Abstract
The purpose of this study was to prospectively compare the efficacy and controllability of pushable coil and detachable coil during embolization of gastroduodenal artery (GDA) while performing percutaneous implantation of port-catheter system for hepatic artery infusion chemotherapy. Fifty patients (M:F = 42:8, age: 31–81 years) with advanced hepatocellular carcinoma undergoing port-catheter system implantation were randomized into pushable coil group and detachable coil group. During catheter fixation, GDA was embolized as close to the origin as possible. Success rate, number of coils used, number of coils removed due to malposition after deployment, time to occlusion, uncoiled GDA length, pushability, and complications were compared. Pushability was graded as no tension, slight tension, and difficult to advance. Embolization was successful in 49 patients. One failure resulted from repeated regurgitation of pushable coil into hepatic artery. Number of coils used and removed coils, time to occlusion, and uncoiled GDA length were 1–3 (mean 2.32), 5 coils in 3 patients, 4–20 min (mean 8.00), and 0–15.0 mm (mean 3.36) in pushable coil group, and 1–5 (mean 2.12), 2 coils in 2 patients, 2–15 min (mean 7.40), and 0–10.2 mm (mean 2.92) in detachable coil group, respectively, without significant difference. Pushability was no tension (n = 24) and slight tension (n = 1) in pushable coil group and no tension (n = 16), slight tension (n = 7), and difficult to advance (n = 2) in detachable coil group. One hepatic artery dissection occurred in the failed case during coil removal. Pushable coils and detachable coils had similar efficacy and controllability during GDA embolization, although there was a trend favoring detachable coil.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Since the first introduction of Gianturco coil [1], various coils have been introduced and are in use for transcatheter embolization of vascular lesions. There are two systems of coil deployment, which are pushable coil and detachable coil. The pushable coil has the advantage in cost-effectiveness and is simple to use, but has the disadvantage that the coil cannot be retrieved once deployment has begun. When deployed inappropriately, the coil has to be removed. On the contrary, the detachable coil has the advantage that the coil can be retrieved when inappropriately placed. The interlock IDC coil (Boston Scientific, Natick, USA) is a platinum coil with thrombogenic fibers, which has mechanical detachable system. Embolization of GDA, vascular communications in congenital heart disease, and renal AVM using the interlock IDC coil has been reported [2–4].
Hepatic artery infusion chemotherapy using the percutaneously implanted port-catheter system is one of the last resort treatments for unresectable, advanced hepatocellular carcinoma [5–8]. During implantation of the port-catheter system, the catheter tip is commonly inserted into the gastroduodenal artery (GDA) followed by coil embolization of the GDA for stabilization of the catheter [9–11].
The purpose of this study was to prospectively compare the efficacy and controllability of the detachable coil (interlock IDC coil; Boston Scientific) and the pushable coil (micro-nester coil; Cook, Bloomington, USA) during embolization of GDA while performing percutaneous implantation of port-catheter system for hepatic artery infusion chemotherapy.
Materials and methods
Patient population
This prospective study was approved by the institutional review board, and written informed consent for the procedure and enrollment in the study was obtained from all patients. All procedures performed were in accordance with the guidelines of the institution.
From December 2011 to November 2012, 50 patients with unresectable, advanced hepatocellular carcinoma undergoing percutaneous port-catheter implantation for hepatic artery infusion chemotherapy were randomized into pushable coil group and detachable coil group using permuted block randomization, and were enrolled in the study. On referral of percutaneous port-catheter system implantation, the study was explained to the patient on the day before the procedure. On the day of procedure when the patient was willing to participate in the study, written informed consent was obtained. The results of permuted block randomization were not informed to the operator until the GDA was selected for embolization. Only after selection of the GDA using a microcatheter, the operator was informed of which coil to be used for embolization of GDA. In all patients, only the coils determined by the permuted block randomization were used. The patients were 42 men and 8 women with ages ranging from 31 to 81 years (mean 58.0 ± 11.8 years).
Criteria for inclusion in the study were any patient over 20 years of age undergoing percutaneous hepatic artery port-catheter implantation for unresectable, advanced hepatocellular carcinoma. Exclusion criteria were patient who cannot give permission or refuse to be enrolled in the study, previous history of hepatic surgery, significant hepatic artery variation on CT/MRI, port catheter fixation in artery other than GDA or its branches, reversed flow in the GDA, and Child-Pugh class C patients. During the case collection period, 85 patients were excluded, and were due to the significant hepatic arterial variation and/or previous history of hepatic surgery in 52, reversed flow in GDA in 25, the patients’ refusal in 6 patients, and Child-Pugh class C in 2 patients.
Procedure of percutaneously port-catheter system implantation
All procedures of percutaneous port-catheter system implantation were performed in the angiography suites by one interventional radiologist to minimize any possible inter-operator bias. The procedures were performed as follows:
-
1.
After sterile preparation, the femoral artery was accessed under ultrasonography guide, and a 5F angiography catheter (Yashiro; Terumo, Tokyo, Japan or RH-R; Cook) was inserted. All patients underwent angiography of superior mesenteric artery, celiac artery, hepatic artery, and any possible extra-hepatic collateral artery for road mapping of the feeders of hepatocellular carcinoma.
-
2.
When present, a microcatheter was inserted coaxially, and transcatheter arterial chemo-embolization was performed for extra-hepatic collateral feeders of the main tumor.
-
3.
Non-hepatic arterial branches originating from the hepatic artery were also embolized using Vortex coils (Boston Scientific) or Tornado coils (Cook) of appropriate size.
-
4.
Percutaneous implantation of the port-catheter system (Healthport LP set; Baxter Healthcare, Deerfield, USA) was performed immediately after angiography and/or chemo-embolization. According to the celiac and common hepatic angiograms, location of the tip of the port catheter was determined: in the GDA, a branch of GDA or gastroepiploic artery. A side-hole was made using a sterile scissor so as the side-hole was located at distal common hepatic artery.
-
5.
A 0.035 inch hydrophilic guide wire (Radiofocus; Terumo) was used to select the artery in which the tip of the port catheter was determined to be placed, and the angiography catheter was exchanged to the port catheter. The port catheter was positioned so as the side-hole was located at distal common hepatic artery.
-
6.
A microcatheter was inserted coaxially, and was passed through the side-hole of the port catheter. The GDA was selected and was embolized using either the micro-nester coil (Cook) or the interlock IDC coil (Boston Scientific), as predetermined by the permuted block randomization. The diameter of the coil used was determined as 100–150 % of the diameter of GDA.
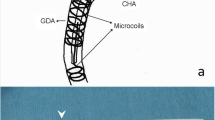
Coil embolization was performed so as the proximal-most location of the coil mass was located as close to the origin of the GDA as possible (Fig. 1). To confirm occlusion of GDA, the microcatheter was retrieved to the proximal-most level of the coil mass and angiography was performed. When flow in the GDA decreased, angiography was repeated in 1 min interval until occlusion. When flow in the GDA persisted without change, additional coiling was performed. Coiling was repeated until complete occlusion of GDA was confirmed by angiography.
Fig. 1 Images of a 78-year-old male with hepatocellular carcinoma in right lobe of liver. A Portal venous phase image of contrast-enhanced CT reveals the large hepatocellular carcinoma replacing near entire right lobe of liver with tumor thrombosis in right portal vein. B Common hepatic arteriography reveals the huge hypervascular tumor staining. C Spot radiography obtained after embolization of the gastroduodenal artery using interlock IDC coil. The tip of the port catheter is located within the distal gastroepiploic artery. D Final port-catheter angiography reveals the coil embolized to the level of origin of gastroduodenal artery.
-
7.
The proximal segment of the port catheter was embedded in the subcutaneous tunnel, and surplus length of the catheter was cut off. Then the port catheter was connected to the port chamber, which was implanted in the subcutaneous fat layer of abdominal wall. Port-catheter angiography was performed to confirm final location of the side-hole.
Definition and statistics
Technical success was defined as successful implantation of the port-catheter system for hepatic artery infusion chemotherapy with occlusion of the GDA by coil embolization.
The success rate and complications were compared between the two groups. The angiograms were reviewed and analyzed to compare the pushable coil group and detachable coil group with parameters of number of coils used for occlusion of GDA, number of coils removed after deployment due to regurgitation into the hepatic artery, time to occlusion of GDA, the shortest distance from origin of GDA to proximal-most part of the coil mass, and pushability of the coil. Pushability of the coil was measured in 3 grades of no tension, slight tension, and difficult to advance. The one interventional radiologist who performed the procedures graded the pushability immediately after the procedure. Angiograms obtained during needling the port-catheter system for chemotherapy and medical records were reviewed for evaluation of follow-up results of the port-catheter system and clinical results of treatment. Survival rates were obtained by Kaplan–Meier survival analysis. All statistics were performed using SPSS 22.0 for windows (SPSS Inc, Chicago, USA). The parameters were compared using χ 2 test. Mean values are provided as mean ± SD.
Results
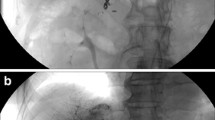
Coil embolization was successful in 49 patients, in 24 patients (96 %) in the pushable coil group and in 25 patients (100 %) in the detachable coil group. One failure resulted in the pushable coil group due to continuous regurgitation of the coil into the hepatic artery (Fig. 2).
Images of a 60-year-old male with hepatocellular carcinoma in left lobe of liver. A, B Portal venous phase images of contrast-enhanced MR reveal the hepatocellular carcinoma in left lateral segment with tumor thrombosis in left portal vein and bile duct invasion. C Image obtained during embolization of gastroduodenal artery using micro-nester coil. The proximal segment of the coil continuously regurged back into the hepatic artery, and was removed. Dissection of the proper hepatic artery occurred during removal. D Follow-up angiography after port-catheter system implantation via left subclavian artery reveals dissection in the proper hepatic artery, occluding right hepatic artery.
The results comparing pushable coil and detachable coil are provided in Table 1. There was no statistically significant difference between the pushable coil and detachable coil in the number of coil used for embolization, time to occlusion of GDA, and the length of uncoiled segment of GDA, although there was a trend favoring detachable coil. During the procedures, 5 coils in 3 patients of the pushable coil group and 2 coils in 2 patients of the detachable coil group were removed using micro-snare due to regurgitation into the hepatic artery after deployment. The pushability of the pushable coil was no tension (n = 24) and slight tension (n = 1), whereas the pushability of detachable coil was no tension (n = 16), slight tension (n = 7), and difficult to advance (n = 2). One complication of hepatic artery dissection occurred in the failed patient with coil regurgitation into the hepatic artery during removal (Fig. 2).
The patients underwent 0 to 15 sessions (mean 5.7 ± 3.8) of intra-arterial chemotherapy after 0 to 15 sessions (mean 5.1 ± 4.0) of port needling and follow-up angiography in the angiography suite. Follow-up angiograms revealed mild port catheter migration but with maintained main flow to the liver in 4 (16 %), port occlusion in 1, and recanalized GDA flow in 1 patient in the pushable coil group, and mild port catheter migration in 1, port occlusion in 1, and hepatic artery occlusion in 1 patient in the detachable coil group.
In 5 patients, complete remission could be achieved after down staging and hepatic resection in 4 and liver transplantation in 1 patient, although 1 patient expired during follow-up due to sepsis. In 11 patients with clinically stable disease, 1 patient is still under treatment, 8 patients expired due to complications of cirrhosis, 1 patient expired due to pneumonia, and 1 patient was transferred to other institution for treatment. In 34 patients with clinically progressed disease, 2 patients are still under treatment, 30 patients expired due to progression of the hepatocellular carcinoma, and 2 patients expired due to sepsis. The 6-month and 1-year survival rates were 76 % and 43.5 %, respectively.
Discussion
Coil embolization is one of the essential interventional procedures in treatment of various vascular lesions including embolization of injured vessel by trauma, arteriovenous fistula and malformation, congenital vascular lesion, and aneurysm of various organs. Along with n- butyl cyanoacrylate glue, coil is also one of the most commonly used embolic materials while performing percutaneous implantation of port-catheter system for hepatic artery infusion chemotherapy.
During percutaneous implantation of port-catheter system, the tip of the indwelling catheter is fixed in a branch artery to lower the rate of catheter dislodgement and hepatic artery obstruction [9–11]. Use of the micro-nester coil in catheter fixation during port-catheter implantation has been reported [12]. Using the micro-nester coil, the mean number of coils used for fixation could be decreased from 4.2 to 2.5, and use of n-butyl cyanoacrylate-lipiodol glue could be decreased considerably. In our study, the mean numbers of coil used were 2.32 ± 0.56 in the micro-nester coil group, and 2.12 ± 0.83 in the interlock IDC coil group, without using n-butyl cyanoacrylate-lipiodol glue. Occlusion of GDA could be obtained with comparable number of coils used, but without additional glue embolization. In our study, the coils were positioned as close to the origin of GDA as possible, which may have increased the packing density and subsequently resulted in GDA occlusion with similar number of coils without adding glue embolization.
The GDA should be occluded as close to the origin as possible to prevent recanalization of the GDA [13] and to prevent flow of the chemotherapeutic agent to the pancreaticoduodenal branches. Recanalization of the GDA after coil embolization occurred in over 20 % of patients undergoing percutaneous port-catheter system implantation or 90Y radioembolization [13]. In these patients, mean distance from origin of GDA to the proximal-most coil mass was 12.6 mm in the recanalized group, whereas it was 9.6 mm in the occluded group. Mean distance from the origin of GDA to proximal-most coil mass of 3.36 ± 3.38 mm in the micro-nester coil and 2.92 ± 2.48 mm could be achieved in our study by intentionally coiling as close to the origin of GDA as possible. Although the distance from the origin of GDA to the coil mass was sufficiently short in both groups to prevent recanalizaton, and the difference was statistically insignificant, there was a trend favoring the interlock IDC coil as repositioning of the coil was possible.
The interlock IDC coil is a mechanically detachable coil by interlocking arm mechanism which can provide controlled delivery. The position of the coil, stability, and packing density can be controlled during the deployment procedure by repeated retrieval and repositioning, until optimally positioned. The interlock coil is potentially a useful device when precise positioning of the coil is required. Although our study failed to prove statistically significant benefit compared to the micro-nester coil, there was a trend favoring the interlock IDC coil in the number of coils required for occlusion, time to occlusion, and precise positioning of the coil.
Although with some advantages, the interlock IDC coil also has some disadvantages. Unless the interventional radiologist is familiar with the other detachable coils which are commonly used in neurointerventional procedure, some learning curve is anticipated. Secondly, as the introducer sheath of the coil is tapered to avoid premature deployment, the tip of the introducer sheath may collapse when tension is given toward the hub of the microcatheter. As a result, the interlock IDC coil may not advance into the microcatheter. Thirdly, the coil and the delivery wire were relatively rigid and difficulty in advancing the coil through the microcatheter was occasionally encountered as in two of the cases in detachable coil group of our study. Subsequently in cases when acute angulation of the celiac artery was anticipated, the 5F angiography catheter was advanced to distal common hepatic artery to overcome the rigidity. And lastly, the relatively higher cost is another disadvantage of the interlock IDC coil. The list price of the micro-nester coil suggested by the manufacturer is $145, where as the list price of the interlock IDC coil ranges $400 to $1,150 according to the length of the coil. Including the coils retrieved due to inappropriate positioning after deployment, the cost of coils used for the patients included in our study ranged $145 to $435 (mean $319 ± 72.5) in the micro-nester coil group, whereas the cost ranged $400 to $3,000 (mean $1,168 ± 518.6) in the interlock IDC coil group.
In conclusion, the micro-nester coil and the interlock IDC coil were similar in the number of coils required for occlusion, time to occlusion, and precise positioning of the coil, although there was a trend favoring detachable coil. Detachable coil has the merit of easy retrieval when coil position is inappropriate and avoid unnecessary removal procedure.
References
Gianturco C, Anderson JH, Wallace D (1975) Mechanical devices for arterial occlusion. Am J Roentgenol Radium Ther Nucl Med 124:428–435
Dudeck O, Bulla K, Wieners G, et al. (2011) Embolization of the gastroduodenal artery before selective internal radiotherapy: a prospectively randomized trial comparing standard pushable coils with fibered interlock detachable coils. Cardiovasc Intervent Radiol. 34:74–80
Seltzer S, Aboulhosn J, Levi DS (2009) Use of interlock fibered detachable coils for occlusion of collaterals, coronary artery fistulae, and patent ductus arteriosus. Catheter Cardiovasc Interv. 74:770–776
Han YM, Song SK, Hwang HP, et al. (2013) Large congenital renal arteriovenous malformation treated with interlock coil embolization. Vasc Med. 18:237–238. doi:10.1177/1358863X13494260
Miyaki D, Aikata H, Honda Y, et al. (2012) Hepatic arterial infusion chemotherapy for advanced hepatocellular carcinoma according to Child-Pugh classification. J Gastroenterol Hepatol 27:1850–1857
Ikeda M, Okusaka T, Furuse J, et al. (2013) A multi-institutional phase II trial of hepatic arterial infusion chemotherapy with cisplatin for advanced hepatocellular carcinoma with portal vein tumor thrombosis. Cancer Chemother Pharmacol 72:463–470
Lorenz M, Müller HH (2000) Randomized, multicenter trial of fluorouracil plus leucovorin administered either via hepatic arterial or intravenous infusion versus fluorodeoxyuridine administered via hepatic arterial infusion in patients with nonresectable liver metastases from colorectal carcinoma. J Clin Oncol 18:243–254
Allen-Mersh TG, Earlam S, Fordy C, Abrams K, Houghton J (1994) Quality of life and survival with continuous hepatic-artery floxuridine infusion for colorectal liver metastases. Lancet 344:1255–1260
Shindoh N, Ozaki Y, Kyogoku S, et al. (1999) Stabilization of a percutaneously implanted port catheter system for hepatic artery chemotherapy infusion. Cardiovasc Intervent Radiol 22:344–347
Tanaka T, Arai Y, Inaba Y, et al. (2003) Radiologic placement of side-hole catheter with tip fixation for hepatic arterial infusion chemotherapy. J Vasc Interv Radiol 14:63–68
Yamagami T, Iida S, Kato T, et al. (2002) Using n-butyl cyanoacrylate and the fixed-catheter-tip technique in percutaneous implantation of a port-catheter system in patients undergoing repeated hepatic arterial chemotherapy. AJR 179:1611–1617
Yamagami T, Kato T, Hirota T, et al. (2008) Value of micronester coils in port-catheter implantation for continuous hepatic arterial infusion chemotherapy with fixed catheter tip method. Eur Radiol. 18:152–157
Enriquez J, Javadi S, Murthy R, et al. (2013) Gastroduodenal artery recanalization after transcatheter fibered coil embolization for prevention of hepaticoenteric flow: incidence and predisposing technical factors in 142 patients. Acta Radiol. 54:790–794. doi:10.1177/0284185113481696
Acknowledgments
This research is an investigator initiated trial, which was supported by a research Grant from Boston Scientific.
Ethical standards
All procedures comply with the current laws of the country in which the procedures were performed.
Conflict of interest
Sung II Park received the research Grant from Boston Scientific. Shin Jae Lee, Myungsu Lee, Mu Sook Lee, Gyoung Min Kim, Man Deuk Kim, Jong Yun Won, and Do Yun Lee have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Park, S.I., Lee, S.J., Lee, M. et al. Prospective randomized trial comparing pushable coil and detachable coil during percutaneous implantation of port-catheter system for hepatic artery infusion chemotherapy. Abdom Imaging 40, 595–600 (2015). https://doi.org/10.1007/s00261-014-0239-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00261-014-0239-1