Abstract
Background
Granulosa cell tumor of the ovary differs from epithelial ovarian tumors in histologic appearance, clinical course and imaging findings. The purpose of this study was to evaluate clinical and imaging features of recurrent ovarian granulosa cell tumors.
Methods
We performed retrospective evaluation of the medical, surgicopathologic records and CT or MR images of 11 patients with pathologically proven recurrent ovarian granulosa cell tumor.
Results
The first recurrence of granulosa cell tumor was diagnosed at between 4 months and 18 years after the initial surgical resection of tumor (mean; 9.7 years). Six patients relapsed after 10 years after initial diagnosis. The recurrent tumors were located in the pelvic cavity alone in three patients, extrapelvic peritoneal cavity alone in two, both pelvic and extrapelvic peritoneal cavity in three, and paraaortic retroperitoneal space in three. The imaging appearances of recurrent masses were variable ranging from solid masses to completely cystic masses.
Conclusion
Recurrent granulosa cell tumor is characterized by late tumor recurrence manifested as a relatively small number of discrete peritoneal or retroperitoneal masses with variable imaging appearances from solid to cystic masses.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Granulosa cell tumor of the ovary is the most common malignant tumor in the category of sex cord-stromal tumors of the ovary, representing 2%–5% of all ovarian tumors [1–3]. Granulosa cell tumor differs from more common epithelial ovarian tumors in histologic appearance, biological profile, clinical course and imaging findings. Granulosa cell tumor is derived from the granulosa cell, a hormonally active component of ovarian stroma that is responsible for estradiol production. Therefore, about two thirds of patients have endocrine manifestations due to hormone secretion by the tumor, leading to early diagnosis [2]. Granulosa cell tumor is considered a low-grade malignancy with a good prognosis and surgery is the mainstay of initial management for patients with a suspected granulosa cell tumor. However, granulosa cell tumor is known for propensity for late recurrence and unpredictable clinical course [4].
Although the use of cross-sectional imaging in the diagnosis and follow-up of ovarian cancer is increasing, there have been few studies of the clinical and imaging findings of recurrent granulosa cell tumors, probably due to relatively small number of cases and quite late recurrence, especially in the radiology literatures [5, 6]. The purpose of this study was to evaluate clinical and imaging features of recurrent ovarian granulosa cell tumors.
Materials and methods
By performing a computerized search of medial records of our institution from January 1992 to January 2003, there were 702 ovarian malignant tumors, of which 34 (4.8%) were granulosa cell tumors. Of these, 12 patients (35%) had pathologically proven diagnoses of recurrent granulosa cell tumors after surgical resection of primary tumor. One patient was excluded from this study because her imaging study was not available for review. A total of eight CT scans and three MR scans of the abdomen and pelvis were available in the 11 patients at the time of first recurrence. Additional seven follow-up CT scans and one MR scan were available after surgery of the first recurrent tumors in six patients. These 11 patients were aged 30–73 years (mean age, 55 years). The mean follow-up period for these patients was 15 years 6 months (range 1–29 years) after the diagnosis of primary granulosa cell tumor. All information of these patients were obtained from operation, pathology and imaging studies. Our retrospective study had institutional review board approval, with waiver of informed consent.
In eight patients, abdominal CT scan (Somatom Plus-S, Plus-4, Volume zoom; Siemens, Erlangen, Germany) was performed following intravenous injection of 100–150 mL of either iopromide (Ultravist; Schering, Berlin, Germany) or iopamidol (Iopamiro 300; Bracco Diagnostics, Milan, Italy) with 7–10 mm slice thickness from the diaphragm to the symphysis pubis. In six of the eight patients, approximately 600–900 mL of oral contrast material (barium sulfate, E-Z CAT; E-Z-EM, Westbury, NY, USA) was administered 1 h before CT scanning and the remaining two patients did not take an oral agent. Unenhanced CT was also performed in one patient. MR imaging was performed with a 1.5 T magnet (Magnetom Vision Plus; Siemens, Erlangen, Germany). T1-weighted axial images and turbo spin-echo T2-weighted axial and sagittal images were obtained. After injection of gadopentate dimeglumine (Magnevist: Schering, Germany) at a dose of 0.1 mmol/kg body weight, T1-weighted axial and sagittal images were also obtained.
We reviewed the medical records for the patient’s clinical characteristics, including age, surgical procedures and stage at diagnosis, postoperative treatment, presenting symptoms at recurrence, and the interval between the time of surgical removal of the primary tumor and the detection of recurrent tumors. Two radiologists retrospectively reviewed the CT and MR imaging findings at the first recurrence for the pattern of tumor recurrence; location, number, size and morphologic appearance of the recurrent masses and the presence or absence of ascites, lymphadenopathy, omental change and distant metastasis. Morphologic appearance of peritoneal metastases was classified as nodular, plaquelike, or infiltrative lesions according to the contour and margin of the mass [7]. Lymphadenopathy was considered to be present when soft-tissue nodules larger than 1 cm in short-axis diameter could be seen on transverse scans along the paraaortic and iliac lymphatic chains.
Results
Table 1 summarizes the clinical data for 11 patients with recurrent granulosa cell tumors. The age at the time of diagnosis of primary granulosa cell tumor was 25–61 years (mean; 42.5 years). The diagnosis of primary tumors was made on the basis of histopathologic results obtained after surgical resection in all patients. The following surgical procedures were performed: unilateral salpingo-oophorectomy in five, total hysterectomy and unilateral salpingo-oophorectomy in one, total hysterectomy and bilateral adnexectomy in four patients. Six patients had stage IA disease at initial presentation, three stage IC disease, and one stage IIIC disease. The initial surgical information and surgico-pathologic staging data were not available in one patient. Postoperatively, four patients received chemotherapy only, and one patient received both chemotherapy and radiotherapy.
The diagnosis of recurrent tumors was also made on the basis of histopathologic results obtained after surgical resection in all patients. The first recurrence of granulosa cell tumor was diagnosed at between 4 months and 18 years (mean; 9.7 years) after the initial surgical resection of granulosa cell tumor: mean 10.7 years for patients presenting with stage I and 4 months for one patient presenting with stage IIIC. Six patients relapsed 10 years after initial diagnosis. At the time of recurrence, eight patients presented with abdominal pain, one with palpable mass and the remaining two were diagnosed on regular follow-up imaging.
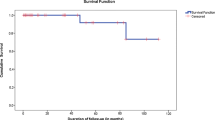
Four patients had one episode of recurrence and the remaining seven patients had two to six (mean = 2.8) episodes of recurrences requiring repeated surgical resections during the course of their disease. After the first recurrence, the mean time to a subsequent relapse in those who had achieved complete remission was 3.9 years. Four of 11 patients were dead of their disease progression. The mean survival was 21 years for three patients with stage I and 1 year for one patient with stage III. Five patients were alive at most recent follow up. The remaining two patients were lost to follow up.
Table 2 summarizes the imaging findings for 11 patients with recurrent granulosa cell tumors at the time of first recurrence. The number of recurrent masses detected on the images at first recurrence was single in three patients, two in five, three in one and more than five in two. All recurrent tumors were discrete round or lobulated except for two infiltrative masses (Fig. 1). The size of maximal diameter of recurrent tumors ranged from 2.5 to 9 cm (mean, 4.9 cm). The recurrent tumors were located in the intraperitoneal pelvis alone in three patients, intraperitoneal abdomen alone in two, both intraperitoneal pelvis and abdomen in three, and paraaortic retroperitoneal space (Figs. 2, 3) in three. The sites of the masses in the intraperitoneal abdomen were as follows: the subphrenic space (n = 2), the perihepatic space (n = 2), hepatorenal fossa (n = 2) and paracolic gutter (n = 1).
Case 11. Recurrent granulosa cell tumor in a 36-year-old woman who underwent total hysterectomy and bilateral salpingooophorectomy for stage IA tumor 6 years ago. A Contrast-enhanced CT scan shows two well-defined nodular soft tissue attenuation masses (arrows) in the pelvic cavity. Small amount of pelvic ascites (A) is present. B Contrast-enhanced CT scan at the level of the hepatic angle shows heterogeneous low attenuated mass infiltrating the hepatorenal fossa (arrows).
Case 8. Recurrent granulosa cell tumor in a 59-year-old woman who was diagnosed as stage IA tumor 16 years ago. A Contrast-enhanced CT scan shows a 4-cm mass of mixed solid and cystic nature (arrows) in the right infrarenal aortocaval space. Arrowhead = IVC. B Sagittal reformatted CT scan again shows a well-defined retroperitoneal mass (arrows) compressing the inferior vena cava (arrowheads).
Case 7. Recurrent granulosa cell tumor in a 47-year-old woman who was diagnosed as stage IA tumor 13 years ago. A Non-enhanced CT scan shows a 5-cm mass of heterogeneous low attenuation (arrows) with internal high attenuation in the left retroperitoneal space at the level of the lower pole of the kidney. B Contrast-enhanced CT scan shows no significant contrast enhancement in the retroperitoneal mass (arrows). Pathology confirmed recurrent granulosa cell tumor containing a large area of necrosis and hemorrhagic degeneration.
On CT, most recurrent masses with a diameter of less than 3 cm appeared as homogeneous low attenuation and those with a diameter of great than 3 cm showed heterogeneous attenuation. One patient (case 5) showed two homogeneous thin-walled unilocular cystic masses in the pelvic cavity. Three patients had single large retroperitoneal masses with a mean diameter of 6 cm (range 4–9 cm). Two masses were located in the right paraaortic space, and one in the left. Two retroperitoneal masses showed heterogeneously solid appearance with cystic portions. In one patient (case 7) with available non-enhanced CT scan, the retroperitoneal mass showed no significant contrast enhancement following administration of contrast material (Fig. 3). On pathologic examination, the recurrent mass showed a large area of necrosis containing hemorrhagic degeneration.
Of the three patients with MR imaging at the first time of recurrence, two patients had isointense solid masses, and one patient had multiple masses with variable configurations from predominantly cystic to predominantly solid tumors on T2-weighted images (Fig. 4). There were various degrees of contrast enhancement in the solid portion, septa, or cystic wall. In one patient (case 4) with follow-up MR imaging, the largest recurrent pelvic mass appeared as a well-defined mainly cystic mass with thick wall. The mass showed high signal intensity on T1-weighted image and mixed high and low signal intensity on T2-weighted image with a fluid-fluid level, a finding suggestive of intratumoral hemorrhage (Fig. 5). Smaller pelvic masses showed unilocular cystic appearance without evidence of hemorrhage.
Case 10. Recurrent granulosa cell tumor in a 30-year-old woman who underwent unilateral salpingo-oophorectomy for stage IC tumor 5 years ago. A Axial T2-weighted turbo spin-echo (TR/TE, 3500/132) MR image shows multiple variable-sized nodular recurrent masses (arrows) with very high signal intensity in both adnexal areas and cul-de-sac (arrows). Small amount of pelvic ascites is present. B Axial T1-weighted spin-echo (TR/TE, 522/14) MR image shows homogeneous low signal intensity of multiple masses (arrows). C Axial fat-saturated gadolinium-enhanced T1-weighted (TR/TE, 840/14) MR image shows various degrees of contrast enhancement in solid portion, septa, or cystic wall of multiple peritoneal seeding masses (arrows).
Case 4. Third episode of recurrent granulosa cell tumor in a 71-year-old woman who underwent unilateral salpingo-oophorectomy for stage IA tumor 26 years ago. A Contrast-enhanced CT scan shows a large well-defined cystic mass (arrow) with peripheral thick irregular wall (small arrows) along the right anterior margin of the mass in the pelvic cavity. Another two smaller nodular masses (arrows) are also seen in the left side of pelvic cavity. R = rectum. B Axial T1-weighted spin-echo (TR/TE, 470/14) MR image shows heterogeneous high signal intensity of the largest pelvic mass (arrow) to the right side of the rectum. Two smaller nodular masses (arrows) show homogeneous low signal intensity. C Axial T2-weighted turbo spin-echo (TR/TE, 4300/132) MR image shows mixed high and low signal intensity of the largest pelvic mass. Fluid-fluid level (short black arrows) is also seen, a finding suggestive of intratumoral hemorrhage. Two smaller nodular masses show homogeneous high signal intensity. The anterior one has thick peripheral wall. D Axial fat-saturated gadolinium-enhanced T1-weighted spin-echo (TR/TE, 736/14) MR image shows contrast enhancement in the cystic wall of multiple peritoneal seeding masses (arrows).
Small amount of pelvic ascites was present in two patients. However, pelvic lymphadenopathy, peritoneal thickening and omental cake were not seen in any patients.
Of the seven patients with multiple episodes of recurrences, two patients had recurrent tumors at the same site as on the previous occasion. But, the remaining five patients had recurrent tumors at the different sites from the previous sites. One patient (Case 3) had multiple distant metastastic masses in the liver parenchyma, lung and peritoneal cavity in the end.
Discussion
Granulosa cell tumors of the ovary represent in excess of 70% of malignant sex cord-stromal tumors, but it is an uncommon neoplasm, accounting for 2%–5% of all ovarian tumors [1]. This neoplasm is divided into adult and juvenile types based on different clinical and histopathologic features. Adult granulosa cell tumors are far more common than the juvenile type, accounting for 95% of all granulosa cell tumors. They occur predominantly in peri- and postmenopausal women, with peak prevalence in women aged 50–55 years [8].
Granulosa cell tumor is considered a low-grade malignancy. The overall 5-year-survival rate of granulosa cell tumor has been reported to be 80%–97%, contrary to the much less favorable 5-year-survival rate of 30%–35% in the patients with invasive epithelial ovarian neoplasms [5, 9]. The good prognosis of the tumor is partly related with early diagnosis due to hormone secretion by the tumor. The production of estrogen by granulosa cell tumors may cause vaginal bleeding in postmenopausal women and menstrual irregularity, menorrhagia, or even secondary amenorrhea in premenopausal women [2].
Granulosa cell tumor is also characterized by indolent, often unpredictable clinical course. Although patients with granulosa cell tumors generally present with stage I disease (78%–91%), relapses tend to occur in a more indolent fashion, often many years after the original diagnosis [2]. In our study, the mean time interval between the initial diagnosis and the first tumor recurrence was 9.7 years. Six out of 11 patients relapsed 10 years after the initial surgical resection of granulosa cell tumor. Hines et al. [10] reported a recurrence 37 years after initial diagnosis and, to our knowledge, it was the latest recurrence reported in the literature.
Relapse rates of 20%–26% have been reported in the larger studies. The studies with 30–100 cases had relapse rates ranging from 2% to 9% and from 34% to 40% [11]. In our study, relapse rate was 35%. This considerable variation may be explained by the variation in follow-up time and selection, and the retrospective design, which increases the risk of recall bias [11].
Generally, recurrent ovarian carcinoma manifests as pelvic masses in the surgical bed, peritoneal seeding, nodal recurrence and pleuropulmonary lesions, and liver metastasis. Peritoneal seeding presents as nodule or mass on the peritoneal surface, most commonly around the liver or cul-de-sac, and mesenteric or omental infiltration. Nodal recurrence appears as enlarged paraaortic nodes, especially at the renal hilar level [12]. The recurrent pathway of granulosa cell tumors observed in this study and previous study by MacSweeney [5] appears to be similar to that seen with epithelial ovarian cancers. Peritoneal seeding as nodules or infiltrative masses on the peritoneal surface, most commonly in the pelvic cavity or around the liver or undersurface of diaphragm was the most common manifestation of recurrent granulosa cell tumors. However, none of the patients showed omental or mesenteric infiltration and a large amount of ascites. Three of 11 patients had single recurrent tumor and nine had less than five recurrent masses at initial recurrence.
A single large retroperitoneal recurrent mass was seen in 3 of 11 patients. We presume retroperitoneal mass may represent lymphatic spread to paraaortic nodes, although none of our patients showed any other enlarged pelvic or abdominal lymphadenopathy. Because this malignant tumor is relatively slowly growing, a single metastastic mass can be growing to be quite large. Without knowing the patient’s remote history of ovarian granulosa cell tumor, the large retroperitoneal mass can be misdiagnosed as primary retroperitoneal tumors such as neurogenic tumor, retroperitoneal sarcoma, or malignant fibrous histiocytoma [13].
There have been several articles demonstrating the imaging findings of primary granulosa cell tumors [6, 8, 14]. The most recent study by Kim and Kim [6] demonstrated large multiseptated cystic mass and medium solid mass with internal cysts were two common forms of granulosa cell tumors and hemorrhage was a common MR finding, although nonspecific. Their study included two cases with recurrent granulosa cell tumors. In our study, recurrent granulosa cell tumors also showed variable imaging appearances from thin-walled unilocular cystic masses to solid masses, even though we could not correlate the imaging findings between the primary tumor and recurrent tumor because there were only two patients who had imaging studies performed prior to the initial surgery of primary granulosa cell tumors. Evidence of hemorrhage was clearly seen in one of four patients with MR imaging. Pathologically, three patients were proven to have hemorrhagic recurrent masses.
Our study has limitations. Because the disease entity is rare and has long duration of disease, the case number is small and this retrospective study limits detailed evaluation of imaging and surgical findings. This study included CT and MR scans obtained by using varying imaging techniques over the long period, and it was impossible to measure the CT attenuation of the tumor for the evaluation of solid or cystic nature of the mass. Imaging studies were not available at every time of recurrence in all patients.
In conclusion, recurrent ovarian granulosa cell tumor is characterized by late tumor recurrence manifested as a relatively small number of discrete peritoneal or retroperitoneal masses with nonexistent or small amount of ascites. Imaging findings of recurrent granulosa cell tumors are variable from solid masses to tumors with variable degrees of cystic portions to completely cystic tumors, like those of primary granulosa cell tumors. Because of the propensity of late tumor recurrence, any new peritoneal and retroperitoneal mass in the patients with previous history of granulosa cell tumor should be considered recurrent tumor until proven otherwise, even if the date of initial presentation is remote.
References
Stuart GC, Dawson LM (2003) Update on granulosa cell tumours of the ovary. Curr Opin Obstet Gynecol 15:33–37
Schumer ST, Cannistra SA (2003) Granulosa cell tumor of the ovary. J Clin Oncol 21:1180–1189
Pautier P, Lhomme C, Culine S, et al. (1997) Adult granulosa-cell tumor of the ovary: a retrospective study of 45 cases. Int J Gynecol Cancer 7:58–65
Crew KD, Cohen MH, Smith DH, et al. (2005) Long natural history of recurrent granulosa cell tumor of the ovary 23 years after initial diagnosis: a case report and review of the literature. Gynecol Oncol 96:235–240
MacSweeney JE, King DM (1994) Computed tomography, diagnosis, staging and follow-up of pure granulosa cell tumor of the ovary. Clin Radiol 49:241–245
Kim SH, Kim SH (2002) Granulosa cell tumor of the ovary: common findings and unusual appearances on CT and MR. J Comput Assist Tomogr 26:756–761
Coakley FV, Choi PH, Gougoutas CA, et al. (2002) Peritoneal metastases: detection with spiral CT in patients with ovarian cancer. Radiology 223:495–499
Outwater EK, Wagner BJ, Mannion C, et al. (1998) Sex cord-stromal and steroid cell tumors of the ovary. Radiographics 18:1523–1546
Stenwig JT, Hazelcamp JT, Beecham JB (1979) Granulosa cell tumors of the ovary. A clinicopathological study of 118 cases with long-term follow-up. Gynecol Oncol 7:136–152
Hines JF, Khalifa MA, Moore JL, et al. (1996) Recurrent granulosa cell tumor of the ovary 37 years after initial diagnosis: a case report and review of the literature. Gynecol Oncol 60:484–488
Lauszus FF, Petersen AC, Greisen J, et al. (2001) Granulosa cell tumor of the ovary: a population-based study of 37 women with stage I disease. Gynecol Oncol 81:456–460
Park CM, Kim SH, Kim SM, et al. (2003) Recurrent ovarian malignancy: patterns and spectrum of imaging findings. Abdom Imaging 28:404–415
Nishino M, Hayakawa K, Minami M, et al. (2003) Primary retroperitoneal neoplasms: CT and MR imaging findings with anatomic and pathologic diagnostic clues. Radiographics 23:45–57
Ko SF, Wan YL, Ng SH, et al. (1999) Adult ovarian granulosa cell tumors: spectrum of sonographic and CT findings with pathologic correlation. AJR 172:1227–1233
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Rha, S.E., Oh, S.N., Jung, S.E. et al. Recurrent ovarian granulosa cell tumors: clinical and imaging features. Abdom Imaging 33, 119–125 (2008). https://doi.org/10.1007/s00261-007-9197-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00261-007-9197-1