Abstract
Spontaneous regression of hepatocellular carcinoma is rare phenomenon. A 74-year-old man was found to have a hepatocellular carcinoma with intrahepatic metastases in the lateral segment of the liver. Before surgery, he developed severe cholangitis due to choledocholithiasis and was treated endoscopically. The tumor marker level decreased markedly, and hepatectomy was performed. The resected tumor demonstrated complete necrosis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Hepatocellular carcinoma (HCC) remains a life-threatening disease not only in Asians but also in Western populations, even though marked advances have been made in the past two decades in therapeutic methods including surgery, percutaneous approaches, and interventional therapy [1]. Spontaneous regression of HCC is an extremely rare phenomenon. To the best of our knowledge, only 15 cases of spontaneous complete regression of HCC have been reported in the English-language literature [2–15]. We describe a rare case of a patient with spontaneous complete necrosis and regression of HCC after cholangitis due to choledocholithiasis.
Case report
A 74-year-old man was admitted to a peripheral hospital in June 2003, with the chief complaint of epigastralgia. Abdominal imaging studies displayed a mass lesion in the left lobe of the liver, and the patient was referred to our hospital in July 2003.
Contrast-enhanced computed tomography (CT) demonstrated good enhancement of the tumor, which was 6 cm in diameter, in the lateral segment of the liver (Fig. 1A). Further, CT showed several nodules around the main tumor in the lateral segment of the liver and a clearly enhancing lesion measuring 1 cm in diameter on Cantlie line, all of which were diagnosed to be intrahepatic metastases. Hepatic angiogram also showed several tumor stains in the lateral segment and medial segment (segment 4) of the liver (Fig. 1B). Serologic tests for hepatitis B surface antigen (HBSAg), HBc, HBe, and hepatitis C virus antibodies were all negative, but the indocyanine green clearance test result at 15 min was 17.3%, suggestive of mild liver dysfunction. Maximum serum levels of α-fetoprotein and PIVKA-II were 2.7 ng/mL (normal range < 10 ng/mL) and 8450 mAU/mL (normal range < 40 mAU/mL), respectively. With the tentative diagnosis of HCC with multiple intrahepatic metastases, we scheduled limited resection of the liver and subsequent interventional therapy. Preoperative transcatheter embolization of the hepatic artery was not performed.
A Abdominal contrast-enhanced CT demonstrates an irregularly enhancing encapsulated tumor, 6 × 6 cm in diameter, in the lateral segment of the liver. B Hepatic angiography shows a large hypervascular tumor in the lateral segment of the liver (arrowhead), with small stains (black arrows) around it. In addition, a tumor stain, 1 cm in diameter, is visible in the medial segment zof the liver (white arrow).
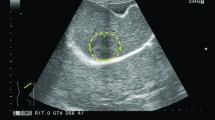
On August 18, 2003, before surgery, the patient developed severe cholangitis due to choledocholithiasis. The serum level of total bilirubin increased to 5.6 mg/dL. Immediately thereafter, endoscopic dilatation of the papilla of Vater and excretion of stones was performed. Abdominal CT 17 days after endoscopic therapy showed a decrease (5 cm in diameter) of the main tumor in the liver, a marked decrease in the degree of early enhancement, and an increase in the nonenhancing area of the tumor (Fig. 2). The small lesion on Cantlie line was no longer visualized. Further, the serum level of PIVKA-II decreased to 80 mAU/mL (Fig. 3). On September 22, 2003, laparotomy was conducted; the small intrahepatic metastasis on Cantlie line could not be visualized even by intraoperative ultrasonography. Therefore, limited resection of the lateral segment of the liver was performed.
Macroscopically, the resected specimen was an elastic, hard tumor that measured 5.0 × 5.0 cm. The cut surface showed areas of yellowish necrotic tissue and hemorrhage and a fibrous capsule (Fig. 4A). Microscopic examination demonstrated that the entire tumor had undergone coagulation necrosis, and ghosts of the tumor cells were arranged in a trabecular pattern, viewed especially clearly by reticulin staining (Fig. 4B). No viable cancer cells were found anywhere in the lesion; therefore, complete necrosis of the HCC was diagnosed. Some granulomatous lesions with inflammatory cell infiltration were found in the noncancerous liver tissue around the main tumor, which were probably derived from the cholangitis caused by choledocholithiasis (Fig. 4C). Interestingly, some vessels feeding the tumor were thickened and occluded due to arterial sclerosis (Fig. 4D).
A The cut surface of the resected specimen consists of two parts: a yellowish necrotic appearance (left) and a reddish appearance with hemorrhage (right). B Histologic examination shows coagulation necrosis of the entire tumor, and ghosts of the tumor cells are arranged in a trabecular pattern, viewed especially well by reticulin staining (reticulin silver impregnation, 200 ×). C Several granulomatous lesions with inflammatory cell infiltration are seen in the on-cancerous liver tissue around the tumor (hematoxylin and eosin stain, 100×). D The wall of the arteries feeding the tumor is thickened. The vessels are occluded due to arterial sclerosis (hematoxylin and eosin stain, 40×).
The postoperative course of the patient was uneventful and he was discharged on postoperative day 10. Follow-up angiography and CT in November 2003 did not demonstrate the intrahepatic metastasis on Cantlie line. At the time of writing, 1 year after surgery, the patient continues to do well without signs of recurrence.
Discussion
We have reported a very rare case of spontaneous regression of HCC with complete necrosis. Complete regression of the HCC and the intrahepatic metastases was confirmed by examination of the surgically resected specimen and by imaging studies. Among the 15 cases of spontaneous regression of HCC reported until now [2–15], regression was confirmed by histopathologic examination of the surgical specimen in only six cases [5, 10–12, 14, 15]. In three cases, the primary HCC and the metastatic tumors in the bone or lung had regressed simultaneously [3, 4, 8]. However, regression of intrahepatic metastases had never been reported until now.
The imaging features of spontaneous regression of HCC are not uniform. In the present case, the early enhancement of the originally viable HCC lesion diminished after possible spontaneous regression; however, a conclusive diagnosis of complete necrosis of the tumor could not be made by imaging studies alone. Ozeki et al. also observed a decrease in the degree of enhancement in a HCC tumor and subsequently demonstrated that the tumor had undergone complete necrosis [10]. Izuishi et al. described loss of enhancement on CT and hypovascularity on angiogram of a HCC that had undergone massive necrosis [12]. Chien et al. reported complete disappearance of a large HCC, 12 cm in diameter, on CT during a 2-year follow-up period [9]. Thus, regressed HCCs exhibit various patterns on imaging studies. A high index of suspicion of spontaneous regression of HCC, occasionally from the decrease in serum levels of tumor markers, and repeated imaging examinations by multiple imaging modalities may lead to a correct diagnosis.
The possible causes of spontaneous regression of HCC are diverse and currently under debate; some of the proposed mechanisms are as follows: an immune mechanism such as excessive production of cytokines such as tumor necrosis factor-α and interluekin-8 in relation to inflammation or infection [11, 16, 17]; perfusion injury such as massive gastrointestinal bleeding or spasm of the hepatic artery that decreases the blood supply to the tumor [6, 7]; endocrine factors such as withdrawal of androgen therapy [5]; and effects of herbal medicines [3]. In the present case, we believe that cholangitis due to choledocholithiasis and the consequent ischemia led to the spontaneous regression. In other words, inflammatory reactions and perfusion injury might play important roles in the spontaneous regression of HCC. This theory is supported by the histopathologic findings that necrosis of the HCC in the reported case was accompanied by an inflammatory reaction, sclerosis, and occlusion of the arteries feeding the tumor.
In conclusion, a rare case of spontaneous regression of HCC with complete necrosis is presented. The possible cause was severe cholangitis after choledocholithiasis. Surgical resection was successful, and the patient is well 1 year after surgery, without evidence of recurrence.
References
JM Llovet A Burroughs J Bruix (2003) ArticleTitleHepatocellular carcinoma Lancet 362 1907–1917 Occurrence Handle10.1016/S0140-6736(03)14964-1 Occurrence Handle14667750
EB Gottfried R Steller F Paronetto CS Lieber (1982) ArticleTitleSpontaneous regression of hepatocellular carcinoma Gastroenterology 82 770–774 Occurrence Handle6174388 Occurrence Handle1:STN:280:DyaL387jvF2msA%3D%3D
KC Lam JCI Ho RTT Yeung (1982) ArticleTitleSpontaneous regression of hepatocellular carcinoma Cancer 50 332–336 Occurrence Handle6282440 Occurrence Handle1:STN:280:DyaL383gvVWrtw%3D%3D
Y Sato K Fujiwara S Nakagawa et al. (1985) ArticleTitleA case of spontaneous regression of hepatocellular carcinoma with bone metastasis Cancer 56 667–671 Occurrence Handle2408740 Occurrence Handle1:STN:280:DyaL2M3isl2hug%3D%3D
GW McCaughan MJ Bilous ND Gallagher (1985) ArticleTitleLong-term survival with tumor regression in androgen-induced liver tumor Cancer 56 2622–2626 Occurrence Handle2996742 Occurrence Handle1:STN:280:DyaL28%2FislKnuw%3D%3D
A Tocci Conte G P Guarascio G Visco (1990) ArticleTitleSpontaneous remission of hepatocellular carcinoma after massive gastrointestinal haemorrhage Br Med J 300 641–642
MJ Gaffey JP Joyce GS Carlson JM Esteban (1990) ArticleTitleSpontaneous regression of hepatocellular carcinoma Cancer 65 2779–2783 Occurrence Handle2160319 Occurrence Handle1:STN:280:DyaK3c3lsVGmuw%3D%3D
RC Ayres DAF Robertson KC Dewbury et al. (1990) ArticleTitleSpontaneous regression of hepatocellular carcinoma Gut 31 722–724 Occurrence Handle2165992 Occurrence Handle1:STN:280:DyaK3czjslCnsg%3D%3D
RN Chien TJ Chen YF Liaw (1992) ArticleTitleSpontaneous regression of hepatocellular carcinoma Am J Gastroenterol 87 903–905 Occurrence Handle1319672 Occurrence Handle1:STN:280:DyaK38zht1KjsA%3D%3D
Y Ozeki N Matsubara K Tateyama et al. (1996) ArticleTitleSpontaneous complete necrosis of hepatocellular carcinoma Am J Gastroenterol 91 391–392 Occurrence Handle8607516 Occurrence Handle1:STN:280:DyaK287ptVSjuw%3D%3D
S Markovic V Ferlan-Marolt Z Hlebanja (1996) ArticleTitleSpontaneous regression of hepatocellular carcinoma Am J Gastroenterol 91 392–393 Occurrence Handle8607517 Occurrence Handle1:STN:280:DyaK287ptVSisg%3D%3D
K Izuishi M Ryu T Hasebe et al. (2000) ArticleTitleSpontaneous total necrosis of hepatocellular carcinoma: report of a case Hepatogastroenterology 47 1122–1124 Occurrence Handle11020894 Occurrence Handle1:STN:280:DC%2BD3cvmslGisg%3D%3D
TJ Jang JI Lee DH Kim et al. (2000) ArticleTitleSpontaneous regression of hepatocellular carcinoma—a case report Korean J Intern Med 15 147–150 Occurrence Handle10992730 Occurrence Handle1:STN:280:DC%2BD3cvktl2nsw%3D%3D
Y Morimoto Y Tanaka T Itoh et al. (2002) ArticleTitleSpontaneous necrosis of hepatocellular carcinoma: a case report Dig Surg 19 413–418 Occurrence Handle12435917
AJ Li MC Wu WM Cong et al. (2003) ArticleTitleSpontaneous complete necrosis of hepatocellular carcinoma: a case report Hepatobiliary Pancreat Dis Int 2 152–154 Occurrence Handle14607670
K Ohba K Omagari T Nakamura et al. (1998) ArticleTitleAbscopal regression of hepatocellular carcinoma after radiotherapy for bone metastasis Gut 43 575–577 Occurrence Handle9824589 Occurrence Handle1:STN:280:DyaK1M%2FntFagtg%3D%3D Occurrence Handle10.1136/gut.43.4.575
S Abiru Y Kato K Hamasaki et al. (2002) ArticleTitleSpontaneous regression of hepatocellular carcinoma associated with elevated levels of Interleukin 18 Am J Gastroenterol 97 774–775 Occurrence Handle10.1111/j.1572-0241.2002.05580.x Occurrence Handle11922591
Acknowledgment
This study was supported in part by Grant-in-Aid for scientific research from the Ministry of Education, Science and Culture, and the Ministry of Health and Welfare of Japan.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ohta, H., Sakamoto, Y., Ojima, H. et al. Spontaneous regression of hepatocellular carcinoma with complete necrosis: case report. Abdom Imaging 30, 734–737 (2005). https://doi.org/10.1007/s00261-005-0313-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00261-005-0313-9