Abstract
Purpose
To investigate the value of 18F-fluorodeoxyglucose positron emission tomography (18F-FDG PET/CT) to predict a pathological complete response (pCR) after neoadjuvant chemotherapy (NAC) in women with human epidermal growth factor receptor 2 (HER2)-positive breast cancer.
Material and methods
Fifty-seven consecutive women with HER2-positive breast cancer, treated with trastuzumab plus taxane-based NAC, were prospectively included. Maximum Standardized Uptake Value of the primary tumor and axillary nodes were measured at baseline (PET1.SUVmax) and after the first course of NAC (PET2.SUVmax). Tumor metabolic volumes were assessed to determine Total Lesion Glycolysis (TLG). The tumor metabolic response (ΔSUVmax and ΔTLG) was calculated.
Results
In univariate analysis, negative hormonal receptor status (p = 0.04), high tumor grade (p = 0.03), and low tumor PET 2 .SUVmax (p = 0.001) were predictive of pCR. Tumor ΔSUVmax correlated with pCR (p = 0.03), provided that tumors with low metabolic activity at baseline were excluded. ΔTLG did not correlate with pCR. In multivariate analysis, tumor PET2.SUVmax < 2.1 was the best independent predictive factor (Odds ratio =14.3; p = 0.004) with both negative and positive predictive values of 76 %. Although the metabolic features of the primary tumor did not depend on hormonal receptor status, both the baseline metabolism and early response of axillary nodes were higher if estrogen receptors were not expressed (p = 0.01 and p = 0.03, respectively).
Conclusion
In HER2-positive breast cancer, very low tumor residual metabolism after the first cycle of NAC (SUVmax < 2.1) was the main predictor of pCR. These results should be further explored in multicenter studies and incorporated into the design of clinical trials.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Neoadjuvant chemotherapy (NAC) is used more and more in order to increase conserving surgery of breast cancer by reducing tumor size [1, 2]. Studies have demonstrated that NAC does not improve survival when compared with adjuvant chemotherapy [3], but women who achieve a pathological complete response (pCR) in the breast and axillary nodes at the end of NAC have significantly improved survival [4].
Breast cancer includes several molecular entities that differ in their clinical behavior, biological characteristics and outcomes [5–7]. The standard of care in the overexpression and/or amplification of human epidermal growth factor receptor 2 (HER2)-positive subtype is characterized by the use of trastuzumab (Herceptin®), which selectively targets HER2 oncoprotein. During neoadjuvant treatment, the synergy between trastuzumab and cytotoxic therapy is very effective. It induces a high rate of complete pathological response at the end of treatment [8] and improves outcomes [9]. However, the features of this HER2-positive subtype are heterogeneous and depend on hormonal receptor (HR) expression [10, 11].
Fluorine-18 fluorodeoxyglucose positron emission tomography (18F-FDG PET/CT) is the gold standard for in vivo evaluation of tumor glucose metabolism. Studies regarding the use of PET/CT to monitor early tumor response to NAC have shown promising results in predicting the final pCR, all tumor subtypes included [12–14]. Nevertheless, because the metabolic behavior of tumors varies considerably among breast cancer subtypes, breast cancer cannot be considered a single entity [15]. Few studies have evaluated the relevance of metabolic response to predict pCR in the HER2-positive subtype specifically, and results are contradictory because of small and heterogeneous patient series [15–18].
The objective of this prospective study was to demonstrate the value of early tumor metabolic changes to predict pCR at surgery in a large group of women with exclusive HER2-positive invasive carcinoma. Different 18F-FDG PET parameters were evaluated, including tumor metabolic volumes. The correlation between PET parameters and the molecular markers of HER2-positive breast cancer, including hormonal receptor status, was also analyzed.
Materials and methods
Patients and treatments
From November 2006 to October 2012, 195 women that were referred to our institution (Centre Georges-François Leclerc, Dijon, France) because of an indication for NAC and clinical stage II or III breast cancer were consecutively evaluated in this prospective study. Only those with non-inflammatory HER2-positive tumors treated with six cycles of standardized trastuzumab and docetaxel-based regimen were included. Patients with high glycemia (> 9 mmol/l) were excluded. The institutional review board approved this prospective study and all women gave their informed consent.
Docetaxel was administered as an intravenous infusion every 3 weeks, at the dose of 100 mg/m2 with a concomitant dose of trastuzumab. About 1 month after the last course of NAC, the tumors were surgically removed, and pCR was defined as no residual invasive cancer in the breast and nodes, though in-situ breast residuals were allowed (ypT0/is ypN0) [10].
Histopathological analysis
Pre-treatment core biopsies from the primary tumor were used to determine the histological type, tumor grade [19], architectural differentiation, nuclear polymorphism and rate of mitosis. The molecular markers examined included estrogen receptor (ER), progesterone receptor (PR) and HER2 expression.
Tumor samples were fixed on buffered formalin, embedded in paraffin and cut with a microtome. Immunohistochemistry was performed with an indirect immunoperoxydase method using antibodies directed against HER2 oncoprotein, ER and PR (HER2: rabbit monoclonal prediluted antibody 4B5; ER: rabbit monoclonal prediluted antibody SP1; PR: rabbit monoclonal prediluted antibody 1E2, Ventana Tucson, AZ, USA). All immunostainings were performed on an automated immunostainer (Ventana XT, Tucson, AZ, USA). ER and PR status were considered positive if the tumor showed at least 10 % of positive cells [20]. HER2 status was graded according to the HercepTest scoring system modified by ASCO/CAP recommendations (0, 1+, 2+ or 3+) [21]. Scores of 3+ were considered positive. In the case of 2+ scores, fluorescent in situ hybridization (FISH) was used to confirm HER2 amplification, using the dual color HER2 and CEN17 probes (ZytoLight, SPEC HER2/CEN17 Dual Color Prob Kit, Zytovision GmbH, Bremerhaven, Germany). HER2 amplification was defined, according to ASCO/CAP criteria, by a ratio of HER2/CEN17 > 2.2 [21].
18F-FDG PET/CT procedures
A first 18F-FDG PET/CT study was performed at baseline. Two different PET/CT imaging systems were used: a Gemini GXL PET/CT scanner from November 2006 to December 2010, and a Gemini TF PET/CT scanner from December 2010 to October 2012 (Philips Medical Systems, Eindhoven, The Netherlands). Patients were instructed to fast for at least 6 h before the intravenous injection of 5 MBq/kg of 18F-FDG for Gemini GXL studies and 3.5 MBq/kg for Gemini TF studies. Emission and transmission scans from the brain to mid-thigh were acquired 60 min later. Scans restricted to the chest with patients in the prone position were started 90 min after the injection of 18F-FDG. Emission data were corrected for dead time, random and scatter coincidences, and attenuation before reconstruction with the RAMLA iterative method. A second 18F-FDG PET/CT study was performed just before the second course of NAC. A chest-restricted acquisition was done 90 min after the injection of the 18F-FDG. For each patient, the same imaging system, 18F-FDG activity and time from injection to acquisition were used for both studies.
A spheroidal volume of interest (VOI) encompassing the primary tumor or nodes was manually drawn on the chest-restricted acquisitions, to measure the Standardized Uptake Value maximal index (SUVmax) at baseline (PET1.SUVmax) and after the first course of NAC (PET2.SUVmax). Measured SUVmax was systematically corrected for body surface area (BSA) and glycemia, as detailed in our previous studies [12, 15].
The metabolic response to NAC was calculated:
Metabolic tumor volume (MTV) was automatically measured inside the tumoral VOI, which had been previously drawn using a dedicated software package (Tumor-tracking; Philips) with margin thresholds set at 41 % of SUVmax, after correction for the breast background activity [threshold = 0.41*(Tumor SUVmax- Contralateral breast background SUVmax)]. Total lesion glycolysis (TLG) was then calculated as SUVmean x MTV, which considers both the metabolic activity and tumor burden. Tumor ∆TLG (%) was calculated.
Three other VOIs were drawn to assess different background SUVmean and SUVmax:
-
on the contralateral breast glandular tissue (breast background)
-
inside the ascending aorta (mediastinal background)
-
on the liver parenchyma, at mid height (hepatic background)
The mediastinal and hepatic SUVmax were used as thresholds on the PET2 examination to distinguish between tumors with low or high residual metabolism.
Statistical analysis
Statistical analysis was performed with the use of WinSTAT software (Microsoft, Redmond, Washington, USA) and Systat software (Systat Inc., Evanston, IL). Data were described by frequency (percentage) or mean and standard deviation (SD).
Correlations between metabolic tumor parameters and the different clinical, biological and pathological variables were assessed with either the Mann–Whitney or the Kruskall-Wallis test.
Tumor metabolic characteristics according to the PET/CT system used and to achievement of pCR were compared with the Mann–Whitney test.
The Chi-square test was used to compare the rates observed.
The predictive value of ΔSUVmax was first evaluated in the whole population. But because previous studies reported ΔSUVmax to be less accurate in response assessment for women with low-metabolic tumors (tumor-to-background ratio of less than 5) [22–24], this analysis was secondly restricted to women with hypermetabolic tumors at baseline. In the present study, a tumor-to-background tumor ratio ≥ 5 was comparable to a tumor PET1.SUVmax ≥ 3.7 (mean contralateral breast tissue SUVmean = 0.74): this threshold was therefore used.
Receiver operating characteristic curves (ROC) were performed to define the optimal threshold of ΔSUVmax and PET2.SUVmax for the prediction of pCR.
Univariate analyses of the different clinical, histopathological and metabolic parameters to predict pCR were performed using a logistic regression model. Multivariate analyses with backward variable selection were done to identify prognostic variables of independent statistical significance. P values < 0.05 were considered significant in all tests.
Results
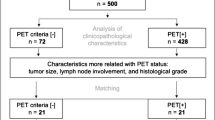
Patients’ characteristics (Table 1)
Among the 195 women evaluated, 72 had HER2-positive breast tumors. Seven of them were excluded because they had undergone a NAC regimen that did not include trastuzumab and docetaxel, and eight were excluded because of obvious upstaging after the first PET exam (stage IV), and in whom NAC was no longer indicated. In the remaining 57 patients, three missed the second PET exams because they declined to continue or because of problems with the equipment. All tumors were invasive ductal carcinoma; none of them belonged to the lobular histological subtype.
The mean tumoral SUVmax (± SD) at baseline was 8.3 ± 4.4 (Table 2) and the mean lymph node SUVmax was 5.9 ± 3.9. After the first cycle of NAC, the mean tumoral PET2.SUVmax was 2.9 ± 1.5. The mean tumoral ∆SUVmax was 58.5 ± 22.7 %. There were no significant differences between patients imaged with the Gemini GXL (n = 39) and the Gemini TF PET/CT (n = 18) systems for mean PET1.SUVmax, PET2.SUVmax and ∆SUVmax.
The mean tumoral TLG1 and ∆TLG (± SD) were calculated at 31.4 ± 38.3 and 84.9 ± 12.8 %, respectively.
The pCR rate was 43.9 % (25/57).
Correlation between metabolic features and clinical/histopathological parameters (Table 2)
Regarding primary tumor metabolism, both higher SUVmax and higher ∆SUVmax were associated with a higher mitotic count (respectively P = 0.001 and P < 0.001). The correlation between ∆TLG and mitotic count was lower (P = 0.02). Baseline TLG was only correlated with PR status: TLG1 was 37.0 ± 40.1 in tumors with negative PR status and 25.7 ± 36.2 in tumors with positive PR status (P = 0.04).
Regarding axillary node metabolism, higher PET1.SUVmax and greater ∆SUVmax were only associated with negative tumor estrogen receptor status. In negative ER tumors, mean PET1.SUVmax was 9.2 ± 4.5 in the nodes and mean ΔSUVmax was 76.6 ± 11.6, whereas these values were 4.7 ± 3.0 and 60.1 ± 19.0 in positive ER tumors (P = 0.01 and P = 0.03, respectively).
Relationship between tumor metabolic parameters and pCR (Tables 3 and 4)
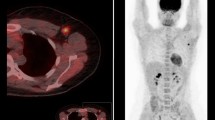
There was a strong correlation between tumor residual SUVmax at PET2 and pathological response: mean PET2.SUVmax was 3.2 ± 1.6 in women without pCR and 2.3 ± 1.1 in those with pCR (P = 0.003) (Fig. 1, Table 3).
ROC analyses were performed for SUV2 for the early prediction of pCR; the area under the curve (AUC) was 0.73 (P = 0.003) (Fig. 2). With an optimal cut-off determined at 2.1, both the negative predictive value (NPV), and the positive predictive value (PPV) of a low PET2.SUVmax to predict pCR were 76 %. Other cut-offs could be used. For example, if the aim rather was to best identify the non-complete responding women, a higher cut-off might be favored to improve the NPV of PET2.SUVmax, but at the expense of the PPV. Indeed, the accurate identification of non-responding women may also be an important point in the design of treatment intensification trials for poor-responding women.
ROC curve analysis of PET2.SUVmax for prediction of pCR. Area under curve = 0.73 ± 0.07; 95 % IC = [0.59–0.88]; p = 0.004; threshold = 2.1; sensitivity is 59 % (13/22), specificity is 88 % (28/32), positive predictive value is 76 % (13/17), negative predictive value is 76 % (28 /37), and accuracy is 76 % (41/54)
Instead of a fixed value, intra-subject background cut-offs (mediastinal or hepatic SUVmax) were used on interim PET to distinguish between tumors with low or high residual metabolism, but this did not predict pCR (P = 0.58 in univariate logistic analysis, both).
In the first analysis, ΔSUVmax did not correlate significantly with pathological response (P = 0.17). But when ΔSUVmax was compared with baseline SUVmax (Fig. 3), we reported ΔSUVmax to be less accurate in response assessment for the subset of five patients with low 18F-FDG uptake at baseline (PET1.SUVmax < 3.7) because of lower metabolic response, despite a 80 % rate of pCR in this subgroup. Therefore a second analysis of ΔSUVmax was restricted to the subset of 52 women with hypermetabolic tumors (PET1.SUVmax ≥ 3.7): there was a correlation between the early percentage decrease in SUVmax and the pathological response at surgery (ΔSUVmax = 58.6 ± 17.6 % in women without pCR vs. 71.3 ± 14.2 % in those with pCR, P = 0.02; Table 3). Using ROC analysis, the AUC was 0.70, 95 % IC = [0.55–0.85], P = 0.02. When an optimal cut-off of 60 % was used, the sensitivity, specificity, positive predictive and negative predictive value of ΔSUVmax to predict pCR were 83 % (15/18), 52 % (16/31), 50 % (15/30), and 84 % (16/19), respectively.
By univariate logistic analysis, tumor PET1.SUVmax (P = 0.03), ΔSUVmax if baseline SUVmax ≥ 3.7 (P = 0.03), tumor PET2.SUVmax (P = 0.001), SBR grade (P = 0.03) and hormonal receptor status (P = 0.04) correlated with pCR (Table 4). By multivariate analysis, tumor PET2.SUVmax was the best independent predictive factor of pCR: a decrease in SUVmax below 2.1 after the first cycle of NAC had a high odds ratio of 14.3 (95 % CI = [2.3–90.9]; P = 0.004).
We found no significant association between the various tumor volume parameters (MTV1, MTV2, ΔMTV, TLG1, TLG2 or ΔTLG) and a pCR.
No correlation was found between axillary metabolic parameters and nodal or tumoral pCR.
Discussion
Because alternative therapies are now available in HER2-positive tumors (e.g. association of an anti-angiogenic drug, dual anti-HER2 blockage, etc.), the early identification of women who do not respond to a trastuzumab/taxane regimen is an important clinical issue. Neoadjuvant chemotherapy allows the quantifiable in vivo assessment of tumor chemosensitivity and is an excellent setting for the translational evaluation of new predictive biomarkers of tumor response.
The interest of the present study is that it included a relatively large population of women with invasive HER2-positive ductal breast carcinoma whose tumor response to taxane and trastuzumab-based neoadjuvant chemotherapy was monitored early with 18F-FDG PET/CT.
Correlation between early metabolic parameters and pCR
The findings demonstrate that in this specific breast cancer subtype, tumor metabolic response after the first cycle of NAC correlated with pCR. Nonetheless, this correlation was strongly linked to the metabolic parameter studied.
A SUVmax lower than 2.1 after the first cycle of NAC was the only independent predictor of pCR (P = 0.004), with an accuracy of 76 %. Because HER2-positive cancers are highly sensitive to trastuzumab associated with chemotherapy, this threshold is very low, meaning a nearly complete metabolic response after the first course of NAC is required to predict pCR. A recent study by Groheux et al., which included 30 patients with the same subtype but a different PET timing (after two courses), also found that a low PET2.SUVmax was the main determinant to predict pCR early, with an accuracy of 90 % [17]. The predictive threshold in this study was higher (SUVmax > 3), but may be explained by a different neoadjuvant regimen, which introduced trastuzumab after four cycles of anthracycline-based chemotherapy.
The predictive value of ΔSUVmax is more conflicting among the few studies. Groheux et al. found an accuracy of 73 % to predict pCR, which is lower than that of PET2.SUVmax [17], but equivalent to the findings of a preliminary study at our institution (76 %) [15]. A study by Koolen et al., however, found that ΔSUVmax evaluated after 3 or 8 weeks of treatment was not accurately associated with a pathological response [18]. Differences between results may be explained by the small numbers of patients, and different regimens and timing for the neoadjuvant treatment.
In the first analysis of the present study, ΔSUVmax was not an appropriate metabolic parameter to predict histological response in the HER2+ subtype. Nonetheless, we observed that, although tumors with low baseline SUVmax frequently reached pCR, their early metabolic response (ΔSUVmax) was always weak and therefore not accurate. This is due to the high impact of the breast background metabolic activity on ΔSUVmax measurements in low-metabolism tumors. This finding is in keeping with previous studies suggesting that ΔSUVmax only be evaluated in cases with a tumor-to-background ratio higher than 5 [22–24]. A statistically significant improvement in the classification of responses was indeed obtained when the predictive value of ΔSUVmax was assessed only in tumors with baseline SUVmax ≥ 3.7 (comparable to a tumor-to-background tumor ratio ≥ 5 because of mean breast tissue SUV measured at 0.74). Similarly, according to the data reported by Groheux et al. [17] , it appeared that none of the four low-metabolism tumors (SUVmax < 3.7) reached the −62 % cutoff used in the study to predict pCR, even though it was finally achieved by three of them, demonstrating many false negative results. Therefore, ΔSUVmax may be an early predictor of pCR, but caution is required when the response of tumors with low tumor-to-background SUVmax ratio is evaluated.
Among other PET parameters, the predictive value of early changes in the metabolic tumor volume was assessed, using the TLG. As previously suggested by a pilot study by Hatt et al., which included a small cohort of 12 women [25], this metabolic parameter was not found to correlate significantly with pCR in the HER2-positive subtype.
The use of intra-subject reference background SUVmax (mediastinal or hepatic) to distinguish between tumors with a poor and those with a good response on interim PET is more robust than absolute SUVmax cut-offs for multicenter settings, and is currently applied in the prognostic stratification of lymphoma [26]. Nevertheless, no predictive value of these thresholds has been found on PET2.
Metabolic characteristics of tumors and lymph nodes according to the clinical and histopathological status
In this HER2-positive subtype, only a higher mitotic activity correlated with both higher baseline tumor metabolism and a greater early decrease in metabolism. These findings corroborate our previous results in a general population of breast cancers [15]. Hormone receptor (HR) status is a major driver of breast cancer clinical phenotype and tumor features, even among HER2-positive patients [10, 11, 27]. The pathological response of tumors to HER2-directed neoadjuvant regimen differs according to ER expression, and a study of Von Minckwitz et al. has reported pCR not to be a prognostic marker in HER2+/HR+ breast cancers [10]. Surprisingly, no significant difference was found in the metabolic behavior of HER2+/HR+ and HER2+/RH- primary tumors, thus confirming the results of Groheux et al. in a smaller cohort of patients [17].
The metabolism of synchronous axillary nodes raises an interesting point: both the baseline metabolism (SUV1) and the early metabolic decrease (ΔSUV) were greater in HER2+/HR- lymph nodes. To our knowledge, this is the first study to evaluate the metabolism of axillary lymph nodes according to the HR status in HER2+ tumors. Several hypotheses could explain these differences. Firstly, breast cancer is a heterogeneous tumor made up of different cell clones [28] that derive from genetic instability acquired by cancer cells during the multi-step process of tumor progression [29]. The few cells that acquire metastatic behavior and present in the involved nodes may have higher proliferation and apoptosis rates in the HER2+/HR- subtype than in the HER2+/HR+ subtype, thus explaining their higher metabolism. Secondly, crosstalk between the ER and HER2 pathways has been shown to play a role in both intrinsic and acquired resistance to endocrine agents and HER2-directed agents in previous studies [30]. Vaz-Luis et al. found a 49 % discordance rate of one of the markers (ER, PR, HER2 status) between HER2-positive primary tumors and metastatic samples, including a switch from HER2-positive to HER2-negative in 17 % of cases [11]. Even though this discordance may be lower between primary and synchronous axillary nodes, the down-regulation of HER2 overexpression in lymph nodes could explain the higher metabolic activity usually observed in the triple-negative subtype [15, 31]. The expression pattern of markers involved in cell proliferation, differentiation and apoptosis in primary and synchronous axillary node metastasis should be compared in the HER2-positive subtype to confirm or rule out these hypotheses.
Limitations of the study
Our study has some limitations. Firstly, only static SUV measurements were performed, while kinetic analysis may present advantages for response assessment [32]. Secondly, due to the small number of women included, we cannot draw any definitive conclusions about the predictive value of PET with an additional stratification of the HER2 subtype into ER-positive and ER-negative tumors. Moreover, the best metabolic surrogate marker of pCR and the optimal threshold may still differ from one single-center trial with small subgroups of patients to another. There is now a crucial need for multicenter prospective trials. One was recently performed (Neo-ALTTO) to determine the value of 18F-FDG PET for the early prediction of response to neoadjuvant lapatinib and trastuzumab, without associated chemotherapy [33]. The results are encouraging: ΔSUVmax was significantly higher in patients who achieved a pCR. Because there had been no prior PET harmonization program, absolute SUVmax were not comparable among cameras and therefore not evaluated. Indeed, the absolute SUVmax measurements can be affected by the use of different PET systems which is currently a limitation for its use as an imaging biomarker in multicentric studies. In contrast, ΔSUV (%) is more reproducible and reliable when data from various scanners with strict intra-subject standardization are analyzed. Guidelines for the Standardization of PET imaging systems have recently been issued and should be applied in multicenter trials using 18F-FDG PET as an imaging biomarker to improve the reproducibility of SUVmax measurements in the future [34, 35].
Conclusion
Because alternative therapies are now available in HER2-positive tumors, the early identification of responding and non-responding women is an important clinical issue. The metabolic response after the first cycle of NAC, assessed with 18FDG-PET, is predictive of the final histological response. Clinical trial now needed to determine whether tailoring early the neoadjuvant drug regimen to the metabolic response could improve the pCR rate in non-responding women and induce a survival benefit.
References
Gralow JR, Burstein HJ, Wood W, Hortobagyi GN, Gianni L, von MG, et al. Preoperative therapy in invasive breast cancer: pathologic assessment and systemic therapy issues in operable disease. J Clin Oncol. 2008;26:814–9.
Fisher B, Brown A, Mamounas E, Wieand S, Robidoux A, Margolese RG, et al. Effect of preoperative chemotherapy on local-regional disease in women with operable breast cancer: findings from National Surgical Adjuvant Breast and Bowel Project B-18. J Clin Oncol. 1997;15:2483–93.
Mauri D, Pavlidis N, Ioannidis JP. Neoadjuvant versus adjuvant systemic treatment in breast cancer: a meta-analysis. J Natl Cancer Inst. 2005;97:188–94.
Kuerer HM, Newman LA, Smith TL, Ames FC, Hunt KK, Dhingra K, et al. Clinical course of breast cancer patients with complete pathologic primary tumor and axillary lymph node response to doxorubicin-based neoadjuvant chemotherapy. J Clin Oncol. 1999;17:460–9.
Perou CM, Sorlie T, Eisen MB, van de RM, Jeffrey SS, Rees CA, et al. Molecular portraits of human breast tumours. Nature. 2000;406:747–52.
Sorlie T, Perou CM, Tibshirani R, Aas T, Geisler S, Johnsen H, et al. Gene expression patterns of breast carcinomas distinguish tumor subclasses with clinical implications. Proc Natl Acad Sci U S A. 2001;98:10869–74.
Sorlie T, Tibshirani R, Parker J, Hastie T, Marron JS, Nobel A, et al. Repeated observation of breast tumor subtypes in independent gene expression data sets. Proc Natl Acad Sci U S A. 2003;100:8418–23.
Buzdar AU, Ibrahim NK, Francis D, Booser DJ, Thomas ES, Theriault RL, et al. Significantly higher pathologic complete remission rate after neoadjuvant therapy with trastuzumab, paclitaxel, and epirubicin chemotherapy: results of a randomized trial in human epidermal growth factor receptor 2-positive operable breast cancer. J Clin Oncol. 2005;23:3676–85.
Gianni L, Eiermann W, Semiglazov V, Manikhas A, Lluch A, Tjulandin S, et al. Neoadjuvant chemotherapy with trastuzumab followed by adjuvant trastuzumab versus neoadjuvant chemotherapy alone, in patients with HER2-positive locally advanced breast cancer (the NOAH trial): a randomised controlled superiority trial with a parallel HER2-negative cohort. Lancet. 2010;375:377–84.
von MG, Untch M, Blohmer JU, Costa SD, Eidtmann H, Fasching PA, et al. Definition and impact of pathologic complete response on prognosis after neoadjuvant chemotherapy in various intrinsic breast cancer subtypes. J Clin Oncol. 2012;30:1796–804.
Vaz-Luis I, Ottesen RA, Hughes ME, Marcom PK, Moy B, Rugo HS, et al. Impact of hormone receptor status on patterns of recurrence and clinical outcomes among patients with human epidermal growth factor-2-positive breast cancer in the National Comprehensive Cancer Network: a prospective cohort study. Breast Cancer Res. 2012;14:R129.
Berriolo-Riedinger A, Touzery C, Riedinger JM, Toubeau M, Coudert B, Arnould L, et al. [18F]FDG-PET predicts complete pathological response of breast cancer to neoadjuvant chemotherapy. Eur J Nucl Med Mol Imaging. 2007;34:1915–24.
Schwarz-Dose J, Untch M, Tiling R, Sassen S, Mahner S, Kahlert S, et al. Monitoring primary systemic therapy of large and locally advanced breast cancer by using sequential positron emission tomography imaging with [18F]fluorodeoxyglucose. J Clin Oncol. 2009;27:535–41.
Rousseau C, Devillers A, Sagan C, Ferrer L, Bridji B, Campion L, et al. Monitoring of early response to neoadjuvant chemotherapy in stage II and III breast cancer by [18F]fluorodeoxyglucose positron emission tomography. J Clin Oncol. 2006;24:5366–72.
Humbert O, Berriolo-Riedinger A, Riedinger JM, Coudert B, Arnould L, Cochet A, et al. Changes in 18F-FDG tumor metabolism after a first course of neoadjuvant chemotherapy in breast cancer: influence of tumor subtypes. Ann Oncol. 2012;23:2572–7.
Koolen BB, Pengel KE, Wesseling J, Vogel WV, Vrancken Peeters MJ, Vincent AD, et al. FDG PET/CT during neoadjuvant chemotherapy may predict response in ER-positive/HER2-negative and triple negative, but not in HER2-positive breast cancer. Breast. 2013;22:691–7.
Groheux D, Giacchetti S, Hatt M, Marty M, Vercellino L, de RA, et al. HER2-overexpressing breast cancer: FDG uptake after two cycles of chemotherapy predicts the outcome of neoadjuvant treatment. Br J Cancer. 2013;109:1157–64.
Koolen BB, Pengel KE, Wesseling J, Vogel WV, Vrancken Peeters MJ, Vincent AD, et al. Sequential (18)F-FDG PET/CT for early prediction of complete pathological response in breast and axilla during neoadjuvant chemotherapy. Eur J Nucl Med Mol Imaging. 2014;41:32–40.
Elston CW, Ellis IO. Pathological prognostic factors in breast cancer. I. The value of histological grade in breast cancer: experience from a large study with long-term follow-up. C. W. Elston & I. O. Ellis. Histopathology. 1991; 19; 403–410. Histopathology. 2002; 41:151–2, discussion.
Zafrani B, Aubriot MH, Mouret E, De CP, De RY, Nicolas A, et al. High sensitivity and specificity of immunohistochemistry for the detection of hormone receptors in breast carcinoma: comparison with biochemical determination in a prospective study of 793 cases. Histopathology. 2000;37:536–45.
Wolff AC, Hammond ME, Schwartz JN, Hagerty KL, Allred DC, Cote RJ, et al. American society of clinical oncology/college of American pathologists guideline recommendations for human epidermal growth factor receptor 2 testing in breast cancer. J Clin Oncol. 2007;25:118–45.
Erdi YE, Mawlawi O, Larson SM, Imbriaco M, Yeung H, Finn R, et al. Segmentation of lung lesion volume by adaptive positron emission tomography image thresholding. Cancer. 1997;80:2505–9.
McDermott GM, Welch A, Staff RT, Gilbert FJ, Schweiger L, Semple SI, et al. Monitoring primary breast cancer throughout chemotherapy using FDG-PET. Breast Cancer Res Treat. 2007;102:75–84.
Doot RK, Dunnwald LK, Schubert EK, Muzi M, Peterson LM, Kinahan PE, et al. Dynamic and static approaches to quantifying 18F-FDG uptake for measuring cancer response to therapy, including the effect of granulocyte CSF. J Nucl Med. 2007;48:920–5.
Hatt M, Groheux D, Martineau A, Espie M, Hindie E, Giacchetti S, et al. Comparison between 18F-FDG PET image-derived indices for early prediction of response to neoadjuvant chemotherapy in breast cancer. J Nucl Med. 2013;54:341–9.
Barrington SF, Qian W, Somer EJ, Franceschetto A, Bagni B, Brun E, et al. Concordance between four European centres of PET reporting criteria designed for use in multicentre trials in Hodgkin lymphoma. Eur J Nucl Med Mol Imaging. 2010;37:1824–33.
Perez EA, Suman VJ, Davidson NE, Gralow JR, Kaufman PA, Visscher DW, et al. Sequential versus concurrent trastuzumab in adjuvant chemotherapy for breast cancer. J Clin Oncol. 2011;29:4491–7.
Heim S, Teixeira MR, Dietrich CU, Pandis N. Cytogenetic polyclonality in tumors of the breast. Cancer Genet Cytogenet. 1997;95:16–9.
Teixeira MR, Pandis N, Bardi G, Andersen JA, Heim S. Karyotypic comparisons of multiple tumorous and macroscopically normal surrounding tissue samples from patients with breast cancer. Cancer Res. 1996;56:855–9.
Gluck S, Arteaga CL, Osborne CK. Optimizing chemotherapy-free survival for the ER/HER2-positive metastatic breast cancer patient. Clin Cancer Res. 2011;17:5559–61.
Groheux D, Giacchetti S, Moretti JL, Porcher R, Espie M, Lehmann-Che J, et al. Correlation of high (18)F-FDG uptake to clinical, pathological and biological prognostic factors in breast cancer. Eur J Nucl Med Mol Imaging. 2011;38:426–35.
Dunnwald LK, Doot RK, Specht JM, Gralow JR, Ellis GK, Livingston RB, et al. PET tumor metabolism in locally advanced breast cancer patients undergoing neoadjuvant chemotherapy: value of static versus kinetic measures of fluorodeoxyglucose uptake. Clin Cancer Res. 2011;17:2400–9.
Gebhart G, Gamez C, Holmes E, Robles J, Garcia C, Cortes M, et al. 18F-FDG PET/CT for early prediction of response to neoadjuvant lapatinib, trastuzumab, and their combination in HER2-positive breast cancer: results from Neo-ALTTO. J Nucl Med. 2013. doi:10.2967/112.119271.
Boellaard R. Standards for PET image acquisition and quantitative data analysis. J Nucl Med. 2009;50 Suppl 1:11S–20S.
Boellaard R. Need for standardization of 18F-FDG PET/CT for treatment response assessments. J Nucl Med. 2011;52 Suppl 2:93S–100S.
Acknowledgments
This study is part of the PharmImage® project. We thank Mr Bastable for proof-reading the text.
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Humbert, O., Cochet, A., Riedinger, JM. et al. HER2-positive breast cancer: 18F-FDG PET for early prediction of response to trastuzumab plus taxane-based neoadjuvant chemotherapy. Eur J Nucl Med Mol Imaging 41, 1525–1533 (2014). https://doi.org/10.1007/s00259-014-2739-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00259-014-2739-1