Abstract
Background
The challenge for radiofrequency ablation (RFA) of hepatocellular carcinomas (HCC) in problematic locations is that the outcome is limited due to insufficient ablation or injury of nearby structures. This study aimed to evaluate effective strategy and treatment results of RFA in these cases.
Methods
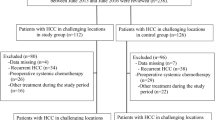
Ultrasound guided percutaneous RFA was performed in 326 HCC patients. Among them, 249 tumors in 215 patients located at liver periphery, including 54 adjacent to GI tract, 110 close to the diaphragm, 49 close to the gallbladder, and 36 tumors close to liver surface. The sizes of the tumors ranged 1.2–7.0 cm (average 3.7 ± 1.3 cm). Individualized treatment strategy was established for tumors in various locations, including “artificial ascites”, “lift-expand” electrode placement, “draw-expand” electrode placement, “Supplementary ablation”, and “accumulative multiple ablations” techniques. Treatment outcome was compared with another 64 central-located tumors (control group) in the same patients. One-month post-RFA contrast CT was used to evaluate early necrosis rate of the treated tumors.
Results
Early tumor necrosis were obtained in 91.6% (228/249) of the problematically located HCC, including 90.7% (49/54) of the tumors adjacent to GI tract, 90.9% (100/110) near the diaphragm, 91.8% (45/49) by the gallbladder, and 94.4% (34/36) close to liver surface. The necrosis rate of control group was 98.4% (63/64), which was higher than the tumors close to diaphragm (P = 0.049). Local tumor recurrence was 8.4% (21/249), comparing with 3.1% (2/64) of the control group (P > 0.05). The 1-, 2- and 3-year survival rate of this group were 81.6%, 63.8%, and 53.6%, respectively. Major complications occurred in 3.2% (11/343) of the treatment sessions, including hemorrhage in two, nearby structure injury in five, and needle tract seeding in four patients.
Conclusions
Individualized treatment strategy for problematically located HCC is helpful in improving RFA outcome and expanding the application range of the therapy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Radiofrequence ablation (RFA) has been proved to be an effective therapy for treating small hepatocellular carcinoma (HCC) [1–3]. Recently, with the development of the therapeutic technique and instrument, the outcome of treating large tumors was improved [4, 5]. In China, many HCC patients have liver cirrhosis, which often make them non-surgical candidates. And post-surgical recurrence rate was as high as 40%–60% [6, 7]. Thus, local therapy, such as RFA is one of the options for the tumors located close to major structures such as GI tract, gallbladder and diaphragm etc. The challenge for these cases is that outcome of RFA is limited due to insufficient ablation or injury of nearby structures. The present study aimed to evaluate the treatment strategy and feasibility of RFA for those HCC in problematic locations.
Materials and methods
Patients
From October 2000 to January 2007, percutaneous ultrasound-guided RFA was performed in 326 patients with HCC. The inclusion criteria for patients were: tumor accessible via a percutaneous approach, absence of portal/hepatic vein main branch tumor thrombus; INR>1.6, platelet count >50,000/μl, tumor size ≤ =7.0 cm, tumor number ≤= 4, and no tumor invasion of major surrounding structures. Among the 326 patients, 215 patients with 249 tumors located in liver periphery were entered in the present study, and were treated with individualized RFA protocol. They were 175 males and 40 females, aged 24–80 years (average 59.2 ± 11.5 years). Seventy-four patients had multiple tumors. The HCC ranged 1.2–7.0 cm in diameters (average 3.7 ± 1.3 cm). There were 128 patients that had liver function of Child-Pugh class-A, 75 had class-B, and 12 class-C. There were 54 patients (25.1%) at stage I in AJCC-TNM system, 114 (53.0%) in stage II–IV. Forty-seven (21.9%) patients had post-surgical recurrent tumors.
The 249 tumors located close to (<1 cm in distance) major surrounding structures included 54 tumors (21.7%) close to GI tract, 110 tumors (44.2%) near the diaphragm, 49 (19.7%) near gallbladder, and 36 (14.5%) close to the liver surface. Treatment outcome was compared with another 64 central located tumors (control group) in the same patients.
Treatment strategy
General principle
The size of the tumors was determined by ultrasound and CT measurements. For tumors with unclear border, contrast-enhanced ultrasound (CEUS) was used to define their margins. Ablated region was planned at least 0.5 cm beyond the tumor border, 1 cm for HCC without clear margin. The steps of ablation were determined by the relationship of the tumor with adjacent structures and the tumor-feeding vessel. Ablation was first conducted at the site where feeding vessel entered the tumor, then the area close to surrounding structures, and the rest of the tumor tissue. It was suggested that larger than 5 cm HCC with rich supply received TACE before RFA.
The process of RFA was performed with real-time ultrasound monitoring.
Ablate large tumors
Based on the size and shape of the liver tumor, various ablating protocols were used. The goal is to obtain complete tumor necrosis with one treatment session.
Single-ablating region smaller than 5 cm in diameter can only be used for ablating small HCC with diameter smaller than 3.5 cm. Multiple overlapping ablations are needed for tumors larger than 3.5 cm. Therefore it is critical to estimate the number and site of the ablations in order to obtain complete necrosis of large HCC. Based on mathematical calculation and clinical practice, the author developed a RFA protocol for HCC of various sizes [5, 8]. For example, for spherical tumor, four ablating spheres, 5 cm in diameter each, are needed to cover a tumor sized 4.0–4.3 cm, 5–8 ablation spheres for 4.4–5.6 cm tumor, and 12 overlapping ablations for 5.7–6.5 cm tumor. In cases of large ellipsoidal tumors, the spherical tumor protocol could be modified and used. For irregularly shaped tumors, the main part of the tumor was ablated using the spherical tumor protocol, whereas the remaining irregular and protruding parts of the lesion were treated using small ablation spheres [9].
Control tumor blood supply
Before RFA, we used color ultrasound to detect the tumor blood supply and identify the entrance of feeding vessel. As the first step of the RFA treatment, 2–3 overlapping high energy ablating foci, 2–3 cm each in diameter, were used to ablate the entering site of the feeding vessel. This method was called “accumulative multiple ablations” (Figure 1). Color Doppler ultrasound was used to confirm the absence of feeding artery. This technique is routinely used in large HCC treatment. It is also suitable for ablating hypervascular HCC in problematic locations. Blocking the blood flow in the tumor is helpful in decreasing heat loss during RFA, and therefore the outcome improves.
A 78-year-oldman with HCC. He was not fit for surgery and TACE due to diabetes and hypertension. A CECT before RFA showed tumor and feeding artery enhanced at arterial phase. B Color ultrasound showed feeding vessel (upward arrow) inside tumor (4 × 4.5cm). C Color ultrasound-guided RFA. The entrance area of feeding vessel was ablated first (left). Accumulative ablations were performed in this area (right). D. Ultrasound-guided RFA of other area of tumor. E. Color ultrasound immediately after RFA showed tumor blood supply disappeared. F. CEUS 1 week after RFA showed the ablated area beyond the tumor and no viability (left). CEUS 3 months after RFA showed no enhancement in ablated area (right). This patient survived for 2 years.
Individualized protocol for tumors adjacent to major structures
For tumors adjacent to the major structures such as the gastrointestinal tract, diaphragm, gallbladder or liver surface, individualized ablation protocols were developed. Insert the needle perpendicularly to the adjacent structure, estimate the distance from the expanded needle tips to the adjacent structure, and plan 2–3 cm small ablating foci near the structure. When the “needle umbrella” is being expanded, lift or draw the needle repeatedly to confirm that the needle tip is not in the structure, and then start the ablation treatment. This technique was called “lift-expand” or “draw-expand” needle placement.
Protocol for ablating HCC adjacent to GI tract (Figure 2)
-
1.
The patient is placed in right-oblique lateral position that allows bowels to move away from the liver.
-
2.
Between the right intercostal space, insert the RFA needle from superior liver surface perpendicular toward the GI structure. Ablate the tumor portion near the GI tract first with overlapping small ablating foci of 2–3 cm sizes.
-
3.
Ask the patient to use abdominal breathing, which induces movement of bowel loops, and avoid the steady heat from RFA.
-
4.
While deploying “needle umbrella”, fix the catheter needle first, then using the “lift-expand” technique repeatedly confirm that the needle tip is not placed beyond the liver surface, and the bowel loops are moving with the breathing motion, and not with the needle-pulling motion. During ablation, 40–100 mL aseptic solution can be injected between the tumor and GI tract for protection purpose.
-
5.
If liver-bowel adhesion is suspected during the procedure, the following options may be chosen: place an ice bag on RUQ abdomen, inject 6–10 mL of ethanol in the GI side tumor portion, or first ablate major portion of the tumor and consider delayed resection 1–3 months later.
-
6.
Post-RFA management: the patients fast for 24–48 h followed by semi-fluid diet for 2 days before full diet is started. Ultrasound or CT follow-up in 24–48 h after RFA is carried out. Anti-inflammatory treatment is expected for patients with mild bowel-wall thickening. Closed imaging follow-up is needed for patients with progressive bowel-thickening or fluid collection between bowel loops.
A 65-year-old-woman with HCC recurrence 2 months after surgical resection and bilioenterotomy. A The tumor (5.2 × 5.0 cm) (T) was located under liver capsule and adhered to (upward arrow) the bowels (triangle). B “lift-expand” place the electrode and place the ice bag on the right upper abdomen. C The patient was kept fasting and given intraveneous hydration for 3 days due to unrelieved abdominal pain. One month follow up ultrasound showed thickened hypoechoic bowel wall (upward arrow) adhering to the ablated area. D CECT before RFA showed tumor in the right lobe near the liver capsule and bowel (left). CECT one month after RFA showed low density in the ablated area in segment 5 with clear margin without enhancement, indicating complete tumor necrosis (right). This patient survived for more than 3 years.
Protocol for ablating HCC adjacent to diaphragm (Figure 3.)
-
1.
The patient is placed in left-oblique lateral position if the tumor is in the left lobe of the liver. For patients with tumor in right liver, right-oblique lateral position is used.
-
2.
Before RFA, inject 30–200 mL aseptic solution between the tumor and the diaphragm to form “artificial ascites”.
-
3.
The RFA starts from the tumor portion close to the diaphragm. The needle is inserted from the caudal direction perpendicular to the diaphragm, the “draw-expand” technique is used to place the needle, and then the ablation is started.
-
4.
When the ablation area is not satisfactorily obtained due to stiffness of tumor tissue or anatomic limitation of the diaphragm, “Supplementary ablation method” is conducted as follows: after finishing a 5-cm (or 4-cm) ablation sphere, the prongs are withdrawn and the RFA electrode is advanced forward for 1 cm in the tumor, and the prongs are then deployed to begin another 5-cm (or 4-cm) ablation sphere (Figure 4). Our experience showed that this technique provided satisfactorily ablation of the deep portion of the tumor, which was near diaphragm.
-
5.
If imaging is limited due to lung disturbance, insert the needle with extra care. Puncture of the diaphragm cannot be ruled out when resistance is experienced during insertion. In this case, withdraw the needle slightly, have a small range local ablation or focal injection of ethanol. Real-time ultrasound monitoring is important during the procedure, and better view of the diaphragm can be obtained when scanning from the direction of right posterior/middle axillary line.
A 47-year-old-man with HCC and AFP of 836ng/ml. He was not fit for surgery due to chronic renal function failure. A CECT showed a tumor near diaphragm (upward arrow). B Ultrasound showed the tumor (3 × 2 cm) located under diaphragm. C Ultrasound-guided injection of 30 ML of aseptic solution (upward arrow) to separate tumor from diaphragm. D Ultrasound-guided RFA was conducted. E CECT one month after RFA showed tumor necrosis. This patient has survived for more than 1 year disease-free.
Protocol for ablating HCC close to the gallbladder (Figure 5)
-
1.
For RFA patients with HCC located close to the gallbladder, a non- or moderate distended gallbladder is preferred. The patient is usually asked to fast for 6 h prior to RFA, or medication is used to constrict the gallbladder.
-
2.
For HCC close to the right-lateral gallbladder wall, approach from the right costal space through liver parenchyma is used, and for lesion near the left side of gallbladder, approach through the left liver is applied. The patient positioning is chosen to facilitate best view of the tumor, and supine position may be helpful to avoid the influence of the costal arch.
-
3.
Prior to the RFA, 40–80 mL of aseptic solution is injected in to the gallbladder fossa and cystic plate with a 20–22 gauge PTC needle. This technique is enables separating the liver tissue from the gallbladder cystic plate, and after the focal tissue edema is created, RFA may be started.
-
4.
Ablate the tumor portion close to the gallbladder. Use “lift-expand” technique to confirm that the needle tip does not stick into the gallbladder wall.
-
5.
Stimulation of the gallbladder may cause gallbladder–cardiac syndrome, therefore vital sign monitoring during RFA is required. When indicated, atropine is used to increase heart rate, oxygen and pain management is applied.
-
6.
In patients with gallstone or chronic cholecystitis, post-RFA anti-inflammatory therapy is used to decrease the risk of acute cholecystitis. For patients with severe abdominal pain, ultrasound and CT follow-up within 3 days is used to identify potential complications.
A 65-year-old man with HCC recurrence after resection. A CECT showed enhanced tumor with unclear margin (upward arrow) near liver surface and gall bladder. B Ultrasound-guided insertion of needle (filled triangle) between liver and gall bladder and injection of 40 mL of aseptic solution to separate tumor from gall bladder (upward arrow). C Color ultrasound showed feeding artery in the deep area of tumor (left). Use of 2–3 small ablations to ablate this area (right). D Use of “accumulative ablation” method to block tumor supply (left). After injecting aseptic solution to make liver capsule edema, “lift-expand” placed electrode into the area adjacent to gall bladder. E During RFA procedure, ultrasound found gall bladder wall slightly thickened and displayed double border. F CECT within 24 h after RFA showed the ablation area beyond the tumor and had no viability. The wall of gall bladder was not injured. This patient has survived for more than 5 years.
Protocol for ablating HCC near to the liver surface
-
1.
Before RFA, inject aseptic solution between the tumor and nearby abdominal membrane, and create “artificial membrane edema” by local injection liquid, which is also helpful.
-
2.
Instead of using one puncture site repeatedly, multiple percutaneous puncture sites should be used to avoid leaving the peripheral area untreated or needle tract seeding.
-
3.
Select puncture route toward the tumor through a layer of normal liver tissue or avoid puncture direction perpendicular to liver surface (Figure 6).
-
4.
After ablating for 3 min, continue ablation with a gentle pressure on the needle, which allows abdominal fluid to accumulate around the puncture site and decreases risk of abdominal wall burning.
Instruments and procedure
RITA-1500 RFA system (RITA Medical System, Mountain View, CA, USA) with a 460-KHz generator was used in this study. Expandable electrodes consisted of a 14-gauge outer insulated needles, 15 cm in length. Nine prongs were deployed and retracted by a movable hub and deployment diameter ranged from 3 to 5 cm. The time to produce a 5-cm ablation sphere was about 20 min.
Aloka SSD-5500 (Tokyo, Japan), Technos DU-8 (Esaote, Italy), logic-9 (GE, USA), and IU-22 (Philips, USA) ultrasound systems were used for scanning and needle guidance. SonoVue® (Bracco, Milan, Italy) is used as the contrast agent for enhancing sonogram in flow evaluation.
All RFA procedures were performed by two sonologists (M.H.C., K.Y.) with more than 10 years’ experience in ultrasound-guided liver interventions. Anaesthetists provided moderate sedation for the patients during RFA with intravenous administration of 2.5–5.0 mg Midazolam (Roche; Basel, Switzerland) and 50–100 μg Fentanyl (Fentaini; Renfu, Yichang, China). Local anesthesia was induced by 5–15 mL of 1% lidocaine (Liduokayin; Yimin, Beijing, China). Some patients with tumors adjacent to the diaphragm, hepatic hilum or ligament felt obvious local and right shoulder pain when the ablation was extended. Intravenous infusion of propofol (Diprivan; Zeneca, Macclesfield, UK) 1–2 mg/kg was used to temporarily enhance anesthesia.
During the ablation procedure, patients’ vital signs, such as blood pressure, heart rate, respiration, and oxygen saturation, were continuously monitored. Generally, the patient stayed in the procedure room for observation for an hour after RFA, followed by 1–3 days’ hospitalization for further observation. Hospitalization days were prolonged for those patients with tumor adjacent to bowel, large ablative range or coagulation function disorder.
Therapy assessment and follow-up
All patients were followed up with contrast-enhanced CT (CECT) 1 month after RFA. For patients with large tumor (>5 cm) close to GI tract or diaphragm, 24-h post-RFA CECT was performed, and further follow-up was done after a 3-month interval in the first year, and every 4–6 months after one year. Every 2–3 months, the patients were followed up with color Doppler or contrast-enhanced ultrasound CEUS. Tumor marker tests were also conducted. CECT and ultrasound were used to identify recurrent or new tumors, and CEUS was used to guide RFA needle placement for recurrent HCC. CECT studies were read blindly by two radiologists with 10 years of experience.
Statistical analysis
The Chi-square test and Fisher’s exact test were used to analyze the difference in early necrosis rate, local recurrence rates. Cumulative survival rate of each group was calculated using the Kaplan–Meier method and compared by log-rank test. The level of significance was set at 0.05 for all tests. SPSS 10.0 software (SPSS, Chicago, IL, USA) was used in statistical analysis.
Result
Treatment efficiency
Using individualized RFA protocol, the early necrosis rate for HCC close to major structures was found to be 91.6% (228/249), and the control group 98.4% (63/64). The necrosis rate of HCC near the diaphragm appeared lower than the control group (P = 0.049), and HCC in other locations had similar necrosis rates (Table 1).
The follow-up period for the patients ranged 2–76 months (median, 15 months). During the follow-up period of 2–33 months after RFA, there were 21 recurrent lesions (8.4%) identified in tumors close to major structures, which showed no statistical difference compared with the two recurrent lesions (3.1%) in the control group. In the 215 patients of our group, post-RFA, newly developed lesions occurred in 86 patients (40.0%) in 1–49 months, and 81 (37.7%) patients with new or recurrent lesions underwent repeated RFA.
As shown in Table 2, the 1-, 2- and 3-year survival rats of our group were 81.6%, 63.8%, and 53.6%, respectively. The survival rate of Stage I HCC was significantly higher than that of State II–IV (P = 0.032), and recurrent (P = 0.0001) HCC patients.
.
Complications
There were 11 major compilations in the total 343 RFA sessions (3.2%), including two hemorrhages, one bowel perforation, one jaundice due to biliary narrowing, two large bloody pleural fluid, one thoracic empyema, and four tumor-seedings in needle tract. Among them, 10 (90.9%) were seen in the group with tumor location close to major structures. Besides, there were mild complications, including one mild skin burn, three small pleural effusions, four biliary dilatations, and three cholecystistis/gallbladder wall thickening. There was no RFA-related death. Other symptoms included abdominal, shoulder, or RUQ pains, post-procedure fever, or transient elevated liver function.
Discussion
Early studies concluded that liver tumors located close to major structures were not indicated for RFA therapy due to risk of ablating injury of the important structure or incomplete treatment of the tumor [2]. In the mean time, because of clinical demands, attempts to use RFA for liver tumors near important structures, such as gallbladder and GI tract have been made [10, 11]. Recently, Teratani et al. [12] reported RFA on 207 patients with 231 HCC adjacent to major vessels or organs. Their data showed that other than the slightly higher incidence of complication, similar recurrence rate comparing with treating HCC in other locations was obtained. The present study is to establish individualized RFA protocol for HCC in various difficult locations, including pre-RFA preparation, techniques of RFA for protecting nearby structures, and prevention/management of the complication.
Treatment efficiency
Currently, due to the limitation of thermal effect range, multiple overlapping ablations are used in RFA for large HCC. The author developed a protocol for RFA treating large HCC, and obtained necrosis rate of 88% [5]. For HCC without clear defined margin, the author used pre-RFA CEUS to identify the infiltrating margin of the tumor. The tumor microvascular infiltration shown in the arterial phase on CEUS is helpful for treatment planning and obtaining complete ablation in one session. For hypervascular HCC adjacent to important organs, we used “accumulative ablation” technique to treat the entrance site of the feeding vessel first, which can significantly decrease the blood flow inside the tumor and minimize thermal loss during RFA. Furthermore, we established individualized RFA protocol for HCC in various difficult locations. Special attention was given to post-RFA CT follow-up within 24 h for large HCC near GI tract and diaphragm for early detection of untreated portion of the tumor and complications.
Though the protocol is recommended, there are many factors influencing the outcome of RFA, including poor needle placement due to stiffness of the tumor, limited distension of needle umbrella due to liver cirrhosis, or limited approach due to lung/diaphragm location. Adjustment of the protocol and use of multiple techniques were needed according to individual clinical situation (see Figure 5).
In the present study, we used individualized RFA protocol on HCC close to important structures, and obtained more than 90% early necrosis rate. Compared with the control group, HCC near the diaphragm showed lower necrosis rate by RFA. This was because RFA needle placement was obstructed by the lung and ribs. RFA on HCC in other difficult locations had similar necrosis rate to that of the control group. A follow-up for 2–76 months revealed that there was no significant difference of local HCC recurrence between the two groups.
It has been reported that post-surgery 1- and 3-year survival rate for HCC is 75–90% and 49–76%, respectively [13–15]. Our data showed RFA on non-surgical candidates with HCC in difficult location had the 1- and 3-year survival rates of 81.6% and 53.6%, respectively. For Stage I HCC, the 3-year survival rate was 73.2%, which is comparable with that after surgical therapy. For the rest of the tumors, the 3-year survival rate was 58.9%, suggesting that RFA can be a therapeutic option for advanced HCC in difficult locations.
Complications
Most major RFA-related complications were associated with HCC in dangerous locations. There were two cases in our group in whom the HCC were large (>6 cm), and partially extruding out of the liver margin. Two hours after RFA, the patients had tumor rupture with extensive hemorrhage due to coughing and body position change. Thereafter, we consider these patients’ RFA contraindicated.
In another case, the tumor was a post-surgical focal recurrent lesion of 4 cm in size. It was located close to the transverse colon. One week after RFA, the patient had delayed colon perforation and went through surgery. We believe that the reason for the incidence is associated with GI-liver adhesion from previous surgery, which was consistent with Livaraghi’s description of the relationship between multiple GI perforations with RUQ surgery induced adhesion [16]. Since the patients were asked to fast at least 24 h before RFA, bowel perforation often happened 2–3 days later. Therefore close follow-up for at least 1 week is important for these patients.
In those 49 patients with HCC adjacent to the gallbladder, no severe complication was seen, but close monitoring of the heart rate during RFA procedure is critical.
RFA on HCC with biliary infiltration may cause bile-duct dilatation. There was one patient who had further bile-duct dilatation after RFA. After percutaneous transhepatic drainage, jaundice was improved and the tumor size decreased in the following 3 weeks. The patient has been surviving for more than 4 years.
There were three patients in whom HCC were partially adhering to the diaphragm, and after RFA, large right hemothorax or thoracic empyema was seen. They were managed with intravenous Reptilas and percutaneous drainage, and got better in months. No perforation of the diaphragm happened.
Our data showed that the rate of needle tract seeding for RFA was 1.8%, compared with the reported rate ranging from 0.2% to 12.5% [17–19]. We believe that the seeding is related to the debris on the needle tip and low temperature along the needle tract. Slow needle withdrawal and good heat control of the needle tract is helpful in reducing seeding.
Conclusion
In the present study, we established and implemented a series of RFA protocols for HCC adjacent to important nearby organs, and obtained satisfactory necrosis rate with low complications. These protocols are helpful in broadening RFA applications and confirming it as one of the minimal invasive therapies for HCC patients.
References
Curley SA, Izzo F, Delrio P, et al. (1999) Radiofrequency ablation of unresectable primary and metastatic hepatic malignancies: results in 123 patients. Ann Surg 230:1–8
Gazelle GS, Goldberg SN, Solbiati L, et al. (2000) Tumor ablation with radio-frequency energy. Radiology 217:633–646
Livraghi T, Goldberg SN, Lazzaroni S, et al. (1998) Small hepatocellular carcinoma: treatment with radio-frequency ablation versus ethanol injection. Radiology 210: 655–661
Livraghi T, Goldberg SN, Lazzaroni S, et al. (2000) Hepatocellular carcinoma: radiofrequency ablation of medium and large lesions. Radiology 214:761–768
Chen MH, Yang W, Yan K, et al. (2004) Large liver tumors: protocol for radiofrequency ablation and its clinical application in 110 patients-mathematic model, overlapping mode, and electrode placement process. Radiology 232:260–271
Yamamoto J, Kosuge T, Takayama T, et al. (1996) Recurrence of hepatocellular carcinoma after surgery. Br J Surg 83:1219–1222
Poon RT, Fan ST, Lo CM, et al. (1999) Intrahepatic recurrence after curative resection of hepatocellular carcinoma: long-term results of treatment and prognostic factors. Ann Surg 229:216–222
Yang W, Chen MH, Yan K, et al. (2002) Study of calculating method for ablation area and program for electrode placement by ultrasound-guided radiofrequency ablation of large liver tumors. Chin J Ultrasonogr 11:244–247
Chen MH, Yang W, Yan K, et al. (2006) Treatment strategy to optimize radiofrequency ablation for liver malignancies. JVIR 17:671–683
Chopra S, Dodd III GD, Chanin MP, et al. (2003) Radiofrequency ablation of hepatic tumors adjacent to the gallbladder: feasibility and safety. Am J Roentgenol 180:697–701
Choi D, Lim HK, Kim MJ, et al. (2004) Therapeutic efficacy and safety of percutaneous radiofrequency ablation of hepatocellular carcinoma abutting the gastrointestinal tract. Am J Roentgenol 183:1417–1424
Teratani T, Yoshida H, Shiina S, et al. (2006) Radiofrequency ablation for hepatocellular carcinoma in so-called high-risk locations. Hepatology. 43:1101–1108
Zhao WH, Feng YZ, Ma ZM, et al. (2001) Prognostic factors of patients with hepatoculluar carcinoma after hepatectomy. Chin J Gen Surg 16:472–474
Poon RT, Fan ST, Lo CM, Liu CL, Wong J (2002) Long-term survival and pattern of recurrence after resection of small hepatocellular carcinoma in patients with preserved liver function: implication for a strategy of salvage transplantation. Ann Surg 235:373–382
Nagasue N, Yukayu H (1989) Liver resection for hepatocellular carcinoma: results from 150 consecutive patients. Cancer Chemother Pharmacol 23:S78–S82
Livraghi T, Solbiati L, Meloni MF, et al. (2003) Treatment of focal liver tumors with percutaneous radio-frequency ablation: complications encountered in a multicenter study. Radiology 226:441–451
Kato T, Reddy KR (2001) Radiofrequency—ablation for hepatocellular carcinoma: help or hazard? Hepatology 33:1336–1337
Llovet JM,Vilana R, Bru C, et al. (2001) Increased risk of tumor seeding after Percutaneous radiofrequency ablation for single hepatocellular carcinoma. Hepatology 33:1124–1129
Rhim H, Yoon KH, Lee JM, et al. (2003) Major complications after radio-frequency thermal ablation of hepatic tumors: spectrum of imaging findings. Radiographics 23: 123–136
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Chen, MH., Yang, W., Yan, K. et al. Radiofrequency ablation of problematically located hepatocellular carcinoma: tailored approach. Abdom Imaging 33, 428–436 (2008). https://doi.org/10.1007/s00261-007-9283-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00261-007-9283-4