Abstract
Flat lesions have been a source of controversy because of concerns that CT colonography (CTC) is insensitive in detecting these lesions, yet they may harbor a high incidence of advanced neoplasia. The wide variation in the reported incidence of flat lesions may in part be due to the lack of a uniform definition of “flat”, and in fact in many prior reports the inclusion criteria for flat are not even clearly specified. Emphasis on the more recent CTC literature suggests that when limited the target lesion to neoplasia (adenomas or adenocarcinoma), the incidence of flat lesions is low and most can be detected by CTC. Using fecal tagging and careful attention to the proper methods of searching for flat lesions with both 3D and 2D techniques can maximize the detection of flat lesions at CTC. Computer-aided detection may be helpful.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Flat lesions of the colon have varied definitions throughout the literature. Particularly in Japan where the incidence of flat lesions (both in the colon and stomach) is reported to be high, detailed classifications of flat lesion morphology have been proposed based primarily on optical endoscopy. The use of indigocarmine dye at endoscopy, magnification endoscopy, and narrow band illumination has improved the detection of flat lesions, yet these techniques are not applied uniformly in clinical practice. Some authors claim that the lower incidence of flat lesions in the Western population may represent under-detection [1]. Some of the older pathology literature suggested that flat lesions might behave more aggressively than non-flat adenomas [2]. As CTC gradually gained acceptance in the radiology community, one criticism raised was the lower detection rate for flat lesions on CTC. As researchers became aware of flat lesions, there has been a proliferation of literature to clarify the definition, incidence, and best ways to detect flat lesions on CTC. This review will summarize the key opinions from the pathology, endoscopy, and primarily the CTC literature.
Definitions
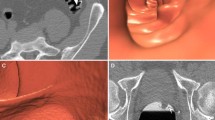
Lesions that have no elevation above the mucosal line are extremely rare. On light microscopy, flat lesions have been described as those in which the thickness of the lesion is less than twice of the adjacent normal mucosa [2–7]. Both of these definitions have no CTC correlation. An endoscopic definition of a flat lesion used by numerous authors is a mucosal elevation with a flat or slightly rounded surface and a height of less than half of the diameter of the lesion [3–5]. Kudo et al. also described flat lesions as level or minimally elevated lesions no more than 10 mm in diameter and laterally spreading tumors as large flat adenomas that are short in height compared to the diameter that is ≥10 mm [8]. The Paris classification defines flat lesions as those protruding below the level of closed jaws of biopsy forceps (2.5 mm) [9]. Pickhardt et al. defined a flat lesion as a shallow plaque-like broad-based lesion with a height of less than one half of its width, and except for some larger lesions, these lesions generally measure ≤3 mm in height [10]. Gluecker et al. [11] defined flat lesions as those with a base at least twice as wide as the height. In a consensus opinion, the proposed CTC definition is <3 mm of vertical elevation above the colonic mucosa [12]. Robbins et al. [13] analyzed the lateral size of lesions categorize as flat in cohort of 5107 screening CTC exams (without colonoscopy correlation for normal exams) and found 125 flat lesions in 106 CTC exams of which only 92 were <3 cm in diameter. Of those 92 lesions, 25% were neoplastic, 5.4% were histologically advanced, and none were malignant. However, of 602 polypoid lesions >3 cm in diameter, more were neoplastic (60.3%), histologically advanced (12.1%), and malignant (0.5%). The maximal lesion height of flat lesions <3 cm averaged 2.2 mm. Robbins et al. formulated a new proposed definition for flat lesions as a maximal height to a width ratio of 0.33 or 0.40, regardless of size. In a study by Lostumbo et al., it was recommended to use the flat lesion definition of height ≤1/2 long axis on a 3D endoluminal view to minimize inter-observer variability in measurements. Using the long axis as the key metric, endoluminal 3D views showed the least inter-observer variability as compared to a 2D lung (W = 1500, L = −200) and 2D soft tissue views (W = 400, L = 10) [14]. Figure 1 shows an example of flat lesions in the three different viewing methods.
Prevalence and aggressiveness
The aggressive potential of flat lesions has not been demonstrated in Western studies, although the large flat lesions as described by Kudo et al. [8] in Japan may be more aggressive than previously thought. Kudo et al. found flat adenomas on optical colonoscopy (OC) to be 39% (5478/14,014) and the laterally spreading tumor to be 3% (428/14,014) of all adenomas and carcinomas detected in their studies. Of the 296 carcinomas detected, 3 were flat lesions (1%) and 35 were laterally spreading tumors (11.8%). Pickhardt et al. [10] found the prevalence of flat lesions on CTC to be 4.2% (59 total lesions in 52/1233 patients) in a healthy screening population. Of the 59 flat lesions, 29 (49.2%) were adenomatous of which only 5 were advanced (8.5%) and 1 large flat lesion was malignant. Kim et al. [15] found the prevalence of advanced adenomas on CTC to be 3.1% (111 of 3536 patients) in a healthy screening population with flat lesions comprising only 7.3% of the advanced adenomas (9/123), none of which exhibited high-grade dysplasia. The prevalence of carcinoma was 0.2% (7 of 3536 patients), of which two of the seven cases were characterized as relatively flat although large. In a higher risk population, Rembacken et al. [2] found the prevalence of adenomas on OC to be 22.5% (225 of 1000 patients) with flat lesions comprising 36.4% of all adenomas. The prevalence of carcinoma was 3% (30 of 1000 patients). Of the 31 carcinomas, 17 (54.8%) were characterized as flat, 3 of which were <10 mm in size and 14 of which were ≥10 mm in size.
Appearance
The Japanese Research Society has a classification range of flat lesion appearances including IIa (flat elevated), IIa/IIc (flat elevated with central depression), IIb (flat), IIc (flat depressed), and IIc/IIa (flat depressed with raised edges) (Fig. 2) [16, 17]. Rembacken et al. [2] describes flat adenomas on OC as patches of erythema or irregularity of a mucosal fold. Park et al. [18] describes flat lesions on CTC appearing as nodular mucosal surfaces, plaque-shaped mucosal elevations, thickened haustral folds, carpet lesions if they involve a large part of the colonic surface, and a slight elevation with a centrally depressed area. Fidler et al. [19, 20] described flat lesions on CTC as flat elevations, areas of smooth or irregular wall thickening (Fig. 3), and “cigar-like” appearances (lesions on a fold projecting into the lumen). On 3D virtual dissection imaging, flat lesions appeared as flame- or pea-shaped lesions [21].
Axial image showing a flat lesion displayed in soft tissue window settings. Note that the lesion is distinguished from normal surrounding mucosa by its sharp margins and variable thickness. (Courtesy: Jeff Fidler, MD and Reproduced with permission from The Atlas of Virtual Colonoscopy, Dachman AH (ed), Springer-Verlag, Inc., New York, NY. 2003. Fig. 14.1b.)
Carpet lesions can mimic converging folds on 2D views (Fig. 4).
Barriers to detection
Fidler et al. [22] showed that of the 51 flat lesions missed in their study, 57% were missed because of errors in detection, 37% were characterized wrong by being interpreted to represent another structure (fold/wall), and 6% were mistaken as intraluminal material. Causes for false positives mentioned by Mang et al. [23] were haustral folds, intramural, and extraluminal structures (connective or fat tissue). In a study by Gluecker et al. [11] with 500 asymptomatic, high-risk patients with 116 lesions of which flat lesions only represented 17% of the total lesions, 83% of lesions ≥5 mm with an irregular surface were missed as compared to 57% of those with a smooth surface (P = 0.04). Lesions next to a region of thickened colonic wall were missed more frequently (86%) than those next to <3 mm wall thickening (58%) (P = 0.05). Optimal preparation for all lesions ≥5 mm resulted in 51% missed polyps as compared to 76% for moderate/poor preparation (P = 0.02). In studies by Pickhardt et al. [10], it was found that adherent stool was a source of false positive results. To differentiate stool from a flat lesion, they recommended stool tagging and translucency rendering on 3D to assess the internal density of a lesion. In a study by Park et al. [24], plaque-like morphology of flat lesions mistook them for fecal material. In addition to poor bowel prep and inadequate colonic distension, flat lesions and small polyp size were the main causes of missed lesions. Flat lesions <1–2 mm hight could not be detected with multi-detector row CT. Fidler et al. [20] found that lesions on or near folds were more difficult to visualize. The group also mentions that flat lesions were more difficult to detect because some readers may be unfamiliar with their rare morphologies.
Optimal viewing methods
Lesion size, defined as the single largest diameter of the polyp head, remains the most important decisive factor in risk stratification of a colonic lesion and also in detecting colonic lesions on CTC. Advanced neoplasia can be defined by size alone (≥10 mm diameter). For lesions ≥10 mm, Johnson et al. [25] did not show a significant difference in using 2D for primary interpretation with 3D for further evaluation (87% sensitivity) as compared to primary 3D endoluminal fly-through interpretation with 2D for further evaluation (88% sensitivity). Zalis et al. [12] recommend evaluation of the colon with window width of 1500 Hounsfield Units (HU), and level setting of −200 HU along with soft tissue settings to characterize flat lesions more precisely. They recommend both 2D multi-planar views and/or 3D endoscopic volume-rendered views. Fidler et al. [20] recommended that both lung (width = 2000 HU, level = −600 HU) and soft tissue (width = 400 HU, level = 20 HU) settings be used since a lesion was more conspicuous on the soft tissue setting. These researchers used 2D axial views for detection along with 2D multi-planar and 3D endoluminal views for further interpretation, but felt that the 3D endoluminal view was the least helpful. In a phantom study using three different workstations, measurements obtained at 2D lung window settings were more accurate than those taken at 2D soft-tissue window settings (P < 0.0001) [26]. In another phantom study, the sensitivity of flat polyp detection increased from 82% to 94% (P = 0.001) when using a 2D wide window setting (width = 1200 HU, level = −100 HU) with planar cross-sectional images available in the transverse, sagittal, and coronal planes vs. the 2D setting along with 3D volume-rendered endoluminal fly-through and target views [23]. The study also demonstrated that multi-detector CT scanners, when using a 1-mm slice thickness, have higher scanning speeds, fewer motion artifacts, and higher spatial resolution compared to single detector-row CT. Park et al. [24] used a four-detector row scanner, 0.8-s gantry rotation speed, and 2.5-mm thick sections in their studies, and admitted that faster speed, higher detector number, and thinner sections could have helped in detecting flat lesions. Gluecker et al. [11] used a 2D search method with 2D multi-planar reconstructions and 3D endoluminal imaging for further evaluation. They recommended that flat lesions be optimally visualized on 2D axial or multi-planar reformatted images with bone or soft-tissue window settings. They did not recommend 3D endoluminal images for flat lesion detection because they may be occult. However, Pickhardt et al. [10] found that flat lesions were more conspicuous and easier to initially detect on a 3D endoluminal view. Park et al. [18] also show that the flat lesion morphology is easier to see on 3D views, particularly the 3D-fly through view. In a small study of 10 patients with 18 flat polyps, all flat lesions initially detected were on the colon window setting (width = 1500 HU, level = −200 HU), although with the presence of IV contrast enhancement, lesions could be distinguished from feces in the soft-tissue window setting (width = 400 HU, level = 20 HU). Lesions on folds had higher conspicuity on the 3D endoluminal view. Park et al. [27] recommended that use of 3D endoluminal fly-through methods for detection of lesions might improve sensitivity of CTC. Park et al. as well as Fidler et al. found that two expert readers instead of one improved sensitivity [20, 24]. Lostumbo et al. [14] showed that when using the flat lesion definition of height ≤3 mm, more data sets were classified as flat in 2D flat (n = 76), 2D soft tissue (n = 82), and 3D (n = 73) views than in the 2D lung (n = 49) view. Therefore, they recommended that whoever is using a method for a measurement; he/she must use the same viewing method consistently because the lesions fitting the definition may change. Lesions were on average significantly more conspicuous in the 3D endoluminal view as compared to the 2D views.
Computer-aided detection
Just as flat lesions are more difficult for the human to detect because they are small and may be less conspicuous, computer-aided detection (CAD) is less sensitive for flat lesions as compared to non-flat lesions. In 2008, Morimoto et al. [28] found that CAD detected 100% of protruding lesions but only 69.2% of flat lesions. In a recent analysis, Summers et al. [29] found that polyps not found by CAD were more frequently flat (of lower height) and that polyps found by CAD were more conspicuous and that increased polyp height contributed to the increased conspicuity. Less conspicuous polyps were flatter. Flat polyps ≤2 mm hight were difficult to tell apart from the colonic wall thickness. They concluded that it is important for manufacturers of CAD programs to recognize that flat and less conspicuous polyps are more difficult to detect with CAD, so they can improve their detection programs by focusing on such polyps. Taylor et al. [30] emphasized the importance of improving lesion detection methods within CAD by focusing on ways to differentiate flat lesions from other objects within the colon. Such a method may be identifying flat lesions based on the extent to which they involve the colon wall, particularly looking for local thickening. In a stand-alone study, we modified our MTANN CAD program to optimize detection of flat lesions and applied the program to 25 patients who had 28 flat lesions from a previously published clinical trial [31] and the software detected 68% (19/28) flat lesions, including 6 lesions missed by readers in the original trial [32, 33]. Figure 5 demonstrates a flat lesion initially missed on CTC, but then detected with CAD. In an observer study of a large Asian cohort who underwent both optical and CT colonography in a 33-month period, researchers searched for lesions ≤2 mm in height proven on endoscopy and identified 23 lesions in 21 patients: eight adenomas 9–30 mm in width, 10 stage T1 or Tis adenocarcinomas 10–25 mm, and five non-adenomatous lesions 8–20 mm in width. The human observers without CAD were 90% sensitive and detected 9/10 adenocarcinomas but none of the 5 non-adenomatous lesions. When combining adenomas and adenocarcinomas, the observers found 66.7% (12/18) lesions. CAD was also 90% sensitive for the carcinomas and 55.6% sensitive for the combined adenoma/carcinoma group. CAD also missed the five non-adenomatous lesions [34]. Thus, there is a reason to believe from recent stand-alone and observer data that CAD could potentially improve reader detection of flat lesions.
Conclusions
When analyzing or reporting on flat lesions in the colon on CTC care should be taken to clearly define the measurements used to define the lesion as flat and the viewing methods used when making those measurements. By current convention the lesion should be 3 mm or less in height. Radiologists interpreting CTC should pay close attention to potential flat lesions and view the polyp candidates on 3D and optimized 2D views. Additional effort to search for flat lesions may improve reader sensitivity. CAD programs should be optimized to include detection of flat lesions.
References
Ross AS, Waxman I (2006) Flat and depressed neoplasms of the colon in Western populations. Am J Gastroenterol 101:172–180
Rembacken BJ, Fujii T, Cairns A, et al. (2000) Flat and depressed colonic neoplasms: a prospective study of 1000 colonoscopies in the UK. Lancet 355(9211):1211–1214
Tsuda S, Veress B, Toth E, et al. (2002) Flat and depressed colorectal tumours in a southern Swedish population: a prospective chromoendoscopic and histopathological study. Gut 51:550–555
Sawada T, Hojo K, Moriya Y (1989) Colonoscopic management of focal and early colorectal carcinoma. Baillieres Clin Gastroenterol 3:627–645
Soetikno R, Friedland S, Kaltenbach T, et al. (2006) Nonpolypoid (flat and depressed) colorectal neoplasms. Gastroenterology 130(2):566–576
Hurlstone DP, Karajeh M, Sanders DS, et al. (2005) Rectal aberrant crypt foci identified using high-magnification-chromoscopic colonoscopy: biomarkers for flat and depressed neoplasia. Am J Gastroenterol 100(6):1283–1289
Kudo S, Kashida H, Nakajima T, et al. (1997) Endoscopic diagnosis and treatment of early colorectal cancer. World J Surg 21:694–701
Kudo S, Kashida H, Tamura T, et al. (2000) Colonoscopic diagnosis and management of nonpolypoid early colorectal cancer. World J Surg 24(9):1081–1090
The Paris endoscopic classification of superficial neoplastic lesions: esophagus, stomach, and colon. Gastrointest Endosc 58(Suppl 6):S3–S43 (2003)
Pickhardt PJ, Nugent PA, Choi JR, et al. (2004) Flat colorectal lesions in asymptomatic adults: implications for screening with CT virtual colonoscopy. AJR 183:1343–1347
Gluecker TM, Fletcher JG, Welch TJ, et al. (2004) Characterization of lesions missed on interpretation of CT colonography using a 2D search method. AJR 182(4):881–889
Zalis ME, Barish MA, Choi JR, et al. (2005) CT colonography reporting and data system: a consensus proposal. Radiology 236:3–9
Robbins J, Pickhardt P, Kim D (2009) Flat (nonpolypoid) lesions at CT colonography: imaging and histologic characteristics using a new morphologic definition [Abstract]. Annual Meeting of the ARRS. Boston, MA
Lostumbo A, Tsai J, Suzuki K, et al. (2009) Comparison of 2D and 3D views for evaluation of flat lesions in CT colonography. Acad Radiol (in press)
Kim DH, Pickhardt PJ, Taylor AJ (2007) Characteristics of advanced adenomas detected at CT colonographic screening: implications for appropriate polyp size thresholds for polypectomy versus surveillance. AJR 188(4):940–944
Anonymous (1983) General rules for the clinical and pathological studies on cancer of the colon, rectum and anus. Part I. Clinical classification. Japanese Research Society for Cancer of the Colon and Rectum. Jpn J Surg 13:557–573
Anonymous (1983) General rules for the clinical and pathological studies on cancer of the colon, rectum and anus. Part II. Histopathological classification. Japanese Research Society for Cancer of the Colon and Rectum. Jpn J Surg 13:574–598
Park SH, Lee SS, Choi EK, et al. (2007) Flat colorectal neoplasms: definition, importance, and visualization on CT colonography. AJR 188:953–959
Fidler J, Johnson C (2009) Flat polyps of the colon: accuracy of detection by CT colonography and histologic significance. Abdom Imaging 34:157–171
Fidler JL, Johnson CD, MacCarty RL, et al. (2002) Detection of flat lesions in the colon with CT colonography. Abdom Imaging 27:292–300
Silva AC, Wellnitz CV, Hara AK (2006) Three-dimensional virtual dissection at CT colonography: unraveling the colon to search for lesions. Radiographics 26(6):1669–1686
Fidler JL, Fletcher JG, Johnson CD, et al. (2004) Understanding interpretive errors in radiologists learning computed tomography colonography. Acad Radiol 11(7):750–756
Mang TG, Schaefer-Prokop C, Maier A, et al. (2005) Detectability of small and flat polyps in MDCT colonography using 2D and 3D imaging tools: results from a phantom study. AJR 185(6):1582–1589
Park SH, Ha HK, Kim MJ, et al. (2005) False-negative results at multi-detector row CT colonography: multivariate analysis of causes for missed lesions. Radiology 235(2):495–502
Johnson DC, Mei-Hsiu C, Toledano AY, et al. (2008) Accuracy of CT colonography for detection of large adenomas and cancers. N Engl J Med 359(12):1207–1217
Young BM, Fletcher JG, Paulsen SR, et al. (2007) Polyp measurement with CT colonography: Multiple-reader, multiple-workstation comparison. AJR 188(1):122–129
Park SH, Ha HK, Kim AY, et al. (2006) Flat polyps of the colon: detection with 16-MDCT colonography—preliminary results. AJR 186:1611–1617
Morimoto T, Iinuma G, Shiraishi J, et al. (2008) Computer-aided detection in computed tomography colonography: current status and problems with detection of early colorectal cancer. Radiat Med 26(5):261–269
Summers RM, Frentz SM, Liu J, et al. (2009) Conspicuity of colorectal polyps at CT colonography: visual assessment, CAD performance, and the important role of polyp height. Acad Radiol 16(1):4–14
Taylor SA, Suzuki N, Beddoe G, et al. (2009) Flat neoplasia of the colon: CT colonography with CAD. Abdom Imaging 34:173–181
Rockey D, Paulson E, Niedzwiecki D, et al. (2005) Analysis of air contrast barium enema, computed tomographic colonography, and colonoscopy: prospective comparison. Lancet 365:305–311
Suzuki K, Sheu I, Rockey CD, et al. (2009) A CAD utilizing 3D massive-training ANNs for detection of flat lesions in CT colonography: preliminary results. Proc SPIE 7260:72601A1–72601A7
Suzuki K, Yoshida H, Nappi J, Armato SG III, Dachman AH (2008) Mixture of expert 3D massive-training ANNs for reduction of multiple types of false positives in CAD for detection of polyps in CT colonography. Med Phys 35:694–703
Park SH, Kim SY, Lee SS (2009) Sensitivity of CT colonography for nonpolypoid colorectal lesions interpreted by human readers and with computer-aided detection. AJR 193:1–9
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lostumbo, A., Suzuki, K. & Dachman, A.H. Flat lesions in CT colonography. Abdom Imaging 35, 578–583 (2010). https://doi.org/10.1007/s00261-009-9562-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00261-009-9562-3