Abstract
Purpose
The aim of this study was to explore the role of [68Ga]Ga-DOTA-FAPI-04 positron emission tomography/computed tomography (PET/CT), compared with 18F-fluorodeoxyglucose [18F]-FDG PET/CT, for evaluating peritoneal carcinomatosis in patients with various types of cancer.
Methods
Patients with suspected peritoneal malignancy, who underwent both [18F]-FDG and [68Ga]Ga-DOTA-FAPI-04 PET/CT between October 2019 and August 2020, were retrospectively analysed. The radiotracer uptake, peritoneal cancer index (PCI) score, and diagnostic performance of [18F]-FDG and [68Ga]Ga-DOTA-FAPI-04 PET/CT were evaluated and compared.
Results
Our cohort consisted of 46 patients, including 16 patients with diffuse-type peritoneal carcinomatosis, 27 with nodular-type peritoneal carcinomatosis, and 3 true-negative patients. A significant difference in standard uptake values (SUV) of lesions between [18F]-FDG and [68Ga]Ga-DOTA-FAPI-04 PET/CT examination was observed (median SUV: 3.48 vs. 9.82; P < 0.001), particularly in peritoneal carcinomatosis from gastric cancer (median SUV: 3.44 vs. 8.05; P = 0.001). Moreover, [68Ga]Ga-DOTA-FAPI-04 PET/CT showed a higher PCI score and better sensitivity than [18F]-FDG PET/CT for the detection of peritoneal carcinomatosis (6 vs. 18; P < 0.001; 72.09% vs. 97.67%; P = 0.002).
Conclusion
[68Ga]Ga-DOTA-FAPI-04 PET/CT demonstrated superior sensitivity over [18F]-FDG PET/CT for the detection of peritoneal carcinomatosis in patients with various types of cancer, particularly gastric cancer. Furthermore, the uptake of [68Ga]Ga-DOTA-FAPI-04 in peritoneal carcinomatosis was significantly higher than that of [18F]-FDG, demonstrating a larger extent of the lesions and yielding a higher PCI score. This could help enhance the image contrast, improve physicians’ diagnostic confidence, and reduce the proportion of missed diagnoses.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Tumour metastasis remains a major challenge in cancer treatment, and about 90% of cancer deaths are caused by metastatic disease [1]. Peritoneal carcinomatosis mainly refers to metastatic malignant spread to the peritoneum, mostly from gastric, colorectal, and ovarian cancers. In addition to secondary causes, several types of peritoneal carcinomatosis arise from primary peritoneal cancer. Peritoneal carcinomatosis was previously considered to be a terminal condition [2]; however, the application of cytoreductive surgery and hyperthermic intraperitoneal chemotherapy has significantly improved the long-term survival [3, 4]. Treatment using pressurised intraperitoneal aerosol chemotherapy and intraperitoneal MOC31PE immunotoxin has also shown promising results in recent years [5, 6].
Beyond these multi-modal treatments, precise evaluation of peritoneal carcinomatosis is the critical determining factor in the selection of appropriate therapy. In post-treatment patients, detection of tumour recurrence is essential for subsequent management. Clinical imaging techniques, such as computed tomography (CT), magnetic resonance imaging (MRI), and 18F-fluorodeoxyglucose (FDG) positron emission tomography (PET)/CT, have routinely been used to evaluate the extent and volume of peritoneal carcinomatosis. Although CT is recommended as the primary modality for peritoneal carcinomatosis detection, its efficacy could be compromised in low-volume tumours [7, 8]. It also remains unconfirmed whether MRI improves lesion evaluation [9, 10]. With a high accuracy for detection of primary lesions and distant metastases, [18F]-FDG PET/CT has markedly improved the staging and restaging of various cancers [11]. However, several types of gastrointestinal cancer, including signet ring cell carcinoma and mucinous adenocarcinoma, are not [18F]-FDG-avid tumours. Additionally, physiological uptake of [18F]-FDG is often observed in the intestinal tract, resulting in difficulty of obtaining images of lesions with sufficient contrast in this area. Overall, the diagnostic impact of [18F]-FDG for the detection of peritoneal carcinomatosis is reported to be low [12,13,14,15].
Cancer-associated fibroblasts (CAFs) are an indispensable factor in tumour growth and progression, and CAFs and extracellular fibrosis make a major contribution to the gross tumour mass [16]. Fibroblast activation protein (FAP) is overexpressed in CAFs of many epithelial cancers and is rarely expressed in normal tissues [17]. Thus, targeting FAP is a promising approach for tumour imaging in various types of cancer [18, 19]. In our previous studies, [68Ga]Ga-DOTA-FAPI-04 PET/CT demonstrated superior diagnostic efficacy compared to that of [18F]-FDG PET/CT for the detection of primary and metastatic lesions in various types of cancer, particularly for identifying peritoneal carcinomatosis [20, 21]. The impressive diagnostic performance of this modality encouraged us to explore the usefulness of [68Ga]Ga-DOTA-FAPI-04 PET/CT further for the detection of peritoneal carcinomatosis in various types of cancer.
We sought to investigate the role of [68Ga]Ga-DOTA-FAPI-04 PET/CT in the evaluation of peritoneal carcinomatosis in patients with various types of cancer and to compare it with that of [18F]-FDG PET/CT.
Materials and methods
Patients
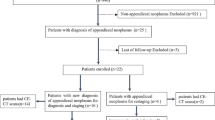
This is a post hoc retrospective analysis of a sub-cohort of patients from a previously prospectively acquired database, namely the patient data screened in a study that was registered at ClinicalTrials.gov (NCT04416165) and was approved by the Clinical Research Ethics Committee of the First Affiliated Hospital of Xiamen University. The study was conducted in accordance with the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards. With agreement from the oncologists and on determination of the patients’ eligibility, patients were recruited for enrolment in the study, from October 2019 through August 2020, at our institute. Written informed consent was obtained from all included patients. The following patients were included: (i) patients with suspected peritoneal malignancy based on diagnostic imaging (CT and MRI) and clinical symptoms; (ii) patients who had undergone both [18F]-FDG and [68Ga]Ga-DOTA-FAPI-04 PET/CT scans within 1 week of each other; (iii) patients previously treated with chemo/radio/targeted therapy, the time interval between completion of therapy and PET/CT scan being more than half a year (to avoid the treatment impact on radiotracer uptake). We excluded patients whose treatment had already started before the [68Ga]Ga-DOTA-FAPI-04 PET/CT scan and those with incomplete histopathological or clinical data. Histopathological findings obtained from biopsy or resected surgical specimens were used as a reference for final tumour diagnosis. If tissue diagnosis was not applicable, we requested clinical and/or imaging follow-up data, including the results of physical examination, laboratory tests, and medical imaging, which were obtained after the PET/CT scans were performed. Lesions were considered malignant based on any of the following follow-up criteria: (i) typical malignant features confirmed by multi-modal medical imaging, (ii) significant progression on follow-up imaging, or (iii) a significant post-treatment tumour size decrease. The minimum follow-up period was 3 months. Patients who died or were lost to follow-up were excluded from the analysis.
Preparation of [18F]-FDG and [68Ga]Ga-DOTA-FAPI-04
[18F]-FDG was manufactured in accordance with the standard method described by our laboratory using the coincidence [18F]-FDG synthesis module (TracerLab FxFN, GE Healthcare, St Giles, UK) [22]. Labelling of [68Ga]Ga-DOTA-FAPI-04 was performed according to a previously described protocol [20]. Quality control of the radiosynthesis of both tracers was performed by ultraviolet and radio-high-performance liquid chromatography. The radiochemical purity exceeded 95% for both [18F]-FDG and [68Ga]Ga-DOTA-FAPI-04, and the final product was sterile.
PET/CT imaging
Patients who underwent [18F]-FDG PET/CT were required to fast for at least 6 h prior to the examination. The dose of intravenously injected [18F]-FDG and [68Ga]Ga-DOTA-FAPI-04 was calculated according to the patient’s weight (3.7 MBq/kg for FDG; 1.8–2.2 MBq/kg for FAPI). Data were acquired using a hybrid PET/CT system (Discovery MI, GE Healthcare) at 1 h after intravenous radiotracer administration. All the scans were performed according to a previously described protocol [20, 21]. All obtained data were transferred to the Advantage Workstation (version AW 4.7, GE Healthcare) and reconstructed using the Bayesian penalised likelihood reconstruction algorithm (Q.clear, GE Healthcare), with a penalisation factor (beta) of 500. The reconstructed images were then co-registered and displayed.
PET/CT imaging review
Fused PET/CT images were viewed on the Advantage Workstation (version AW 4.7, GE Healthcare). Both [18F]-FDG and [68Ga]Ga-DOTA-FAPI-04 PET/CT scans were interpreted by two board-certified nuclear medicine physicians. To prevent any bias, studies were reviewed in groups according to the tracer used. All [18F]-FDG PET/CT images were reviewed as group 1 (reviewed by H.C and L.Z, with 10 and 16 years of experience in nuclear oncology, respectively), and [68Ga]Ga-DOTA-FAPI-04 PET/CT images were reviewed as group 2 (reviewed by Z.L and L.S, with 12 and 15 years of experience in nuclear oncology, respectively). Reviews were performed in the absence of clinical data (including CT, MRI, and histopathological results) and information from the other PET/CT scan. Any difference of opinion was resolved by consensus.
On transaxial images, regions-of-interest (ROIs) were drawn around the tumour lesions for semiquantitative analysis. The maximum standard uptake values (SUV) were automatically calculated and used to quantify tracer uptake in peritoneal carcinomatosis lesions. The maximum SUVs, median, and range were recorded for both [18F]-FDG and [68Ga]Ga-DOTA-FAPI-04 PET/CT images. Patterns of peritoneal carcinomatosis were classified into either omental cake type (diffuse type) or nodular type. CT images were used as reference to distinguish diffuse pattern from physiological intestinal uptake and nodular pattern from hypermetabolic lymph nodes. For diffuse-type peritoneal carcinomatosis, only the lesion SUVs were recorded. For nodular-type peritoneal carcinomatosis, both SUV and nodular size (cm) were recorded. The results were considered positive if the lesion activity exceeded that of the adjacent background tissues (visual interpretation). If multiple positive lesions were present in one patient, the average SUV was calculated, which was obtained by averaging the SUVs of all lesions or the SUVs of the five largest lesions (> 5 lesions). CT images were used as reference to ensure the SUVs were measured from the same lesions from two different image sets.
The peritoneal cancer index (PCI) of each individual (based on PET/CT images and using similar estimation method for all patients) was used to assess the extent of peritoneal carcinomatosis in the peritoneal cavity, which was quantified by assessing Sugarbaker’s 13 regions and the corresponding lesion sizes [23, 24].
Statistical analyses
All statistical analyses were conducted using SPSS 22.0 statistical analysis software (IBM, Armonk, NY, USA). The Wilcoxon matched-pairs signed-rank test was used to compare the SUVs derived from [18F]-FDG and [68Ga]Ga-DOTA-FAPI-04 PET/CT images. The same test was used to compare PCI-FDG and PCI-FAPI. For categorical variables, McNemar’s test, the chi-squared test, Yates’ correction of the chi-squared test, or Fisher’s exact test was used to analyse the differences between groups. The results of the visually interpreted PET/CT images were compared with the histopathological results (obtained via biopsy or surgery) or follow-up data, which were used as the reference standard. The sensitivity of [18F]-FDG and [68Ga]Ga-DOTA-FAPI-04 PET/CT was calculated to evaluate the diagnostic performance of both modalities. Two-tailed P values < 0.05 were considered significant.
Results
Characteristics of the patients
Between October 2019 and August 2020, 47 patients with suspected peritoneal malignancy underwent paired [18F]-FDG and [68Ga]Ga-DOTA-FAPI-04 PET/CT scans. One patient was excluded from the analysis due to loss to follow-up. Of the 46 included patients, 14 were male and 32 were female, and the median age of the patients was 57 years (range, 32–80 years). The final diagnosis, based on surgical exploration (n = 11), image-guided percutaneous biopsy (n = 16), and radiographic follow-up (n = 19), showed that 43 patients had peritoneal malignancy and 3 patients did not. Of the 43 patients with peritoneal malignancy, 1 patient was diagnosed with primary peritoneal carcinoma (diffuse malignant peritoneal mesothelioma) and the remaining 42 patients had peritoneal carcinomatosis. In most cases, the primary site of peritoneal carcinomatosis was the gastrointestinal tract, which included 13 gastric cancer, 10 colorectal cancer, and 6 pancreatic cancer cases. Twenty-one patients had newly diagnosed malignancy in stage IV and the remaining 22 patients had recurrent disease. The median follow-up time was 6.8 months (range, 3.5–9.5 months). The characteristics of the patients are shown in Table 1.
PET/CT patterns of peritoneal carcinomatosis
Among the 43 patients with peritoneal tumours, two different patterns of tracer uptake were observed on [68Ga]Ga-DOTA-FAPI-04 (42 PET-positive cases) and [18F]-FDG PET/CT (31 PET-positive cases), which suggested two different forms of malignant tumour invasion. An omental-cake-type (diffuse type) pattern was observed in 16 patients, corresponding to diffuse and infiltrative peritoneal involvement. The remaining 27 patients demonstrated a nodular-type pattern, corresponding to focal and nodular peritoneal involvement. Representative PET images of the two types of peritoneal carcinomatosis are presented in Fig. 1.
The representative [68Ga]Ga-DOTA-FAPI-04 PET maximum intensity projection images of the diffuse type of peritoneal carcinomatosis and nodular-type of peritoneal carcinomatosis. a Patient with diffuse type of peritoneal carcinomatosis. The abnormal activity in the upper part of the body is from enlarged internal mammary lymph nodes, right hilar lymph nodes, and cardiophrenic angle lymph nodes (highly suggestive of metastatic lymph nodes). b Patient with nodular-type of peritoneal carcinomatosis. The abnormal activity in the upper part of the body is from enlarged right supraclavicular lymph nodes, internal mammary lymph nodes, hilar lymph nodes, and cardiophrenic angle lymph nodes (highly suggestive of metastatic lymph nodes)
Comparison of FAPI and FDG uptake in peritoneal carcinomatosis
There was a significant difference in the SUVs of lesions between [18F]-FDG and [68Ga]Ga-DOTA-FAPI-04 PET/CT (3.48 vs. 9.82; P < 0.001) (Table 2). Specifically, these lesions showed significantly lower uptake of [18F]-FDG than that of [68Ga]Ga-DOTA-FAPI-04 in the following malignancies: (i) gastric cancer (median SUV: 3.44 vs. 8.05; P = 0.001); (ii) colorectal cancer (median SUV: 3.86 vs. 10.14; P = 0.028); (iii) ovarian cancer (median SUV: 5.37 vs. 11.77; P = 0.011); and (iv) pancreatic cancer (median SUV: 3.31 vs. 7.80; P = 0.028) (Table 2). In addition, we noted that among all cancer types, gastric and pancreatic cancer showed the lowest FDG uptake in peritoneal carcinomatosis. A representative case showing the different SUVs of peritoneal carcinomatosis in the two types of scans is presented in Fig. 2.
A 57-year-old woman with newly diagnosed ovarian carcinoma underwent [18F]-FDG and [68Ga]Ga-DOTA-FAPI-04 PET/CT for tumour staging before treatment. [68Ga]Ga-DOTA-FAPI-04 PET/CT (a) shows higher tracer uptake (SUV, 21.6–22.1 vs. 8.9–10.0) compared to that of [18F]-FDG PET/CT (b) in peritoneal carcinomatosis. SUV, standard uptake value; PET/CT, positron emission tomography/computed tomography
Comparison of the peritoneal cancer index between the two scans
Among the 43 patients, the median PCI score derived from [18F]-FDG PET/CT was 6 (range, 0–29), whereas it was 18 (range, 0–39) when derived from [68Ga]Ga-DOTA-FAPI-04 PET/CT. The PCI score in gastric cancer, ovarian cancer, and pancreatic cancer for each patient was markedly lower in [18F]-FDG than in [68Ga]Ga-DOTA-FAPI-04 PET/CT (median PCI: 2 (range, 0–16) vs. 17 (range, 2–39); P = 0.002; 10 (range, 0–26) vs. 20 (range, 0–32); P = 0.028; 4 (range, 0–29) vs. 16 (range, 6–36); P = 0.028, respectively). Although no statistically significant difference was found, colorectal cancer showed greater PCI scores in [68Ga]Ga-DOTA-FAPI-04 than in [18F]-FDG PET/CT. When the patients were classified into two categories based on a cut-off PCI value of 20, [18F]-FDG PET/CT imaging showed that the number of patients with PCI > 20 in gastric cancer, colorectal cancer, ovarian cancer, pancreatic cancer, and other types of cancer was 0, 0, 1, 1, and 3, respectively. In contrast, for [68Ga]Ga-DOTA-FAPI-04 imaging, the corresponding numbers of patients were 5, 1, 4, 2, and 7, respectively. In total, the number of patients with PCI > 20 based on [68Ga]Ga-DOTA-FAPI-04 PET/CT examination was markedly higher than that based on [18F]-FDG PET/CT examination (5 vs. 19; P < 0.001). A representative case with differences in PCI scores between the two scans is presented in Fig. 3.
A 58-year-old woman who was diagnosed with ovarian cancer based on cytology of her ascitic fluid. [68Ga]Ga-DOTA-FAPI-04 PET/CT shows intense FAPI uptake in the omental-cake-type pattern of peritoneal carcinomatosis and peritoneal surfaces (a). [18F]-FDG PET/CT shows peritoneal carcinomatosis with low to moderate activity throughout the abdomen and pelvis (b). [68Ga]Ga-DOTA-FAPI-04 PET/CT shows larger lesion extent than [18F]-FDG PET/CT for peritoneal carcinomatosis. Therefore, the PCI score derived from [68Ga]Ga-DOTA-FAPI-04 PET/CT is much higher than that from [18F]-FDG PET/CT (PCI-FAPI vs. PCI-FDG, 27 vs. 9). The patient subsequently underwent a computed tomography–guided biopsy of the cake-shaped omentum with intense FAPI uptake, which further confirmed the peritoneal carcinomatosis from ovarian cancer
Diagnostic performance of FDG and FAPI PET/CT in peritoneal carcinomatosis
Peritoneal carcinomatosis was detected by [18F]-FDG PET/CT in 31 of 43 patients, leading to a sensitivity of 72.09%, while the sensitivity of [68Ga]Ga-DOTA-FAPI-04 PET/CT for the diagnosis of peritoneal carcinomatosis was 97.67% (P = 0.002, Table 3). Specifically, the diagnostic performance of [18F]-FDG PET/CT was the worst in gastric cancer, with a sensitivity of 53.85% (7/13), compared with 100% (13/13) for [68Ga]Ga-DOTA-FAPI-04 PET/CT (P = 0.015). Among the 6 patients with gastric cancer presenting negative [18F]-FDG PET findings, 4 of 6 were diagnosed with gastric signet ring cell carcinomas (GSRCC). A significant difference was observed in positive FDG PET findings between signet ring cell carcinoma and adenocarcinoma (P = 0.021). Importantly, [68Ga]Ga-DOTA-FAPI-04 PET/CT showed intense uptake in peritoneal carcinomatosis in all patients with gastric cancer, including in GSRCC. A representative case comparing the two scans for peritoneal carcinomatosis from signet ring cell carcinomas is presented in Fig 4. In addition, [18F]-FDG PET/CT showed relatively lower sensitivity in colorectal cancer (71.43%) and pancreatic cancer (66.67%) than in [68Ga]Ga-DOTA-FAPI-04 PET/CT (100%). Out of the 46 cases of suspected peritoneal malignancy, 4 patients showed negative results on [68Ga]Ga-DOTA-FAPI-04 PET/CT. Final diagnosis by surgical exploration (n = 2) and radiographic follow-up (n = 2) confirmed peritoneal carcinomatosis in only 1 patient. These findings yielded 3 true-negative and 1 false-negative case with [68Ga]Ga-DOTA-FAPI-04 PET/CT. [18F]-FDG PET/CT gave 3 true-negative and 12 false-negative results. Thus, the negative predictive values were 75% (3/4) and 20% (3/15) for [68Ga]Ga-DOTA-FAPI-04 and [18F]-FDG PET/CT, respectively (Table 3). Due to the limited number of cases in this study, we were unable to obtain the PET/CT data of false-positives. Therefore, the specificity and positive-predictive value could not be established in this study.
A 44-year-old man with a history of gastrectomy for gastric signet ring cell carcinoma presented with symptoms of abdominal pain and rising carcinoembryonic antigen levels. He underwent PET/CT scan to detect recurrence. [68Ga]Ga-DOTA-FAPI-04 PET/CT images show intense activity throughout the abdomen and pelvis, especially around the liver and small bowel mesenterium (a). However, [18F]-FDG PET/CT images revealed much lower tracer uptake in these regions (b). PET/CT, positron emission tomography/computed tomography
Among the 16 patients with omental-cake-type pattern of peritoneal carcinomatosis, [68Ga]Ga-DOTA-FAPI-04 PET/CT was positive in all 16 patients, while [18F]-FDG PET/CT was positive in 13 of the 16 patients. Moreover, the extent of lesions on [68Ga]Ga-DOTA-FAPI-04 PET/CT was significantly greater than that on [18F]-FDG, which was reflected by the greater PCI score derived from [68Ga]Ga-DOTA-FAPI-04 PET/CT (median PCI, 16 vs. 32, P < 0.001). Regarding the other 27 patients with nodular-type peritoneal carcinomatosis, [68Ga]Ga-DOTA-FAPI-04 PET/CT was positive in 26 of 27 patients, while [18F]-FDG PET/CT was positive in 18 of the 27 patients. Lesion-by-lesion analysis was further performed in this patient group, with a total number of 124 nodular lesions evaluated (those lesions which were visible on the CT images and were confirmed by surgical exploration or radiographic follow-up). The median lesion size for the 124 lesions was 1.12 cm (range, 0.34–3.67 cm). The [18F]-FDG PET-positive lesions had mostly a large volume of disease (median, 1.64 cm; 0.74–3.67 cm), with involvement of tumour into the adjacent soft tissues, such as the omentum, mesentery, and fibroadipose tissue. In contrast, [18F]-FDG PET-negative lesions demonstrated low-volume disease, and the peritoneal implants from these patients were relatively small, ranging from 0.34 to 3.42 cm (median 1.01 cm). Less than half of the nodular-type lesions (49/124) were detected by [18F]-FDG PET, resulting in a sensitivity of 39.52%. When the cut-off value of the lesion size was set at 1.34 cm, according to the receiver operating curve, the detection performance of [18F]-FDG PET/CT showed statistically significant differences in terms of tumour size (P < 0.001). Impressively, most of the nodular-type lesions (115/124) were detected by [68Ga]Ga-DOTA-FAPI-04 PET/CT, which yielded a significantly higher sensitivity (92.74%) than that of [18F]-FDG PET/CT for the detection of nodular-type lesions (P < 0.001). The representative case of nodular-type peritoneal carcinomatosis on the two PET scans is presented in Fig. 5.
A 61-year-old man with newly diagnosed pancreatic cancer underwent PET/CT scan for tumour staging. On the images of [68Ga]Ga-DOTA-FAPI-04 PET/CT, numerous nodules with intense activity are observed scattered throughout the abdomen and pelvis (upper row, lesions in the liver capsule, dotted arrow; middle row, lesions in the mesenterium, solid arrow; lower row, lesions in the pelvis, solid arrow) (a). In addition, abnormal [68Ga]Ga-DOTA-FAPI-04 activity is observed in the upper part of the body, located in the sternum, thickened pleura, and enlarged internal mammary lymph nodes (highly suggestive of metastatic lesions). However, [18F]-FDG PET/CT demonstrated negative or minimal uptake in these nodular-type lesions (b). PET/CT, positron emission tomography/computed tomography
Furthermore, debulking surgery was performed in 9 patients (4 patients with diffuse-type and 5 patients with the nodular-type peritoneal carcinomatosis), during which multiple small carcinoma nodules were observed on the peritoneal and mesenteric surfaces, which were consistent with the [68Ga]Ga-DOTA-FAPI-04 PET/CT findings (Fig. 6).
a, b A 45-year-old woman with a history of bilateral salpingo-oophorectomy for ovarian cancer presented with symptoms of abdominal pain and rising cancer antigen 125 levels. She underwent PET/CT scan for recurrence detection. Both [68Ga]Ga-DOTA-FAPI-04 and [18F]-FDG PET/CT showed multiple small nodules with intense activity in the liver capsule (upper row, white dotted arrow), mesocolon adjacent to the ascending colon (middle row, white and blue solid arrows), and ileocecal junction (lower row, green solid arrow). Moreover, [68Ga]Ga-DOTA-FAPI-04 PET/CT revealed another small nodule with intense activity in the pelvis (lower row, green dotted arrow), which was not visualised on [18F]-FDG PET/CT. The patient subsequently underwent a debulking procedure, during which multiple small carcinoma nodules were observed on the peritoneal and mesenteric surfaces, which is consistent with the [68Ga]Ga-DOTA-FAPI-04 PET/CT findings (c). PET/CT, positron emission tomography/computed tomography
Discussion
This retrospective study investigated the role of [68Ga]Ga-DOTA-FAPI-04 PET/CT in the evaluation of peritoneal carcinomatosis and compared it with [18F]-FDG PET/CT. The results of our study demonstrated that peritoneal carcinomatosis lesions show a higher uptake of [68Ga]Ga-DOTA-FAPI-04 than that of [18F]-FDG, providing a more sensitive and accurate diagnosis of peritoneal carcinomatosis. Moreover, [68Ga]Ga-DOTA-FAPI-04 PET/CT may be more useful than [18F]-FDG PET/CT for delineating the extent of lesions in patients with peritoneal carcinomatosis, especially in patients with gastric, pancreatic, and colorectal cancer. This could be helpful in preoperative assessments of cancer distribution and might be used as a prognostic factor of survival.
Peritoneal carcinomatosis often involves low-volume lesions; individual lesions may be small and few in number and may vary in gross morphology, developing as flat plaques, large sheets, discrete masses, or small nodules [25]. Early disease may involve microscopic lesions and may be limited to the ascitic fluid. More advanced disease may extend along the parietal peritoneum, stud visceral surfaces, or cause omental or mesenteric caking [26], but research in this field is limited.
[18F]-FDG PET/CT, the imaging modality most widely used in oncology, has a significant impact on tumour staging/restaging and evaluation of response to treatment [11, 27]. However, the diagnostic performance of [18F]-FDG PET/CT in peritoneal carcinomatosis has been controversial [12,13,14]. This heterogeneity may be due to the particular anatomical features of the peritoneum and the variable [18F]-FDG uptake in different types of primary tumours. Moreover, physiologically, [18F]-FDG accumulates in the intestinal tract, with a relatively high SUV, making it difficult to obtain clear images with high tumour-to-background contrast in lesions in this area. In contrast, previous studies by us and Kratochwil C showed no physiological accumulation of [68Ga]Ga-DOTA-FAPI-04 in the intestinal tract, resulting in very low rates of non-specific uptake in the peritoneal cavity [18, 20, 21]. Such low background activity may facilitate the detection of peritoneal carcinomatosis. More importantly, [68Ga]Ga-DOTA-FAPI-04 uptake in peritoneal carcinomatosis was much higher than that of [18F]-FDG. Consistent with previous clinical investigations, the present study showed that almost all peritoneal carcinomatosis lesions demonstrated higher [68Ga]Ga-DOTA-FAPI-04 uptake than [18F]-FDG, despite the histological origin of the tumour. Consequently, [68Ga]Ga-DOTA-FAPI-04 PET/CT revealed higher sensitivity, a larger lesion extent, and greater PCI score than those of [18F]-FDG PET/CT.
The PCI was first described by Sugarbaker in 1996 and was considered to be the standard for describing carcinomatosis for colorectal cancer and mesothelioma [28]. In recent years, the PCI score has been used to describe and explain the tumour spread pattern and disease severity in patients, regardless of the histological origin. It assesses the extent of peritoneal disease at diagnosis by quantitatively combining the cancer implant size with the tumour distribution throughout 13 abdominopelvic regions, producing a maximum score of 39 [29]. A cut-off PCI score of 20 was found to be a useful stratification tool for the treatment of patients with advanced gastric and colorectal cancer, as the treatment regimen can be tailored based on the PCI score [30, 31]. Recently, Shin et al. reported that the PCI score can be used as a new prognostic factor for patients diagnosed with serous epithelial ovarian cancer [32]. Hence, accurate assessment of the PCI score in patients with peritoneal carcinomatosis is important for patient management and tailoring the treatment. In the present study, [68Ga]Ga-DOTA-FAPI-04 PET/CT revealed a larger disease extent, which led to a significantly higher PCI score than did [18F]-FDG PET/CT. Moreover, surgical exploration was performed in 9 patients with peritoneal carcinomatosis, during which multiple small carcinoma nodules were observed on the peritoneal and mesenteric surfaces, which were highly consistent with the abnormal foci observed on [68Ga]Ga-DOTA-FAPI-04 PET/CT. Such rich detail cannot be achieved using either CT or [18F]-FDG PET/CT alone, which indicates that [68Ga]Ga-DOTA-FAPI-04 PET/CT may be a promising tool for the non-invasive evaluation of PCI. Accurate and comprehensive imaging findings from [68Ga]Ga-DOTA-FAPI-04 PET/CT could guide resection of peritoneal disease, particularly in areas that are easily omitted by surgeons, such as the omentum, falciform ligament, and umbilical round ligament.
Kim et al. analysed 14 studies (671 patients), while Chang et al. analysed 7 studies (513 patients) to evaluate the diagnostic performance of [18F]-FDG PET/CT for detecting peritoneal carcinomatosis and obtained an overall sensitivity of 72.4–87% [12, 33], which was similar to our sensitivity of 72.09%. In terms of specific tumour origins, peritoneal carcinomatosis from gastric cancer demonstrated the lowest sensitivity (53.85%) in [18F]-FDG PET/CT. Although [18F]-FDG PET/CT is a useful diagnostic tool in many cancers, some types of gastric cancers, particularly signet ring cell carcinomas and their peritoneal carcinomatosis, are not [18F]-FDG-avid [34,35,36]. Signet ring cell carcinomas and non-solid type, poorly differentiated adenocarcinomas tend to infiltrate the gastric wall with a large amount of stromal tissue, leading to a low concentration of cancer cells [37]. This may partly explain why [18F]-FDG PET/CT showed low to moderate uptake in these tumour lesions. However, as the tumour invades the peritoneal tissues, stromal fibroblastic changes may occur [38, 39]. Therefore, PET imaging of fibroblast activation with [68Ga]Ga-DOTA-FAPI may demonstrate superior sensitivity as compared to [18F]-FDG PET/CT for the detection of peritoneal carcinomatosis. Indeed, the results of our study demonstrated that [68Ga]Ga-DOTA-FAPI PET/CT showed higher sensitivity than [18F]-FDG PET/CT in detecting peritoneal carcinomatosis, especially those from gastric, pancreatic, and colorectal cancer (although the difference was not statistically significant in pancreatic and colorectal cancer). Future research using larger number of participants would provide a more comprehensive overview of the usefulness of [68Ga]Ga-DOTA-FAPI PET/CT in peritoneal carcinomatosis derived from different types of cancer.
Regarding nodular-type peritoneal carcinomatosis, our results showed that the performance of [18F]-FDG PET/CT for detecting peritoneal carcinomatosis is associated with tumour size. [18F]-FDG PET–positive lesions mostly had a large volume of disease, whereas [18F]-FDG PET–negative lesions demonstrated a low volume of disease, and the peritoneal implants in these patients were markedly small (< 1 cm). The morphological characteristics of most of these foci were below the resolution power of the PET scanner. This result was consistent with the study reported by Turlakow et al. [40]. Encouragingly, [68Ga]Ga-DOTA-FAPI-04 PET/CT showed a superior diagnostic efficacy compared to that of [18F]-FDG PET/CT (92.74% vs. 39.52%) for nodular-type peritoneal carcinomatosis, even in very small peritoneal nodules. In fact, tumour lesions exceeding 1 to 2 mm in size require the formation of a supporting stroma. As the stroma volume can be larger than the tumour volume, stroma-targeted PET imaging may be more sensitive than glycolysis PET imaging for detecting small lesions with sufficient FAP-expressing stroma [41]. This may partially explain why FAPI performed better in the small peritoneal metastasis. However, the peritoneum was not surgically explored in 35 of the initial 46 patients because of the retrospective nature of this study. Therefore, histopathological confirmation of peritoneal lesions was not available, and false-positive status in this group could not be established.
Our study aimed to explore the reliability of clinical data obtained using [68Ga]Ga-DOTA-FAPI-04 PET/CT for the detection of peritoneal carcinomatosis. However, the study had some limitations. First, the patient population in this study was relatively small and heterogeneous (with different types of cancer). Second, this was a retrospective study that aimed to compare the diagnostic performance of peritoneal carcinomatosis between two types of PET scans. Patients with false-positive PET imaging findings were not included in this study (probably due to the small patient population). As such, prospective studies with a larger patient population are warranted in future. In addition, due to absence of prognostic validation, the clinical value of more intense uptake and larger extent of lesion (PCI score) obtained by [68Ga]Ga-DOTA-FAPI-04 imaging requires further investigation.
Conclusions
[68Ga]Ga-DOTA-FAPI-04 PET/CT demonstrated superior sensitivity over [18F]-FDG PET/CT for the detection of peritoneal carcinomatosis in patients with various types of cancer, particularly gastric cancer. Furthermore, the uptake of [68Ga]Ga-DOTA-FAPI-04 in peritoneal carcinomatosis was significantly higher than that of [18F]-FDG, demonstrating a larger lesion extent and higher PCI score. This could help enhance the image contrast, improve physicians’ diagnostic confidence, and reduce missed diagnosis.
Data availability
Not applicable.
References
Hanahan D, Weinberg RA. The hallmarks of cancer. Cell. 2000;100(1):57–70. https://doi.org/10.1016/s0092-8674(00)81683-9.
Glehen O, Osinsky D, Cotte E, Kwiatkowski F, Freyer G, Isaac S, et al. Intraperitoneal chemohyperthermia using a closed abdominal procedure and cytoreductive surgery for the treatment of peritoneal carcinomatosis: morbidity and mortality analysis of 216 consecutive procedures. Ann Surg Oncol. 2003;10(8):863–9. https://doi.org/10.1245/aso.2003.01.018.
Cashin PH, Mahteme H, Spang N, Syk I, Frodin JE, Torkzad M, et al. Cytoreductive surgery and intraperitoneal chemotherapy versus systemic chemotherapy for colorectal peritoneal metastases: a randomised trial. Eur J Cancer. 2016;53:155–62. https://doi.org/10.1016/j.ejca.2015.09.017.
Jacobson R, Sherman SK, Dahdaleh F, Turaga KK. Peritoneal metastases in colorectal cancer. Ann Surg Oncol. 2018;25(8):2145–51. https://doi.org/10.1245/s10434-018-6490-x.
Froysnes IS, Andersson Y, Larsen SG, Davidson B, Oien JT, Julsrud L, et al. ImmunoPeCa trial: long-term outcome following intraperitoneal MOC31PE immunotoxin treatment in colorectal peritoneal metastasis. Eur J Surg Oncol. 2019. https://doi.org/10.1016/j.ejso.2019.04.014.
Alyami M, Hubner M, Grass F, Bakrin N, Villeneuve L, Laplace N, et al. Pressurised intraperitoneal aerosol chemotherapy: rationale, evidence, and potential indications. Lancet Oncol. 2019;20(7):e368–e77. https://doi.org/10.1016/S1470-2045(19)30318-3.
Marin D, Catalano C, Baski M, Di Martino M, Geiger D, Di Giorgio A, et al. 64-Section multi-detector row CT in the preoperative diagnosis of peritoneal carcinomatosis: correlation with histopathological findings. Abdom Imaging. 2010;35(6):694–700. https://doi.org/10.1007/s00261-008-9464-9.
Gryspeerdt S, Clabout L, Van Hoe L, Berteloot P, Vergote IB. Intraperitoneal contrast material combined with CT for detection of peritoneal metastases of ovarian cancer. Eur J Gynaecol Oncol. 1998;19(5):434–7.
Brizi MG, Natale L, Manfredi R, Barbaro B, Vecchioli A, Marano P. Staging of pancreatic ductal adenocarcinoma with spiral CT and MRI. Rays. 2001;26(2):151–9.
Low RN. MR imaging of the peritoneal spread of malignancy. Abdom Imaging. 2007;32(3):267–83. https://doi.org/10.1007/s00261-007-9210-8.
Kostakoglu L, Agress H Jr, Goldsmith SJ. Clinical role of FDG PET in evaluation of cancer patients. Radiographics. 2003;23(2):315–40; quiz 533. https://doi.org/10.1148/rg.232025705.
Kim SJ, Lee SW. Diagnostic accuracy of (18)F-FDG PET/CT for detection of peritoneal carcinomatosis; a systematic review and meta-analysis. Br J Radiol. 2018;91(1081):20170519. https://doi.org/10.1259/bjr.20170519.
Suzuki A, Kawano T, Takahashi N, Lee J, Nakagami Y, Miyagi E, et al. Value of 18F-FDG PET in the detection of peritoneal carcinomatosis. Eur J Nucl Med Mol Imaging. 2004;31(10):1413–20. https://doi.org/10.1007/s00259-004-1577-y.
Lopez-Lopez V, Cascales-Campos PA, Gil J, Frutos L, Andrade RJ, Fuster-Quinonero M, et al. Use of (18)F-FDG PET/CT in the preoperative evaluation of patients diagnosed with peritoneal carcinomatosis of ovarian origin, candidates to cytoreduction and hipec. A pending issue. Eur J Radiol. 2016;85(10):1824–8. https://doi.org/10.1016/j.ejrad.2016.08.006.
Soyka JD, Strobel K, Veit-Haibach P, Schaefer NG, Schmid DT, Tschopp A, et al. Influence of bowel preparation before 18F-FDG PET/CT on physiologic 18F-FDG activity in the intestine. J Nucl Med. 2010;51(4):507–10. https://doi.org/10.2967/jnumed.109.071001.
Kalluri R. The biology and function of fibroblasts in cancer. Nat Rev Cancer. 2016;16(9):582–98. https://doi.org/10.1038/nrc.2016.73.
Chen X, Song E. Turning foes to friends: targeting cancer-associated fibroblasts. Nat Rev Drug Discov. 2019;18(2):99–115. https://doi.org/10.1038/s41573-018-0004-1.
Kratochwil C, Flechsig P, Lindner T, Abderrahim L, Altmann A, Mier W, et al. (68)Ga-FAPI PET/CT: tracer uptake in 28 different kinds of cancer. J Nucl Med. 2019;60(6):801–5. https://doi.org/10.2967/jnumed.119.227967.
Lindner T, Loktev A, Altmann A, Giesel F, Kratochwil C, Debus J, et al. Development of quinoline-based theranostic ligands for the targeting of fibroblast activation protein. J Nucl Med. 2018;59(9):1415–22. https://doi.org/10.2967/jnumed.118.210443.
Chen H, Pang Y, Wu J, Zhao L, Hao B, Wu J, et al. Comparison of [(68)Ga]Ga-DOTA-FAPI-04 and [(18)F] FDG PET/CT for the diagnosis of primary and metastatic lesions in patients with various types of cancer. Eur J Nucl Med Mol Imaging. 2020. https://doi.org/10.1007/s00259-020-04769-z.
Chen H, Zhao L, Ruan D, Pang Y, Hao B, Dai Y, et al. Usefulness of [(68)Ga]Ga-DOTA-FAPI-04 PET/CT in patients presenting with inconclusive [(18)F]FDG PET/CT findings. Eur J Nucl Med Mol Imaging. 2020. https://doi.org/10.1007/s00259-020-04940-6.
Zhao L, Zhuang Y, Fu K, Chen P, Wang Y, Zhuo J, et al. Usefulness of [(18)F]fluorodeoxyglucose PET/CT for evaluating the PD-L1 status in nasopharyngeal carcinoma. Eur J Nucl Med Mol Imaging. 2020. https://doi.org/10.1007/s00259-019-04654-4.
Sugarbaker PH. Peritonectomy procedures. Ann Surg. 1995;221(1):29–42. https://doi.org/10.1097/00000658-199501000-00004.
Pletcher E, Gleeson E, Labow D. Peritoneal cancers and hyperthermic intraperitoneal chemotherapy. Surg Clin North Am. 2020;100(3):589–613. https://doi.org/10.1016/j.suc.2020.02.009.
van Baal J, van Noorden CJF, Nieuwland R, Van de Vijver KK, Sturk A, van Driel WJ, et al. Development of peritoneal carcinomatosis in epithelial ovarian cancer: a review. J Histochem Cytochem. 2018;66(2):67–83. https://doi.org/10.1369/0022155417742897.
Raptopoulos V, Gourtsoyiannis N. Peritoneal carcinomatosis. Eur Radiol. 2001;11(11):2195–206. https://doi.org/10.1007/s003300100998.
Akin EA, Qazi ZN, Osman M, Zeman RK. Clinical impact of FDG PET/CT in alimentary tract malignancies: an updated review. Abdom Radiol (NY). 2020;45(4):1018–35. https://doi.org/10.1007/s00261-020-02447-0.
Jacquet P, Sugarbaker PH. Clinical research methodologies in diagnosis and staging of patients with peritoneal carcinomatosis. Cancer Treat Res. 1996;82:359–74. https://doi.org/10.1007/978-1-4613-1247-5_23.
Archer AG, Sugarbaker PH, Jelinek JS. Radiology of peritoneal carcinomatosis. Cancer Treat Res. 1996;82:263–88. https://doi.org/10.1007/978-1-4613-1247-5_17.
Mo S, Cai G. Multidisciplinary treatment for colorectal peritoneal metastases: review of the literature. Gastroenterol Res Pract. 2016;2016:1516259. https://doi.org/10.1155/2016/1516259.
Abdalla Ahmed S, Abou-Taleb H, Ali N, MB D. Accuracy of radiologic- laparoscopic peritoneal carcinomatosis categorization in the prediction of surgical outcome. Br J Radiol. 2019;92(1100):20190163. https://doi.org/10.1259/bjr.20190163.
Elzarkaa AA, Shaalan W, Elemam D, Mansour H, Melis M, Malik E, et al. Peritoneal cancer index as a predictor of survival in advanced stage serous epithelial ovarian cancer: a prospective study. J Gynecol Oncol. 2018;29(4):e47. https://doi.org/10.3802/jgo.2018.29.e47.
Chang MC, Chen JH, Liang JA, Huang WS, Cheng KY, Kao CH. PET or PET/CT for detection of peritoneal carcinomatosis: a meta-analysis. Clin Nucl Med. 2013;38(8):623–9. https://doi.org/10.1097/RLU.0b013e318299609f.
Smyth EC, Verheij M, Allum W, Cunningham D, Cervantes A, Arnold D, et al. Gastric cancer: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2016;27(suppl 5):v38–49. https://doi.org/10.1093/annonc/mdw350.
Lim JS, Kim MJ, Yun MJ, Oh YT, Kim JH, Hwang HS, et al. Comparison of CT and 18F-FDG pet for detecting peritoneal metastasis on the preoperative evaluation for gastric carcinoma. Korean J Radiol. 2006;7(4):249–56. https://doi.org/10.3348/kjr.2006.7.4.249.
Honma Y, Terauchi T, Tateishi U, Kano D, Nagashima K, Shoji H, et al. Imaging peritoneal metastasis of gastric cancer with (18)F-fluorothymidine positron emission tomography/computed tomography: a proof-of-concept study. Br J Radiol. 2018;91(1089):20180259. https://doi.org/10.1259/bjr.20180259.
Yoshioka T, Yamaguchi K, Kubota K, Saginoya T, Yamazaki T, Ido T, et al. Evaluation of 18F-FDG PET in patients with advanced, metastatic, or recurrent gastric cancer. J Nucl Med. 2003;44(5):690–9.
Capobianco A, Cottone L, Monno A, Manfredi AA, Rovere-Querini P. The peritoneum: healing, immunity, and diseases. J Pathol. 2017;243(2):137–47. https://doi.org/10.1002/path.4942.
Lv ZD, Wang HB, Li FN, Wu L, Liu C, Nie G, et al. TGF-beta1 induces peritoneal fibrosis by activating the Smad2 pathway in mesothelial cells and promotes peritoneal carcinomatosis. Int J Mol Med. 2012;29(3):373–9. https://doi.org/10.3892/ijmm.2011.852.
Turlakow A, Yeung HW, Salmon AS, Macapinlac HA, Larson SM. Peritoneal carcinomatosis: role of (18)F-FDG PET. J Nucl Med. 2003;44(9):1407–12.
Calais J, Mona CE. Will FAPI PET/CT Replace FDG PET/CT in the next decade?-point: an important diagnostic, phenotypic and biomarker role. AJR Am J Roentgenol. 2020. https://doi.org/10.2214/AJR.20.24302.
Funding
This work was funded by National Natural Science Foundation of China (Grant numbers 81772893 and 81701736) and the key medical and health projects in Xiamen (Grant number 3502Z20191104).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethics approval
All procedures involving human participants were carried out in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. This article does not contain any experiments with animals.
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Consent for publication
Informed consent was obtained from all individual participants included in the study.
Code availability
Not applicable.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Oncology - General
Rights and permissions
About this article
Cite this article
Zhao, L., Pang, Y., Luo, Z. et al. Role of [68Ga]Ga-DOTA-FAPI-04 PET/CT in the evaluation of peritoneal carcinomatosis and comparison with [18F]-FDG PET/CT. Eur J Nucl Med Mol Imaging 48, 1944–1955 (2021). https://doi.org/10.1007/s00259-020-05146-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00259-020-05146-6