Abstract
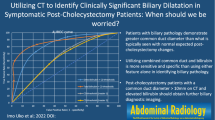
Purpose: To evaluate common duct (CD) dilation by computed tomography (CT) in patients with intact gallbladders and diameter change over time in remote and interval cholecystectomy patients, frequency of visualization of the CD, and its relationship to age. Methods: This IRB-approved retrospective study evaluated baseline CD diameter, intrahepatic biliary dilation, and interval duct diameter change in patients with CTs ≥ 2 years apart (n = 324), in block-randomized order by two blinded board-certified radiologists. 272 patients were divided into three groups: (1) prior cholecystectomy before the first CT, (2) cholecystectomy between the first and last CTs, and (3) no cholecystectomy. A subset of 191 nonoperated patients was evaluated for age-related dilation. Results: Group 1 ducts were significantly larger than the other groups at both baseline and follow-up CTs (p < 0.001). Group 2 showed a greater increase in duct size than the other groups at follow-up (p < 0.001). The CD was measurable in 89% of the CT studies. In nonoperated patients, there was a statistically significant correlation between CD size and increasing age (p < 0.001), although the CD size remained within normal size limits. Conclusion: Remote cholecystectomy patients have larger CD diameters than the nonoperated and interval cholecystectomy groups. Greater increase in ductal diameter occurred between studies in the interval cholecystectomy patients, suggesting that dilation occurs after cholecystectomy. Also, the CD dilates slightly with age in nonoperated patients.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Post-cholecystectomy dilation of the common duct (CD) was first recognized by Oddi [1] in 1887 in animals as substituting for the reservoir function of the gallbladder. However, for humans, this concept remains controversial in the surgical, radiographic, and sonographic literature. Several prospective sonographic studies demonstrated that while the majority of patients did not have a substantial increase in diameter of the common hepatic duct after cholecystectomy, there was a minor trend towards dilation [2, 3]. In other prospective studies, postcholecystectomy CD measurements were not significantly increased [4–6]. A recent large series suggests a 7-mm diameter threshold by ultrasound [7], but the literature regarding bile duct diameter on computed tomography (CT) is even less conclusive.
The purpose of our study was to help in resolving the controversy surrounding the normal limits of CD diameter on CT in post-cholecystectomy patients, which would have important implications in managing such conditions. Patients with CD dilation after cholecystectomy may undergo further investigations including laboratory analysis, imaging evaluation, and endoscopic retrograde cholangiopancreatography (ERCP), so understanding what represents important dilation can be helpful to limit the radiation dose associated with repeat CT exams and the potential complications of ERCP. Unlike prior reports, our study examined the CD diameter by CT at baseline and greater than two years after cholecystectomy in remote and interval cholecystectomy patients and also over the same interval in nonoperated patients. Furthermore, we evaluated the frequency of CT visualization of the CD at the porta hepatis in unenhanced and contrast-enhanced studies, as it was previously reported that the normal CD was visualized by CT in only 30–66% patients [8, 9]. In the subset of nonoperated patients, we also assessed whether the size of the extrahepatic bile duct increased with age in patients, based on long-term CT follow-up.
Materials and methods
This IRB-approved, HIPAA-compliant retrospective study evaluated baseline CD diameter, central intrahepatic biliary dilation, and interval duct diameter change in patients (ages 17–84) with abdominal CTs at least 2 years apart between 1/1/2002 and 12/31/2008 (n = 324). Twenty patients were excluded because they did not have two CTs greater than two years apart. Patients were identified by a radiology clinical database within a departmental mini-PACS. The study was performed at a tertiary care academic hospital with inpatient and outpatient facilities.
We evaluated the ability to visualize and measure the CD in the remaining 304 patients on either unenhanced CT (UECT) or contrast-enhanced CT (CECT) examinations at 5-mm intervals. A total of 608 scans were interpreted (104 UECT; 504 CECT). The study population consisted of 172 women and 132 men with a mean age of 51.9 ± 14.9 years.
Each CD was measured in block-randomized order by two blinded, experienced, board-certified abdominal radiologists, one with 13 years faculty experience (ML) and the other with 33 years faculty experience (LLB). UECT and CECT studies at 5-mm intervals were included, using a variety of scanners over the 7-year period from which the data were collected. Scanners included General Electric 4, 16, and 64 detector-row scanners and Philips 16, 40, and 64 detector row scanners. The axial diameter of the CD was measured at the porta hepatis adjacent to the main portal vein in all patients, and the results were expressed to the nearest tenths of millimeters using the electronic calipers of the PACS. The diameter of the CD was measured from outer wall-to-outer wall at its margin with adjacent fat. Coronal reformatted images were not routinely utilized during the time interval and not included for review. The presence or the absence of intrahepatic biliary dilation was also determined, which was considered present when the bile ducts were well visualized beyond the first branching of the right or left hepatic ducts. It was also considered present if the intrahepatic bile ducts measured greater than 2 mm or if it was 40% greater in size than the adjacent portal vein branch [10, 11].
In our study, the common hepatic duct and the common bile duct were not evaluated separately, and the intrahepatic and intrapancreatic CD portions were excluded from measurement consideration. The duct was measured at a point separate from cystic duct, when possible to discern. A diameter of 6 mm or less was considered a normal measurement of the CD at the porta hepatis. Patients with acute pancreaticobiliary disease (acute cholecystitis, active biliary obstruction, chronic pancreatitis, etc.) by clinical and/or laboratory criteria, hepatobiliary malignancy, extensive surgery beyond routine cholecystectomy, significant postoperative complications, subsequent operations for biliary disease, or nonvisualization of the CD were excluded (n = 32) from diameter analysis. The CT images and reports, laboratory analysis (total bilirubin, indirect bilirubin, direct bilirubin, AST, and ALT values), and medical records of all the subjects were reviewed by an investigator who was not involved in the image measurement on CT.
The 272 patients with a measureable CD who met the inclusion criteria were divided into three groups. The baseline and follow-up CD diameters as well as interval change in CD size were statistically compared among the groups, which were as follows: (1) remote cholecystectomy (mean of 12.8 years before baseline CT), (2) interval cholecystectomy (between the first and last CT), and (3) no cholecystectomy (Table 1). In Group 1, remote cholecystectomy was defined as surgery greater than 2 years prior to the first CT, although all patients had greater than 3 years follow-up.
Statistical analysis was performed by a biostatistician investigator who was not involved in data collection or duct measurements. Clinical data and duct diameters were evaluated using Chi Square, ANOVA, and Tukey’s HSD tests. Chi-square tests were used to compare discrete variables among the three groups, and one-way analysis of variance (ANOVA) was used to compare continuous variables. When the ANOVA was significant, Tukey’s HSD test was used to define which groups differed. A p-value of <0.05 was considered to be statistically significant.
The subset of 191 nonoperated patients (group 3) was stratified into five groups based on age at the time of the first CT exam to evaluate for age-related dilation. The study population consisted of 107 women and 84 men with a mean age of 53.6 ± 15.6 years. Only patients for whom the CD was visualized were included. The five age groups were stratified as follows: (1) <40 (n = 26), (2) 40–49 (n = 35), (3) 50–59 (n = 53), (4) 60–69 (n = 31), and (5) ≥70 years (n = 46). Clinical data and duct diameters were evaluated using chi-square, ANOVA, and Tukey’s HSD tests.
Results
Common duct dilation by CT
In patients with a history of prior cholecystectomy, abnormal caliber ducts (>6 mm) were found in 32 patients (59%) at both the baseline and follow-up CT dates. Twenty-three of the 48 prior-cholecystectomy patients had their baseline CT greater than or equal to 10 years after gallbladder removal. Of these 23 patients, 16 (70%) had dilated CDs at both baseline and follow-up CT examinations (Table 2).
For patients who underwent interval cholecystectomy (group 2) and were studied before and a minimum of two years after cholecystectomy, the follow-up was up to 5.8 years after cholecystectomy. Abnormal caliber ducts (>6 mm) were found in 7 patients (21%) before surgery and 22 patients (67%) postoperatively. The interval dilation for Group 2 (mean 1.8 mm) was statistically greater than the change in other groups (p < 0.001) (Table 2). After cholecystectomy, the diameter of the CD increased in 26 patients, decreased in 8 patients, and was unchanged in 1 patient. Thirteen patients (39%) had normal-sized CDs before and after cholecystectomy.
Group 3 patients demonstrated normal caliber ducts in 163 patients (84%) at baseline CT, and 155 patients (79%) at follow-up CT, at least 2 years later (Table 2).
The prior cholecystectomy group had a larger mean duct diameter than the other two groups at both baseline CT (p < 0.001) and follow-up CT (p < 0.001). Group 2 showed a greater increase in duct size than the other groups at follow-up (p < 0.001) (Table 2).
Regarding observer agreement, the two reader measurements were more concurrent with their measurements at the first and follow-up CTs in the remote cholecystectomy group (Group 1) (p < 0.0001). The difference between readers in the remote cholecystectomy group was 0.18 mm. When evaluating CD diameter in the interval cholecystectomy and nonoperated patients, reader 2 tended to measure the ducts’ mean to be 1.0 mm larger than reader 1 (p < 0.001). Although there was direct correlation between the two observers at both time points, a stronger correlation was present for the remote and interval cholecystectomy groups and a moderate correlation was observed between the rates for the nonoperated group. Variation in reader measurements, especially in NECT, may be related to uncertainty about CD wall margins. Also, despite the definitions and consensus before the readings were done, there may still be reader variability in the performance of CD diameter measurements. However, this difference in reader measurements is also found to be present in the real-life application of measuring the CD diameter in everyday patients.
Baseline central intrahepatic biliary dilation was significantly more common in the prior cholecystectomy group (14/48, 29%) than that in the interval cholecystectomy (3/33, 9%) or no cholecystectomy (5/191, 3%) groups (p < 0.001). Between the two readers, reader 1 was more likely to report intrahepatic biliary dilation at CT1 and CT2. However, there was a stronger inter-reader agreement with intrahepatic biliary dilation on CECT studies (p < 0.0001).
Frequency of CT visualization of the CD
The frequency of visualization of the suprapancreatic CD on either UECT or CECT at 5-mm intervals was evaluated in the group of 304 patients who underwent 608 examinations (Figs. 1, 2, 3, and 4). Overall, the CD was measureable in 89% of the CT studies using 5-mm slices, and was measureable much more often in contrast-enhanced relative to unenhanced studies (Fig. 5).
Relationship of CD diameter and age
In the stratification by age at first CT of the 191 non-cholecystectomy patients (group 3), the mean diameters of the CD in each age group at the first and follow-up CT are reported in Table 3. The mean interval between CT examinations was 3.81 ± 1.26 years. The average diameter of the CD was 5.07 mm. The CD diameters for men and women were 4.91 and 5.20 mm, respectively. There was a statistically significant correlation between CD size and increasing age (p < 0.001), but the absolute change was only 0.2–0.3 mm/decade.
Discussion
Common bile duct dilation in postcholecystectomy patients is often referenced as a normal finding in daily ultrasound and CT interpretations. Despite the common belief that CD dilation occurs after cholecystectomy, the normal expected postsurgical CD size continues to be debated without definitive evidence of dilation in asymptomatic patients. Current sonographic studies regarding CD diameter in post-cholecystectomy patients have yielded inconsistent findings [4–6, 12] and limited studies have compared the change in CD diameter in precholecystectomy and postcholecystectomy patients.
More recent studies with longer follow-up show minimal increases in bile duct size after cholecystectomy [2, 13]. Prior sonographic studies evaluating postcholecystectomy CD dilation included small patient numbers, did not evaluate for preexisting CD dilation, and included symptomatic patients with acute pancreaticobiliary disease or exploratory biliary surgery beyond routine cholecystectomy. In some prior studies, the imaging appearance itself contributed to the definition of abnormal or normal groupings. Furthermore, most of these studies had less than 2 years follow-up after cholecystectomy.
There is a paucity of available CT data regarding CD dilation. In a study by Senturk et al [14], the mean CD diameters in 46 patients with prior cholecystectomy were significantly greater than the age-matched control group. They hypothesized that an upper limit of 10 mm seemed appropriate for cholecystectomized subjects. In other studies, no significant change in CD diameters in patients after cholecystectomy was found [4, 5, 15, 16]. Since the CT is an outer wall–outer wall measurement juxtaposed to the inner wall–inner wall diameter by ultrasound, slightly larger diameters would be expected by CT, although this has not been studied to our knowledge.
Our study has several design advantages compared with prior evaluations. Patients with the possible influence of biliary tree-related pathology on CD diameter were excluded. Another advantage was a large number of nonoperated patients with long-term follow-up (greater than 2 years) were studied, providing a control group. Lastly, longitudinal CT evaluation for compensatory dilation of the CD in pre- and post-cholecystectomy patients has not been performed previously, to our knowledge.
Based on this study design, patients with prior cholecystectomy have larger CD diameters than the groups with no-cholecystectomy and interval-cholecystectomy by CT. The prior cholecystectomy patients (group 1) routinely had dilated CDs (>6 mm) at baseline and follow-up CT exams. Greater increase in duct diameter occurred between the two studies in the interval cholecystectomy patients relative to the other 2 groups, suggesting that dilation indeed occurs after cholecystectomy. Only 13 patients (39%) had normal-sized CDs before and after cholecystectomy, and dilated CDs were found in 7 patients (21%) before surgery and 22 patients (67%) postoperatively. This suggests that the extrahepatic biliary system that is normal before cholecystectomy will dilate in most cholecystectomized patients without clinical evidence of pancreaticobiliary disease, although the postoperative CD was only mildly dilated (mean duct size of 6.9 mm).
Continued technologic advances in CT have resulted in improved spatial resolution and improved ability to evaluate the biliary system. Current CT technology provides sufficient anatomic resolution to visualize the CD in most patients. However, visualization of the CD is more difficult in UECT studies. UECT does not allow one to differentiate the CD lumen from the wall. Visualization of the normal CD by CT has been reported in 30–66% of patients [8, 9, 17], and we are not aware of a more recent evaluation using more modern CT technology. Although one third of CDs were not visible by CT by previous reports, the ability of CT to evaluate the biliary system has markedly improved, as demonstrated by this study. Utilization of coronal reformatted images would be expected to improve evaluation of CD size even further, although these images were not used for measurement purposes in our study.
CT evaluation of CD dilation in patients without cholecystectomy over time is limited. There remains conflicting data regarding CD diameter as a function of age [18–21]. In our study recently published evaluating CD dilation in nonoperated patients with ultrasound [22], we demonstrated an increased duct size with the increasing age, although not clinically significant as the duct size remained within normal size limits. The CD diameter in the >70 years age group was slightly decreased at baseline (up to −0.5 mm) compared with the 50–59 and 60–69 years age groups. The cause of slightly decreased CD size in the oldest population is uncertain and may be related to small patient numbers. The overall trend suggests gradual CD dilation based on the data as a whole. A statistically significant direct correlation similarly exists between age and the CD diameter by CT measurements in patients without cholecystectomy, suggesting that the results are not technology specific to ultrasound. This study supports more recent research that the CD does dilate with the increasing age in asymptomatic nonoperated patients, although the duct size remains within normal size limits. A CD size of ≤6 mm in asymptomatic noncholecystectomized patients should be considered normal.
The clinical importance is substantial since patients with post-cholecystectomy CD dilation are more commonly identified as the usage of CT continues to increase, and these patients may undergo further invasive and noninvasive investigations. The morbidity of ERCP and the radiation dose associated with repeat CT exams and the additional costs of these examinations are difficult to justify in asymptomatic patients.
We believe that our results confirm that a larger CD diameter after remote cholecystectomy may be a normal finding and is commonly seen in patients with normal laboratory values, even up to 10 mm as previously suggested in the CT literature, despite some contrary data in the ultrasound literature. Therefore, in asymptomatic patients with remote cholecystectomy, a CD diameter of up to 10 mm should be considered normal. A slightly dilated CD (≤7 mm) in asymptomatic patients with interval cholecystectomy should also be considered normal. Bile duct dilation in patients after cholecystectomy may require no further evaluation when there is no laboratory or clinical signs of biliary obstruction. Second, although the CD does dilate with age, the change is small in nonoperated patients.
Further work in this area would include CT evaluation of CD diameter in asymptomatic cholecystectomized patients with long-term follow-up of substantially more than 2 years. Also, this study evaluated only one section of the CD. This may not reflect the overall CD diameter at multiple points. It would be useful to know whether another modality, such as MRCP, can lead to reliable CD measurements at multiple points and whether this would affect the conclusions reached in this study.
References
Oddi R (1887) D’une disposition a sphincter speciale de l’ouverture du canal choledoque. Arch Ital Biol 8:317–322.
Feng B, Song Q (1995) Does the common bile duct dilate after cholecystectomy? Sonographic evaluation in 234 patients. AJR 165(4):859–861.
Park SM, Kim WS, Bae IH, et al. (2012) Common bile duct dilatation after cholecystectomy: a 1-year prospective study. J Korean Surg Soc 83(2):97–101.
Mueller PR, Ferucci JT Jr, Simeone JF, et al. (1981) Postcholecystectomy bile duct dilatation: myth or reality? AJR 136(2):355–358
Puri SK, Gupta P, Panigrahi P, et al. (2001) Ultrasonographic evaluation of the common duct diameter in pre and post cholecystectomy patients. Trop Gastroenterol 22(1):23–24.
Skalicky M, Dajcman D, Hojs R (2002) Effect of cholecystectomy for gallstones on the surface of the papilla of Vater and the diameter of the common bile duct. Eur J Gastroenterol Hepatol 14(4):399–404.
Matcuk GR, Grant EG, Ralls PW (2014) Ultrasound measurements of the bile ducts and gallbladder: normal ranges and effects of age, sex, cholecystectomy, and pathologic states. Ultrasound Q 30(1):41–48.
Co CS, Shea WJ Jr, Goldberg HI (1986) Evaluation of common bile duct diameter using high resolution computed tomography. J Comput Assist Tomogr 10(3):424–427
Foley WD, Wilson CR, Quiroz FA, Lawson TL (1980) Demonstration of the normal extrahepatic biliary tract with computed tomography. J Comput Assist Tomogr 4(1):48–52.
Brant WE, Helms CA (2012) Fundamentals of Diagnostic Radiology, Fourth Edition. Philadelphia: Lippincott Williams & Wilkins, pp 934–935.
Parulekar SG (2002) Transabdominal sonography of bile ducts. Ultrasound Q 18:187–202.
Graham MF, Cooperberg PL, Cohen MM, Burhenne HJ (1980) The size of the normal common hepatic duct following cholecystectomy: an ultrasonographic study. Radiology 135:137–139.
Majeed AW, Johnson AG (1999) The preoperatively normal bile duct does not dilate after cholecystectomy: results of a 5 year study. Gut 45:741–743.
Senturk S, Miroglu TC, Bilici A, et al. (2012) Diameters of the common bile duct in adults and postcholecystectomy patients: a study with 64-slice CT. Eur J Radiol 81(1):39–42.
Kaim A, Steinke K, Frank M, et al. (1998) Diameter of the common bile duct in the elderly patient: measurement by ultrasound. Eur J Radiol 8(8):1413–1415.
Perret RS, Sloop GD, Borne JA (2000) Common bile duct measurements in an elderly population. J Ultrasound Med 19(11):727–730.
Schulte SJ, Baron RL, Teefey SA, et al. (1990) CT of the extrahepatic bile ducts: wall thickness and contrast enhancement in normal and abnormal ducts. AJR 154:79–85.
Bachar GN, Cohen M, Belenky A, Atar E, Gideon S (2003) Effect of aging on the adult extrahepatic bile duct. J Ultrasound Med 22:879–882.
Horrow MM, Horrow JC, Niakosari A, Kirby CL, Rosenberg HK (2001) Is age associated with size of adult extrahepatic bile duct: Sonographic study. Radiology 221:411–414.
Perrett RS, Sloop GD, Borne JA (2000) Common bile duct measurements in an elderly population. J Ultrasound Med 19:727–730.
Wu CC, Ho YH, Chen CY (1984) Effect of aging on common bile duct diameter: a real-time ultrasonographic study. J Clin Ultrasound 12:473–478.
McArthur TA, Planz V, Fineberg NS, et al. (2013) The common duct dilates after cholecystectomy and with advancing age: reality or myth? J Ultrasound Med 32(8):1385–1391.
Conflict of interest
The authors declare that they have no conflict of interest.
Disclosure
The authors have nothing to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
McArthur, T.A., Planz, V., Fineberg, N.S. et al. CT evaluation of common duct dilation after cholecystectomy and with advancing age. Abdom Imaging 40, 1581–1586 (2015). https://doi.org/10.1007/s00261-014-0308-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00261-014-0308-5