Abstract
Purpose
To determine whether radiation doses during computed tomography (CT) colonography (CTC) can be further reduced while maintaining image quality using model-based iterative reconstruction (MBIR).
Methods
Twenty patients underwent CTC at a standard dose in supine and prone positions and at a reduced dose in the supine position. All other scan parameters (except noise index) were held constant. Acquisitions were reconstructed using 3 algorithms: filtered back projection (FBP), adaptive statistical iterative reconstruction (ASIR), and MBIR. Noise was assessed quantitatively by comparing the SD in Hounsfield units at 5 standard locations. Qualitative assessment was made by 2 experienced radiologists blinded to technique who subjectively scored image quality, noise, and sharpness (from 0 to 4).
Results
The standard-dose and reduced-dose CT dose index/dose-length product were 6.7/328 and 2.7 mGy/129 mGy-cm, respectively (60 % reduction). Measured mean noise level increased from the standard to the reduced dose (FBP, from 58.6 to 97.2; ASIR from 35.8 to 60.6; and MBIR from 16.6 to 21.9). MBIR had significantly less noise than ASIR on 2-dimensional images at both standard and reduced doses (P < .01).
Conclusions
Radiation dose in CTC using MBIR can be reduced by 60 % while maintaining image quality and reducing image noise.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Computed tomography (CT) colonography (CTC) is a noninvasive technique for colon cancer screening. This technique is comparable to optical colonoscopy for detection of clinically significant polyps [1–3]. The potential risk from radiation exposure during CTC is an issue of public concern, and there is continued debate about it among medical professionals [4–7]. The potential health risk from low-dose radiation exposure (<10 millisievert [mSv]) is largely theoretical; estimates of cancer risk are based primarily on studies of Japanese atomic bomb survivors and are best described by the linear no-threshold model [8]. Our aim is to reduce the radiation dose during CTC as much as possible while maintaining image quality.
Traditionally, the radiation dose during CTC has been approximately one-half that associated with standard abdominal CT examinations [9, 10]. With the introduction of adaptive statistical iterative reconstruction (ASIR), radiation dose during CTC can be reduced by approximately 50 % (about 4 mSv), without loss of image quality [11]. Model-based iterative reconstruction (MBIR) is a sophisticated computationally intense algorithm with greater noise reduction than current software algorithms such as ASIR [12]. Thus, it is possible that MBIR may permit reduction of the radiation dose during CTC by reducing image noise and maintaining image quality.
We therefore investigated potential dose reduction and image quality implications during CTC using MBIR. We hypothesized that radiation dose during CTC can be further reduced by 60 % by reducing noise and maintaining image quality, compared to our current low-dose CT technique using ASIR.
Methods
Prior to the study, we obtained institutional review board approval and written informed patient consent, including consent for additional radiation dose, per HIPAA (Health Insurance Portability and Accountability Act) guidelines. Twenty patients scheduled for CTC between February 24, 2012 and November 5, 2012 were prospectively recruited. The ages of patients ranged from 53 to 81 years (mean, 65 years). Eleven patients were men; 9 were women. No colorectal polyps were visible in this patient group.
After cathartic colon preparation with stool tagging, all patients underwent standard CTC with supine and prone acquisitions at the standard dose and an additional supine acquisition at the reduced dose. The standard-dose acquisition was performed at 120 kilovolt (kVp), with the dose-modulation control indexed to 1.25-mm slice thickness and automatic tube current modulation turned on with a selected noise index of milliampere (mA) 65 (minimum mA 30; maximum mA 100). Reduced-dose acquisition was performed at 120 kVp, with the dose-modulation control indexed to 1.25-mm slices and automatic mA parameters of noise index set at 70 (minimum mA 30; maximum mA 100) for the expected reduction in radiation dose of 60 %. All CTC examinations were performed on a 64-multidetector CT (MDCT) scanner (Discovery CT750 HD, GE Healthcare). Patient preparation and mechanical insufflation techniques were the same as those described for the National CT Colonography Trial [13].
All 20 patients had 3 scans: standard-dose CTC in the supine and prone positions and reduced-dose CTC in the supine position only. Images from both of the supine acquisitions were reconstructed with filtered back projection (FBP), ASIR (70 %), and MBIR. Duration of the reconstruction using MBIR was approximately 1 h per patient per acquisition (2 h total per patient), with real-time reconstruction using ASIR.
Quantitative assessment
Image noise was recorded by selecting a region of interest (≤1,600 mm2) in 5 standard locations in each patient and recording the SD. The 5 locations were posterior right hepatic lobe, right lower pole kidney, right psoas, left psoas, and aorta at the level of the lower pole of the right kidney. Image noise was measured at both the standard dose and the reduced dose for each reconstruction algorithm. Body mass index (BMI [weight in kg divided by height in m2]) was calculated using the measured height and weight of the patient from the medical record.
Qualitative assessment
Qualitative assessment was performed in the same manner as described by Flicek et al [11]. Two experienced CTC radiologists reviewed the image data (>500 proven cases) for the study in a blinded fashion on an advanced workstation (GE AW 4.3_05, CTC software version Voxtool 6.12.3; GE Healthcare). Axial 0.625-mm thick images were used for the 2-dimensional scoring. The 2 readers independently recorded their scores after previewing 4 test cases, discussing the ratings, and agreeing on how to determine the ratings. Both readers reviewed the same images. The images were standardized to be reviewed by colon location, with randomized assessment of CT technique.
For each patient, the 2 readers evaluated image quality, noise, and sharpness assessments at 3 similar sites in the colon: at the ileocecal valve, at a prominent fold in the rectosigmoid junction, and at the splenic flexure. These sites allowed assessment of the technique for a simulated lesion (ileocecal valve) and in areas with potential beam hardening (rectosigmoid within bony pelvis) and without potential beam hardening (splenic flexure).
The 2 readers graded image quality (both 2-dimensional and 3-dimensional images) on a 5-point scale, ranging from 0 (nondiagnostic) to 4 (well seen without artifacts and with high confidence of detecting a colorectal lesion ≥5 mm). A score of 1 indicated severe artifact with low confidence; 2 indicated moderate artifact or moderate diagnostic confidence; and 3 indicated mild artifact or high confidence.
The 2 readers graded image noise using a 5-point scale from 0 (nondiagnostic) to 4 (no perceptible noise). A score of 1 indicated severe noise; 2 indicated moderate perceptible noise; and 3 indicated mild perceptible noise.
The 2 readers used a 5-point scale to assess image sharpness by evaluating the aortic contour in the upper abdomen. A score of 0 indicated nondiagnostic; 1 indicated poorly defined edge sharpness; 2 indicated moderately unsharp edges; 3 indicated mildly unsharp edges; and 4 indicated very sharp edges.
Statistical analysis
Quantitative noise was calculated as the mean of the SD measured at the 5 locations listed previously. Quantitative noise was compared between the standard-dose image and the reduced-dose image for each reconstruction algorithm (FBP, ASIR, and MBIR).
The subjective scores of each reader were averaged for aortic sharpness, overall quality, and noise. For each algorithm, scores were averaged for both the 2-dimensional and the 3-dimensional images at the standard dose and at the reduced dose, except that aortic sharpness was not evaluated on the 3-dimensional images. The mean scores of both readers were compared between the standard-dose image and the reduced-dose image at each location and overall for each reconstruction algorithm. The clinical significance for qualitative assessments of image noise and quality was considered to be a difference in score ≥1. The intraclass correlation coefficient was calculated to measure the interobserver agreement between image noise and quality at the standard dose and at the reduced dose. A correlation of ≥0.7 was considered excellent, 0.3 to 0.7 was considered good, and <0.3 was considered poor.
Qualitative scores were also analyzed using mixed-effect models. For each mixed-effect model, we included fixed effects for method (FBP vs ASIR vs MBIR), for dose (standard vs reduced), for location (rectosigmoid junction vs splenic flexure vs ileocecal valve), and for reader. Random effects allow covariance to vary due to subject. Post hoc pairwise comparisons were conducted to compare means for subgroups of different dose and method combinations (adjustment for multiple testing used the Tukey method).
The statistical software program SAS 9.2 (SAS Institute Inc) was used for data analysis, and statistical significance was defined as P ≤ .05.
Results
Patient validation
Table 1 summarizes the study results. Averaged data for all 20 patients, as well as by group per BMI (<30 and ≥30), are shown for illustrative purposes.
Radiation dose
The dose-length product (DLP) was recorded for each patient during the standard-dose and reduced-dose acquisitions. For comparison purposes, the DLP was then used to estimate the effective dose using the International Commission on Radiological Protection publication 60 conversion coefficients, although this method may underestimate the actual effective dose [14]. The standard-dose CT dose index was 6.7 mGy and the DLP was 327.8 mGy-cm, with an estimated effective dose of 4.9 mSv. The reduced-dose CT dose index was 2.7 mGy and the DLP was 129.1 mGy-cm, with an estimated effective dose of 1.9 mSv. The reduced dose was therefore approximately 61 % lower than the standard dose.
Quantitative assessment
For FBP, quantitative noise at the standard dose was 58.6, increasing to 97.2 at the reduced dose for all patients. For ASIR, quantitative noise at the standard dose was 35.8, increasing to 60.6 at the reduced dose. For MBIR, quantitative noise at the standard dose was 16.6, increasing to 21.9 at the reduced dose. There was a statistically significant reduction in noise on images reconstructed with MBIR compared to that with ASIR at both the standard dose and the reduced dose (P < .001).
Qualitative assessment
There were no differences >1 in mean subjective scores for overall image quality and sharpness among standard-dose ASIR, standard-dose FBP, and reduced-dose MBIR. Mean subjective score differences >1 did exist for noise and sharpness as discussed in the following section.
2-Dimensional image scores
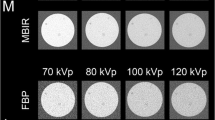
Overall, 2-dimensional image quality for FBP, ASIR, and MBIR at standard dose/reduced dose was 3.9/3.7, 4.0/3.9, and 4.0/4.0, respectively; there was no significant difference in image quality between ASIR and MBIR. Table 2 summarizes the mean differences in scores among standard-dose ASIR, standard-dose FBP, and reduced-dose MBIR on 2-dimensional images. There was significantly less subjective noise on 2-dimensional images using MBIR at the reduced dose than with standard-dose ASIR and FBP (mean difference between reduced-dose MBIR and standard-dose FBP is >1). No significant difference in sharpness or image quality was found among reduced-dose MBIR, standard-dose ASIR, and standard-dose FBP. There was also no significant difference in subjective noise or image quality between images reconstructed with MBIR at the standard dose and those at the reduced dose (Fig. 1).
Axial images for comparison of standard-dose and reduced-dose computed tomography colonography techniques at level of ileocecal valve. A–C Standard-dose 2D images using FBP, ASIR, and MBIR. D–F Reduced-dose 2D images using FBP, ASIR, and MBIR. There is noticeably less noise on the MBIR images (C and F) without loss of image quality. G and H, Standard-dose 3D images using FBP and ASIR. I Reduced-dose 3D image using MBIR. Images G–I are comparable; slightly increased image artifact with reduced-dose MBIR (mucosal nodularity) is noted but does not significantly degrade image quality. The arrow on the 2D images is the location and direction of view for the 3D camera only.
3-Dimensional image scores
Subjective noise on 3-dimensional images was slightly higher on reduced-dose MBIR than on standard-dose FBP (P = .02) (Table 3). There was no statistically significant difference in subjective noise between reduced-dose MBIR and standard-dose ASIR (P = .99). There was no statistically significant difference in subjective 3-dimensional image quality between reduced-dose MBIR and standard-dose ASIR (P = .73) or standard-dose FBP (P = .81) (Fig. 1).
BMI
Evaluation by patient size is limited because of the small number of patients (10 with BMI <30 and 10 with BMI ≥30). BMI averaged 27 for this cohort. When BMI was added to the mixed-effects model, it was only significant for aortic sharpness (P < .001). BMI did not significantly affect mean subjective scores for noise or image quality.
Interobserver agreement
Interobserver agreement was generally good to excellent. The intraclass correlation coefficient values between readers for 2-dimensional image standard-dose noise, reduced-dose noise, standard-dose quality, and reduced-dose quality were 0.86 (95 % CI 0.81–0.89), 0.85 (0.79–0.89), 0.07 (−0.25 to 0.31), and 0.45 (0.26–0.59), respectively.
The intraclass correlation coefficient values between readers for 3-dimensional image standard-dose noise, reduced-dose noise, standard-dose quality, and reduced-dose quality were 0.68 (95 % CI 0.57–0.76), 0.43 (0.23–0.57), 0.46 (0.28–0.60), and 0.35 (0.13–0.52), respectively.
Discussion
In this study, additional radiation dose reductions of up to 60 % were found to be possible during CTC using MBIR without loss of image quality. In addition, image noise was significantly reduced using MBIR. Interestingly, the trend of slightly higher-quality scores in smaller patients noticed during the ASIR pilot study [11] was not repeated in the current study. Furthermore, BMI did not significantly affect image noise or quality. In fact, in many instances, scores were slightly higher in larger patients than in smaller patients. This finding is most likely due to the use of automated exposure control, resulting in higher-quality images in larger patients; the ASIR pilot study was performed using manual exposure control. Nevertheless, both large and small patients experienced >60 % radiation dose reduction with MBIR than with the standard dose (63 % for patients with BMI ≥30 and 67 % for patients with BMI <30).
Several other studies using MBIR have shown similar findings. Pickhardt et al [15] reported preliminary study results showing a mean radiation dose reduction of 74 % during routine abdominal CT examinations using reduced-dose MBIR over standard-dose ASIR while maintaining image quality. Yoon et al [16] compared FBP, ASIR, and MBIR at different radiation doses using porcine colon phantoms and showed that both ASIR and MBIR images had less noise and image quality comparable to that of FBP at the same radiation dose. Furthermore, Katsura et al [17] demonstrated that MBIR during chest CT can reduce radiation dose nearly 80 % without sacrificing nodule detectability.
The inherent noise reduction achieved with MBIR may complement other radiation dose-reduction techniques. Chang et al [18] demonstrated a 16 % decrease in DLP during CTC by decreasing the kVp from 120 kVp to 100 kVp; however, noise increased by 32 %. MBIR may complement such techniques, allowing for synergistic radiation dose reductions while preserving image quality.
The reconstruction time required for MBIR can add as much as 1 h per acquisition (2 h per examination). Currently, this additional time requirement could create a work flow delay that could prove disruptive to current radiology practices. For CTC examinations, the additional 2 h for a reconstruction would not be acceptable if patients were waiting for same-day colonoscopy (if a polyp was detected at CTC). Patients not requiring a same-day examination procedure could take advantage of the radiation reduction available with MBIR. In lieu of the limited number of examinations that can be reconstructed per day on a single MBIR computer system, CT examinations could be prioritized. Since CTC examinations are already considered low dose when ASIR is used, should higher-dose procedures be triaged for reconstruction using a lower-dose protocol, for even more radiation savings? Furthermore, should examinations for younger patients who are more susceptible to the effects of radiation be prioritized for MBIR reconstructions? Our study did not address these work flow and ethical issues. However, further evaluation and discussion should facilitate community and practice consensus. Our hope is that technical advances will increase the throughput speed with MBIR, so that every patient will benefit from its utilization.
This study had several limitations. First, there was no optical colonoscopy reference standard. Thus, we cannot assess the diagnostic performance of reduced-dose CTC using MBIR. However, given the preserved image quality, it follows that accuracy would be maintained, although additional studies are needed. Second, while interobserver agreement was generally good, image-quality measurements are subjective; additional or different readers may have produced different results. Third, the small number of patients (N = 20) in this study precludes the widespread application of our findings, but if our findings and their diagnostic accuracy could be verified by future studies with more participants, it would validate them. Finally, our average dose of 6.7 mGy was higher than expected, likely due to an average BMI of 27 for this study population.
In conclusion, our findings show that additional radiation dose reductions exceeding 60 % during CTC are possible with MBIR, while maintaining overall image quality and reducing noise. Additional evaluation to verify diagnostic accuracy is warranted.
Abbreviations
- ASIR:
-
Adaptive statistical iterative reconstruction
- BMI:
-
Body mass index (weight in kg divided by height in m2 [kg/m2])
- CT:
-
Computed tomography
- CTC:
-
Computed tomography colonography
- DLP:
-
Dose-length product
- FBP:
-
Filtered back projection
- HIPAA:
-
Health Insurance Portability and Accountability Act
- kVp:
-
Kilovolts peak
- mAs:
-
Milliamperes-second
- MBIR:
-
Model-based iterative reconstruction
- MDCT:
-
Multidetector computed tomography
- mSv:
-
Millisievert
References
Pickhardt PJ, Hassan C, Halligan S, Marmo R (2011) Colorectal cancer: CT colonography and colonoscopy for detection: systematic review and meta-analysis. Radiology 259(2):393–405
Regge D, Laudi C, Galatola G, et al. (2009) Diagnostic accuracy of computed tomographic colonography for the detection of advanced neoplasia in individuals at increased risk of colorectal cancer. JAMA 301(23):2453–2461
Levin B, Lieberman DA, McFarland B, et al. (2008) Screening and surveillance for the early detection of colorectal cancer and adenomatous polyps, 2008: a joint guideline from the American Cancer Society, the US Multi-Society Task Force on Colorectal Cancer, and the American College of Radiology. CA Cancer J Clin 58(3):130–160
Friedel DM, Iqbal S, Stavropoulos SN, et al. (2012) Evolving role of computed tomographic colonography in colon cancer screening and diagnosis. South Med J. 105(10):551–557
Perisinakis K, Seimenis I, Tzedakis A, et al. (2012) Screening computed tomography colonography with 256-slice scanning: should patient radiation burden and associated cancer risk constitute a major concern? Invest Radiol. 47(8):451–456
Brenner DJ, Georgsson MA (2005) Mass screening with CT colonography: should the radiation exposure be of concern? Gastroenterology 129(1):328–337
Berrington de Gonzalez A, Kim KP, Knudsen AB, et al. (2011) Radiation-related cancer risks from CT colonography screening: a risk-benefit analysis. AJR Am J Roentgenol 196(4):816–823
Verdun FR, Bochud F, Gundinchet F, et al. (2008) Quality initiatives radiation risk: what you should know to tell your patient. Radiographics 28(7):1807–1816
Hara AK, Johnson CD, Reed JE, et al. (1997) Reducing data size and radiation dose for CT colonography. AJR Am J Roentgenol 168(5):1181–1184
van Gelder RE, Venema HW, Serlie IW, et al. (2002) CT colonography at different radiation dose levels: feasibility of dose reduction. Radiology 224(1):25–33
Flicek KT, Hara AK, Silva AC, et al. (2010) Reducing the radiation dose for CT colonography using adaptive statistical iterative reconstruction: a pilot study. AJR Am J Roentgenol 195(1):126–131
Thibault JB, Sauer KD, Bouman CA, Hsieh J (2007) A three-dimensional statistical approach to improved image quality for multislice helical CT. Med Phys 34(11):4526–4544
Johnson CD, Chen MH, Toledano AY, et al. (2008) Accuracy of CT colonography for detection of large adenomas and cancers. N Engl J Med. 359(12):1207–1217 (Erratum in: N Engl J Med. 2008;359(26):2853)
Christner JA, Kofler JM, McCollough CH (2010) Estimating effective dose for CT using dose-length product compared with using organ doses: consequences of adopting International Commission on Radiological Protection publication 103 or dual-energy scanning. AJR Am J Roentgenol. 194(4):881–889 (Erratum in: AJR Am J Roentgenol. 2010;194(5):1404)
Pickhardt PJ, Lubner MG, Kim DH, et al. (2012) Abdominal CT with model-based iterative reconstruction (MBIR): initial results of a prospective trial comparing ultralow-dose with standard-dose imaging. AJR Am J Roentgenol. 199(6):1266–1274
Yoon MA, Kim SH, Lee JM, et al. (2012) Adaptive statistical iterative reconstruction and Veo: assessment of image quality and diagnostic performance in CT colonography at various radiation doses. J Comput Assist Tomogr. 36(5):596–601
Katsura M, Matsuda I, Akahane M, et al. (2013) Model-based iterative reconstruction technique for ultralow-dose chest CT: comparison of pulmonary nodule detectability with the adaptive statistical iterative reconstruction technique. Invest Radiol. 48(4):206–212
Chang KJ, Caovan DB, Grand DJ, Huda W, Mayo-Smith WW (2013) Reducing radiation dose at CT colonography: decreasing tube voltage to 100 kVp. Radiology. 266(3):791–800 (Epub 2012 Dec 21)
Ethical Statement
This study conformed to current US laws. Before the study was conducted, institutional review board approval was obtained and documented, and informed consent was obtained from patients per the guidelines of the Health Insurance Portability and Accountability Act.
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Millerd, P.J., Paden, R.G., Lund, J.T. et al. Reducing the radiation dose for computed tomography colonography using model-based iterative reconstruction. Abdom Imaging 40, 1183–1189 (2015). https://doi.org/10.1007/s00261-014-0271-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00261-014-0271-1