Abstract
The advent of multi-detector computed tomography (MDCT) has drastically improved the outcomes of patients with multiple traumatic injuries. However, there are still diagnostic challenges to be considered. A missed or the delay of a diagnosis in trauma patients can sometimes be related to perception or other non-visual cues, while other errors are due to poor technique or poor image quality. In order to avoid any serious complications, it is important for the practicing radiologist to be cognizant of some of the most common types of errors. The objective of this article is to review the various types of errors in the evaluation of patients with multiple trauma injuries or polytrauma with MDCT.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Errors in radiology have been a highly debated topic as early as the 1920s because of their serious medical and legal implications [1]. This topic is especially important in patients with polytrauma, which is defined as traumatic injuries affecting multiple organs concurrently and being life threatening, even though the mortality of polytrauma patients has significantly dropped from 40% to 10% from 1907 to 2008 [2]. Only 10% of these errors are due to human perception or other non-visual cues [3–5]. With the implementation of multi-detector computed tomography (MDCT), errors can also be caused by poor image quality and technique [6].
A trauma team, which consists of emergency physicians, surgeons, radiologists, and the ancillary staff, works very efficiently if they are given sufficient patient information [7, 8]. If patients are unconscious, uncooperative, hemodynamically unstable, or do not have an adequate clinical history, then they become particularly challenging [9, 10]. An incomplete history results in 10% likelihood in the delay of diagnosis [11] and insufficient physical exam in a patient with abdominal injuries is only 60% reliable [12, 13]. Twenty-five percent of unconscious patients with serious head injuries have equivocal or misleading clinical findings. Therefore, a patient with polytrauma is a catalyst for multiple errors as well as serious complications for various reasons: inadequate history, quick life-saving decisions, multiple concurrent tasks, and multidisciplinary approach. Moreover, the vast majority of physicians working at a level 1 trauma center comprise junior medical staff, often still poorly experienced in the management of polytrauma patients [4, 7]. Therefore, errors can occur because of the severity and complexity of the injuries or due to the patient’s pre-existing medical conditions [9].
Because of all these factors, a radiologist must review a patient’s studies thoroughly.
A complete history, including the type and the mechanism of injury, is instrumental in directing the physician to perform a more thorough physical exam [14, 15]. By knowing this, radiologists can avoid future mistakes, which are common among a specific patient population. For example, blunt trauma in the elderly has more severe injuries than in children [16]. Approximately 40% of the cases of a delayed diagnosis are due to a clinical survey oversight: 15% occur during the primary survey, 25% occur during secondary survey, and 50% occur during tertiary survey or re-evaluation. Errors in the execution or reporting of diagnostic exams can also contribute to these oversights in the secondary and tertiary surveys. The rate of misdiagnosis (incorrect or even not performed diagnosis) ranges widely from 2% to 40% based on how the frequency of error was determined (trauma registries, retrospective chart review, and retrospective review of all admissions) and a clear numerical estimation is difficult just because of the considerable heterogeneity of the methods of retrospective assessment between the different centers [17]. At the end of a large retrospective study, Geyer et al. concluded that only a few missed injuries in initial WBCT reading are clinically relevant; however, as the vast majority of these injuries are detectable, the radiologist has to be alert for commonly missed findings to avoid a delayed diagnosis [18]. Therefore, the errors in emergency radiology are multivariable [19, 20]. Since MDCT’s implementation in the evaluation of the patients with polytrauma, the cause for different and recurrent types of errors in addition to their rationale has been discussed extensively [21–24].
Typically, errors with MDCT are commonly associated with perception or non-visual cues, but about 60% of the missed cases are caused by poor technique or poor image quality [2, 25] which is known as technical and methodological errors.
Technical and methodological errors
Since inception of faster multi-detector CT scanners with higher resolution, various members of the medical staff are able to perform “whole-body” Computed Tomography (WBCT) scans on both the stable and unstable patient. With the appropriate technique, adequate contrast enhancement, and sufficient clinical information, MDCT has become the gold standard for the evaluation of patients with polytrauma. At many institutions, a WBCT protocol [26–28] is routinely performed in patients with polytrauma. This is especially important in the assessment of patients with spinal and pelvic fractures, which are frequently missed on plain-film radiography. MDCT is also essential in the identification of traumatic injuries to head, chest, or abdomen. Above all, this is critical in locating the source of bleeding with a vascular injury, which are more acutely important and of greater clinical relevance than fractures of the extremities or solid organ injuries [29]. Blunt cerebral-vascular injuries are frequently under-diagnosed in patients with polytrauma [30]. Therefore, these patients should also undergo a contrast-enhanced MDCT involving the carotid and vertebral vessels in the arterial phase. MDCT technology results in reduction of the temporal resolution, which has several advantages in the detection and characterization of vascular injuries [31]. The primary cause of death in patients with polytrauma is primarily due to severe hemorrhage from traumatic broncho-pulmonary vessel injury [32]. Therefore, MDCT protocols in the polytrauma patient should also include CTA of the chest [33].
MDCT has a high sensitivity for the detection of active bleeding in the trauma patient [34]. The sensitivity of active hemorrhage with MDCT in patients with visceral injury or pelvic fractures is 13%–18% [35, 36]. This carries a significant morbidity and mortality in polytrauma patients because it suggests a vascular or solid organ injury [37]. The detection and localization of active extravasation improves patient care, thus it avoids a delay or a missed diagnosis. The topic of vascular injuries in polytrauma patients with solid organ (liver, spleen, kidney), gastrointestinal/mesenteric, and pelvic sources of bleeding have been discussed extensively and many classifications of injuries were established based on CT findings [29, 31, 38–43].
From the authors’ perspective, it is not sufficient to just identify the region of extravasation, but it is even more important to differentiate whether it is arterial or venous hemorrhage. This is important because patients with hemorrhage are not always hemodynamically unstable. Therefore, the use of the appropriate MDCT protocol is important to find the source of the bleed for the interventional radiologist before the patient succumbs to hypovolemic shock [43].
Current MDCT protocols are highly sensitive for active hemorrhage and should be tailored as necessary. A non-contrast study should always be performed in order to assess for parenchymal lesions in the presence of hemoperitoneum or the “sentinel clot” sign (this is important in identifying the source of bleeding when other findings of vessel injury are not present, or identifying intramural hematoma of the aorta, which cannot be seen on contrast-enhanced study). Then, a biphasic—arterial and venous—study after the injection of approximately 100–130 mL of iodinated contrast (370–40 mgI/mL) at high flow rate of 3–5 mL/s [44] allows the identification of any eventual active bleeding also defining its characteristics (low or high flow, arterial or venous origin). Bolus tracking is preferred in any case over manual technique for timing of the arterial phase. A slice thickness in the range of 0.5–3 mm is recommended for evaluating vasculature in the arterial phase, but 3–5-mm slice thickness is sufficient for identifying solid organ injury with venous phase. In order to immediately evaluate the progress of the bleeding sites, additional scans can be performed soon after the acquisition of the venous phase, so differentiating life-threatening massive arterial bleedings from insidious low-flow venous bleedings. If there is suspicion of injury to the kidneys or ureters, delayed excretory phase is recommended as nephrographic phase at 500–700 s delay. This phase is important not only in the dynamics of vascular extravasations (changing in morphology) but also to assess for trauma to ureters, which is managed either conservatively or with a percutaneous drainage catheter with or without ureteral stenting [41] (Fig. 1). For bladder injury, active distension of the bladder followed by MDCT Cystogram with diluted contrast material is required to exclude a bladder leak [45–47]. It is important to avoid false-negative cases to recognize that passive distension of the bladder, using excreted contrast material only, during a routine MDCT study cannot be relied on to diagnose bladder rupture, even with clamping of a urethral catheter [45, 48, 49], even if the bladder is distended. Between 300 and 350 mL of 5% diluted contrast media is instilled into the bladder followed by axial CT imaging of the pelvis [49]. The distension of the bladder with diluted contrast material before performing CT of the abdomen and pelvis CT has shown satisfactory results [46].
28-year-old male patient admitted to the Emergency Department after a motor vehicle accident. A Contrast-enhanced axial scan shows deep renal lacerations with a surrounding peri-renal hematoma. B Contrast-enhanced axial scan shows a high-density fluid within the urinary pelvis (arrow). Fluid within the pelvis should not be mistaken for a venous bleeding. C In the delayed acquisition, axial CT scan shows urine extravasation from the left pyelo-ureteral junction (arrow). D Coronal MIP image shows continuity of the left collecting system which suggests a non-operative management. Urinary leak from the pyelo-ureteral junction is also seen (arrow). E After six hours of follow-up, coronal MIP reformation demonstrates integrity of the collecting system without any urinary leak.
At our institution, MDCT cystography is performed after the initial CT of the abdomen and pelvis [50]. This technique consists of pre- and post-cystography CT scans, to insure extra-luminal contrast material from the procedure is actually from the bladder. If the bladder is filled before the CT scan, a urinary leak can be confused with an active bleeding. Therefore, contrast medium, which leaks due to lower urologic injuries, can interfere with the CTA for pelvic arterial extravasation, thus resulting in a delay of localization and plans for embolization [51]. Another way to avoid a delayed diagnosis is with the use of the post-processing tool multiplanar reformations (MPR). This is helpful in identifying spine fractures, pelvic fractures, diaphragmatic injuries, hematoma, and regions of active hemorrhage. MPR can also better delineate a ureteral or bladder injury. The most common location for a bladder injury involves the dome of the bladder [51]. MDCT scanners have improved imaging quality using faster acquisitions and thinner slice thickness. Isotropic datasets of large regions are acquired with reformations to provide a roadmap of the vascular and bony structures [52].
Axial, sagittal, and coronal planes are important to identify the vessel of origin of active hemorrhage as well as to understand the extent and severity of injury by identifying the area of active hemorrhage [53]. MPR can also be used to accurately classify vessel injury such as pseudo-aneurysm and arterio-venous fistulae. In all cases, coronal and sagittal MPRs should be calculated using the complete reconstruction matrix for only one body region such as thorax and abdomen and head and neck. This is crucial, as only this strategy allows for optimal high-resolution good-quality MPR reconstructions knowing that the pixel matrix is fixed and limited and so stretched over just one body region and not the entire torso.
Differentiating an active arterial bleeding from other entities such as pseudo-aneurysms and arterio-venous fistulae remains difficult in some cases, with 25% of the latter two conditions misdiagnosed or even non-diagnosed [43]. The use of standardized MDCT protocols may increase diagnostic sensitivity, with significant therapeutic and prognostic implications: when an active bleeding or a contained vascular injury is detected, in fact, the trauma surgeon can then decide whether a conservative therapy, endovascular intervention, or emergency surgery is the best course of action.
Spectrum of diagnostic errors
One of the most commonly type of error in diagnostic radiology is the failure of recognition. For instance, one of the most common causes of error in polytrauma patients is failure to detect fractures, which may account for 41%–80% of diagnostic errors in the Emergency Department [53–56]. Missed fractures are most commonly located in the peri-articular regions, shoulder girdle, and feet. Spine injuries comprise only 10% of all initially missed diagnoses. These are common at the cranio-cervical junction and cervico-thoracic junction. Transverse process fractures are associated with vertebral body fractures in approximately 10% of the cases and are associated with intra-abdominal injuries in up to 50% of the cases [57, 58].
In comparison, the fractures of the extremities missed liver and spleen injuries contribute to 10%–15% of missed findings. Injuries to the small and large bowel also contribute to diagnostic errors (approximately 15%–20% of delayed diagnoses). Diaphragmatic injuries are uncommon and also represent only 5% of all delayed diagnoses. Vascular injuries constitute only 5% of delayed diagnoses [17]. Among children with polytrauma, uretero-pelvic junction injuries were missed in approximately 50% of cases on initial evaluation [59]. Finally, more than 80% of women with a unknown pregnancy are undiagnosed on initial evaluation and clinical guidelines and radiological protocols are not established for emergent imaging in pregnant women [60].
Perceptual errors, in general, can be related to multiple cognitive and physiological factors, including level of observer alertness or fatigue, duration of the observation task, any distractions, conspicuity of the abnormality as well as many others [61].
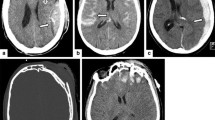
Another type of error is incorrectly classifying a normal finding as abnormal; this phenomenon is often common among radiology residents or inexperience radiologists who are being overly cautious [62]. As a result, this will cause an unnecessary hospital admission. For example, patient movement or respiratory motion can sometimes simulate fracture or cause a double contour within a solid organ which can mimic a subcapsular hematoma. Streak artifact from bones (arms commonly) can simulate a parenchymal laceration in the solid organs (spleen and liver typically). Anatomic variants, actually of no clinical relevance, may mislead the observer, as in the case of splenic clefts, often misdiagnosed with low-grade parenchymal laceration (Fig. 2) [7, 63].
36-year-old female post a high-energy deceleration injury in comatose status. A Contrast-enhanced axial CT scan shows a deep splenic cleft. This finding may be confused with a splenic laceration especially when there are traces of blood in between (B arrow). C–E Three non-contiguous enhanced CT scans show large amount of active bleeding in the left subphrenic space which was erroneously related to a splenic injury. Location and disposition of active bleeding would have addressed the suspicion on a diaphragmatic arterial injury. The patient was taken to the operating room. The spleen was intact at laparotomy. However, a diaphragmatic arterial injury was found. This injury is managed ideally with angiographic embolization.
Conversely, intentional under-calling is a tendency to interpret abnormality finding as negative [64]. This can occur because of pressure from others to reduce the number of false-positive interpretations, thus thereby minimizing any unnecessary follow-up. Some have described this type of error as faulty reasoning [65].
Another category of error is not due to failure to detect or characterize an abnormal finding but assign it an incorrect etiology or underestimate–overestimate the severity of the related pathologic condition (e.g., a radiologist may address to operative management when not necessary) (Fig. 3). Provenzale et al. classified these last two types of error as a error of misinterpretation [62].
60-year-old male patient run over by a car. A Axial contrast-enhanced scan reveals ruptured left renal cyst with signs of active bleeding. A wide meta-traumatic mesenteric infiltration from trauma is also appreciable, with small, not refurnished blood collections, suggestive for mesenteric haematomas (arrow). Coronal reformation image (b) better depicts the ruptured left renal cyst, also highlighting the presence of a subtle subcapsular haematoma. CT control performed 48 h later (C, D) shows evident increase of the subcapsular blood collection and diffuse imbibitions and inhomogenity of the retroperitoneal spaces from haemoretroperitoneum, with ruptured cyst more evident. No active bleeding was demonstrated at CT. Finally, the patient was successfully managed non-operatively.
Another form of observer error that can result in important findings being overlooked is due to the “satisfaction of search” (SOS) error. This is defined as once a major abnormal finding has been detected, the radiologist’s search time is quickly abbreviated from the rest of the study [66], thus further abnormalities are left virtually undetected. This is a deliberate truncation of a search rather than a faulty search pattern [67].
Another main reason why radiologists are sued is the failure to suggest the next appropriate study. Radiologists must recommend the most appropriate study according to the American College of Radiology appropriateness criteria. The American College of Radiology “Practice Guideline for Communication of Diagnostic Imaging Findings” states that “follow-up or additional diagnostic studies to clarify or confirm the impression should be suggested when appropriate” [68]. This is the case, for example, of a polytrauma patient who has equivocal findings.
However, errors in communication are most frequent cause of medical malpractice against radiologists [69, 70]. In addition to issuing a final written report, the radiologist should communicate important findings directly to the emergency physician or surgeon [71]. In emergency radiology, a quick diagnosis and treatment is essential to improve the management and outcome of trauma patients. Therefore, if the communication between the radiology and referring physician does not occur and is not documented, the radiologist can be held accountable when there are adverse or unexpected clinical outcomes. Therefore, documentation should always include the date, time, name of the person who was spoken to, and what was discussed [72].
Conclusion
Polytrauma is an acute multi-organ disease, which requires immediate clinical assessment and evaluation. With the advent of MDCT, patient outcomes have significantly improved, but diagnostic errors still persist and can result in serious mismanagement with grave consequences for patients. In addition, radiologists can be held accountable for any misfortunate turn of events.
Therefore, a strong relationship with the trauma team is important before and after the MDCT, in order to obtain an adequate history and important findings on physical exam.
Diagnostic error rate can be reduced using shared guidelines and established pre-programmed WBCT protocols, applying an institutional-based logistic and personal concept, organizing institutional morbidity and mortality conferences on difficult clinical cases and unexpected death, external and internal quality assurance system and external registries, and allowing for research and development in the fields of emergency radiology and patient care. Finally, young emergency radiologists, as well as possessing a strong knowledge, should have a working experience of least of 1 year at major trauma centers as assistants to expert colleagues.
References
Roberts F (1928) Errors in the interpretation of radiograms of the chest: their correction by tele-radiography. Br Med J 2:599–601
Nicolaou S, Eftekhari A, Sedlic T, et al. (2008) The utilization of dual source CT in imaging of polytrauma. Eur J Radiol 68:398–408
Ivatury RR, Guilford K, Malhotra AK, et al. (2008) Patient Safety in Trauma: maximal impact management errors at a level I trauma center. J Trauma 64:265–272
Gruen RL, Jurkovich GJ, McIntyre LK, et al. (2006) Patterns of errors contributing to trauma mortality: lessons learned from 2,594 deaths. Ann Surg 244:371–380
Teixeira PG, Inaba K, Hadjizacharia P, et al. (2007) Preventable or potentially preventable mortality at a mature trauma center. J Trauma 63:1338–1347
Rieger M, Czermak B, El Attal R, et al. (2009) Initial clinical experience with a 64-MDCT whole-body scanner in an emergency department: better time management and diagnostic quality? J Trauma 66:648–657
West RW (2000) Radiology malpractice in the emergency room setting. Emerg Radiol 7:14–18
George JE, Espinosa JA, Quattrone MS (1992) Legal issues in emergency radiology. Practical strategies to reduce risk. Emerg Med Clin N Am 10:179–203
Buduhan G, McRitchie DI (2000) Missed injuries in patients with multiple trauma. J Trauma 49:600–605
Biffl WL, Harrington DT, Cioffi WG (2003) Implementation of a tertiary trauma survey decreases missed injuries. J Trauma 54:38–43
Sung CK, Kim KH (1996) Missed injuries in abdominal trauma. J Trauma 41:276–282
Poletti PA, Wintermark M, Schnyder P (2002) Traumatic injuries: role of imaging in the management of the polytrauma victim (conservative expectation). Eur Radiol 12:969–978
Schurink GW, Bode PJ, van Luijt PA, et al. (1997) The value of physical examination in the diagnosis of patients with blunt abdominal trauma: a retrospective study. Injury 28:261–265
Tomczak PD, Buikstra JE (1999) Analysis of blunt trauma injuries: vertical deceleration versus horizontal deceleration injuries. J Forensic Sci 44:253–262
Fitzharris M, Franklyn M, Frampton R (2004) Thoracic aortic injury in motor vehicle crashes: the effect of impact direction, side of body struck, and seat belt use. J Trauma 57:582–590
Newgard CD (2008) Defining the “older” crash victim: the relationship between age and serious injury in motor vehicle crashes. Accid Anal Prev 40:1498–1505
Stanescu L, Talner LB, Mann FA (2006) Diagnostic errors in polytrauma: a structured review of the recent literature. Emerg Radiol 12:119–123
Geyer LL, Korner M, Linsenmaier U, et al. (2013) Incidence of delayed and missed diagnoses in whole-body multidetector CT in patients with multiple injuries after trauma. Acta Radiol 54:592–598
FitzGerald R (2001) Error in radiology. Clin Radiol 56:938–946
Tuddenham WJ (1962) Visual search, image organization, and reader error in roentgen diagnosis: studies of the psychophysiology of roentgen image perception. Radiology 78:694–704
West OC, Anderson J, Lee JS, et al. (2002) Patterns of diagnostic error in trauma abdominal CT. Emerg Radiol 9:195–200
Wechsler RJ, Spettell CM, Kurtz AB, et al. (1996) Effects of training and experience in interpretation of emergency body CT scans. Radiology 199:717–720
Lal NR, Murray UM, Eldevik OP, et al. (2000) Clinical consequences of misinterpretations of neuroradiologic CT scans by on-call radiology residents. Am J Neuroradiol 21:124–129
Roszler MH, McCarroll KA, Rashid T, et al. (1991) Resident interpretation of emergency computed tomographic scans. Invest Radiol 26:374–376
Hirshberg A, Wall MJ Jr, Allen MK, et al. (1994) Causes and patterns of missed injuries in trauma. Am J Surg 168:299–303
Ptak T, Rhea J, Novelline R (2001) Experience with a continuous, single-pass whole-body multi-detector CT protocol for trauma: the three-minute multiple trauma CT scan. Emerg Radiol 8:250–256
Ptak T, Rhea JT, Novelline RA (2003) Radiation dose is reduced with a single-pass whole-body multi-detector row CT trauma protocol compared with a conventional segmented method: initial experience. Radiology 229:902–905
Fanucci E, Fiaschetti V, Rotili A, et al. (2007) Whole-body 16-row multislice CT in emergency room: effects of different protocols on scanning time, image quality and radiation exposure. Emerg Radiol 13:251–257
Pinto A, Niola R, Tortora G, et al. (2010) Role of multidetector-row CT in assessing the source of arterial haemorrhage in patients with pelvic vascular trauma. Comparison with angiography. Radiol Med 115:648–667
Mutze S, Rademacher G, Matthes G, et al. (2005) Blunt cerebrovascular injury in patients with blunt multiple trauma: diagnostic accuracy of duplex Doppler US and early CT angiography. Radiology 237:884–892
Anderson SW, Lucey BC, Rhea JT, et al. (2007) 64 MDCT in multiple trauma patients: imaging manifestations and clinical implications of active extravasation. Emerg Radiol 14:151–159
Barendregt WB, de Boer HH, Kubat K (1993) Quality control in fatally injured patients: the value of the necropsy. Eur J Surg 159:9–13
Weninger P, Mauritz W, Fridrich P, et al. (2007) Emergency room management of patients with blunt major trauma: evaluation of the multislice tomography protocol exemplified by an urban trauma center. J Trauma 62:584–591
Roy-Choudhury SH, Gallacher DJ, Pilmer J, et al. (2007) Relative threshold of detection of active arterial bleeding: in vitro comparison of MDCT and digital subtraction angiography. Am J Roentgenol 189:238–246
Yao DC, Jeffrey RB Jr, Mirvis SE, et al. (2002) Using contrast enhanced helical CT to visualize arterial extravasation after blunt abdominal trauma: incidence and organ distribution. Am J Roentgenol 178:17–20
Willmann JK, Roos JE, Platz A, et al. (2002) Multidetector CT: detection of active hemorrhage in patients with blunt abdominal trauma. Am J Roentgenol 179:437–444
Hamilton JD, Kumaravel M, Censullo ML, et al. (2008) Multidetector CT evaluation of active extravasation in blunt abdominal and pelvic trauma patients. RadioGraphics 28:1603–1616
Poletti PA, Mirvis SE, Shanmuganathan K, et al. (2000) CT criteria for management of blunt liver trauma: correlation with angiographic and surgical findings. Radiology 216:418–427
Park SJ, Kim JK, Kim KW, et al. (2006) MDCT findings of renal trauma. Am J Roentgenol 187:541–547
Sica G, Bocchini G, Guida F, et al. (2010) Multidetector computed tomography in the diagnosis and management of renal trauma. Radiol Med 115:936–949
Stuhlfaut JW, Anderson SW, Soto JA (2007) Blunt abdominal trauma. Current imaging techniques CT findings in patients with solid organ, bowel and mesenteric injury. Semin Ultrasound CT MRI 28:115–129
Atluri S, Richard HM 3rd, Shanmuganathan K (2011) Optimizing multidetector CT for visualization of splenic vascular injury. Validation by splenic arteriography in blunt abdominal trauma patients. Emerg Radiol 18:307–312
Albrecht T, Foert E, Holtkamp R, et al. (2007) 16-MDCT angiography of aortoiliac and lower extremity arteries: comparison with digital subtraction angiography. Am J Roentgenol 189:702–711
Sandler CM, Francis IR, Baumgarten DA, et al. (2007) Suspected lower urinary tract trauma. In: ACR appropriateness criteria. Reston, VA: American College of Radiology
Quagliano PV, Delair SM, Malhotra AK (2006) Diagnosis of blunt bladder injury: a prospective comparative study of computed tomography cystography and conventional retrograde cystography. J Trauma 61:410–421
Deck AJ, Shaves S, Talner L, et al. (2000) Computerized tomography cystography for the diagnosis of traumatic bladder rupture. J Urol 164:43–46
Mee SL, McAninch JW, Federle MP (1987) Computerized tomography in bladder rupture: diagnostic limitations. J Urol 137:207–209
Vaccaro JP, Brody JM (2000) CT cystography in the evaluation of major bladder trauma. RadioGraphics 20:1373–1381
Peng MY, Parisky YR, Cornwell EE, et al. (1999) CT cystography versus conventional cystography in evaluation of bladder injury. Am J Roentgenol 173:1269–1272
Spencer Netto FA, Hamilton P, Kodama R, et al. (2008) Retrograde urethrocystography impairs computed tomography diagnosis of pelvic arterial hemorrhage in the presence of a lower urologic tract injury. J Am Coll Surg 206:322–327
Chan DP, Abujudeh HH, Cushing GL Jr, et al. (2006) CT cystography with multiplanar reformation for suspected bladder rupture: experience in 234 cases. Am J Roentgenol 187:1296–1302
Vu M, Anderson SW, Shah N, et al. (2010) CT of blunt abdominal and pelvic vascular injury. Emerg Radiol 17:21–29
Berlin L (2001) Defending the “missed” radiographic diagnosis. Am J Roentgenol 176:317–322
Guly HR (2001) Diagnostic errors in an accident and emergency department. Emerg Med J 18:263–269
Williams SM, Connelly DJ, Wadsworth S, et al. (2000) Radiological review of accident and emergency radiographs: a 1-year audit. Clin Radiol 55:861–865
Brooks A, Holroyd B, Riley B (2004) Missed injury in major trauma patients. Injury 35:407–410
Krueger MA, Green DA, Hoyt D, et al. (1996) Overlooked spine injuries associated with lumbar transverse process fractures. Clin Orthop 327:191–195
Patten RM, Gunberg SR, Brandenburger DK (2000) Frequency and importance of transverse process fractures in the lumbar vertebrae at helical abdominal CT in patients with trauma. Radiology 215:831–834
Onuora VC, Patil MG (1993) al-Jasser AN: missed urological injuries in children with polytrauma. Injury 24:619–621
Bochicchio GV, Napolitano LM, Haan J, et al. (2001) Incidental pregnancy in trauma patients. J Am Coll Surg 192:566–569
Pitman AG (2006) Perceptual error and the culture of open disclosure in Australian radiology. Australas Radiol 50:206–211
Provenzale JM, Kranz PG (2011) Understanding errors in diagnostic radiology: proposal of a classification scheme and application to emergency radiology. Emerg Radiol 18:403–408
Scaglione M, Romano L, Forner AL, et al. (1996) Computerized tomography in the differential diagnosis of congenital lobulations and traumatic lacerations of the spleen. Report of a case. Radiol Med 92:324–326
Woodring JH (1990) Pitfalls in the radiologic diagnosis of lung cancer. Am J Roentgenol 154:1165–1175
Renfrew DL, Franken EA Jr, Berbaum KS, et al. (1992) Error in radiology: classification and lessons in 182 cases presented at a problem case conference. Radiology 183:145–150
Samuel S, Kundel HL, Nodine CF, et al. (1995) Mechanism of satisfaction of search: eye position recordings in the reading of chest radiographs. Radiology 194:895–902
Berbaum KS, Brandser EA, Franken EA, et al. (2001) Gaze dwell times on acute trauma injuries missed because of satisfaction of search. Acad Radiol 8:304–314
American College of Radiology (2005) ACR practice guideline for communication of diagnostic imaging findings. In: 2005 practice guideline & technical standards. Reston, VA: American College of Radiology, pp 5–9
Harrigal CL, Erly WK (2007) On-call radiology: community standards and current trends. Semin Ultrasound CT MR 28:85–93
Thomson CB, Greaves I (2008) Missed injury and the tertiary trauma survey. Injury 39:107–114
Pinto A, Acampora C, Pinto F, et al. (2011) Learning from diagnostic errors: a good way to improve education in radiology. Eur J Radiol 78:372–376
Raskin MM (2006) Survival strategies for radiology: some practical tips on how to reduce the risk of being sued and losing. J Am Coll Radiol 3:689–693
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Scaglione, M., Iaselli, F., Sica, G. et al. Errors in imaging of traumatic injuries. Abdom Imaging 40, 2091–2098 (2015). https://doi.org/10.1007/s00261-015-0494-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00261-015-0494-9