Abstract
Purpose
In patients undergoing 18F-FDG PET/CT, incidental colonic focal lesions can be indicative of inflammatory, premalignant or malignant lesions. The maximum standardized uptake value (SUVmax) of these lesions, representing the FDG uptake intensity, might be helpful in differentiating malignant from benign lesions, and thereby be helpful in determining the urgency of colonoscopy. The aim of our study was to assess the incidence and underlying pathology of incidental PET-positive colonic lesions in a large cohort of patients, and to determine the usefulness of the SUVmax in differentiating benign from malignant pathology.
Methods
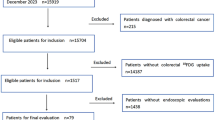
The electronic records of all patients who underwent FDG PET/CT from January 2010 to March 2013 in our hospital were retrospectively reviewed. The main indications for PET/CT were: characterization of an indeterminate mass on radiological imaging, suspicion or staging of malignancy, and suspicion of inflammation. In patients with incidental focal FDG uptake in the large bowel, data regarding subsequent colonoscopy were retrieved, if performed within 120 days. The final diagnosis was defined using colonoscopy findings, combined with additional histopathological assessment of the lesion, if applicable.
Results
Of 7,318 patients analysed, 359 (5 %) had 404 foci of unexpected colonic FDG uptake. In 242 of these 404 lesions (60 %), colonoscopy follow-up data were available. Final diagnoses were: adenocarcinoma in 25 (10 %), adenoma in 90 (37 %), and benign in 127 (53 %). The median [IQR] SUVmax was significantly higher in adenocarcinoma (16.6 [12 – 20.8]) than in benign lesions (8.2 [5.9 – 10.1]; p < 0.0001), non-advanced adenoma (8.3 [6.1 – 10.5]; p < 0.0001) and advanced adenoma (9.7 [7.2 – 12.6]; p < 0.001). The receiver operating characteristic curve of SUVmax for malignant versus nonmalignant lesions had an area under the curve of 0.868 (SD ± 0.038), the optimal cut-off value being 11.4 (sensitivity 80 %, specificity 82 %, positive predictive value 34 %, negative predictive value 98 %).
Conclusion
In these patients with incidental colonic focal activity undergoing PET/CT (the largest series published to date), malignancies had significantly higher SUVmax values than all other types of lesions. However, SUVmax could not distinguish between benign lesions and adenomas. In conclusion, all incidental findings in the colon should be further evaluated and lesions with SUVmax ≥11.4 should be evaluated without delay.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
PET or combined PET/CT using 18F-FDG has found widespread clinical application in the diagnosis and management of both malignant and benign diseases [1–5]. Incidental colonic focal lesions are observed in 1.3 – 3.4 % of patients who undergo FDG PET/CT for other reasons than expected colonic disease [6–11]. Unexpected increased FDG uptake in the large bowel is often nonspecific, yet it can also be indicative of inflammatory sites, or premalignant or malignant lesions [12–14]. Physiological FDG activity is commonly seen in the large bowel, but is usually of relatively low intensity [14] and typically follows a diffuse or linear pattern [12, 15]. Therefore it can hardly be mistaken for malignancy [14]. Yet, occasionally physiological bowel uptake of FDG may be focal [12, 14, 15], which hampers differentiation of a malignant change from a normal variant [14]. FDG PET/CT has been shown to assist differentiation of malignant from benign pulmonary nodules [7, 16]. In the large bowel, however, the capacity of PET/CT to differentiate of benign from malignant disease is to be less clear [15].
A few studies have demonstrated that 8.5 – 21 % of unexpected PET/CT foci in the colon correspond to malignant lesions upon further evaluation [6, 7]. There is a good correlation between the location of FDG uptake and the location of lesions observed on colonoscopy [12, 17]. Therefore, it is currently recommended that all incidentally detected colonic foci should be evaluated by colonoscopy [8, 18, 19].
As focal colonic FDG accumulation is not always related to pathological findings, the decision as to whether to perform further diagnostic evaluation can be difficult. A predictor of the risk of malignancy would therefore be helpful in determining the urgency of colonoscopy. The maximum standardized uptake value (SUVmax), representing the intensity of FDG uptake, is potentially helpful in differentiating malignant from benign FDG activity. Until now, few studies have evaluated the relationship between the SUVmax of incidental colonic PET-positive lesions and the corresponding colonoscopic findings. These small, mainly retrospective studies showed conflicting results [6, 8, 19–21]. One study showed a significant difference in SUVmax between false-positive lesions versus high-grade adenomas and malignancies [22], while five studies concluded that the SUVmax was not able to differentiate different groups of aetiology [6, 8, 19–21]. Therefore, we aimed to evaluate the SUVmax of incidentally detected PET-positive lesions in the colon on PET/CT in a large cohort of patients, and to correlate the SUVmax with the outcome of the corresponding colonoscopy.
Methods
The electronic records of all consecutive patients who had undergone FDG PET/CT during the period January 2010 to March 2013 in the St. Antonius Hospital, Nieuwegein, The Netherlands, were retrospectively reviewed. All patients with incidental focal FDG uptake in the large bowel mentioned in the PET/CT scan report were included. Diffuse, linear or segmental colonic FDG uptake was not taken into account, because this is usually physiological. Uptake was considered incidental in patients with a known gastrointestinal (GI) tract disorder in combination with focal FDG accumulation in areas not consistent with the known preexisting pathology, or in patients referred for PET/CT with a diagnosis of a non-GI tract disorder. The intensity of the FDG uptake was noted as the SUVmax, measured with the hybrid viewer software provided by the workstation manufacturer (Hermes Medical Solutions, Stockholm, Sweden). Only FDG activity greater than that of background liver uptake was considered abnormal. The body-low-dose CT component was used to determine the exact anatomical location of the focus. Electronic records were reviewed for findings on colonoscopy and histopathology, if available.
PET/CT protocol
Imaging was performed with a Philips Gemini TF-64 combined PET/CT device (Philips Medical Systems, Eindhoven, The Netherlands). All patients were prepared for the PET/CT scan in accordance with the EANM and SNMMI guidelines [23, 24]. The capillary blood glucose level of all patients was <10 mmol/L before injection of FDG. The interval between FDG injection (2.5 MBq/kg body weight) and the start of acquisition was 60 ± 5 min. No oral or intravenous contrast medium was used. The emission scan took 3 min per bed position, with 50 % overlapping slices and typically nine or ten bed positions for adequate coverage from the head to the upper legs.
Correlation with colonoscopy
Data regarding subsequent colonoscopy were retrieved from the electronic records of all patients with an incidental finding of focal FDG uptake in the large bowel. Colonoscopy was considered diagnostic if performed within 120 days of the PET/CT scan. In patients with a longer interval between PET/CT and colonoscopy, the focal FDG uptake was considered as not further evaluated and the data were not included in the analysis. Colonoscopy reports were analysed for abnormalities correlating with the incidental finding on the PET/CT scan. When a biopsy or polypectomy of the location of the focus was recorded, the pathology report was subsequently evaluated. The final diagnosis was defined, using colonoscopy findings, combined with additional histological assessment of the lesion, if available. Subsequently, the final diagnosis was placed into one of the following four categories: malignant lesions; advanced adenomas; non-advanced adenomas; and benign lesions (including hyperplastic polyps, inflammatory lesions and normal colonoscopic and/or histopathological findings). Advanced adenomas were defined as adenomas with a size of 1 cm or more, prominent villous features or high-grade dysplasia. Each area of FDG accumulation with negative colonoscopy or histopathological result was considered to represent a site of physiological uptake.
Outcome parameters
The assessed parameters were incidence, final diagnosis and intensity of FDG uptake in incidental colonic focal PET-positive lesions. The location was determined using the body low-dose CT scan. The final diagnosis was made on the basis of corresponding colonoscopic findings, combined with histopathological results, if available. The intensity of FDG uptake was measured in terms of SUVmax, an analogue scale ranging from zero (no uptake) to 40 (maximal uptake).
Statistical analysis
Statistical analysis was performed using SPSS Software for Windows (version 21.0; IBM SPSS statistics, IBM corporation, Chicago, IL, USA). Descriptive statistics were used to describe the incidence of unexpected focal colonic FDG accumulation. The Kruskal-Wallis test was used to compare the median SUVmax between groups in per-patient and per-focus analysis. Differences were considered significant when p < 0.05. An receiver operating characteristic (ROC) curve was plotted to define the optimal cut-off point to differentiate malignant from non-malignant lesions.
Results
Per-patient analysis
Between January 2010 and March 2013, 7,318 patients underwent PET/CT in the St. Antonius Hospital. Of these patients, unexpected colonic focal FDG uptake was mentioned in the PET/CT report of 359 (5 %), and of these 359 patients, 40 had two, and 2 had three separate incidental colonic findings on one PET/CT scan. Colonoscopy was performed in 203 of these 359 patients (57 %) within 120 days (median 25 days [interquartile range, IQR, 13 – 47]) of PET/CT. On colonoscopy, corresponding lesions were detected in 142 of the 203 patients (70 %; Fig. 1).Demographic data of the 203 patients with unexpected focal colonic FDG uptake and corresponding colonoscopy are shown in Table 1.
Of the 359 patients with incidental FDG-avid colonic foci, 156 did not undergo subsequent colonoscopic evaluation. The majority of these patients had advanced illnesses or terminal cancer, so that there were no consequences of a colonoscopy for (palliative) treatment. The reasons for lack of additional colonoscopy are presented in Table 2.
Per-focus analysis
A total of 404 incidentally detected FDG-avid foci in the colon were found, of which 244 (60 %) were followed up with colonoscopy. In two patients, the area of FDG uptake could not be evaluated because the colonoscope was unable to pass a distally located stenotic segment. Of the 242 evaluable sites with unexpected FDG accumulation, 92 (38 %) showed no mucosal abnormality. In the remaining 150 sites; colonic cancer was diagnosed in 25 (10 %), advanced adenomas in 64 (27 %), non-advanced adenomas in 26 (11 %), hyperplastic polyps in 25 (10 %) and inflammation in 10 (4 %). Of the adenomas (advanced and non-advanced), 45 were tubular adenomas, 6 were villous adenomas and 39 tubulovillous adenomas. At sites with no mucosal abnormality, hyperplastic polyps and inflammatory sites were considered benign lesions (Table 3).
The SUVmax of all evaluable areas of increased FDG uptake ranged from 3.1 to 28.4. The overall median SUVmax was 8.7 (IQR 6.3 – 11.4); the median SUVmax in benign lesions, non-advanced adenomas, advanced adenomas and malignant lesions were 8.2, 8.3, 9.7, and 16.6, respectively. There was a significant difference in median SUVmax between the benign and the malignant group (p = 0.0001), between the non-advanced adenoma and the malignant group (p = 0.0001) and between the advanced adenoma and the malignant group (p = 0.001). There was also a significant difference between the advanced adenomas and the benign lesions (p = 0.03). There was no significant difference in median SUVmax between the benign and the non-advanced adenomas, nor between the non-advanced and advanced adenomas (Table 4).
An ROC curve was plotted to evaluate the accuracy of the SUVmax in differentiating malignant from nonmalignant incidentally detected foci in the colon. The area under the curve was 0.868 (SD ± 0.038). The optimal cut-off SUVmax was 11.4 (sensitivity 80 %, specificity 82 %, positive predictive value 34 %, negative predictive value 98 %), in which lesions with SUVmax ≥11.4 had a high risk of being malignant (Fig. 2).
ROC curve of malignant versus nonmalignant incidental FDG-avid lesions in the colon on PET/CT. The area under the curve is 0.868. The optimal SUVmax cut-off to differentiate malignant from nonmalignant incidentally detected foci in the colon is 11.4 (sensitivity 80 %, specificity 82 %, positive predictive value 34 %, negative predictive value 98 %)
Discussion
In 150 (62 %) of 242 evaluated sites with unexpected focal colonic FDG uptake, colonoscopy revealed an abnormal finding. Of the 150 positive lesions, a significant percentage were (pre)malignant: 25 (17 %) adenocarcinomas and 64 (43 %) advanced adenomas. This finding is in accordance with the findings of other studies [6, 17, 24, 25]. However, in 92 foci of increased FDG uptake, despite careful endoscopic examination, no visible lesions were found on colonoscopy, representing 38 % false-positive PET/CT lesions. A possible source of false-positive lesions on PET/CT FDG-PET is (transient) inflammation, physiological uptake [12–15] or uptake in the GI lymphoid tissue [18]. Other studies considering incidental focal FDG-enhanced lesions on PET/CT have shown conflicting false-positive percentages. Peng et al. [10] found a normal colon in 56 % of evaluated patients with focal colonic FDG uptake. Both Gutman et al. [6] and Treglia et al. [25] found that 23 % of unexpected colonic foci had no correlative colonic lesion on colonoscopy, while Putora et al. [8] and Farquharson et al. [11] found a negative colonoscopy result in 13.7 % and 16.7 % of patients with incidental focal colonic FDG uptake, respectively.
We found that malignant lesions had a significantly higher median SUVmax than all other types of lesions. Luboldt et al. [22] found that the mean SUVmax in high-grade adenomas and malignancies were significantly higher than the values in false-positive lesions. However, in five other previous studies evaluating the aetiology of incidental colonic FDG accumulation, no significant differences in median SUVmax were found between different groups of diagnoses [6, 8, 19–21]. We found a median SUVmax of 16.6 (IQR 12 – 20.8) for incidentally found colonic neoplasms, and lower median SUVmax for premalignant and benign lesions (ranging from 8.2 to 9.7). In previous studies a median or mean SUVmax ranging from 5.7 to 17.3 were found for incidental carcinomas in the colon [6, 8, 19, 20–22].
Our results indicate that all incidental focal lesions showing FDG uptake with a SUVmax ≥11.4 have a high risk of being malignant and should be examined by colonoscopy without delay. Luboldt et al. [22] suggested a SUVmax cut-off of ≥5 for differentiating malignant from nonmalignant lesions. This is a much lower cut-off value than we suggested. However, Luboldt et al. included only patients with known colorectal carcinoma. For that reason, the two studies should not be compared. In contrast, however, according to our results, the SUVmax is not able to differentiate benign lesions from non-advanced adenomas. These results indicate that all incidental findings in the colon (including those with SUVmax <11.4) should be further evaluated. This is in accordance with the findings of many previous studies which have also shown that incidental focal colorectal uptake of FDG is associated with a high risk of neoplastic disease, and colonoscopy should be suggested in the PET/CT report [6, 8, 10, 11, 17, 19, 25].
Our study had some limitations. First, approximately 40 % of the patients with unexpected focally increased FDG uptake in the large bowel did not undergo further colonoscopic evaluation (Table 2). Therefore, we are unable to comment on the correlation of the colonoscopic findings of these lesions. However, both the median SUVmax and location of the incidental lesions without colonoscopic evaluation were comparable to those of the lesions followed-up by colonoscopy. The median (IQR) SUVmax was 7.8 (6.3 – 9.6) in the nonevaluated incidental foci, and 27 % and 50 % were located in the ileocaecal region and rectosigmoid, respectively. Of the lesions evaluated by colonoscopy, 23 % and 60 were located in the ileocaecal region and rectosigmoid, respectively. Similar studies have shown comparable percentages on follow-up [6, 8, 11, 17]. Second, in 13 patients, the colonoscopy following the PET/CT scan was not performed to evaluate the unexpected PET/CT focus but for change in stools, rectal bleeding or follow-up of polyps. These patients were nevertheless included in the study if the colonoscopy was performed within 120 days of the PET/CT scan and the lesion correlated with the area of intense FDG uptake was properly described. Last, the baseline characteristics of 203 patients with incidental focal colonic activity and subsequent colonoscopy were retrieved. However, demographic data were not collected for all 7,318 patients who underwent PET/CT. Consequently, these two groups were not compared.
Conclusion
In conclusion, malignant colonic lesions had significantly higher SUVmax values on FDG PET/CT than all other types of lesions. The SUVmax may be helpful in differentiating malignant from nonmalignant lesions, with an optimal cut-off of ≥11.4. However, SUVmax cannot differentiate benign lesions from adenomas. Consequently, all incidental hotspots in the colon should be further evaluated by colonoscopy. SUVmax may help in determining the urgency of colonoscopy, but not in determining whether to perform a colonoscopy or not. SUVmax alone is therefore not sufficiently discriminative to differentiate malignant, premalignant and benign lesions. A prognostic score model including more additional factors (e.g. size of the focus, bowel wall thickening, pathological lymph node) could probably predict the presence and aetiology of pathological changes more precisely.
References
Scheibler F, Zumbé P, Janssen I, Viebahn M, Schröer-Günther M, Grosselfinger R, et al. Randomized controlled trials on PET: a systematic review of topics, design, and quality. J Nucl Med. 2012;53(7):1016–25.
Krause BJ, Schwarzenböck S, Souvatzoglou M. FDG PET and PET-CT. Recent results. Cancer Res. 2013;187:351–69.
Israel O, Keidar Z. PET-CT imaging in infectious conditions. Ann N Y Acad Sci. 2011;1228:150–66.
Treglia F, Taralli S, Giordano A. Emerging role of whole-body 18F-fluorodeoxyglucose positron emission tomography as a marker of disease activity in patients with sarcoidosis: a systematic review. Sarcoidosis Vasc Diffuse Lung Dis. 2011;28(2):87–94.
Cavalcanti Filho JL, de Souza Leão Lima R, de Souza Machado Neto L, Kayat Bittencourt L, Domingues RC, da Fonseca LM. PET-CT and vascular disease: current concepts. Eur J Radiol. 2011;80(1):60–7.
Gutman F, Alberini JL, Wartski M, Vilain D, Le Stanc E, Sarandi F, et al. Incidental colonic focal lesions detected by FDG PET-CT. AJR Am J Roentgenol. 2005;185:495–500.
Zhuang H, Hickeson M, Chacko TK, Duarte PS, Nakhoda KZ, Feng Q, et al. Incidental detection of colon cancer by FDG positron emission tomography in patients examined for pulmonary nodules. Clin Nucl Med. 2002;27:628–32.
Putora PM, Müller J, Borovicka J, Plasswilm L, Schmidt F. Relevance of incidental colorectal FDG-PET-CT-enhanced lesions. Onkologie. 2013;36:200–4.
Kim S, Chung JK, Kim BT, Kim SJ, Jeong JM, Lee DS, et al. Relationship between gastrointestinal F-18-fluorodeoxyglucose accumulation and gastrointestinal symptoms in whole-body PET. Clin Positron Imaging. 1999;2:273–80.
Peng J, He Y, Xu J, Sheng J, Cai S, Zhang Z. Detection of incidental colorectal tumours with 18F-labelled 2-fluoro-2-deoxyglucose positron emission tomography/computed tomography scans: results of a prospective study. Colorectal Dis. 2011;13(11):e374–8.
Farquharson AL, Chopra A, Ford A, Matthews S, Amin SN, De Noronha R. Incidental focal colonic lesions found on 18Fluorodeoxyglucose positron emission tomography/computed tomography scan: further support for a national guideline on definitive management. Colorectal Dis. 2011;14:e56–61.
Prabhakar HB, Sahani DV, Fischman AJ, Mueller PR, Blake MA. Bowel hot spots at PET-CT. Radiographics. 2007;27:145–59.
Zasadny K, Wahl R. Standardized uptake values of normal tissues at PET with 2-[fluorine-18]-fluoro-2-deoxy-D-glucose: variations with body weight and a method for correction. Radiology. 1993;189:847–50.
Cook GJR, Fogelman I, Maisey MN. Normal physiological and benign pathological variants of 18-fluoro-2-deoxyglucose positron emission tomography scanning: potential for error in interpretation. Semin Nucl Med. 1996;26:308–14.
Kostakoglu L, Hardoff R, Mirtcheva R, Goldsmith SJ. PET-CT fusion imaging in differentiating physiologic from pathologic FDG uptake. Radiographics. 2004;24:1411–31.
Vansteenkiste JF, Stroobants SG. The role of positron emission tomography with 18F-fluoro-2-deoxy-D-glucose in respiratory oncology. Eur Respir J. 2001;17:802–20.
Tatlidil R, Jadvar H, Bading JR, Conti PS. Incidental colonic fluorodeoxyglucose uptake: correlation with colonoscopic and histopathologic findings. Radiology. 2002;224:783–7.
Drenth JP, Nagengast FM, Oyen WJ. Evaluation of (pre-)malignant colonic abnormalities: endoscopic validation of FDG-PET findings. Eur J Nucl Med. 2001;28:1766–9.
Kei PL, Vikram R, Yeung HW, Stroehlein JR, Macapinlac HA. Incidental finding of focal FDG uptake in the bowel during PET-CT: CT features and correlation with histopathologic results. AJR Am J Roentgenol. 2010;194(5):W401–6.
Israel O, Yefremov N, Bar-Shalom R, Kagana O, Frenkel A, Keidar Z, et al. PET-CT detection of unexpected gastrointestinal foci of 18F-FDG uptake: incidence, localization patterns, and clinical significance. J Nucl Med. 2005;46(5):758–62.
Chen YK, Kao CH, Liao AC, Shen YY, Su CT. Colorectal cancer screening in asymptomatic adults: the role of FDG PET scan. Anticancer Res. 2003;23(5b):4357–61.
Luboldt W, Volker T, Wiedemann B, Zöphel K, Wehrmann U, Koch A, et al. Detection of relevant colonic neoplasms with PET/CT: promising accuracy with minimal CT dose and a standardised PET cut-off. Eur Radiol. 2010;20(9):2274–85.
Boellaard R, O’Doherty MJ, Weber WA, Mottaghy FM, Lonsdale MN, Stroobants SG, et al. FDG PET and PET/CT: EANM procedure guidelines for tumour PET imaging: version 1.0. Eur J Nucl Med Mol Imaging. 2010;37(1):181–200.
Jamar F, Buscombe J, Chiti A, Christian PE, Delbeke D, Donohoe KJ, et al. EANM/SNMMI guideline for 18F-FDG use in inflammation and infection. J Nucl Med. 2013;54(4):647–58.
Treglia G, Calcagni ML, Rufini V, Leccisotti L, Meduri GM, Spitilli MG, et al. Clinical significance of incidental focal colorectal (18)F-fluorodeoxyglucose uptake: our experience and a review of the literature. Colorectal Dis. 2012;14(2):174–80.
Kamel EM, Thumshirn M, Truninger K, Schiesser M, Fried M, Padberg B, et al. Significance of incidental 18F-FDG accumulations in the gastrointestinal tract in PET-CT: correlation with endoscopic and histopathologic results. J Nucl Med. 2004;45(11):1804–10.
Conflicts of interest
None.
Authors’ contributions
F. van Hoeij: Carried out the data collection, carried out the data analysis and drafted the manuscript.
R. Keijsers: Participated in the design of the study, participated in its coordination, contributed to acquisition and interpretation of data and was involved in drafting the manuscript of revising it critically for important intellectual content.
B. Loffeld: Contributed to collection of data.
G. Dun: Contributed to collection of data.
P. Stadhouders: Participated in the design of the study, contributed to collection of data.
B. Weusten: Participated in the design of the study, participated in its coordination, contributed to analysis, acquisition and interpretation of data and was involved in drafting the manuscript of revising it critically for important intellectual content.
All authors read and approved the final manuscript.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
van Hoeij, F.B., Keijsers, R.G.M., Loffeld, B.C.A.J. et al. Incidental colonic focal FDG uptake on PET/CT: can the maximum standardized uptake value (SUVmax) guide us in the timing of colonoscopy?. Eur J Nucl Med Mol Imaging 42, 66–71 (2015). https://doi.org/10.1007/s00259-014-2887-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00259-014-2887-3