Abstract
Purpose
The purpose of this study was to investigate the performance of 68Ga-PSMA-617 PET/CT in predicting risk stratification and metastatic risk of prostate cancer.
Methods
Fifty newly diagnosed patients with prostate cancer as confirmed by needle biopsy were continuously included, 40 in a train set and ten in a test set. 68Ga-PSMA-617 PET/CT and clinical data of all patients were retrospectively analyzed. Semi-quantitative analysis of PET images provided maximum standardized uptake (SUVmax) of primary prostate cancer and volumetric parameters including intraprostatic PSMA-derived tumor volume (iPSMA-TV) and intraprostatic total lesion PSMA (iTL-PSMA). According to prostate cancer risk stratification criteria of the NCCN Guideline, all patients were simplified into a low-intermediate risk group or a high-risk group. The semi-quantitative parameters of 68Ga-PSMA-617 PET/CT were used to establish a univariate logistic regression model for high-risk prostate cancer and its metastatic risk, and to evaluate the diagnostic efficacy of the predictive model.
Results
In the train set, 30/40 (75%) patients had high-risk prostate cancer and 10/40 (25%) patients had low-to-moderate-risk prostate cancer; in the test set, 8/10 (80%) patients had high-risk prostate cancer while 2/10 (20%) had low-intermediate risk prostate cancer. The univariate logistic regression model established with SUVmax, iPSMA-TV and iTL-PSMA could all effectively predict high-risk prostate cancer; the AUC of ROC were 0.843, 0.802 and 0.900, respectively. Based on the test set, the sensitivity and specificity of each model were 87.5% and 50% for SUVmax, 62.5% and 100% for iPSMA-TV, and 87.5% and 100% for iTL-PSMA, respectively. The iPSMA-TV and iTL-PSMA-based predictive model could predict the metastatic risk of prostate cancer, the AUC of ROC was 0.863 and 0.848, respectively, but the SUVmax-based prediction model could not predict metastatic risk.
Conclusions
Semi-quantitative analysis indexes of 68Ga-PSMA-617 PET/CT imaging can be used as “imaging biomarkers” to predict risk stratification and metastatic risk of prostate cancer.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Prostate cancer is a type of tumor with the highest malignancy in men, and about one in six new cases of male cancer worldwide is prostate cancer [1]. The biological behaviors of prostate cancer at different degrees of malignancy also largely differ, directly impacting disease outcome and responses to treatment. Therefore, accurate risk stratification of prostate cancers before treatment and the development of individualized treatment regimen, play a vital role to improve the clinical outcome of patients. For low- and moderate-risk prostate cancer patients, good prognosis and longer biochemical recurrence-free survival may be achieved through active surveillance programs, radical prostatectomy or radiotherapy treatment [2]. However, high-risk prostate cancer patients are at increased risks of metastasis, recurrence and a higher mortality [3]. Currently, the commonly used prostate cancer risk stratification criteria are based on clinical stage, Gleason score (GS), and pre-treatment prostate-specific antigen (PSA) level. Although there are many risk stratification criteria being introduced, the definition of high-risk prostate cancer has not yet been standardized. D’Amico et al. first proposed that patients with PSA > 20 ng/mL or GS ≥8 or clinical stage ≥ T2c are high-risk patients [4]. The American Urological Association (AUA) and the European Association of Urology (EAU) adopted the D’Amico risk stratification criteria [5]. However, the National Comprehensive Cancer Network (NCCN) guidelines are different from the D’Amico criteria, which limit high-risk cancers to those at clinical stage of T3a or above [4, 6]. Interestingly, due to the variations among evaluators that often occur when defining the T stage, it is debatable whether the clinical stage should even be included in the risk stratification criteria. At present, there is a need for an objective and accurate “imaging biomarker” for the diagnosis of high-risk prostate cancers. In this study, we explore the feasibility of establishing such a noninvasive prostate cancer risk stratification criteria based on imaging analysis.
PSMA is a type II transmembrane protein, which has higher expression in cancerous prostate cells than in normal prostate cells. Meanwhile, its expression level is positively correlated with the degree of malignancy, tendency of metastasis and risk of early recurrence [7,8,9,10,11]. In recent years, 68Ga-PSMA PET/CT imaging targeting PSMA was rapidly developed. This new imaging method had shown good clinical application prospects in detecting primary lesions, metastatic lesions and postoperative recurrent lesions of prostate cancer [12,13,14,15,16]. Study results confirmed that levels of 68Ga-PSMA uptake in primary prostate cancer were significantly correlated with GS and pre-treatment PSA levels [17, 18]. Since GS and pre-treatment PSA levels are important indicators for risk stratification of prostate cancers, 68Ga-PSMA PET/CT is potentially valuable in assessing the risk stratification of prostate patients. Currently, Maximum Standardized Uptake Value (SUVmax) is the most commonly used semi-quantitative parameter in PET/CT, which is used to assess tumor burden of prostate cancer, and thus can be used as an “imaging biomarker” to assess the degree of malignancy of prostate cancers. Recent studies proposed volume-based parameters of the 68Ga-PSMA PET/CT, such as PSMA-derived tumor volume (PSMA-TV) and total lesion PSMA(TL-PSMA), which can reflect tumor burden of prostate patients more accurately, and thus are more valuable in assessing patient prognosis and monitoring treatment efficacy [19]. However, the targeted population of this study is postoperative prostate cancer patients, so these studies mainly focused on the correlation between patients’ whole-body tumor burden from metastatic lesions and the PSA levels. There is a lack of research to explore the correlation among volume-based parameters of intraprostatic tumor burden, PSA levels, and the degree of prostate cancer malignancy. It has been confirmed that 68Ga-PSMA PET/CT correlates with the tumor burden of primary prostate cancers relatively well, and its extant of intraprostatic tumor distribution are in good agreement with the histopathological volume of the prostate cancer [20,21,22]. Therefore, this technique may become a novel noninvasive imaging indicator for the assessment of prostate cancer. Building on previous studies, we aim to use semi-quantitative 68Ga-PSMA PET/CT indexes (including SUVmax and volume-based parameters) to analyze the correlation among primary prostate cancer (Primary PCa) imaging, GS and PSA levels, and to evaluate the predictive value of this method for prostate cancer risk stratification and metastasis risk.
Materials and methods
Patients
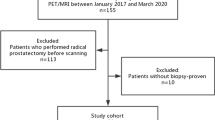
Fifty newly diagnosed patients with biopsy-confirmed prostate cancer were included. A total of 40 patients were consecutively included between May 2016 and June 2017 as the train set for the construction of a predictive model after 68Ga-PSMA-617 PET/CT staging in our hospital. In addition, a total of ten patients were consecutively included between July 2017 and January 2018 as the test set for the testing of accuracy of this predictive model. Inclusion criteria were: biopsy proven diagnosis of prostate cancer and patients signed informed consent and willingness to accept follow-up. Exclusion criteria were: patients who had received local or systemic treatment, or those with incomplete clinical and imaging data. Clinical parameter of all patients such as biopsy, pre-treatment PSA level, rectal examination, pelvic MRI and others were obtained four weeks before the 68Ga-PSMA PET/CT imaging. The median age of 40 patients was 67 years old (median age: 67 years; age range: 51–83 years). According to the NCCN guidelines [6], patients were divided into the low-intermediate risk group (PSA ≤ 20 ng/mL, Gleason score 6-7, and cT1–T2c) and the high-risk group (PSA > 20 ng/mL, Gleason score 8–10, or cT3-T4). Systemic biopsy and postoperative pathology results were collected as references for subsequent semi-quantitative analysis of 68Ga-PSMA-617 PET/CT. This study was approved by the ethics committee of our institute (ethical approve no. 2016YJZ15), and all patients were informed and signed consent.
68Ga-PSMA ligand and PET/CT imaging
DKFZ-PSMA-617 was obtained from ABX advanced biochemical compounds (Radeberg, Germany) and met Good Manufacturing Practice (GMP) quality standards.68Ga was obtained from a 68Ge/68Ga radionuclide generator (ITG, Germany) and used to label PSMA ligand. 68Ga-PSMA-617 was synthesized by incubating 68GaCl3 with the ligand in a pH = 4.0 buffer at 85 °C for 5 min. After a Sep-Pak C18 (Waters, Germany) cartridge purification, the radiotracer was obtained in over 99% radiochemical purification yield by both radio-thin layer chromatography (TLC) and high performance liquid chromatography (HPLC) analysis.
68Ga-PSMA-617 was intravenously injected into each patient (median activity: 215 MBq; range: 110–312 MBq) and PET and CT scans were performed after 60 ± 10 min. The scanning instrument was Gemini TF scanner (Philips Medical Systems, The Netherlands). CT scans were performed from head to the middle-thigh followed by the PET acquisition. CT acquisition and reconstruction parameters were: CT voltage 120 keV, current 100 mAs, pitch 0.8 mm, tube single turn rotation time 0.5 s, and scanning layer thickness 3 mm. CT reconstruction used a standard reconstruction method: 512 × 512 matrix and reconstruction layer thickness of 3~5 mm. PET acquisition and reconstruction used 3D model acquisition, scanned at a total of 9~10 beds, with acquisition time of 90 s for each bed. PET image reconstruction used ordered-subsets expectation maximization method (OSEM). Attenuation corrections of the PET images were performed using data from CT imaging. Whole-body CT and PET images were eventually obtained.
Imaging analysis
All 68Ga-PSMA-617 PET/CT images were analyzed using Fusion Viewer software in the Extended Brilliance Workstation (EBW, Philips, Netherlands). Axial, coronal, and sagittal images of CT scan, PET scan and merged PET/CT images were obtained for whole body analysis. Two experienced nuclear medicine practitioners jointly interpreted all 68Ga-PSMA-617 PET/CT scans, and performed comprehensive analysis on the original and merged images. A consensus conclusion was reached through discussion in case of disagreement. First, position of the prostate cancer lesions on PET/CT image was estimated based on biopsy results. Visual analysis determined whether prostate cancer lesions and surrounding normal prostate tissues can be distinguished. At this time the researchers were only informed of location of the prostate cancer lesions but not the GS score of the patient. If radiotracer uptake of a lesion was higher than its surrounding prostate tissue, the lesion was then identified as positive. The point of the highest radiotracer uptake within the positive prostate cancer lesion was selected as the center, and volume of interests (VOIs) were drawn in 3D using the threshold method, manually adjusting the VOIs to match the edge of the positive lesion. For prostate cancer lesions that cannot be clearly identified, VOIs were drawn directly on the PET/CT images based on information of lesion location and size from postoperative pathology. SUVmax, SUVmean and volume-based parameters in the VOIs were measured and calculated, based on previous studies [17, 19]. Volume-based parameters of 68Ga-PSMA-617 PET/CT in this study included intraprostatic PSMA-derived tumor volume (iPSMA-TV) and intraprostatic total lesion PSMA (iTL-PSMA), where iTL-PSMA = SUVmean * iPSMA-TV. The image analysis method for patients in the test set was similar to that described above. Two physicians experienced in nuclear medicine delineated suspicious prostate cancer lesions in 68Ga-PSMA PET/CT imaging without any knowledge of the clinical data of patients in testing the sample set, meanwhile, SUVmax and volume-based parameters were also obtained. Criteria to determine lymph node and distant metastasis referred to published studies. In addition to normal physiological uptake, radiotracer uptake higher than surrounding tissues in PET images was considered pathological uptake and determined as suspected metastasis. VOIs of the metastatic lesions were drawn using methods similar to that of the primary prostate cancers, and SUVmax of the metastatic lesions was measured. In addition, SUVmax of the non-tumor prostate tissue was measured as a reference of physiological uptake by normal prostate gland. SUVmax of the gluteal muscle was also measured as a baseline reference value. The differences in SUVmax, iPSMA-TV and iTL-PSMA of 68Ga-PSMA-617 PET/CT imaging in different groups of primary prostate cancer patients were analyzed, and the predictive value of the above parameters for prostate cancer risk stratification and metastasis risk were analyzed.
Statistical analysis
Results were reported as percentages, median values and ranges. The correlation among semi-quantitative PET/CT parameters, GS and pre-treatment PSA levels was analyzed using Spearman’s rank correlation coefficient (p). Wilcoxon-Mann-Whitney U-test was used to examine the differences in semi-quantitative PET/CT parameters among subgroups. The SUvmax and volume-based parameters of PET/CT were used to construct the two-class logistics prediction model of prostate cancer risk stratification and metastatic risk. The diagnostic efficiency of the model was evaluated by ROC curve. The cutoff value of the predictive model was obtained from the Youden index, which was used as the standard to test the diagnostic accuracy of this predictive model. All statistical analyses were completed using SPSS version 22.0 software (IBM Corp., Armonk, NY). A P value of less than 0.05 was considered statistically significant.
Results
GS scores of the 40 patients in the train set was 6–10. Gleason scores from TRUS-guided biopsy were 6 in four patients (10%), 7 in 16 patients (40%), 8 in eight patients (20%), 9 in ten patients (25%), and 10 in two patients (5%). The median PSA level in all patients was 35 ng/ml (range of 4–1549 ng/ml), among which 13 patients (33%) had PSA ≤ 20 ng/ml and 27 patients (67%) had PSA > 20 ng/ml. There were 20 cases (50%) with clinical stage greater than or equal to cT3a, and the remaining 50% lower than cT3a. According to the NCCN guidelines, risk stratifications of all patients were as follows: 30 cases of high risk patients (75%), and ten cases of low-intermediate risk patients (25%). Among a total of 40 patients, 17 received radical prostatectomy (referred to as RP), four received external beam radiation therapy (EBRT), 16 received anti-androgens therapy (AS), and three received chemotherapy. Among the patients receiving RP, 4/17 (23%) had different GS of postoperative specimens from that of preoperative biopsy; of these four patients, three had higher GS and one had lower GS. In addition, four (24%) patient’s T staging changed, two changed from T2b to T2c, while two changed from T2c to T3a. However, after comprehensive GS, PSA and T staging, the risk stratification did not change in these patients. When patients in the test and train sets were compared, the differences in their age, height, weight, contrast medium injection volume, GS, PSA level and T staging had no statistical significance (p < 0.05). The basic clinical data of patients are shown in Table 1.
By visual analysis of 68Ga-PSMA-617 PET/CT images of all patients, results showed that 38 of 40 patients (95%) in the train set had a higher radiotracer uptake in their primary prostate cancer lesions than the surrounding normal prostate tissues, while the primary lesions of two patients cannot be visually resolved (5%). These two patients underwent radical prostatectomy surgery, and postoperative pathology determined prostate cancer GS of 6, belonging to the low-intermediate risk prostate cancer group. Although the prostate cancer and normal prostate tissue in these two patients were not distinguishable on 68Ga-PSMA-617 PET/CT, immunohistochemical results showed that PSMA expression in the cancer lesions was higher than that in the surrounding prostate tissues (for an example of a patient without visualization of the primary prostate cancer, see Fig. 1). The visual analysis results showed that there were increased trends of 68Ga-PSMA-617 uptake in the prostate tumor lesions with the Gleason score. The 68Ga-PSMA PET/CT and postoperative pathologic findings were comparatively analyzed in 17 patients receiving RP, the intraprostatic 68Ga-PSMA high uptake sites was consistent with or roughly similar to pathologically identified prostate cancer lesions in 14/17 (76%) patients. In addition, 26/40 patients (65%) also received prostate multiparametric MRI. Both mpMRI and 68Ga-PSMA PET/CT accurately diagnosed prostate cancer in 22/26 (85%) patients, among which, the localization of mpMRI detected lesions was generally consistent with 68Ga-PSMA high uptake sites in 18 patients. Two patients had false negative mpMRI and positive 68Ga-PSMA PET/CT, one patient had true positive mpMRI and false negative 68Ga-PSMA PET/CT, and another patient had false negative results for both imaging techniques.
68Ga-PSMA-617 PET/CT with maximum-intensity projection a, fused PET/CT b and axial PET c, and HE stain d, PSMA stain e of a patient with prostatectomy-proven prostate cancer (cT2b; Gleason score 3 + 3; PSA 4.02 ng/ml). The primary prostate cancer (red arrows pointing to tumor area known from radical prostatectomy) was negative to 68Ga-PSMA-617 PET/CT, but positive to HE stain and PSMA-immunohistochemistry
Semi-quantitative analysis of 68Ga-PSMA-617 PET/CT was performed for all patients. The median SUVmax of all primary prostate cancer lesions was 12.1 (range: 2.4–33.8), which was significantly higher than that of the normal prostate tissues (median SUVmax: 4.0, range: 2.2–6.0) and the gluteal muscle (median SUVmax: 1.0, range: 0.6–1.7). The maximal 68Ga-PSMA-617 uptake of the primary prostate cancer lesion (SUVmax), tumor volume (iPSMA-TV) and tumor total PSMA expression (iTL-PSMA) were all significantly correlated with the Gleason score (Spearman correlation coefficient was 0.42, 0.63 and 0.63 respectively, p < 0.01). Comparing the subgroup with GS ≥ 8 and that with GS < 8, the 68Ga-PSMA-617 PET/CT semi-quantitative parameters of the first group were all higher than that of the latter group, i.e., median SUVmax of 14.2 vs. 10.5, median iPSMA-TV of 26.1 vs. 6.4, and median iTL-PSMA of 147.2 vs. 33.3. These differences were statistically significant (p = 0.01, p < 0.001 and p < 0.001 respectively) (see Table 2).
In addition, semi-quantitative parameters of 68Ga-PSMA-617 PET/CT (such as SUVmax, iPSMA-TV and iTL-PSMA) were positively correlated with PSA levels (Spearman correlation coefficients of 0.43, 0.60 and 0.65 respectively, all at p < 0.01). In the subgroup of patients with PSA > 20 ng/ml, iPSMA-TV and iTL-PSMA of their primary tumors were higher than the patients with PSA ≤ 20 ng/ml, i.e., median iPSMA-TV of 15.0 vs. 5.2, and median iTL-PSMA of 102.4 vs. 28.6. The differences were statistically significant (all p = 0.001). Although the maximum 68Ga-PSMA-617 uptake (SUVmax) in the PSA > 20 ng/ml prostate cancer patient subgroup had a higher trend as compared to that in the PSA ≤ 20 ng/ml subgroup, i.e., median SUVmax of 12.3 vs. 10.1, a statistically significant difference was not reached between the two groups (p = 0.151); see Table 2 for details.
As for the differences in SUVmax and volume-based parameters of 68Ga-PSMA-617 PET/CT imaging in different risk groups, PET/CT semi-quantitative parameters of the high-risk group were all higher than that of the low-intermediate risk group, i.e., median SUVmax of 13.3 vs. 6.9, median iPSMA-TV of 15.0 vs. 6.1, and median iTL-PSMA of 101.7 vs. 25.4. These differences were statistically significant (p = 0.001, p = 0.004 and p < 0.001, respectively) (see Table 2).
A risk prediction model for prostate cancer was constructed based on semi-quantitative parameters of 68Ga-PSMA-617 PET/CT, i.e., SUVmax, iPSMA-TV and iTL-PSMA. The univariate logistic regression model derived from each parameter had good accuracy for the diagnosis of high-risk prostate cancer (p = 0.008, p = 0.049 and p = 0.026 respectively). Area under the ROC curve (AUC) was 0.843 for the SUVmax model, 0.802 for the iPSMA-TV model, and 0.900 for the iTL-PSMA model (see Fig. 2 for details). Positive lesions were observed under 68Ga-PSMA PET/CT in all patients of the testing sample set. Using cutoff values of 0.72, 0.82, and 0.80 for SUVmax, iPSMA-TV and iTL-PSMA, respectively, the sensitivity and specificity of SUVmax, iPSMA-TV and iTL-PSMA for predicting patients with high-risk prostate cancer in the testing sample set were 87.5% and 50% (SUVmax), 62.5% and 100% (iPSMA-TV), and 87.5% and 100% (iTL-PSMA), respectively.
This study also explored the potential value of 68Ga-PSMA-617 PET/CT in predicting the risk of prostate cancer metastasis. High pathological 68Ga-PSMA-617 uptake outside the prostate tissue was detected in 15 of 40 patients (38%) who were identified as metastatic patients. A total of 79 metastatic lymph nodes were detected in 14 patients, and the median SUVmax of all metastatic lymph nodes was 6.9 (range: 1.8–47.5), with median diameter of 0.7 cm (range: 0.3–2.8 cm). Bone metastases were found in nine patients, but semi-quantitative analysis found 52 cases of bone metastases, with median SUVmax of 6.98 (range: 2.2–25.7). In addition, lung metastatic lesion was found in one patient with a SUVmax of 4.74.
Further we analyze the correlation between the risk of metastasis and the radiotracer uptake in primary lesions. It seems that SUVmax, iPSMA-TV and iTL-PSMA in the primary prostate cancer lesions of the metastatic group were all higher than those in the non-metastatic group, among which the inter-group differences in iPSMA-TV and iTL-PSMA were statistically significant, but not the SUVmax (see Table 3 for details). As shown in binary univariate logistic regression analysis of the predictive value of PSMA-derived volume-based parameters and conventional risk factors (e.g. GS, PSA and staging) on prostate cancer metastatic risk, the above parameters were all related to metastatic risk, the obtained OR values were 1.110 for iPSMA-TV, 1.005 for iTL-PSMA, 3.765 for GS, 1.014 for PSA level and 12.184 for staging (all p < 0.05, see Supplementary Table 1). The univariate logistic model constructed by iPSMA-TV and iTL-PSMA can accurately predict the metastatic risk of prostate cancer, and the AUC of the ROC was 0.863 and 0.848, respectively, as shown in Fig. 3. In the test set, five of ten patients (50%) were detected with high pathological 68Ga-PSMA-617 uptake outside the prostate tissue, and were identified as metastatic patients. Using cutoff values of 0.30 and 0.33 for iPSMA-TV and iTL-PSMA, respectively, the sensitivity and specificity of iPSMA-TV and iTL-PSMA for predicting patients with metastatic prostate cancer in the testing sample set were 100% and 100% (iPSMA-TV), and 100% and 80% (iTL-PSMA), respectively.
Discussion
Previous studies have confirmed the application value of 68Ga-PSMA PET/CT in the diagnosis and risk stratification of primary prostate cancer, but most of the published studies were based on 68Ga-PSMA-11 [17, 18, 23], while studies focusing on the newly developed radiotracer 68Ga-PSMA-617 were few. The present study first explored the application value of 68Ga-PSMA-617 PET/CT in primary prostate cancer. The results of this study showed that 68Ga-PSMA-617 PET/CT was able to detect 95% of primary prostate cancer, and the detection rate was similar to that of 68Ga-PSMA-11 PET/CT. Although the prostate cancer lesions could not be identified in two cases (5%) of this study, their GS were both 6, which were considered to be clinically insignificant prostate cancer. The 68Ga-PSMA-617 PET/CT as a non-invasive imaging examination can effectively detect clinically significant prostate cancer to provide useful information for subsequent clinical decision-making.
In addition, the present study also confirmed that semi-quantitative parameters of 68Ga-PSMA-617 PET/CT such as SUVmax, iPSMA-TV and iTL-PSMA, were correlated with GS score and pre-treatment PSA levels, among which these volume-based parameters (iPSMA-TV and iTL-PSMA) had a better correlation with the GS and PSA than the SUVmax. Furthermore, SUVmax, iPSMA-TV and iTL-PSMA of 68Ga-PSMA PET/CT can be used as semi-quantitative “imaging biomarkers” to predict the risk stratification of prostate cancer, while volume-based parameters (iPSMA-TV and iTL-PSMA) can predict the metastatic risk. To our best knowledge, this study is the first to explore the use of multiple semi-quantitative parameters of 68Ga-PSMA-617 PET/CT (including SUVmax and volume-based parameters) to determine the risk stratification and predict the metastatic risk of prostate cancer.
PSMA overexpression in primary prostate cancer was positively correlated with advanced tumor stage, high GS and pre-treatment PSA levels [7, 9, 10]. Another study pointed out that PSMA overexpression of the primary prostate cancer is an independent risk factor for prostate cancer recurrence and metastasis [24]. Therefore, 68Ga-PSMA PET/CT imaging targeting PSMA has a great potential in assessing the risk stratification and metastatic risk of prostate cancer. Previous studies have shown that the maximum uptake value SUVmax of 68Ga-PSMA-11 in primary prostate cancer was significantly associated with GS and PSA levels [17, 18, 25]. Since 68Ga-PSMA-617 and 68Ga-PSMA-11 belong to the same type of PSMA ligands, the maximum uptake value (SUVmax) of 68Ga-PSMA-617 in prostate cancer was similarly correlated with GS and PSA levels, consistent with previous studies on 68Ga-PSMA -11 PET/CT.
In addition to SUVmax, several studies suggested that tumor volume-based semi-quantitative PET/CT parameters, such as the metabolic tumor volume (MTV) and total lesion glycolysis (TLG) in 18F-FDG PET/CT, were better indicators of tumor malignancy and prognosis [26, 27]. Recently, Schmuck et al. first put forward the concept of volume-based parameters of 68Ga-PSMA PET/CT such as PSMA-derived tumor volume (PSMA-TV) and total lesion PSMA (TL-PSMA). They confirmed that for postoperative prostate cancer patients, PSMA-TV and TL-PSMA can better assess the tumor burdens of systemic recurrence and metastatic lesions than SUVmax, which had a better correlation with the patients’ PSA level [19]. There is no study on the application value of volume-based parameters of 68Ga-PSMA PET/CT in assessing primary prostate cancer lesions. Rahbar et al. and Fendler et al. confirmed that the intraprostatic localization and extent of prostate cancer may be estimated by 68Ga-PSMA PET/CT [20, 22]. So volume-based parameters 68Ga-PSMA PET/CT can accurately reflect the actual tumor load in the prostate. Based on these above studies, this study defined parameters such as intraprostatic PSMA-TV (iPSMA-TV) and intraprostatic TL-PSMA (iTL-PSMA) for the evaluation of primary prostate cancer lesions. Our results showed that these volume-based parameters of 68Ga-PSMA PET/CT positively correlated with GS and pre-treatment PSA levels and are superior to SUVmax, which can better reflect the tumor burden and affected range of the primary prostate cancer.
For prostate cancer risk stratification, the risk stratification prediction model constructed by semi-quantitative parameters SUVmax, iPSMA-TV and iTL-PSMA of 68Ga-PSMA-617 PET/CT can accurately identify high-risk prostate cancer patients. These three semi-quantitative parameters can be used as independent “imaging biomarkers” of high-risk prostate cancer to assess patients’ risk. In light of the clinical needs, a good prediction model for high-risk prostate cancer should first have high sensitivity to screen out all patients with high malignancy and high metastatic risk, and have reasonable specificity [28]. In this study, a blinding test in the testing sample set showed that both SUVmax and iTL-PSMA predictive models had high sensitivity (87.5% in both model), but the specificity was more superior with the iTL-PSMA predictive model than with the SUVmax model (specificity was 100% and 50%, respectively), confirming that 68Ga-PSMA PET/CT can be used as an objective noninvasive imaging method to predict high-risk prostate cancer. Given the small sample size of this study, the established predictive model still had good diagnostic efficacy in another group of randomly included patients, confirming better general applicability of the model. However, larger sample size is needed to improve the accuracy and stability of this prediction model. Although the iTL-PSMA prediction model has the best diagnostic performance as compared to the SUVmax and iPSMA-TV predictive models, considering the better objectivity of the operator-independent parameter SUVmax, SUVmax is more suitable for clinical application in the case of similar diagnostic performance.
Previous studies have shown that the metastatic risk of primary prostate cancer is related to Gleason, clinical staging and tumor size [29]. The results of this study also confirmed the correlation between these conventional risk factors and prostate cancer metastasis risk. Furthermore, results of this study suggest that the tumor burden is a risk factor for tumor metastasis. The volume-based parameters of 68Ga-PSMA-617 PET/CT can accurately predict the risk of metastasis. Although SUVmax had a trend to be associated with metastatic risk, statistical significance was not reached. Marc A. Bjurlin proposed [28] “An optimal definition of high-risk prostate cancer should ultimately be a balance that favors high sensitivity, whereby all patients with locally advanced or occult metastatic disease are included, with an acceptable level of specificity, whereby most patients with otherwise organ-confined disease are excluded.” In the diagnosis of high-risk prostate cancer, the assessment of occult metastatic lesions has very important significance. The 68Ga-PSMA PET/CT as a whole-body non-invasive imaging examination can evaluate both primary prostate cancer and metastatic lesions. A series of studies have confirmed that 68Ga-PSMA PET/CT not only is superior to traditional imaging examinations in terms of diagnostic sensitivity and specificity of primary prostate cancer and metastatic lesions, but also can more accurately reflect the malignancy and staging of prostate cancer [30,31,32,33,34,35]. Therefore, 68Ga-PSMA PET/CT has its own advantages in predicting risk stratification of prostate cancer. This study preliminarily confirmed that 68Ga-PSMA-617 PET/CT could predict high-risk prostate cancer and its metastatic risk, which can be used as a reference for the diagnosis of high-risk prostate cancer.
The limitation is that this is a small retrospective study. Nevertheless, through analysis of the limited samples in this study, we found the potential application value of 68Ga-PSMA-617 PET/CT in determining the risk stratification and predicting the metastatic risk of prostate cancer. In the future, a prospective study of larger sample size is needed to further confirm the correlation between these quantitative parameters of 68Ga-PSMA-617 PET/CT and patient outcomes. In addition, although these volume-based parameters of 68Ga-PSMA-617 PET/CT showed a desirable application value than SUVmax, due to the intrinsic measurement errors for these parameters, more PET/CT images and comparative pathological studies are needed to establish accurate and stable lesion quantification measures. Nevertheless, it is exciting that an operator-independent parameter SUVmax can also accurately determine the risk stratification of prostate cancer.
Conclusion
68Ga-PSMA-617 PET/CT is of good application value in the diagnosis and risk stratification of primary prostate cancers. Its semi-quantitative parameters SUVmax and volume-based parameters are correlated with Gleason score and pre-treatment PSA levels, and thus can be used as “imaging biomarkers” to determine prostate cancer risk stratification and risk of metastasis.
References
Torre LA, Bray F, Siegel RL, Ferlay J, Lortet-Tieulent J, Jemal A. Global cancer statistics, 2012. CA Cancer J Clin. 2015;65(2):87–108. https://doi.org/10.3322/caac.21262.
Klotz L, Vesprini D, Sethukavalan P, Jethava V, Zhang L, Jain S, et al. Long-term follow-up of a large active surveillance cohort of patients with prostate cancer. J Clin Oncol. 2015;33(3):272–7. https://doi.org/10.1200/JCO.2014.55.1192.
Cooperberg MR, Broering JM, Carroll PR. Time trends and local variation in primary treatment of localized prostate cancer. J Clin Oncol. 2010;28(7):1117–23. https://doi.org/10.1200/JCO.2009.26.0133.
D'Amico AV, Whittington R, Malkowicz SB, Schultz D, Blank K, Broderick GA, et al. Biochemical outcome after radical prostatectomy, external beam radiation therapy, or interstitial radiation therapy for clinically localized prostate cancer. JAMA. 1998;280(11):969–74.
European Association of Urology Guidelines on prostate cancer. uroweb.org [online]. http://uroweb.org/guideline/prostate-cancer. Accessed 24 April 2018
National Comprehensive Cancer Network. (NCCN) Clinical practice guidelines in oncology. Prostate Cancer, Version 2. 2017. https://www.nccn.org/professionals/physician_gls/pdf/prostate.pdf.
Marchal C, Redondo M, Padilla M, Caballero J, Rodrigo I, Garcia J, et al. Expression of prostate specific membrane antigen (PSMA) in prostatic adenocarcinoma and prostatic intraepithelial neoplasia. Histol Histopathol. 2004;19(3):715–8. https://doi.org/10.14670/HH-19.715.
Minner S, Wittmer C, Graefen M, Salomon G, Steuber T, Haese A, et al. High level PSMA expression is associated with early PSA recurrence in surgically treated prostate cancer. Prostate. 2011;71(3):281–8. https://doi.org/10.1002/pros.21241.
Ross JS, Sheehan CE, Fisher HA, Kaufman RP Jr, Kaur P, Gray K, et al. Correlation of primary tumor prostate-specific membrane antigen expression with disease recurrence in prostate cancer. Clin Cancer Res. 2003;9(17):6357–62.
Sweat SD, Pacelli A, Murphy GP, Bostwick DG. Prostate-specific membrane antigen expression is greatest in prostate adenocarcinoma and lymph node metastases. Urology. 1998;52(4):637–40.
Wright GL Jr, Grob BM, Haley C, Grossman K, Newhall K, Petrylak D, et al. Upregulation of prostate-specific membrane antigen after androgen-deprivation therapy. Urology. 1996;48(2):326–34.
Afshar-Oromieh A, Avtzi E, Giesel FL, Holland-Letz T, Linhart HG, Eder M, et al. The diagnostic value of PET/CT imaging with the (68)Ga-labelled PSMA ligand HBED-CC in the diagnosis of recurrent prostate cancer. Eur J Nucl Med Mol Imaging. 2015;42(2):197–209. https://doi.org/10.1007/s00259-014-2949-6.
Afshar-Oromieh A, Holland-Letz T, Giesel FL, Kratochwil C, Mier W, Haufe S, et al. Diagnostic performance of 68Ga-PSMA-11 (HBED-CC) PET/CT in patients with recurrent prostate cancer: evaluation in 1007 patients. Eur J Nucl Med Mol Imaging. 2017;44(8):1258–68. https://doi.org/10.1007/s00259-017-3711-7.
Ceci F, Uprimny C, Nilica B, Geraldo L, Kendler D, Kroiss A, et al. (68)Ga-PSMA PET/CT for restaging recurrent prostate cancer: which factors are associated with PET/CT detection rate? Eur J Nucl Med Mol Imaging. 2015;42(8):1284–94. https://doi.org/10.1007/s00259-015-3078-6.
Eiber M, Weirich G, Holzapfel K, Souvatzoglou M, Haller B, Rauscher I, et al. Simultaneous 68Ga-PSMA HBED-CC PET/MRI improves the localization of primary prostate cancer. Eur Urol. 2016;70(5):829–36. https://doi.org/10.1016/j.eururo.2015.12.053.
Verburg FA, Pfister D, Heidenreich A, Vogg A, Drude NI, Voo S, et al. Extent of disease in recurrent prostate cancer determined by [(68)Ga]PSMA-HBED-CC PET/CT in relation to PSA levels, PSA doubling time and Gleason score. Eur J Nucl Med Mol Imaging. 2016;43(3):397–403. https://doi.org/10.1007/s00259-015-3240-1.
Uprimny C, Kroiss AS, Decristoforo C, Fritz J, von Guggenberg E, Kendler D, et al. 68Ga-PSMA-11 PET/CT in primary staging of prostate cancer: PSA and Gleason score predict the intensity of tracer accumulation in the primary tumour. Eur J Nucl Med Mol Imaging. 2017;44(6):941–9. https://doi.org/10.1007/s00259-017-3631-6.
Sachpekidis C, Kopka K, Eder M, Hadaschik BA, Freitag MT, Pan L, et al. 68Ga-PSMA-11 dynamic PET/CT imaging in primary prostate cancer. Clin Nucl Med. 2016;41(11):e473–e9. https://doi.org/10.1097/RLU.0000000000001349.
Schmuck S, von Klot CA, Henkenberens C, Sohns JM, Christiansen H, Wester HJ, et al. Initial experience with volumetric 68Ga-PSMA I&T PET/CT for assessment of whole-body tumor burden as a quantitative imaging biomarker in patients with prostate cancer. J Nucl Med. 2017. https://doi.org/10.2967/jnumed.117.193581.
Rahbar K, Weckesser M, Huss S, Semjonow A, Breyholz HJ, Schrader AJ, et al. Correlation of intraprostatic tumor extent with (6)(8)Ga-PSMA distribution in patients with prostate cancer. J Nucl Med. 2016;57(4):563–7. https://doi.org/10.2967/jnumed.115.169243.
Zamboglou C, Drendel V, Jilg CA, Rischke HC, Beck TI, Schultze-Seemann W, et al. Comparison of 68Ga-HBED-CC PSMA-PET/CT and multiparametric MRI for gross tumour volume detection in patients with primary prostate cancer based on slice by slice comparison with histopathology. Theranostics. 2017;7(1):228–37. https://doi.org/10.7150/thno.16638.
Fendler WP, Schmidt DF, Wenter V, Thierfelder KM, Zach C, Stief C, et al. 68Ga-PSMA PET/CT detects the location and extent of primary prostate cancer. J Nucl Med. 2016;57(11):1720–5. https://doi.org/10.2967/jnumed.116.172627.
Zang S, Shao G, Cui C, Li TN, Huang Y, Yao X, et al. 68Ga-PSMA-11 PET/CT for prostate cancer staging and risk stratification in Chinese patients. Oncotarget. 2017;8(7):12247–58. https://doi.org/10.18632/oncotarget.14691.
Perner S, Hofer MD, Kim R, Shah RB, Li H, Moller P, et al. Prostate-specific membrane antigen expression as a predictor of prostate cancer progression. Hum Pathol. 2007;38(5):696–701. https://doi.org/10.1016/j.humpath.2006.11.012.
Koerber SA, Utzinger MT, Kratochwil C, Kesch C, Haefner MF, Katayama S, et al. (68)Ga-PSMA-11 PET/CT in newly diagnosed carcinoma of the prostate: correlation of intraprostatic PSMA uptake with several clinical parameters. J Nucl Med. 2017;58(12):1943–8. https://doi.org/10.2967/jnumed.117.190314.
Park SY, Cho A, Yu WS, Lee CY, Lee JG, Kim DJ, et al. Prognostic value of total lesion glycolysis by 18F-FDG PET/CT in surgically resected stage IA non-small cell lung cancer. J Nucl Med. 2015;56(1):45–9. https://doi.org/10.2967/jnumed.114.147561.
Park SY, Cho A, Bae MK, Lee CY, Kim DJ, Chung KY. Value of 18F-FDG PET/CT for predicting the World Health Organization malignant grade of Thymic epithelial tumors: focused in volume-dependent parameters. Clin Nucl Med. 2016;41(1):15–20. https://doi.org/10.1097/RLU.0000000000001032.
Bjurlin MA, Rosenkrantz AB, Beltran LS, Raad RA, Taneja SS. Imaging and evaluation of patients with high-risk prostate cancer. Nat Rev Urol. 2015;12(11):617–28. https://doi.org/10.1038/nrurol.2015.242.
Tokuda Y, Carlino LJ, Gopalan A, Tickoo SK, Kaag MG, Guillonneau B, et al. Prostate cancer topography and patterns of lymph node metastasis. Am J Surg Pathol. 2010;34(12):1862–7. https://doi.org/10.1097/PAS.0b013e3181fc679e.
Afshar-Oromieh A, Babich JW, Kratochwil C, Giesel FL, Eisenhut M, Kopka K, et al. The rise of PSMA ligands for diagnosis and therapy of prostate cancer. J Nucl Med. 2016;57(Suppl 3):79S–89S. https://doi.org/10.2967/jnumed.115.170720.
Afshar-Oromieh A, Malcher A, Eder M, Eisenhut M, Linhart HG, Hadaschik BA, et al. PET imaging with a [68Ga]gallium-labelled PSMA ligand for the diagnosis of prostate cancer: biodistribution in humans and first evaluation of tumour lesions. Eur J Nucl Med Mol Imaging. 2013;40(4):486–95. https://doi.org/10.1007/s00259-012-2298-2.
Eiber M, Weirich G, Holzapfel K, Souvatzoglou M, Haller B, Rauscher I, et al. Simultaneous (68)Ga-PSMA HBED-CC PET/MRI improves the localization of primary prostate cancer. Eur Urol. 2016;70(5):829–36. https://doi.org/10.1016/j.eururo.2015.12.053.
Maurer T, Gschwend JE, Rauscher I, Souvatzoglou M, Haller B, Weirich G, et al. Diagnostic efficacy of (68)gallium-PSMA positron emission tomography compared to conventional imaging for lymph node staging of 130 consecutive patients with intermediate to high risk prostate cancer. J Urol. 2016;195(5):1436–43. https://doi.org/10.1016/j.juro.2015.12.025.
Sachpekidis C, Baumer P, Kopka K, Hadaschik BA, Hohenfellner M, Kopp-Schneider A, et al. (68)Ga-PSMA PET/CT in the evaluation of bone metastases in prostate cancer. Eur J Nucl Med Mol Imaging. 2018. https://doi.org/10.1007/s00259-018-3936-0.
Janssen JC, Meissner S, Woythal N, Prasad V, Brenner W, Diederichs G, et al. Comparison of hybrid (68)Ga-PSMA-PET/CT and (99m)Tc-DPD-SPECT/CT for the detection of bone metastases in prostate cancer patients: additional value of morphologic information from low dose CT. Eur Radiol. 2018;28(2):610–9. https://doi.org/10.1007/s00330-017-4994-6.
Acknowledgements
We want to express our gratitude to all the members of our PET staff for their contribution in performing this study. We thank Puyun Chen, Weikai Peng, and Yeqing Liu for their technical assistance.
Funding
This study was funded by the National Natural Science Foundation of China projects (81571705), Natural Science Foundation of Beijing Municipality (7171002), Beijing Municipal Commission of Health and Family Planning (2015-3-072), Beijing Nova Program (Z171100001117020), and Interdisciplinary Medicine Seed Fund of Peking University (BMU2017MX007).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
None.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. The study was approved by the Ethics Committee of the Peking University Cancer Hospital & Institute (permit 2016YJZ15).
Informed consent
Informed consent was obtained from all individual participants included in the study.
Electronic supplementary material
Supplementary Table 1
(DOC 30 kb)
Rights and permissions
About this article
Cite this article
Liu, C., Liu, T., Zhang, N. et al. 68Ga-PSMA-617 PET/CT: a promising new technique for predicting risk stratification and metastatic risk of prostate cancer patients. Eur J Nucl Med Mol Imaging 45, 1852–1861 (2018). https://doi.org/10.1007/s00259-018-4037-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00259-018-4037-9