Abstract
Purpose
Percutaneous ablation of functioning adrenal adenomas has been an alternative to videolaparoscopic treatment. This study aimed to evaluate the feasibility, safety and efficacy of radiofrequency ablation (RFA) in the treatment of functioning adrenal tumors using a computed tomography (CT)-guided percutaneous technique as demonstrated by our experience and the literature.
Methods
Eleven adult patients (mean age 46 years) with a diagnosis of functioning adrenal adenoma underwent CT-guided RFA between October 2011 and August 2012. All RFA procedures were performed using a needle electrode with a single lateral filament and the RITA® 1500X radiofrequency generator. The RFA protocol consisted of two cycles of 5 min each with 1-min interval, with no additional ablation cycles. Contrast-enhanced CT scans were obtained and analyzed for immediate treatment success and possible complications.
Results
Maximum tumor dimension ranged from 1.2 to 3.4 cm. The mean procedure time was 74 min, and length of hospital stay ranged from 0.9 to 3.2 days (mean 1.8 days). One patient had residual pneumothorax and one patient had neuritis involving the T10 dermatome. Of 11 patients, 10 recovered from their condition. Only one patient remained with hyperaldosteronism, but with reduced anti-hypertensive medication.
Conclusions
CT-guided percutaneous RFA was a safe and effective treatment for functioning adrenal adenomas, with short hospital length of stay and low complication rate.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Laparoscopic resection is an established treatment for benign adrenal lesions [1]. Most functioning adenomas are represented by primary hyperaldosteronism (PH) and Cushing’s syndrome (CS). Reported complication rates range from 3.2 % to 20 % and include the occurrence of hemorrhage, damage to adjacent organs and/or structures (e.g., spleen), surgical wound infection, cardiac complications (postoperative myocardial infarction and/or angina), and infectious complications [1, 2].
Less invasive treatment options, such as selective arterial embolization and percutaneous ethanol injection, have been described [3, 4], but without proven efficacy. Percutaneous radiofrequency ablation (RFA) and cryoablation have been evaluated as new therapeutic modalities for the treatment of both benign and malignant adrenal masses [5–7]. Only minor complications have been associated with these treatment options, with pneumothorax and retroperitoneal hematoma reported as the most common complications [8]. There is only one report in the literature of a case of major complication using cryoablation [6], but no reports concerning RFA [5, 7].
RFA is a low-cost procedure associated with low morbidity and mortality rates and quick patient recovery, which makes this therapy an attractive alternative to surgical treatment. Pandharipande et al [9] conducted a cost-effectiveness study using a complex mathematical model to compare percutaneous RFA versus nephron-sparing surgery for small unilateral renal cell carcinomas. They found a significantly lower cost difference in ablative treatment regarding the surgical technique. However, few case series have used RFA in the treatment of functioning adrenal adenomas. To change the treatment paradigm, more case series are needed to prove the efficacy of this method.
This study aimed to evaluate the feasibility, safety and efficacy of RFA in the treatment of functioning adrenal tumors using a computed tomography (CT)-guided percutaneous technique as demonstrated by our experience and the literature.
Materials and methods
Patients
The results of CT-guided RFA procedures performed in 11 patients with a diagnosis of functioning adrenal adenoma between October 2011 and August 2012 were analyzed. The study was approved by the local Ethics Committee (Institutional Review Board-equivalent) and was conducted in accordance with the provisions of the Declaration of Helsinki. Informed consent was obtained from all patients prior to their inclusion in the study.
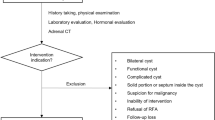
A list of patients with functioning adrenal adenomas (DATABASE), including PH and CS was provided by our institution. Of this list, 16 patients were referred to RFA treatment. All patients were referred from the outpatient endocrinology clinic of our institution with a diagnosis of functioning adrenal tumor and divided into two disease groups, as follows: PH and CS. The diagnosis was based on medical history, physical examination, and specific laboratory tests. For PH, serum aldosterone and plasma renin activity were measured by radioimmunoassay. In cases of CS, measurement of post-suppression plasma cortisol, urinary cortisol, and salivary cortisol levels by chemoluminescence confirmed the diagnosis.
Patients were eligible for the study if they were 18 years or older, had a functioning adrenal adenoma confirmed by clinical criteria, specific biochemical analysis, previous magnetic resonance imaging (MRI) or CT of the upper abdomen, and had typically benign lesions diagnosed by specific imaging protocols (CT and/or MRI), or in cases of doubtful diagnosis, by biopsy. Image analysis included nodule dimensions, site, signal intensity index (SII) at MRI and/or density at CT without contrast. Typical nodules had density <10 HU at CT without contrast and/or SII >16 % at in/out phase of T1-weighted gradient-recalled echo (GRE) sequence (Fig. 1) [10, 11]. The reasons for non-inclusion were as follows: (a) maximum tumor diameter greater than 3.5 cm (relative contraindication); (b) patients with familial syndromes; (c) coagulopathy; (d) pregnant women; (e) suspected pheochromocytoma characterized by an increase in plasma and urinary metanephrines; (g) nephropathy with creatinine clearance <50 %; (h) allergy to iodinated contrast agents; and (i) bilateral adrenal disease since bilateral nodules present nodular adrenal hyperplasia and not bilateral adenomas in most cases. Patients with potentially inaccessible nodules or who decided on surgery were excluded from the study. Histological confirmation was not necessary since all patients had clinical diagnosis confirmation with typical image at CT or MR as well. None of the patients had primary neoplasm. All patients with clinical suspicion had plasma and urinary catecholamines and metanephrines tested and also had image exams if pheochromocytoma was suspected.
Of 16 selected patients, the procedure was performed in 11. Of 5 excluded patients, 2 died of other causes not related to the underlying disease and 3 chose surgical treatment. Of 11 selected patients, 1 had two nodules in the same gland, totalizing 12 treated nodules.
Before RFA, all patients were evaluated by an endocrinologist to optimize blood pressure control and correct any electrolyte disturbances. To insure appropriate monitoring and safety, all RFA procedures were performed in the hospital setting with attendance by an anesthesiologist and nurse anesthetist. Pre-planning was based on CT scans obtained on a 64-channel multidetector helical CT scanner (Brilliance, Philips Medical Systems, Best, The Netherlands) in the department of radiology at our institution.
Techniques for percutaneous RFA
The patient was positioned at the discretion of the interventional radiologist to allow for the best approach and access to safely achieve the target lesion during RFA (Fig. 1).
First, the patients were provided with further explanations about the procedure and step-by-step guidelines. General anesthesia was then induced. Immediately before RFA, a prophylactic dose of parenteral antibiotics (cefuroxime 1.5 g or ciprofloxacin 200 mg) was administered intravenously. A single RFA needle with a 2-cm active tip (StarBurst® electrodes; RITA Medical Systems, Mountain View, CA, USA) was placed, and the tip was inserted gradually into the center of the target lesion under real-time CT guidance (Figs. 2, 3). An electrical circuit was thus established connecting the needle tip, the two plates of insulating material attached to the skin, which served as ground wires, and the radiofrequency generator (Model 1500X; RITA Medical Systems, Mountain View, CA, USA).
All patients were treated using 10- or 15-cm rigid needles or 25-cm flexible needles, depending on the patient’s abdominal circumference and distance from the skin to the target lesion. A renal RFA protocol was used, consisting of two cycles of 5 min each with 1-min interval. No additional ablation cycles were performed other than those preset by the manufacturer.
Contrast-enhanced CT scans were then obtained and analyzed for immediate treatment success (Fig. 4) and for possible complications, which, if present, were classified as major or minor according to the criteria proposed by Goldberg et al. [12]. In the presence of pneumothorax, we adopted the flowchart proposed by Manhire et al. [13].
Total procedure time was defined as the interval between time of first image acquisition to locate the site and time of final control image acquisition after the procedure.
Post-percutaneous RFA
Patients were transferred to the ward after postanesthesia assessment. Response to ablative treatment was assessed through appropriate clinical, laboratory, and MRI evaluation performed 3 months after the procedure in all cases (Fig. 5).
Results
The sample consisted of 11 patients with 12 adrenal nodules, 4 patients were male and 7 were female. Mean age was 46 years (range 33–60 years) (Table 1). All patients underwent only one session of RFA. The procedure was considered technically successful in all patients as assessed immediately after RFA. Of 11 patients analyzed, 9 were diagnosed with PH and 2 with CS. Maximum tumor dimension ranged from 1.2 to 3.4 cm (mean 1.94 cm) (Table 1). Half of the tumors were located in the right gland and the other half in the left gland.
All procedures were performed with the patient under general anesthesia with orotracheal intubation, except for one case which was performed with the patient under unconscious sedation. Patients were positioned on the CT table according to the site and side of the tumor. Dorsal access was obtained in 8 cases with the patient in the prone position, and transhepatic access in 3 cases with the patient in the supine position. The latter patient positioning was very useful in cases of nodules located in the right adrenal gland.
There were two anesthetic complications during RFA, which were adequately resolved during the procedure without later clinical repercussions. One complication was hypoventilation in an obese female patient (body mass index of 35), who was in the prone position under unconscious sedation. The episode was managed by mask ventilation via an Ambu bag, and the patient stabilized. The other case involved a patient with PH who had bradycardia during ablation, with the heart rate lowered by 30 beats per minute (bpm). The patient received atropine intravenously, returning to normal levels.
There were two cases of complications related to the percutaneous technique, both classified as minor complications. In the first case, a laminar pneumothorax occurred when the needle was placed in the left adrenal gland through a posterior approach. The patient had no clinical repercussions and was managed conservatively. In the second case, a female patient with a nodule in the right gland treated by the transhepatic approach had neuritis as a late complication (on postoperative day 5) involving the T10 right dermatome, which was attributed to the close proximity of innervation to the tumor being treated. The patient was managed conservatively with analgesics, with improvement in 15 days without sequelae.
Total procedure time ranged from 51 to 111 min (mean 74.1 min), and length of hospital stay ranged from 0.9 to 3.2 days (mean 1.8 days) (Table 1).
With respect to the objective parameters used in the image assessment (MR control), we observed that the only criterion for radiological cure among the three assessed patients was the enhancement pattern after paramagnetic enhancement. SII and larger lesion diameter were not useful in our methods (Table 2).
Discussion
No radiofrequency indication has been established in the literature. In a Chinese study [8], the authors found equivalent efficacy among the methods used in PH treatment in a comparison between videolaparoscopy versus radiofrequency for the treatment of functioning adenoma.
Traditionally, adrenalectomy has been the treatment of choice for patients with aldosterone-producing adenoma (APA). Laparoscopic adrenalectomy (LA), first introduced by Gagner et al. [14] in the last decade, has replaced the open approach as the gold standard treatment [15]. Despite its benefits, there are some risks and drawbacks associated with LA [15]. Overall morbidity associated with this minimally invasive method is as high as 9.5 %, and mortality is 0.2 %; for APA, in particular, the reported morbidity rate is 8 % [15]. In addition, the number of cases in most centers is limited and the advanced laparoscopic techniques required to perform adrenalectomy often result in a long operating time, associated with a relatively steep learning curve for surgeons in training, which warrants a search for easier to use and less invasive alternative therapies [8].
CT-guided percutaneous RFA is an alternative to LA for functioning adrenal adenomas. The adrenal glands are surrounded by adipose tissue in the perinephric space, which acts as a heat insulator to prevent thermal injury to adjacent organs or important vasculatures, thus making APA a suitable lesion for RFA. Most APAs are benign and tumor seeding and recurrence are not common; however, in the presence of recurrence or residual lesion, RFA can be readily repeated [8].
Important technical advances have allowed safe and effective ablation of adrenal masses as an alternative minimally invasive therapy [16–19]. Previous studies have demonstrated the successful treatment of adrenal tumors using RFA, and their main findings are briefly described in Table 3. Mayo-Smith and Dupuy [20] demonstrated a success rate of 84 % (11/13 patients) in the treatment of patients with metastases or primary malignant adrenal tumors. Wood et al. [21] reported a success rate of 53 % (8/15 patients) in the treatment of metastatic adrenal tumors (mean follow-up, 10.3 months). Arima et al. [22] showed an initial success rate of 75 % (3/4 patients) after using RFA in functioning adrenal tumors, achieving 100 % success after repeat treatment of one tumor. Liu et al. [8] reported a 95.8 % (23/24 patients) technical success rate in the treatment of functioning adrenal adenomas, also achieving 100 % success after repeat treatment of one case. Mendiratta-Lala et al. [5] achieved technical and clinical success in 100 % of cases (13/13 patients). The only case series about the treatment of adenomas was conducted by Liu et al. [8]. The authors reported a 95.8 % (23/24 patients) technical success rate in the treatment of functioning adrenal adenomas, also achieving 100 % success after repeating the treatment of one case. However, the study included only patients with hyperaldosteronism.
Our study also included CS and PH. Our experience revealed a success rate of 91 % (10/11 patients) (Table 2). We believe that treatment failure in the patient who was not cured was due to the location of the adenoma, which was virtually attached to the inferior vena cava in the right adrenal gland. The vessel is known to dissipate heat, reducing the effectiveness of the ablation procedure [5].
There was an unusual case in our cohort of a patient who had undergone left adrenalectomy for a myelolipoma, and RFA was performed for a functioning adenoma in the right adrenal gland and renal cell carcinoma in the middle third of the right kidney. Ablation of both the adenoma and the renal tumor was successfully performed in the same procedure, with excellent clinical response as assessed by laboratory and imaging tests.
A limitation of this study is the patient population. Future studies involving a larger number of patients, including those with adenomas and carcinomas, may help to further determine the value of RFA for the treatment of adrenal tumors, regardless of the functional status of the tumor. Moreover, additional randomized studies comparing a group of patients undergoing RFA vs. surgery should be conducted to reinforce the importance of the percutaneous ablative method.
We reported on our experience with RFA as the primary treatment modality for patients with functioning adrenal tumors. We achieved high rates of technical and clinical success with minimal complications, suggesting that RFA may be a safe and effective method for outpatient treatment of small benign functioning adrenal lesions, which is supported by recent studies addressing this topic. We believe that more case series are needed to show the efficacy and replication of this method so that the treatment paradigm for patients with functioning adrenal adenomas may be changed. In conclusion, CT-guided percutaneous RFA was a safe and effective treatment for functioning adrenal adenomas and is a potential replacement for surgical treatment.
References
Fu B, Zhang X, Wang GX, et al. (2011) Long-term results of a prospective, randomized trial comparing retroperitoneoscopic partial versus total adrenalectomy for aldosterone producing adenoma. J Urol 185:1578–1582. doi:10.1016/j.juro.2010.12.051
Morino M, Beninca G, Giraudo G, et al. (2004) Robot-assisted vs laparoscopic adrenalectomy: a prospective randomized controlled trial. Surg Endosc 18:1742–1746. doi:10.1007/s00464-004-9046-z
Shibata T, Maetani Y, Ametani F, Itoh K, Konishi J (2000) Percutaneous ethanol injection for treatment of adrenal metastasis from hepatocellular carcinoma. AJR Am J Roentgenol 174:333–335
Shibata T, Sagoh T, Maetani Y, et al. (2003) Transcatheter arterial embolization for bleeding from bile duct tumor thrombi of hepatocellular carcinoma. Hepatogastroenterology 50:1119–1123
Mendiratta-Lala M, Brennan DD, Brook OR, et al. (2011) Efficacy of radiofrequency ablation in the treatment of small functional adrenal neoplasms. Radiology 258:308–316. doi:10.1148/radiol.10100690
Welch BT, Atwell TD, Nichols DA, et al. (2011) Percutaneous image-guided adrenal cryoablation: procedural considerations and technical success. Radiology 258:301–307. doi:10.1148/radiol.10100631
Wolf FJ, Dupuy DE, Machan JT, Mayo-Smith WW (2011) Adrenal neoplasms: Effectiveness and safety of CT-guided ablation of 23 tumors in 22 patients. Eur J Radiol . doi:10.1016/j.ejrad.2011.04.054
Liu SY, Ng EK, Lee PS, et al. (2010) Radiofrequency ablation for benign aldosterone-producing adenoma: a scarless technique to an old disease. Ann Surg 252:1058–1064. doi:10.1097/SLA.0b013e318f66936
Pandharipande PV, Gervais DA, Mueller PR, Hur C, Gazelle GS (2008) Radiofrequency ablation versus nephron-sparing surgery for small unilateral renal cell carcinoma: cost-effectiveness analysis. Radiology 248:169–178. doi:10.1148/radiol.2481071448
Goldman SM, Coelho RD, Freire Filho Ede O, et al. (2004) Imaging procedures in adrenal pathology. Arq Bras Endocrinol Metabol 48:592–611. doi:S0004-27302004000500004
Israel GM, Korobkin M, Wang C, Hecht EN, Krinsky GA (2004) Comparison of unenhanced CT and chemical shift MRI in evaluating lipid-rich adrenal adenomas. AJR Am J Roentgenol 183:215–219
Goldberg SN, Grassi CJ, Cardella JF, et al. (2005) Image-guided tumor ablation: standardization of terminology and reporting criteria. J Vasc Interv Radiol 16:765–778. doi:10.1097/01.RVI.0000170858.46668.65
Manhire A, Charig M, Clelland C, et al. (2003) Guidelines for radiologically guided lung biopsy. Thorax 58:920–936
Gagner M, Lacroix A, Bolte E (1992) Laparoscopic adrenalectomy in Cushing’s syndrome and pheochromocytoma. N Engl J Med 327:1033. doi:10.1056/NEJM199210013271417
Assalia A, Gagner M (2004) Laparoscopic adrenalectomy. Br J Surg 91:1259–1274. doi:10.1002/bjs.4738
Curley SA, Izzo F, Delrio P, et al. (1999) Radiofrequency ablation of unresectable primary and metastatic hepatic malignancies: results in 123 patients. Ann Surg 230:1–8
Goldberg SN, Solbiati L, Hahn PF, et al. (1998) Large-volume tissue ablation with radio frequency by using a clustered, internally cooled electrode technique: laboratory and clinical experience in liver metastases. Radiology 209:371–379
Lindner NJ, Scarborough M, Ciccarelli JM, Enneking WF (1997) CT-controlled thermocoagulation of osteoid osteoma in comparison with traditional methods. Z Orthop Ihre Grenzgeb 135:522–527. doi:10.1055/s-2008-1039739
Rossi S, Fornari F, Buscarini L (1993) Percutaneous ultrasound-guided radiofrequency electrocautery for the treatment of small hepatocellular carcinoma. J Interv Radiol 8:195–203
Mayo-Smith WW, Dupuy DE (2004) Adrenal neoplasms: CT-guided radiofrequency ablation–preliminary results. Radiology 231:225–230. doi:10.1148/radiol.2311031007
Wood BJ, Abraham J, Hvizda JL, Alexander HR, Fojo T (2003) Radiofrequency ablation of adrenal tumors and adrenocortical carcinoma metastases. Cancer 97:554–560. doi:10.1002/cncr.11084
Arima K, Yamakado K, Suzuki R, et al. (2007) Image-guided radiofrequency ablation for adrenocortical adenoma with Cushing syndrome: outcomes after mean follow-up of 33 months. Urology 70:407–411. doi:10.1016/j.urology.2007.04.03
Ethical standards
The authors declare that the experiments described herein comply with the current laws of Brazil.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Nunes, T.F., Szejnfeld, D., Xavier, A.C.W. et al. Percutaneous ablation of functioning adrenal adenoma: a report on 11 cases and a review of the literature. Abdom Imaging 38, 1130–1135 (2013). https://doi.org/10.1007/s00261-013-9995-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00261-013-9995-6