, 10].
Clinical features, diagnosis, and prognosis
As stated above, sarcoidosis is a multisystemic disease, and virtually every organ system can be involved in the course of the disease. The lungs are the most commonly affected organ and their involvement may be detected in up to 90% of the patients [2]. The severity of lung involvement is highly variable in the patients, ranging from minimally symptomatic disease to life-threatening lung fibrosis with pulmonary hypertension [12]. In addition to pulmonary parenchymal involvement, bilaterally enlarged hilar lymph nodes are very common and, also very typical, for pulmonary sarcoidosis. In addition to the lungs, eyes, heart, skin, liver, and central nervous system may all be involved separately or concomitantly in the course of the disease. The diagnosis of sarcoidosis is established on the basis of clinical symptoms supported by the histological detection of non-caseating granulomas in one or more organs.
The clinical course of sarcoidosis is highly variable. In 50% of the cases, the disease resolves spontaneously in 2 years and even more so after 5 years [8]. Overall two-thirds of the patients with sarcoidosis generally undergo clinical remission within a decade after the diagnosis with few or no clinical sequela. Up to one-third of the patients have unrelenting sarcoidosis which may end up in significant organ dysfunction. Recurrence after more than 1 year is uncommon but may be observed in less than 5% of the patients. The recurrence of the disease may be detected in virtually any organ system. The overall death rate due to sarcoidosis is less than 5%, and the most common cause is unrelenting pulmonary fibrosis culminating in severe respiratory failure, cardiac dysfunction, or neurologic involvement [4].
Liver involvement in sarcoidosis
Liver involvement in sarcoidosis is highly variable in terms of clinical presentation. The clinical presentation may range from asymptomatic to full-blown portal hypertension and liver failure. Histopathologically, granulomatous liver involvement was detected in 40%–70% of the patients [13]. However, there is not much data based on controlled trials on the evaluation of liver involvement in sarcoidosis [14]. Hepatic lesions can be detected in only 5% of sarcoidosis patients on CT [15]. The great majority of the afflicted patients are clinically asymptomatic. In symptomatic patients, abdominal pain, fever, and weight loss are among the common symptoms, but the severity of the symptoms may amount to pruritus, jaundice, and chronic cholestasis in some patients. Severe liver failure, cirrhosis, Budd–Chiari syndrome, and portal hypertension are rare in sarcoidotic liver involvement [14]. Portal hypertension was proposed to be secondary to obstruction of portal flow in the presence of portal area with associating hyalinization and fibrosis of the portal triad ending up with presinusoidal block [16].
Imaging
Liver imaging is generally unremarkable in most of the sarcoidosis patients, and imaging is not critical, except for extraordinary circumstances, to the correct clinical diagnosis. However, liver involvement, as noted above, can have significant clinical consequences for the patient, and early detection and characterization of the liver findings might be significant for the affected patients. Ultrasonography is the first imaging tool in assessment of liver sarcoidosis. Heterogeneous echogenicity and coarse echo pattern may appear on US in the presence of diffuse parenchymal involvement. Focal liver lesions and dilatation of intrahepatic and/or extrahepatic biliary ducts may also be detected on US. CT and MRI are useful to depict imaging features such as subcapsular fibrosis and wedge-shaped atrophic areas in diffuse involvement [4, 17, 18]. MRI may be helpful to differentiate liver sarcoids from other nonneoplastic and neoplastic focal liver lesions. Biliary involvement in liver sarcoidosis may appear with biliary duct dilatation on CT while MRI may be more helpful by revealing biliary duct wall thickening resulting from fibrosis [4, 18]. In order to better categorize the imaging findings, we decided to break down the discussion to several subgroups including diffuse and focal liver involvement and biliary-hilar findings.
Diffuse involvement of the liver
As briefly mentioned above, despite the relatively high microscopical involvement of the liver on biopsy specimens, macroscopic findings are rare and difficult to detect on routine imaging studies with hepatomegaly which is the most common finding and was reported in 29% of the cases [17].
Ultrasonography (US) is generally the first imaging modality used in these patients with sarcoidosis demonstrating clinical symptoms related to liver dysfunction. Coarsening of the liver parenchyma, focal calcifications and contour irregularity are the expected findings [18]. Sarcoid-related parenchymal hepatic fibrosis is also a well-known clinical entity. CT and MRI findings in sarcoid-related chronic liver disease vary significantly among patients from normal morphologic appearance to full-blown cirrhotic liver (Figs. 1, 2). Liver sarcoidosis is among the reasons for liver transplantation, and recurrence of the disease in the liver is unusual with anecdotal cases reported in the literature (Fig. 3) [19]. Massive subcapsular fibrosis representing the loss of hepatocytes and replacement with mass-forming fibrosis, visualized in cirrhosis, can also be detected in the affected patients (Fig. 4) [20]. Peripheral wedge-shaped parenchymal atrophy was also reported to be common which appears as increased enhancement on immediate contrast-enhanced images that become isointense on delayed images. The combination of macroregenerative nodules and peripheral wedge-shaped atrophy was reported to be a helpful finding for the differential diagnosis of sarcoid-related chronic parenchymal liver disease (Fig. 5) [4]. The combination of liver cirrhosis pattern and peripheral wedge-shaped atrophy may also be observed in primary sclerosing cholangitis (PSC) [4]. The presence of these two entities in both hepatic sarcoidosis and PSC suggests a common underlying immune-based mechanism in the pathogenesis of these two conditions [21–23].
CT image of a patient with sarcoidotic involvement of the liver. Contrast-enhanced axial CT of a 57-year-old woman with advanced pulmonary sarcoidosis. Liver presents with normal appearance with enlargement of the spleen, consistent with portal hypertension. Also note several enlarged lymph nodes around the celiac axis (arrows)
Contrast-enhanced fat-suppressed axial T1-weighted MRI of a 55-year-old male patient with biopsy-proven chronic liver disease due to sarcoidosis demonstrates severe fibrosis of the liver parenchyma with contour irregularity and linearly enhanced foci throughout the liver representing fibrosis in the delayed phase (arrows)
55-year-old woman with a long history of hepatic sarcoidosis treated with liver transplantation. Several years after the transplant sarcoidosis recurred in the liver causing end stage liver disease and portal hypertension. Equilibrium phase fat-suppressed T1-weighted image of the liver demonstrates diffuse heterogeneity of the liver parenchyma with ill-defined hypointense areas, fibrosis, contour irregularity, and splenomegaly. Also note the mildly enlarged lymph nodes in the liver hilum (arrows)
42-year-old male with biopsy-proven liver sarcoidosis. Contrast-enhanced fat-suppressed axial T1-weighted MRI reveals prominent enhancement in the subcapsular areas of the right liver lobe representing massive fibrosis in this location (arrows). Also note the chronic occlusion of the main portal vein (arrowheads)
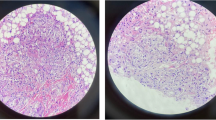
Hepatic granulomas are detected in approximately 4% of the liver biopsies. Pathologically, they are composed of microscopic aggregates of macrophages and lymphocytes, with or without necrosis, and multinucleated giant cells. They form as a response to various exogenous and/or endogenous antigenic stimuli [24]. Both in sarcoidosis and PBC, portal tracts are affected with the tendency of granulomas accumulating in periportal regions [24]. Another useful, but non-specific, feature of hepatic sarcoidosis is periportal thickening, which is best demonstrated on T2-weighted MR images as high signal intensity areas [18, 25] (Fig. 6). Periportal thickening is a non-specific imaging feature and can be detected in multiple benign and malignant clinical conditions. It has been hypothesized that this increased periportal signal might be due to sarcoid granulomas, which have tendency to locate in this area [15].
Portal hypertension is uncommon in the course of the disease. Underlying causes of portal hypertension in hepatic sarcoidosis include cirrhosis, formation of arteriovenous shunts in areas of liver granulomas, and extrinsic compression of portal vein by enlarged perihilar lymph nodes [1]. Portal vein thrombosis does not infrequently occur in liver sarcoidosis and probably results from obliteration of small portal veins secondary to granulomatous phlebitis [26].
Focal involvement of the liver
Detection of focal hepatic lesions was reported to occur in 5% of the patients with liver sarcoidosis [27]. These focal nodules represent the sarcoid granulomas [17, 25, 28, 29]. Hepatic nodules in sarcoidosis usually manifest with well-defined hypo- or hyperechoic appearance on US [30, 31]. They typically appear as low-attenuating subcentimeter lesions on CT (Fig. 7) [16]. Contrast-enhanced CT reveals low-attenuated nodules with less enhancing compared to the liver parenchyma. Sarcoid nodules were reported to be slightly hypointense–isointense on T1-weighted images, while hypointense on T2-weighted images and the contrast enhancement is not expected to be prominent on dynamic contrast-enhanced MRI studies (Figs. 8, 9) [25]. Hypointense appearance of these nodules may be used to differentiate sarcoid nodules from metastases and inflammatory processes which usually manifest with hyperintense appearance on T2-weighted images [31]. When these nodules increase in size and coalesce, they appear as hyperintense lesions on T2-weighted images [13].
61-year-old female with known pulmonary sarcoidosis. Axial post-contrast CT image shows innumerable hypodense lesions throughout the liver (arrows). Also note periportal prominence (arrowheads). Splenic involvement was also confirmed with several subcentimeter hypodense lesions scattered throughout the splenic parenchyma
Among the neoplastic conditions in the differential diagnosis of hepatic sarcoidosis, metastatic liver disease and primary cholangiocarcinoma of the liver should be considered. Larger lesions which represent the coalescence of smaller sarcoid granulomas can also be visualized in other infectious disorders causing granulomatous liver diseases [16, 32–35].
In selected patients with unclear medical history and laboratory findings, image-guided liver biopsy might be helpful in a minimally invasive manner.
Biliary and hilar findings
Biliary ductal dilatation secondary to cholestasis is a relatively common finding in sarcoid liver disease and has been reported to be detected in 20% of the patients in one study evaluating the sarcoid-related chronic liver disease [4]. Cholestasis may be intrahepatic or extrahepatic. Extrahepatic mechanical biliary obstruction may also be detected in sarcoidotic biliary involvement. The underlying mechanism can be either primary involvement of the common hepatic duct or external compression of the extrahepatic bile ducts by the enlarged hilar lymph nodes. The imaging findings may simulate a biliary tumor; therefore, caution should be exercised in reporting these patients, and more clinical information should be requested from the referring physicians for the correct diagnosis (Fig. 10) [33]. Clinical, imaging, and histopathological features of PSC have been also reported in patients with hepatic sarcoidosis [21, 36–38]. The presence of macronodules in the liver parenchyma does not help as they can be detected in both PSC and chronic hepatic sarcoidosis [4]. The morphology of the affected bile ducts is also not helpful, as they tend to appear similarly in PBC and sarcoidotic biliary involvement [39, 40]. There are conflicting opinions in the medical literature regarding whether there is a common underlying immunologic mechanism in these conditions [4]. Devaney et al. reported clinicopathologic features in 100 patients with hepatic sarcoidosis. In their paper, the authors reported pathologic findings similar to PBC in 19 patients [41]. Periportal halo sign, the low signal intensity halo surrounding the enhancing portal veins, was described as a specific finding in PBC cases. The authors attributed this sign to the underlying periportal fibrosis and periportal cellular depletion [42] (Fig. 11). Chronic intrahepatic cholestasis is reported to be one of the rare manifestations of sarcoid liver disease and may mimic PSC and PBC (Fig. 10A) [39, 41].
45-year-old woman with biopsy-proven pulmonary and hepatic sarcoidosis presenting with new onset jaundice. A Thick slab MRCP image demonstrates focal biliary strictures (arrowheads) reminiscent of PSC. B Axial contrast-enhanced CT obtained 2 days after the MRCP demonstrates diffuse circumferential thickening of the proximal common bile duct at the time of the onset of jaundice (arrow). C Axial contrast-enhanced CT obtained 2 years after the first CT and MRCP scans shows significant resolution of the wall thickening in the common hepatic duct wall after medical treatment (arrow). The absence of intrahepatic biliary dilation is an important finding for exclusion of mechanical biliary obstruction. The patient was clinically asymptomatic with normal serum bilirubin levels at the time of this CT scan. The patient was treated with intense immunosuppressive therapy with prednisolone and azathioprine with good clinical and imaging response
Lymphadenopathy is another common finding in sarcoidosis and reported to be detected in about 40% of the afflicted patients [4]. In the intraabdominal compartment, enlarged lymph nodes are most commonly seen in porta hepatis followed by paraaortic and paraceliac areas (Fig. 12) [43]. Sarcoid lymph nodes may demonstrate central hypoenhancing areas mimicking granulomatous infection and may appear in unusual morphologic shapes and locations (Fig. 13). Massive lymphadenopathy in the paraaortic region is rare but may be encountered in patients with systemic sarcoidosis. The imaging characteristics of enlarged lymph nodes are not morphologically distinctive and may easily be confused with other infectious, inflammatory, and neoplastic causes of lymphadenopathy.
65-year-old male with known pulmonary sarcoidosis. A Axial fat-saturated T2-weighted image demonstrates conglomerating lymph nodes in the liver hilum. B Diffusion-weighted image (b = 500 s/mm2) demonstrates enlarged lymph nodes (arrows). Patient declined percutaneous biopsy and these lymph nodes remained stable on long-term follow-up (not shown)
55-year-old male patient with known chronic parenchymal liver disease due to sarcoidosis. Axial post-contrast CT scan demonstrates conglomerating lymph nodes (arrows) extending deep into the liver hilum with central hypoenhancing areas mimicking granulomatous infection. Percutaneous biopsy of these lymph nodes revealed sarcoid granulomas with no evidence of tuberculosis
Conclusion
The imaging findings of liver sarcoidosis can be subtle and somewhat non-specific mimicking other nonneoplastic and neoplastic diseases of the liver. However, with the relevant clinical information, it may be possible to diagnose the disease in a non-invasive manner as there are some, somewhat non-specific, imaging features which may guide the imager to the correct diagnosis. In the presence of relevant clinical information, the detection of multiple 1–2 mm hypodense/hypointense parenchymal nodules, the presence of hilar lymph nodes, and the peripheral wedge-shaped atrophic areas in the liver may be helpful. It should be taken into account that biliary involvement of sarcoidosis may easily mimic a hilar cholangiocarcinoma and, in that case, more invasive studies, like endoscopic retrograde cholangiopancreatography or surgery, might be necessary for correct diagnosis. In patients with diffuse or focal liver disease, where non-invasive differential diagnosis is impossible, image-guided biopsy may be crucial for the diagnosis. Detailed knowledge of the clinical history, awareness of the potential imaging findings, and the common mimickers are mandatory for the correct diagnosis.
References
Karagiannidis A, Karavalaki M, Koulaouzidis A (2006) Hepatic sarcoidosis. Ann Hepatol 5:251–256
Koyama T, Ueda H, Togashi K, et al. (2004) Radiologic manifestations of sarcoidosis in various organs. Radiographics 24:87–104
Iannuzzi MC, Rybicki BA, Teirstein AS (2007) Sarcoidosis. N Engl J Med 357:2153–2165
Ferreira A, Ramalho M, de Campos ROP, et al. (2013) Hepatic sarcoidosis: MR appearances in patients with chronic liver disease. Magn Reson Imaging 31:432–438
Boeck G (1899) Multiple benign sarcoid of the skin. J Cutan Genitourin Dis 17:543–550
Pietinalho A, Hiraga Y, Hosoda Y, et al. (1995) The frequency of sarcoidosis in Finland and and Hokkaido, Japan: a comparative epidemiological study. Sarcoidosis 12:61–67
Rybicki BA, Major M, Popovich J Jr, Maliarik MJ, Iannuzzi MC (1997) Racial differences in sarcoidosis incidence: a 5 year study in a health maintenance organization. Am J Epidemiol 145:234–241
Valeyre D, Prasse A, Nunes H, et al. (2014) Sarcoidosis. Lancet 383:1155–1167
Baughman RP, Lower EE, du Bois RM (2003) Sarcoidosis. Lancet 361:1111–1118
Newman LS, Rose CS, Bresnitz EA, et al. (2004) A case control etiologic study of sarcoidosis: environmental and occupational risk factors. Am J respir Crit Care Med 170:1324–1330
Müller-Quernheim J, Schurmann M, Hofmann S, et al. (2008) Genetics of sarcoidosis. Clin Chest Med 29:391–414
Baughman RP, Culver DA, Judson MA (2011) A concise review of pulmonary sarcoidosis. Am J Respir Crit Care Med 183:573–581
Jung G, Brill N, Poll LW, Koch JA, Wettstein M (2004) MRI of hepatic sarcoidosis: large confluent lesions mimicking malignancy. AJR 183:171–173
Cremers JP, Drent M, Baughman RP, Wijnen PA, Koek GH (2012) Therapeutic approach of hepatic sarcoidosis. Curr Opin Pulm Med 18:472–482
Dourakis SP, Cokkinos DD, Soultati AS, et al. (2007) A case of liver sarcoidosis mimicking cirrhosis. Clin Imaging 31:47–49
Suzuki K, Morise Z, Furuta S, et al. (2011) Hepatic sarcoidosis mimicking hilar cholangiocarcinoma: case report and review of the literature. Case Rep Gastroenterol 5:152–158
Warshauer DM, Dumbleton SA, Molina PL, et al. (1994) Abdominal CT findings in sarcoidosis: radiologic and clinical correlation. Radiology 192:93–98
Kessler A, Mitchell DG, Israel HL, Goldberg BB (1993) Hepatic and splenic sarcoidosis: ultrasound and MR imaging. Abdom Imaging 18:159–163
Cengiz C, Rodriguez-Davalos M, deBoccardo G, et al. (2005) Recurrent hepatic sarcoidosis post liver transplantation manifesting with severe hypercalcemia: a case report and review of the literature. Liver Transpl 11:1611–1614
Naschitz JE, Enat R, Yeshurun D, et al. (1991) Massive subcapsular fibrosis of the liver: ultrasonic and computed tomographic characteristics. J Clin Gastroenterol 13:470–474
Ilan Y, Rappaport I, Feigin R, Ben-Chetrit E (1993) Primary sclerosing cholangitis in sarcoidosis. J Clin Gastroenterol 16:326–328
Maambo E, Brett AS, Vasudeva R, Burns RG (2007) Hepatobiliary sarcoidosis presenting as sclerosing cholangitis: long-term follow-up. Dig Dis Sci 52:3363–3365
Tombazzi C, Waters B, Ismail MK, et al. (2008) Sarcoidosis mimicking primary sclerosing cholangitis requiring liver transplantation. Ann Hepatol 7:83–86
Lagana SM, Moreira RK, Lefkowitch JH (2010) Hepatic granulomas: pathogenesis and differential diagnosis. Clin Liver Dis 14:605–617
Warshauer DM, Semelka RC, Ascher SM (1994) Nodular sarcoidosis of the liver and spleen: appearance on MR images. J Magn Reson Imaging 4:553–557
Moreno-Merlo F, Wanless IR, Shimamatsu K, et al. (1997) The role of granulomatous phlebitis and thrombosis in the pathogenesis of cirrhosis and portal hypertension in sarcoidosis. Hepatology 26:554–560
Scott GC, Berman JM, Higgins JL Jr (1997) CT patterns of nodular hepatic and splenic sarcoidosis: a review of the literature. J Comput Assist Tomogr 21:369–372
Gay S, Shaffer H, Futterer S, Aitchison PM, Patel SJ (1996) Sarcoidosis of the liver with involvement of liver, spleen, abdominal and thoracic lymph nodes, and lungs. AJR 167:245
Hoeffel C, Bokemeyer C, Hoeffel JC, et al. (1996) CT hepatic and splenic apperances with sarcoidosis. Eur J Radiol 23:94–96
Vardhanabhuti V, Venkatanarasimha N, Bhatnagar G, et al. (2012) Extra-pulmonary manifestations of sarcoidosis. Clin Radiol 67:263–276
Gezer NS, Başara I, Altay C, et al. (2015) Abdominal sarcoidosis: cross-sectional imaging findings. Diagn Interv Radiol 21:111–117
Pungpagong S, Steers JL, Wallace MB, Krishna M, Keaveny AP (2006) Hepatobiliary sarcoidosis mimicking Klatskin’s cholangiocarcinoma. Gastrointest Endosc 64:124–125
Rezeig MA, Fashir BM (1996) Biliary tract obstruction due to sarcoidosis: a case report. Am J Gastroenterol 92:527–528
McCluggage WG, Sloan JM (1994) Hepatic granulomas in Northern Ireland: a thirteen year review. Histopathology 25:219–228
Matheus T, Munoz S (2004) Granulomatous liver disease and cholestasis. Clin Liver Dis 8:229–246
Kaassis M, Rabot AF, Person C, Boyer J (1997) Primary sclerosing cholangitis and sarcoidosis. Ann Med Interne (Paris) 148:456–458
Lidar M, Langevitz P, Livneh A, Weiss P, Yosepovich A (2003) Sclerosing cholangitis associated with systemic sarcoidosis. J Clin Gastroenterol 36:84–85
Keller K, Hofmann WJ, Kayser K, et al. (1997) Coincidence of primary sclerosing cholangitis and sarcoidosis-case report and review of the literature. Z Gastroenterol 35:33–39
Alam I, Levenson SD, Ferrell LD, Bass NM (1997) Diffuse intrahepatic biliary strictures in sarcoidosis resembling sclerosing cholangitis. Case report and review of the literature. Dig Dis Sci 42:1295–1301
Bloom R, Sybert A, Mascatello VJ (1978) Granulomatous biliary tract obstruction due to sarcoidosis. Am Rev Res Dis 117:783–787
Devaney K, Goodman ZD, Epstein MS, Zimmerman HJ, Ishak KG (1993) Hepatic sarcoidosis. Clinicopathologic features in 100 patients. Am J Surg Pathol 17:1272–1280
Wenzel JS, Doohoe A, Ford KL 3rd, et al. (2001) Primary biliary cirrhosis: MR imaging findings and description of periportal halo sign. Am J Roentgenol 176:885–889
Warshauer DM, Molina PL, Hamman SM, et al. (1995) Nodular sarcoidosis of the liver and spleen: analysis of 32 cases. Radiology 195:757–762
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Karaosmanoğlu, A.D., Onur, M.R., Saini, S. et al. Imaging of hepatobiliary involvement in sarcoidosis. Abdom Imaging 40, 3330–3337 (2015). https://doi.org/10.1007/s00261-015-0533-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00261-015-0533-6