Abstract
Purpose
In this paper, we aimed to evaluate the positron emission tomography (PET) performance of, to the best of our knowledge, the third commercially available whole-body integrated PET/magnetic resonance (MR) system.
Methods
The PET system performance was measured following the NEMA standards with and without simultaneous MR operation. PET spatial resolution, sensitivity, scatter fraction, count-rate performance, accuracy of count losses and random corrections, image quality, and time-of-flight (TOF) resolution were quantitatively evaluated. Clinical scans were acquired at the PET/MR system and compared with images acquired at a PET/CT with the same digital detector technology.
Results
Measurement results of essential PET performance were reported in the form of MR idle (MR pulsing). The axial, radial, and tangential spatial resolutions were measured as 2.72 mm (2.73 mm), 2.86 mm (2.85 mm), and 2.81 mm (2.82 mm) FWHM, respectively, at 1 cm radial offset. The NECR peak was measured as 129.2 kcps (129.5 kcps) at 14.7 kBq mL−1 (14.2 kBq mL−1). The scatter fraction at NECR peak was 37.9% (36.5%), and the maximum slice error below NECR was 4.1% (4.5%). Contrast recovery coefficients ranged from 51.8% (52.3%) for 10 mm hot sphere to 87.3% (87.2%) for 37 mm cold sphere. TOF resolution at 5.3 kBq mL−1 was measured at 535 ps (540 ps). With point source, TOF was measured to be 474 ps (485 ps). Clinical scans revealed similar image quality from the PET/MR and the comparative PET/CT system.
Conclusion
The PET performance of the newly introduced integrated PET/MR system is not significantly affected by the simultaneous operation of an MR sequence (2-point DIXON sequence). Measurement results demonstrate comparable performance with other state-of-the-art PET/MR systems. The clinical benefits of high spatial resolution and long axial coverage remain to be further evaluated in specific clinical imaging applications.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The integrated positron emission tomography (PET) and magnetic resonance (MR) imaging is emerging as a powerful multimodality imaging tool in clinical practice and in medical research. Integrated PET/MR combines the unique advantage from MRI and PET to achieve simultaneous imaging with physical co-registration. MR compensates for the lack of structural information in PET images without introducing extra ionizing radiation dose compared to CT. The wide diversity of contrast mechanism and superior soft tissue contrast of MR also makes PET/MR a better choice compared with PET/CT in many clinical applications such as brain imaging, prostate imaging, and cardiac imaging [1,2,3,4,5]. Furthermore, the simultaneity of PET and MR acquisition enables new applications requiring accurate time and spatial alignment between the data obtained with these two modalities such as MR-based PET motion correction and joint reconstruction with MR and PET. After being introduced into clinical use in early 2010s, PET/MR has been adopted in many important areas of diagnostic medicine, such as neurology, oncology, and cardiology [6,7,8,9,10].
The integration of PET and MR is technically challenging, primarily due to the mutual interference between these two modalities [11]. On one side, the rapidly switching MR gradient causes mechanical vibration and eddy current heating, which could induce system stability issues and errors in PET quantification. Therefore, PET detectors need to be enclosed by adequate radio frequency (RF) shielding to prevent the RF interference from the MR RF system. On the other side, metallic components in PET detectors could disrupt the homogeneity of MR B0 field, and thus all electronic and mechanic components need to be carefully selected for a PET/MR system. In addition, the conductive components in RF shielding and electronic circuits are prone to eddy current heating during MR imaging and hence could potentially cause additional MR image artifacts [12, 13]. Finally, the digital programming operating on the PET systems could unexpectedly introduce RF noise to the MR receiving chain. With very limited and precious real estate inside the MR bore, it is extremely difficult to tackle all these challenges without significantly compromising the performance of the two subsystems [14].
The first commercially available whole-body PET/MR system was introduced by Philips [15]. This system uses a sequential configuration with a common patient bed connecting two spatially separated MR and PET subsystems. With the development of silicon-based photodetectors, two integrated systems, the Siemens Biography mMR [16] and the GE SIGNA PET/MR [17, 18] were released to the market in early 2010s. Compared to sequential configuration, the integrated systems feature shorter scanning time, more compact installation footprint, better spatial registration, and temporal correlation. Therefore, the integrated systems have been rapidly adopted as mainstream configuration for whole-body PET/MR [19].
In this paper, we aimed to evaluate the PET performance of, for the first time, the third commercially available whole-body integrated PET/MR system, uPMR 790 manufactured by United Imaging Healthcare (Fig. 1) [20]. We followed the standardized procedures described in NU2-2012 and NU2-2018 (for time-of-flight resolution) protocol of the National Electrical Manufacturers Association (NEMA), and the PET system performance was measured with and without simultaneous MR operation.
Methods
System design and specification
All performance measurements were conducted on the UIH uPMR 790 PET/MR scanners in Zhongshan Hospital, Shanghai, and United Imaging Healthcare Co. Ltd., Shanghai. The uPMR 790 system comprises a 3-T super conducting magnet, a gradient system with a set of second-order active shimming coil (45 mT s−1, 200 T m−1 s−1), and a 48-channel RF-receiving system.
The PET detector system is installed between the gradient coil and RF body coil. The entire PET ring comprises 20 modules with a transverse field of view (FOV) of 60 cm and an axial field of view of 32 cm. Each module contains 5 × 14 blocks with 14 blocks along the axial direction. Each block has 4 SiPM detector channels coupled with a 7 × 8 array of 15.5 × 2.76 × 2.76 mm3 LYSO crystals through proprietary design of internal light guide. The entire PET system comprises 112 axial crystal rings and each ring contains 700 crystals, making 78,400 crystals in total. The PET system has a claimed energy resolution of 13% (value provided by the manufacturer). Design and performance specifications for the PET and MR subsystems are summarized in Table 1. Figure 2 is a conceptual drawing showing the placement of the PET detector modules in the system.
The PET system performance was evaluated following the NEMA NU2-2012 standards [21], except for the time-of-flight (TOF) resolution which was evaluated following the NEMA NU2-2018 standards and vendor-provided approach [22]. PET data was acquired in the absence and presence of continuous MR pulsing during the entire data acquisition. The Water Fat Imaging (WFI) sequence, a two-point DIXON technique provided by the manufacturer for PET attenuation correction and anatomical localization, was used to evaluate the impact of clinical MRI operations on PET performance. The following sections provide details of the measurements in accordance with the NEMA standards [21, 22]. All measurements were repeated three times independently on different machines over 1 year timespan. The detector module temperature was kept at 16.5 ± 0.5 °C during the measurements, and we have provided the average results.
PET spatial resolution
Three capillary tubes with inner diameter of 0.5 mm (outer diameter: 1 mm) were filled with 18FDG solution. The initial activity in each tube was measured to be above 1.1 kBq so that there were enough counts throughout the experiment. The capillary tubes were placed on a holder provided by the manufacturer in the patient bore. The position of the three point sources was adjusted to the same transverse plane at 1 cm, 10 cm, and 20 cm from the center of the plane as confirmed by quick PET scout scans. Following NEMA 2012 standards [21], data were collected at two axial positions, the center of the axial field of view and 12 cm (3/8 of axial FOV) from the center of FOV.
For each configuration, a total of 900,000 counts were collected. The data was reconstructed with Fourier Rebinning and Filtered Back Projection with no smoothing or apodization. The image matrix dimension was 1023 × 1023 × 531 with 0.6 mm isotropic voxel size. The spatial resolution in full-width half maximum (FWHM) in axial, radial, and tangential directions were calculated following the NEMA standards with a built-in software tool in the system [21].
PET scatter fraction, count losses, and randoms
A scatter phantom as described in the NEMA standard was filled with 370 MBq of 18FDG solution [21]. Two foam holders outside the axial FOV were used to place the phantom on the patient bed at the center of FOV trans-axially. Thirty-eight frames of data were collected during 16.75 h (protocols shown in Table 2). Delayed window method was used for random estimation. Count rates, peak count values, and scatter fraction were calculated following the NEMA standard [21].
Sensitivity
A phantom with 5 concentric aluminum sleeves was used for sensitivity measurement. A 700-mm plastic tube was filled with 14 MBq of 18FDG to minimize the effect of dead time and randoms and was placed at the center of the phantom. Data acquisition with 3 min duration was conducted starting with 5 sleeves, and it was repeated immediately with MR pulsing. The same procedure was repeated 3 more times, with one sleeve removed each time. The whole process was performed with the phantom placed both at the center of FOV and 10 cm off center. No patient bed nor MR coil except for the volume transmission coil were inside the FOV during data acquisition. Randoms were estimated through delayed window method and subtracted from the data.
PET accuracy
Data collected from “Scatter Fraction, Count Losses and Randoms” was used in this analysis to measure the accuracy of corrections for dead time losses and random event counts in images. Images were reconstructed into a 256 × 256 × 113 matrix with 2.4 × 2.4 × 2.85 mm3 voxel size using Ordered Subset Expectation Maximization (OSEM) algorithm with 20 subsets and 2 iterations with point spread function (PSF) [23] and TOF modeling. Corrections for scatter [24], attenuation, randoms, and dead time were applied. Images were further analyzed according to the NEMA standard to calculate the relative count rate errors for each slice in each acquisition. Five slices on each end of the axial FOV were excluded as they contained high statistical noise, which was also suggested in the NEMA 2012 standards [21].
Image quality
A NEMA image quality phantom (Data Spectrum Corp, NC, USA) and a body scatter phantom were filled and positioned on the patient bed following the NEMA standards [21]. The background was filled with 18FDG with activity concentration of 5.3 kBq mL−1 (as calibrated at the start of imaging). The hot spheres were filled with 4 times activity concentration of the background while the cold spheres were filled with water. The line source was filled with 114 MBq (as calibrated at the start of imaging) of 18FDG. The image quality phantom was placed in the center of the axial FOV and scanned for 6.72 min, using a 22.4-cm axial step (30% overlap between bed positions). Since the phantom was filled only once, the acquisition time with MR pulsing was extended to 7 min to compensate for the decay of 18F during the MR idle scan. Image was reconstructed using the standard clinical protocols (matrix: 256 × 256 × 113, voxel size: 2.2 × 2.2 × 2.85 mm3, OSEM with 20 subsets and 3 iterations, with PSF and TOF). A built-in phantom attenuation template measured using a CT scan was used for the co-registration to the non-attenuation-corrected phantom image. No MR coils besides the body transmission coil were placed inside the FOV. To evaluate the convergence property of the reconstruction algorithm, image quality analysis was repeated with the phantom images reconstructed using OSEM with one to ten iterations. The standard background variability vs. contrast recovery curve was plotted for all spheres within the phantom for the MR idle condition.
TOF resolution
Data collected from “Scatter Fraction, Count Losses, and Randoms” was used in this analysis to measure the time-of-flight resolution of the system. Following the instructions from NEMA NU2-2018 standards [22], the TOF resolution at each activity concentration in the measurements listed in Table 2 was calculated. In addition to the NEMA method, we also used a 22Na point source (Ø0.5 × 0.5 × 0.5 mm3, 480 kBq) placed at the center of the FOV to evaluate the TOF resolution based on the vendor-provided approach used in other United Imaging PET/CT systems [25] .
Derenzo resolution phantom
To further validate the spatial resolution in larger scale and clinical relevant setting, a resolution testing with Derenzo phantom [26, 27] was conducted to check the system spatial resolution using iterative reconstruction. The phantom was filled with 50 MBq of 18FDG solution and was scanned back to back at the center of FOV with MR idle and MR pulsing, and each with 30 min scan duration. The images were reconstructed with the build-in OSEM algorithm (FOV: 300 mm, matrix size: 256 × 256, slice thickness: 1.2 mm, iteration number: 50 with PSF and TOF).
Clinical images
Comparative clinical scans were acquired at Zhongshan Hospital with the UIH uMI 780 PET/CT system (United Imaging Healthcare, Shanghai, China) [28] and the UIH uPMR 790 PET/MR system. The patient was injected with 298 MBq of 18FDG then imaged with PET/CT (50 min post-injection) and PET/MR (95 min post-injection). The acquisition time of the PET/CT scan was 2 min for each bed, with 6 bed positions in total, while the acquisition time for PET/MR was 3 min/bed with 5 bed positions in total. The reconstruction parameters for PET/CT are as follows (150 × 150 image size in 600 mm transaxial FOV, 3D OSEM with 3 iterations, and 10 subsets with PSF and TOF modeling. A post-filter of 3 mm FWHM Gaussian was applied) while PET/MR reconstruction used the same standard clinical setting as described in the NEMA image quality session [21].
For each of the bed positions in the body, a WFI scan accelerated with compressed sensing technique was used for PET attenuation correction. This sequence provides 4 images: in-phase, out-phase, water and fat, which were later segmented to generate the PET attenuation map with 4 classes: soft tissue, fat, lung, and air. The in-phase image can be also viewed as a high-resolution T1 image. Truncation completion outside the MR FOV was achieved by segmenting the non-attenuation-corrected PET images. For the head scan, an ultrashort echo time (UTE) sequence was used for bone segmentation. The attenuation maps for non-patient objects inside the PET FOV, including patient bed, solid MR coils such as posterior array coil and head coil, were generated through CT scans and included in the reconstruction, while flexible surface coils were ignored. More details about MR-based attenuation correction can be found in a previous publication regarding this topic [29].
Additional clinical PET/MR images for different body parts were retrospectively collected from clinical scans with Institutional Review Board (IRB) approval. Patients were injected with 3.7 MBq kg−1 and scanned at 45 to 90 min post-injection, and all images were reconstructed with clinical protocols. Representative clinical images were included in the Supplementary material.
Results
Spatial resolution
Spatial-resolution FWHM values with or without MR pulsing are summarized in Table 3. The results are averaged from three independent measurements, and each contains a placement of the source at the center of the axial FOV and 12 cm off the axial center. There is no significant difference in spatial resolution observed with or without MR pulsing.
Scatter fraction, count losses, and randoms
Count rate plots and scatter fraction plots at different activity concentrations for both MR idle and MR pulsing are shown in Fig. 3. Figure 4 presents comparisons of the NECR vs. activity curve from the acquisition between MR idle and MR pulsing, randomly selected from one of three measurements. Peak count rate values are summarized in Table 4. The NECR peak (average with standard deviation from three measurements) was measured as 129.2 ± 4.4 kcps at 14.7 kBq mL−1 for MR idle and 129.5 ± 3.3 kcps at 14.2 kBq mL−1 for MR pulsing. The scatter fraction at NECR peak was 37.9 ± 1.4% for MR idle and 36.5 ± 1.4% for MR pulsing.
Sensitivity
Table 5 shows the sensitivity values for each radial offset and for both MR idle and MR pulsing (each set averaged from three independent measurements). Figure 5 is a comparison (randomly selected from one of the three measurements) of the axial sensitivity profile for the 0-cm radial offset case at different axial slices between MR idle and MR pulsing. The sensitivity at center is 15.9 ± 0.5 cps kBq−1 for MR idle and 16.0 ± 0.8 cps kBq−1 for MR pulsing.
Accuracy
Figure 6 shows the maximum and minimum slice count rate error vs. activity concentration, for acquisitions under MR idle and MR pulsing. The maximum absolute slice error below peak NECR activity was 4.1% for MR idle and 4.5% for MR pulsing (averaged from two measurements).
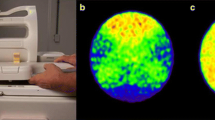
Image quality
Contrast recovery and background variability values (averaged from three measurements) are shown in Table 6 for both MR idle and MR pulsing. The transverse and coronal reconstructed phantom images are shown in Fig. 7. The contrast recovery against different background variability is shown in Fig. 8.
TOF resolution
TOF resolution as a function of activity concentration is shown in Fig. 9 (from one of the three measurements). Averaged from three measurements, the TOF resolution based on NEMA method at 5.3 kBq mL−1 is 535 ± 1 ps FWHM for MR idle and 540 ± 5 ps FWHM for MR pulsing. Additionally, with the vendor-provided point source approach, TOF resolutions is measured as 474 ps for MR idle and 485 ps for MR pulsing.
Derenzo resolution phantom
Images of the Derenzo phantom are shown in Fig. 10. Rods with the size of 2 mm in the phantom can be clearly appreciated in both MR idle and MR pulsing situations.
Clinical images
Comparative PET/CT and PET/MR images of the same patient are shown in Fig. 11. Because of the different body positions during PET/CT and PET/MR scan, slices of a single coronal image were not matched perfectly.
Discussion
Even with persisting debate on its killer applications in clinical setting, integrated PET/MR has been gradually adopted worldwide at a steady pace in the past 5 years [30,31,32]. The major breakthrough on the PET detector technology allows TOF capability on both GE SIGNA PET/MR and the current system reported in this work. Before broader clinical investigation of a PET/MR system, NEMA measurement serves as the fundamental characterization to quantify the system level performance [21]. To our best knowledge, this is the first report of NEMA measurements of the UIH uPMR 790 system and the third of all commercially available systems.
Different from a PET/CT system which works in a sequential mode, PET/MR features simultaneous operation of both PET and MR acquisition. With both modalities located concentrically within the same imaging space, it is essential to characterize the system interference between the PET and MR subsystems. Similar approach was employed by Grant et al. [17] on NEMA NU2-2012 measurements of previous PET/MR systems [21], except for the TOF resolution measurement which was new for NEMA NU2-2018 [22].
The reported PET/MR system features one of the highest NEMA spatial resolutions among clinical PET/CT and PET/MR systems [33,34,35,36], mainly due to the small scintillation crystals used in the PET detectors [37]. No significant spatial resolution degradation was observed during MR operation. Spatial resolution was shown to degrade from the center to the edge of the transaxial FOV, especially the resolution along the radial direction, which is due to the well-known parallax effect [38]. No significant impact of MR operation was observed on count rate performance. Scatter fraction shows a small decrease under MR pulsing, which could be the result of a shifting energy peak caused by detector heating from MR pulsing. There is virtually no impact from MR operation to the PET system sensitivity. On average, the TOF resolution with MR pulsing is less than 2% different from that with MR idle at the same activity concentration. The maximum slice error below NECR was 4.1% with MR idle and 4.5% with MR pulsing, which are both at very low activity concentrations and are most likely due to the high statistical noise. For most activity concentration values below NECR peak, the slice error is below 2%. These results suggest uPMR 790 is able to provide accurate quantitative measurements. No significant difference was found in the contrast recovery between MR idle and MR pulsing, while a slight increase on background variability was observed with MR pulsing, possibly due to noise injection from the RF system.
The PET/MR system and the PET/CT system with similar digital detector technology provide comparable PET image quality. Furthermore, the PET/MR system is capable of PET acquisition simultaneously with MR operation in clinical settings. Compared with other commercially available systems, the presented system features higher NEMA resolution and longer axial coverage. The clinical benefits of this enhanced system performance remain to be further evaluated in specific clinical imaging applications. The benefit of TOF in this PET/MR would also require further investigation using phantoms and clinical dataset.
One major limitation of this study is the selection of attenuation correction pulse sequence as the MR pulsing condition. It is appropriate to select the Dixon-based gradient echo sequence to justify the system performance under clinical scans but future work is needed to evaluate the system performance under extremely intensive MR sequence for research. Interrogation of PET/MR (GE SIGNA PET/MR) stability under aggressive pulse sequence was reported previously by Deller et al. [39].
Conclusion
PET performance of the United Imaging uPMR 790 PET/MR system was tested following NEMA NU2-2012 standard with both MR idle and MR pulsing. No significant effect of MR pulsing on the system performance was found. Measurement results demonstrate comparable performance with other state-of-art PET/MR systems. Testing results demonstrate higher NEMA spatial resolution and longer axial coverage while slightly lower sensitivity than other commercially available systems [14]. Clinical images confirmed that system is capable of generating simultaneous high-quality PET and MR images in clinical setting. The clinical benefits of high spatial resolution and long axial coverage remain to be further evaluated in specific clinical imaging applications.
Data availability
All of NEMA raw data images are stored at the Department of Nuclear Medicine, Zhongshan Hospital, Fudan University, China, and United Imaging Healthcare Co., Ltd., China.
References
Bailey DL, et al. Combined PET/MR: the real work has just started. Summary report of the third international workshop on PET/MR imaging; February 17-21, 2014, Tubingen, Germany. Mol Imaging Biol. 2015;17(3):297–312.
Bailey DL, et al. Combined PET/MR: where are we now? Summary report of the second international workshop on PET/MR imaging April 8-12, 2013, Tubingen, Germany. Mol Imaging Biol. 2014;16(3):295–310.
Bailey DL, et al. Summary report of the first international workshop on PET/MR imaging, March 19-23, 2012, Tubingen, Germany. Mol Imaging Biol. 2013;15(4):361–71.
Bailey DL, et al. Combined PET/MRI: from status quo to status go. Summary report of the fifth international workshop on PET/MR imaging, February 15-19, 2016, Tubingen, Germany. Mol Imaging Biol. 2016;18(5):637–50.
Bailey DL, et al. Combined PET/MRI: multi-modality multi-parametric imaging is here: summary report of the 4th international workshop on PET/MR imaging; February 23-27, 2015, Tubingen, Germany. Mol Imaging Biol. 2015;17(5):595–608.
Abgral R, et al. Clinical utility of combined FDG-PET/MR to assess myocardial disease. JACC Cardiovasc Imaging. 2017;10(5):594–7.
Nakajo K, et al. Diagnostic performance of fluorodeoxyglucose positron emission tomography/magnetic resonance imaging fusion images of gynecological malignant tumors: comparison with positron emission tomography/computed tomography. Jpn J Radiol. 2010;28(2):95–100.
Grueneisen J, et al. Integrated PET/MRI for whole-body staging of patients with primary cervical cancer: preliminary results. Eur J Nucl Med Mol Imaging. 2015;42(12):1814–24.
Shin HW, et al. Initial experience in hybrid PET-MRI for evaluation of refractory focal onset epilepsy. Seizure. 2015;31:1–4.
Miller-Thomas MM, Benzinger TL. Neurologic applications of PET/MR imaging. Magn Reson Imaging Clin N Am. 2017;25(2):297–313.
Vaska P, Cao T. The state of instrumentation for combined positron emission tomography and magnetic resonance imaging. In: Seminars in nuclear medicine. 2013. Elsevier.
Herzog H, Lerche C. Advances in clinical PET/MRI instrumentation. PET Clin. 2016;11(2):95–103.
Herzog H, Van Den Hoff J. Combined PET/MR systems: an overview and comparison of currently available options. Q J Nucl Med Mol Imaging. 2012;56(3):247–67.
Hope TA, et al. Summary of the first ISMRM-SNMMI workshop on PET/MRI: applications and limitations. J Nucl Med. 2019;60(10):1340–6.
Zaidi H, et al. Design and performance evaluation of a whole-body ingenuity TF PET-MRI system. Phys Med Biol. 2011;56(10):3091–106.
Delso G, et al. Performance measurements of the Siemens mMR integrated whole-body PET/MR scanner. J Nucl Med. 2011;52(12):1914–22.
Grant AM, et al. NEMA NU 2-2012 performance studies for the SiPM-based ToF-PET component of the GE SIGNA PET/MR system. Med Phys. 2016;43(5):2334.
Levin CS, et al. Performance of a high sensitivity time-of-flight PET ring operating simultaneously within a 3T MR system. In: EJNMMI physics. 2014. Springer.
Bailey DL, et al. Combined PET/MRI: global warming-summary report of the 6th international workshop on PET/MRI, March 27-29, 2017, Tubingen, Germany. Mol Imaging Biol. 2018;20(1):4–20.
Cao T, Chen S, Pang L. NEMA NU2-2012 performance measurements of the United-Imaging uPMR790: a HD TOF simultaneous PET/MR system. J Nucl Med. 2018;59(supplement 1):1856.
Association, N.E.M., NEMA Standards Publication NU-2 2012 performance measurements of positron emission tomographs. 2012: Rosslyn, VA.
Association, N.E.M., NEMA Standards Publication NU-2 2018 performance measurements of positron emission tomographs. 2018: Rosslyn, VA.
Hoffman EJ, Huang SC, Phelps ME. Quantitation in positron emission computed tomography: 1. Effect of object size. J Comput Assist Tomogr. 1979;3(3):299–308.
Watson CC, Newport D, Casey ME. A single scatter simulation technique for scatter correction in 3D PET. In: Three-dimensional image reconstruction in radiology and nuclear medicine: Springer; 1996. p. 255–68.
Lv Y, et al. Mini EXPLORER II: a prototype high-sensitivity PET/CT scanner for companion animal whole body and human brain scanning. Phys Med Biol. 2019;64(7):075004.
Bunka M, et al. Imaging quality of (44)Sc in comparison with five other PET radionuclides using Derenzo phantoms and preclinical PET. Appl Radiat Isot. 2016;110:129–33.
Cox BL, et al. Development of a novel linearly-filled Derenzo microPET phantom. Am J Nucl Med Mol Imaging. 2016;6(3):199–204.
Zhang Q, et al. Comparison of (68)Ga-PSMA-11 PET-CT with mpMRI for preoperative lymph node staging in patients with intermediate to high-risk prostate cancer. J Transl Med. 2017;15(1):230.
Liu G, et al. Validation of MR-based attenuation correction of a newly released whole-body simultaneous PET/MR system. Biomed Res Int. 2019;2019:8213215.
Amorim BJ, et al. Clinical impact of PET/MR in treated colorectal cancer patients. Eur J Nucl Med Mol Imaging. 2019;46(11):2260–9.
Galgano S, et al. Practical considerations for clinical PET/MR imaging. PET Clin. 2018;13(1):97–112.
Mansi L, Ciarmiello A. Perspectives on PET/MR imaging: are we ready for clinical use? J Nucl Med. 2014;55(4):529–30.
Rausch I, et al. Performance evaluation of the biograph mCT flow PET/CT system according to the NEMA NU2-2012 standard. EJNMMI Phys. 2015;2(1):26.
Vandendriessche D, et al. Performance characteristics of silicon photomultiplier based 15-cm AFOV TOF PET/CT. EJNMMI Phys. 2019;6(1):8.
Rausch I, et al. Performance evaluation of the Vereos PET/CT system according to the NEMA NU2-2012 standard. J Nucl Med. 2019;60(4):561–7.
van Sluis J, et al. Performance characteristics of the digital biograph vision PET/CT system. J Nucl Med. 2019;60(7):1031–6.
Moses WW. Fundamental limits of spatial resolution in PET. Nucl Instrum Methods Phys Res A. 2011;648 Supplement 1:S236–40.
MacDonald LR, Dahlbom M. Parallax correction in PET using depth of interaction information. IEEE Trans Nucl Sci. 1998;45(4):2232–7.
Deller TW, et al. PET imaging stability measurements during simultaneous pulsing of aggressive MR sequences on the SIGNA PET/MR system. J Nucl Med. 2018;59(1):167–72.
Acknowledgments
The authors thank Shanghai Municipal Key Clinical Specialty (shslczdzk03401).
Funding
Supported by National Key Research and Development Plan “Digital Diagnosis and Treatment Equipment Research and Development” Key Specialty (2016YFC0103900), Shanghai Science and Technology Commission “Science and Technology Innovation Action Plan” in the Field of Cooperation in the Field of Industry, Education and Research (19DZ1930700), Shanghai Municipal Key Clinical Specialty(shslczdzk03401).
Author information
Authors and Affiliations
Contributions
HS contributed to the design of this study. SC designed and performed the experiments. SC, YG, and HY were in charge of the preparation of the NEMA phantom and of the acquisition. SC, XC, and LH analyzed the data. SC and TC drafted the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Consent for publication
Not applicable.
Conflict of interest
Xin Chen, Tuoyu Cao, and Lingzhi Hu are employees of United Imaging Healthcare. The other authors working with Zhongshan Hospital have full control of the data and declare that they have no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Technology
Supplementary information
ESM 1
(DOCX 1057 kb).
Rights and permissions
About this article
Cite this article
Chen, S., Gu, Y., Yu, H. et al. NEMA NU2-2012 performance measurements of the United Imaging uPMR790: an integrated PET/MR system. Eur J Nucl Med Mol Imaging 48, 1726–1735 (2021). https://doi.org/10.1007/s00259-020-05135-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00259-020-05135-9