Abstract
“Ischaemic memory” is defined as a prolonged functional and/or biochemical alteration remaining after a particular episode of severe myocardial ischaemia. The biochemical alteration has been reported as metabolic stunning. Metabolic imaging has been used to detect the footprint left by previous ischaemic episodes evident due to delayed recovery of myocardial metabolism (persistent dominant glucose utilization with suppression of fatty acid oxidation). β-Methyl-p-[123I]iodophenylpentadecanoic acid (BMIPP) is a single-photon emission computed tomography (SPECT) radiotracer widely used for metabolic imaging in clinical settings in Japan. In patients with suspected coronary artery disease but no previous myocardial infarction, BMIPP has shown acceptable diagnostic accuracy. In particular, BMIPP plays an important role in the identification of prior ischaemic insult in patients arriving at emergency departments with acute chest pain syndrome. Recent data also show the usefulness of 123I-BMIPP SPECT for predicting cardiovascular events in patients undergoing haemodialysis. Similarly, SPECT or PET imaging with 18F-FDG injected during peak exercise or after exercise under fasting conditions shows an increase in FDG uptake in postischaemic areas. This article will overview the roles of ischaemic memory imaging both under established indications and in ongoing investigations.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Acute myocardial ischaemia is associated with many pathophysiological and biochemical reactions. Acute ischaemia in acute coronary syndrome (ACS) is usually identified based on electrocardiography (ECG) changes, wall motion abnormalities found on echocardiography, elevated serum biomarkers, and chest discomfort [1–4]. However, in some patients with unstable angina, ECG changes may be nondiagnostic and serum biomarkers may not be elevated, and therefore accurately diagnosing ASC may be difficult for emergency physicians and cardiologists.
An imaging method that could identify a persistent physiological consequence of recent myocardial ischaemia would be of particular interest since it could establish a causal relationship between an episode of chest pain and acute myocardial ischaemia [4]. One method is to image P-selectin which is rapidly mobilized to the endothelial surface under myocardial ischaemia. Greater adhesion of P-selectin to the postischaemic myocardium has been identified through molecular echocardiography involving microbubbles in rats undergoing experimental ischaemia and reperfusion [5]. The current report is the first to deal with the concept of molecular ultrasonic imaging of ischaemic memory. One of the main hallmarks of myocardial ischaemia is an inflammatory cascade, for example involving endothelial overexpression of leucocyte adhesion molecules. In addition, a reduction in myocardial perfusion with regional wall motion abnormality is often associated with coronary occlusion [1–4]. Another important aspect of myocardial ischaemia is metabolic shift from the use of aerobic fatty acid substrate to anaerobic glucose metabolism in the ischaemic myocardium [6–8]. These methods of identifying recent ischaemia (memory) of the myocardium may play an important role in accurately diagnosing and determining the severity of myocardial ischaemia [9].
There are a number of alternative methods for identifying persistent functional alterations after ischaemia. Myocardial perfusion study using single-photon emission computed tomography (SPECT) has been used in patients with acute chest pain. When a perfusion tracer is injected during or shortly after chest pain, the tracer is immediately trapped in the myocardium. Therefore, regional myocardial ischaemia may be identified on SPECT imaging after resolution of the chest pain [10]. However, since there may be rapid recovery of myocardial perfusion, one limitation of a perfusion study is false-negative findings [11]. Quantitative analysis of regional wall motion may be used to assess postsystolic dysfunction after recovery from myocardial ischaemia. Tissue strain echocardiography can potentially identify prolonged abnormalities in regional function after ischaemia [12]. While echocardiography can be useful for serial monitoring of global and regional left ventricular function after ischaemia, it may have limited value for ischaemic memory imaging. Transient myocardial ischaemia may often cause persistent regional dysfunction after the recovery phase of myocardial perfusion without leaving evidence of myocardial necrosis. Such delayed recovery of regional function after reperfusion (stunned myocardium) is well documented [1–4, 13]. In addition, delayed recovery of myocardial metabolism (metabolic stunning) has been reported [14, 15].
During fasting, the human heart uses free fatty acids as a major energy source under normoxic conditions [15]. During myocardial ischaemia, the myocardial energy metabolism is shifted from fatty acid utilization to glucose utilization. After recovery from myocardial ischaemia, such accelerated glucose utilization may persist as a form of compensatory energy production [15]. Schelbert et al. were the first to demonstrate the alteration in fatty acid metabolism using 11C-palmitate in a canine ischaemic model [16]. Occlusion-reperfusion canine studies with chronic myocardial ischaemia have suggested prolonged metabolic alteration over 4 weeks after 30 min of coronary occlusion, which is associated with sustained myocardial metabolic dysfunction [16–18]. Such metabolic adaptation may represent the earliest response to myocardial ischaemia and may continue after reperfusion [19]. These earlier studies identified this pathophysiological condition especially in myocardial metabolism and suggested the usefulness of metabolic imaging for detecting prior ischaemic episodes. Initial findings gave rise to the concept of ischaemic memory imaging.
We introduced the concept of ischaemic memory as a component of the ischaemic footprint and defined it as a prolonged functional or metabolic alteration after recovery from severe ischaemia [7, 20–22]. Later studies have confirmed the clinical importance of this concept [19, 23, 24]. Radionuclide imaging of myocardial metabolism has been developed as ischaemic memory imaging for the detection of metabolically dysfunctional myocardium [7, 20, 21]. Ischaemic memory imaging has had a great impact on the ability to identify areas that have previously experienced myocardial ischaemic insult without having to use pharmacological or exercise stress. In this article, we provide an overview of ischaemic memory imaging.
Ischaemic memory imaging using fatty acid analogues
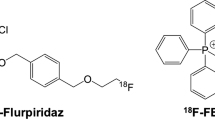
There are a number of radionuclide techniques for evaluating fatty acid metabolism in vivo [25]. Among them, radiolabelled fatty acid imaging has been the most widely used for ischaemic memory imaging in clinical settings. With various radiolabelled fatty acids and fatty acid analogues, 123I-labelled 15-(p-iodophenyl)-3(R,S)-methyl pentadecanoic acid (BMIPP) has been extensively studied in basic research and clinical settings. BMIPP was approved for clinical use and for reimbursement by the Japanese Ministry of Health, Labor, and Welfare in March 1993. To date, BMIPP has been approved only for clinical use in Japan and many clinical reports have been published in Japan [22]. BMIPP is a methyl-branched fatty acid analogue that inhibits beta-oxidation [25]. This compound is designed for high uptake in the myocardium with slow washout from the myocardium. In normal myocardium, BMIPP enters the myocardial cell as BMIPP-CoA and most of the fraction is retained in the lipid pool. Back-diffusion into the blood is very limited. A very small fraction of BMIPP-CoA metabolizes into the end-product p-iodophenylacetic acid via alpha-oxidation followed by beta-oxidation [7, 26]. Of note, increased back-diffusion of nonmetabolized BMIPP from the myocardium appears in postischaemic myocardium [27] (Fig. 1). These properties of BMIPP make it suitable for SPECT imaging. On the other hand, BMIPP uptake may not directly reflect fatty acid oxidation. Instead, BMIPP uptake is based on fatty acid uptake, the turnover rate of the lipid pool, and adenosine triphosphate concentration [28]. In most clinical settings, the combination of the iodinated fatty acid imaging and perfusion imaging is required to demonstrate perfusion/fatty acid metabolism mismatch (Fig. 2).
Representative patient: a 73-year-old woman who had three-vessel coronary bypass graft surgery. One month after surgery, she had exercise stress–rest perfusion imaging and rest BMIPP imaging. The stress perfusion SPECT showed mild perfusion abnormalities in the inferolateral region (arrows). In contrast, BMIPP SPECT identified severe reduction of BMIPP uptake in the same area (arrowheads)
The radiation dosage from 123I-BMIPP is 4.7 mSv per 5 mCi injection [29].
Image acquisition and interpretation
In view of myocardial substrate use, BMIPP is usually administered intravenously under fasting conditions in a non-emergency setting. The majority of other BMIPP studies in non-emergency settings have been performed under fasting conditions [9, 30], with SPECT imaging obtained 15–30 min after tracer administration [7, 21, 31]. In some facilities additional delayed data acquisition has been performed [23]. BMIPP SPECT images can be evaluated using an approach similar to that for myocardial perfusion imaging. To precisely assess an alteration in fatty acid metabolism, it is recommended that BMIPP and myocardial perfusion imaging be compared to identify the perfusion/fatty acid mismatch pattern [7, 20, 21]. On the other hand, a single BMIPP scan may be used in an emergency room to detect prior ischaemia [23, 24]. In normal subjects, BMIPP shows relatively homogeneous radiotracer distribution in the left ventricular (LV) myocardium [31].
As with myocardial perfusion imaging, a semiquantitative five-point scoring scale with a 17-segment model is applied for BMIPP SPECT imaging [23]. As part of this approach, we recently developed an automated program to evaluate BMIPP SPECT images using a polar map display. This automated quantification analysis of the summed BMIPP score was correlated with standard visual analysis [32].
Basic mechanisms of BMIPP myocardial uptake
A number of reports indicate altered kinetics of BMIPP under various myocardial substrate conditions in a canine model (Table 1). Lipid or glucose infusion significantly increases back-diffusion of nonmetabolized BMIPP in coronary sinus sampling after BMIPP administration [33]. The administration of etomoxir, a fatty acid transporter inhibitor, also increases BMIPP back-diffusion [34]. These data indicate that BMIPP uptake may reflect fatty acid utilization in the myocardium. In an occlusion/reperfusion canine model, Hosokawa et al. [35] showed this increase in the back-diffusion of BMIPP. Such increased back-diffusion may cause a decrease in BMIPP uptake relative to perfusion in severely ischaemic myocardium (Fig. 1).
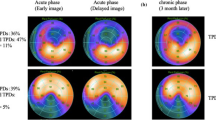
Detecting previous episodes of myocardial ischaemia with BMIPP in acute chest pain
Ito et al. found serial changes in BMIPP uptake and washout in ten patients experiencing a first episode of angina without myocardial infarction but with regional wall motion abnormalities [36]. Significant BMIPP abnormalities were not seen during the acute phase (< 27 h from the first episode) despite severe wall motion and perfusion abnormalities. On the other hand, a significant decrease in BMIPP uptake with increased washout from the myocardium were seen during the subacute phase (5–12 days from the first episode). In contrast, perfusion and systolic function showed only moderate improvement. These preliminary results suggest serial significant changes in BMIPP kinetics during the recovery phase of ischaemic episodes. Such dynamic changes may be associated with changes in the lipid pool size and back-diffusion of the fatty acid pool. While such a result typically leads to BMIPP abnormalities in the first episode of ischaemia, many other clinical conditions may cause BMIPP abnormalities due mainly to repeated ischaemic episodes with delayed recovery of BMIPP (Fig. 3). These abnormalities may be due to a reduced coronary flow reserve in the dysfunctional area. In a study of chronic coronary artery disease (CAD), the severity of BMIPP uptake was found to be closely related to the reduction of coronary flow reserve as assessed by quantitative 15O-labelled water PET myocardial perfusion imaging [37].
Representative patient: a 41-year-old woman who had chest pain and was diagnosed with acute myocardial infarction. Her coronary angiogram shows total occlusion in the left anterior descending artery 6, and stent placement provided immediate revascularization. After 11 days, she had rest myocardial perfusion imaging and BMIPP imaging. While resting myocardial perfusion SPECT performed on admission did not show significant perfusion abnormalities, BMIPP SPECT performed the next day showed a reduction in BMIPP uptake in the anterior to apex (arrows)
Kawai et al. also investigated the use of BMIPP in comparison with myocardial perfusion imaging performed at rest and coronary angiography in 111 consecutive patients with acute chest pain [21]. BMIPP imaging performed within 48 h of the last chest pain showed a sensitivity of 74 % and a specificity of 92 % in identifying significant coronary stenosis; these results were better than those obtained with resting myocardial perfusion imaging also performed within 24 h of the onset of chest pain. This report is the first to show the value of BMIPP in identifying prior ischaemic insult after recovery from chest pain in emergency departments. Other studies also support this finding [38, 39]. Based on these previous three studies comparing the diagnostic accuracy of BMIPP and myocardial perfusion imaging, BMIPP showed higher sensitivity than myocardial perfusion imaging (Table 2). In contrast, BMIPP and myocardial perfusion imaging showed similar specificity for detecting ACS or unstable angina.
BMIPP has been studied mainly in Japan since March 1993. The clinical value of BMIPP imaging has recently been recognized in the US. Kontos et al. in a multicentre study involving over 500 patients in emergency departments found that BMIPP may add incremental value to the early diagnosis of ACS, potentially allowing the presence or absence of ACS to be determined earlier in the evaluation process. On a five-point scoring scale with a 17-segment model, a BMIPP score of ≥12 was associated with cardiac death [40]. This multicentre study confirmed the incremental value of BMIPP imaging to the clinical information in those suspected of having ACS.
Possibility for detecting mild to moderate ischaemia
The most common indication for BMIPP SPECT has been unstable angina implying a severe ischaemic episode. Although data are limited, there has been some examination of the relationship between rest BMIPP and mild to moderate ischaemia with myocardial perfusion imaging or negative stress myocardial perfusion imaging.
Two studies have looked at the discrepancy between a positive BMIPP defect and negative stress myocardial perfusion imaging. Iwado et al. found that only one patient among 24 showed a BMIPP defect in spite of negative thallium stress myocardial perfusion imaging. These patients did not have coronary stenosis after revascularization [41]. This might indicate that there is little possibility of detecting mild ischaemia using BMIPP. Another study showed that the discrepancies between BMIPP findings and stress myocardial perfusion imaging data are very limited. With negative thallium imaging, the incidence of a positive BMIPP defect was limited and in most patients there was multivessel disease. Only one patient did not have abnormal coronary artery stenosis, suggesting very mild ischaemia [42]. These results suggest that there is little possibility of detecting mild ischaemia using BMIPP. Among patients who had no coronary stenosis, 23 % showed a BMIPP defect. The frequency of an abnormal BMIPP finding increased in proportion to the extent of coronary vessel lesions [43]. This study did not actually compare mild to moderate ischaemia with a BMIPP abnormality. However, based on these findings, a BMIPP defect might be associated with mild ischaemia in some patients.
Using a different approach, Dilsizian compared stress–rest thallium myocardial perfusion imaging and found a correlation between the thallium summed stress score and the BMIPP defect score. Based on their findings, a mild to moderate range of thallium summed stress score (4 to 11) seems to correlate with the BMIPP defect score (less than 10) [6]. Currently available data on the association between mild to moderate ischaemia and BMIPP findings are limited. Further examination of this possibility is required.
Vasospastic angina
Another application of BMIPP imaging is in patients with vasospastic angina (VSA) [44–46]. In these patients, exercise or pharmacological stress may not induce coronary spasms and therefore stress myocardial perfusion imaging may not identify any perfusion abnormalities. Based on these three studies, BMIPP showed good sensitivity and specificity for detecting VSA (Table 2). A regional BMIPP defect was closely associated with acetylcholine- or ergonovine-induced vasospastic coronary territories [44, 45]. The frequency of an abnormal BMIPP defect was higher than that found using rest myocardial perfusion imaging.[44]. In addition, it is difficult to evaluate disease activity using current diagnostic testing. In the follow-up study, patients treated with nitrates or calcium channel blockers showed improved symptoms and reduced BMIPP abnormalities [44]. These data indicate that BMIPP is useful for diagnosing VSA and for evaluating disease activities or therapeutic effects. In the presence of acute chest pain, the diagnosis of VSA is also challenging. In this setting, VSA has been found to be more frequent in patients with BMIPP defects than in patients without BMIPP abnormalities [21]. Rest BMIPP has also been shown to have higher sensitivity in the detection of acute chest pain due to coronary vasospasm than either rest or stress myocardial perfusion imaging [47]. These findings indicate the usefulness of rest BMIPP imaging for diagnosing acute chest pain due to coronary vasospasm. Therefore, BMIPP imaging is considered to be the method of choice for the noninvasive identification of regional abnormalities such as ischaemic memory in these patients.
Prognostic value of BMIPP
Based on the concept that BMIPP abnormalities are associated with severe ischaemia and jeopardized myocardium, we hypothesized that those with severe BMIPP abnormalities may have a poor outcome. A number of studies have indicated that combined BMIPP and perfusion imaging might have prognostic value for identifying high-risk subgroups among patients with CAD without prior myocardial infarction [48–50]. We retrospectively analysed 167 consecutive patients with angina who underwent stress perfusion and resting BMIPP imaging [48]. Over a 48-month follow-up, the BMIPP defect score at rest, stress perfusion score, absence or presence of diabetes, and left ventricular ejection fraction were found to be independent predictors in multivariate Cox analysis (Fig. 4). No hard event was observed in patients with normal BMIPP uptake, whereas two patients with nearly normal stress perfusion but abnormal BMIPP uptake had hard cardiac events. These preliminary reports may indicate that a decrease in BMIPP uptake is an important prognostic indicator independent of stress-induced ischaemia on myocardial perfusion imaging in patients with angina without prior myocardial infarction.
Event-free Kaplan-Meier curves in patients with chronic CAD without evidence of myocardial infarction and normal (BMIPP-negative) and abnormal (BMIPP-positive) imaging. The curves indicate a higher risk of cardiac events in those with abnormal BMIPP uptake (modified from Matsuki et al. [48]; permission obtained from the publisher)
BMIPP has recently been shown to have similar prognostic value in patients with diabetes [51]. The finding of impaired myocardial fatty acid metabolism, which may be detected using BMIPP, may be able to identify individuals with various conditions who are at high risk of a cardiovascular event.
Clinical indications for the use of BMIPP based on clinical guidelines
Since BMIPP has been approved only in Japan, there has been only one set of guidelines developed regarding its clinical use. Based on these previous clinical reports, BMIPP SPECT imaging is considered to be a class I indicator for the diagnosis of unstable angina (class I, evidence level B) according to the guidelines for the clinical use of nuclear cardiology imaging determined by the Japanese Circulation Society [52]. The diagnosis of VSA is a class IIa indicator.
Detection of myocardial ischaemia without stress
There have been a number of reports indicating the clinical value of BMIPP imaging at rest for identifying ischaemic myocardium in CAD patients without evidence of myocardial infarction [39, 43, 44, 46, 53–55]. A systematic review of the published literature confirms that BMIPP imaging at rest shows moderate sensitivity and high specificity in detecting ischaemic lesions in patients with a high prevalence of CAD [30]. It is important to note that all of these data were obtained with BMIPP imaging at rest, not under stress, to identify ischaemia or ischaemic memory.
Dilsizian et al. showed that BMIPP imaging has the unique property of maintaining sensitivity even when performed up to 30 h after symptom resolution with exercise stress [23]. In addition, there was 91 % agreement between BMIPP at rest and stress thallium data regarding ischaemic abnormalities. The aim of this study was to establish a new protocol for detecting myocardial ischaemia using BMIPP.
Myocardial ischaemia detection in patients undergoing haemodialysis and in chronic kidney disease
Another important application of BMIPP imaging is in the diagnosis of CAD in patients undergoing haemodialysis. These patients often have silent myocardial ischaemia. However, for many of these patients, undergoing stress myocardial perfusion imaging may not be feasible. Nishimura et al. demonstrated a high prevalence of BMIPP abnormalities, and coronary arteriography confirmed coronary stenosis in those showing BMIPP abnormalities [52, 56]. In this respect, BMIPP imaging may hold promise for identifying ischaemia at rest without stress study. We prospectively studied 155 patients undergoing haemodialysis without angiographic evidence of coronary obstruction to confirm the high incidence of BMIPP abnormalities [57]. During a mean follow-up of 5.1 years, stepwise Cox hazard analysis indicated that reduced BMIPP uptake and increased insulin resistance were two major independent predictors for cardiac death. Cardiac death-free survival rates at 5 years were the lowest (32.2 %) in the subgroup with both BMIPP summed scores >12 and index of insulin resistance (HOMA-IR) >5.1 compared with any other combination (52.9 – 98.7 %). This study had several new and important findings. One is that patients with undergoing haemodialysis often have microvessel disease without any major obstruction in the coronary arteries, and such patients have a poor outcome. In a similar manner, we prospectively studied 375 asymptomatic patients undergoing haemodialysis and compared the results with BMIPP imaging results. In the follow-up study, we concluded that severe BMIPP defects are associated with a high risk of cardiac death [58]. Furthermore, we have shown similar prognostic value of BMIPP imaging in patients without evidence of CAD undergoing haemodialysis [58]. The results of these single-centre studies showing the prognostic value of BMIPP imaging in patients undergoing haemodialysis have recently been validated through a multicentre study [59].
Such microvessel disease may show up on BMIPP imaging as an area of regional reduction in BMIPP uptake. Furthermore, BMIPP imaging may hold promise for risk stratification in these patients. In its recent guidelines, the Japanese Society for Dialysis Therapy suggested that BMIPP might be useful for assessing the risk of a cardiovascular event [60].
Ischaemic memory imaging using a glucose analogue
Glucose analogue (FDG)
18F-FDG is a glucose analogue (with one hydroxyl group replaced by an 18F) that is used with PET to measure glucose utilization. FDG enters the cells in proportion to the amount of glucose entering via a glucose transporter. After phosphorylation, unlike glucose, 18F FDG-6-phosphate becomes metabolically trapped by the cells. Therefore, FDG myocardial uptake reflects the rate of exogenous glucose utilization. While FDG is most commonly used for oncological studies, it is also used to assess myocardial glucose utilization [8, 13]. In particular, FDG is often used to accurately assess myocardial viability in dysfunctional myocardium [13, 61–63]. Another important clinical application is the use of FDG to detect myocardial ischaemia.
Image acquisition and interpretation
When FDG is administered under postprandial or glucose-loaded conditions, it accumulates on normal, dysfunctional but viable, and ischaemic myocardium, but not on infarcted myocardium. Therefore, FDG imaging can be used to assess myocardial viability under a glucose-loaded conditions. Under fasting conditions, on the other hand, normal myocardium may use fatty acids as a major energy source in preference to glucose, and therefore FDG uptake is suppressed in normal myocardium [64]. Only ischaemic myocardium uses mainly glucose. Thus, FDG accumulates only in ischaemic regions and not in normal regions or along necrotic scars. In order to identify ischaemic myocardium, FDG is administered after a fast of at least 6 h or after an overnight fast [65].
FDG imaging is performed around 60 min after FDG administration by PET, PET/CT, or SPECT with ultra-high energy collimators. SPECT may be performed with two different energy windows simultaneously, and therefore both perfusion and glucose imaging can be performed using a SPECT system after coinjection of a 99mTc perfusion agent and FDG. For example, when both the 99mTc perfusion agent and FDG are administered at peak exercise, a SPECT dual tracer study provides both stress perfusion and stress glucose distribution in the myocardium. For PET acquisitions, a perfusion study may be obtained at peak stress. Immediately after perfusion imaging, FDG is administered and poststress FDG imaging is performed 60 min later.
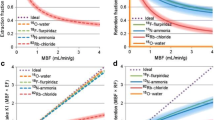
Detection of myocardial ischaemia with FDG
With PET, ischaemic myocardium shows high regional FDG uptake (Fig. 5). Previous animal studies have indicated that this increased postischaemic glucose utilization occurs mainly to replenish myocardial glycogen stores depleted during myocardial ischaemia [18, 66–71]. Using PET, Camici et al. were the first to report an increase in FDG uptake in ischaemic myocardium after exercise in patients with CAD [66]. Similarly, He et al. found increased FDG uptake in the vascular territories of coronary stenosis when FDG was injected at peak exercise under fasting conditions [72]. They used dual-tracer SPECT studies with FDG and 99mTc-sestamibi. SPECT imaging was performed with simultaneous acquisition for perfusion and glucose metabolism using ultra-high energy collimators. They concluded that exercise-induced regional myocardial FDG uptake was highly specific and sensitive for stress-induced myocardial ischaemia [72, 73]. All of these studies may support the concept of a prolonged metabolic shift after recovery from myocardial ischaemia, as previously described. However, this diagnostic approach to the detection of stress-induced myocardial ischaemia using fasting FDG imaging needs further validation before more definite conclusions can be drawn.
Representative patient with unstable angina. Rest–exercise myocardial perfusion PET images show mild stress-induced ischaemia in the lateral region (arrow). High FDG uptake is noted in the same area on the poststress FDG PET image under a fasting state, indicating a postischaemic condition (arrowhead)
Fink et al. studied FDG imaging in patients with chronic kidney disease and demonstrated an inverse relationship between glomerular filtration rate (eGFR) and the metabolic rate of glucose but not between eGFR and cardiac workload [74]. This is the first study to have demonstrated that renal dysfunction may cause preclinical myocardial metabolic changes. However, there are some technical limitations to this approach. Standard fasting conditions may not be reliable for suppressing FDG uptake in normal myocardium. In particular, this study may not be suitable in those with diabetes and/or abnormal glucose tolerance. Fasting FDG study may often show heterogeneous distribution of FDG uptake in normal subjects, mainly due to inadequate fasting conditions [75, 76]. Such normal variation may cause false-positive findings in the identification of ischaemia. In addition, in many patients with CAD, the availability of the imaging technique is limited, and thus this approach is difficult to apply in these patients. Nonetheless, these studies closely support the previous results in animals that showed persistent upregulation of glucose utilization in postischaemic myocardium. On the other hand, the use of SPECT imaging to probe metabolic alterations along with the simultaneous study of myocardial perfusion may hold promise for identifying ischaemic myocardium when FDG becomes more widely available.
Conclusion
“Ischaemic memory” is defined as a phenomenon in which an ischaemic footprint in the form of a prolonged metabolic alteration remains after an episode of severe myocardial ischaemia. Ischaemic memory imaging has been used to identify areas showing metabolic dysfunction, and therefore, it has had a great impact on the identification of areas of prior ischaemic insult. The iodinated fatty acid analogue BMIPP and FDG have been used for this purpose. In particular, BMIPP plays an important role in the identification of prior ischaemic insult in patients with acute chest pain syndrome arriving at emergency departments. The clinical role of ischaemic memory imaging has been extended from the diagnosis of unstable angina to risk assessment in patients who are not suitable stress test subjects such, for example those undergoing haemodialysis (Fig. 6). SPECT or PET imaging with FDG injected during peak exercise or after exercise under fasting conditions have shown increases in FDG uptake in postischaemic areas. The use of ischaemic memory imaging is a new and important alternative to stress myocardial perfusion imaging for identifying ischaemic myocardium.
Ischaemic memory imaging applications. The initially established clinical indications for the use of ischaemic memory imaging are the diagnosis of unstable angina and vasospastic angina. Further indications for the use of ischaemic memory imaging, which are the subject of ongoing investigations, include detection of myocardial ischaemia after exercise stress and assessment of the risk of cardiovascular events in patients in whom stress testing is considered high risk (AP angina pectoris, CKD chronic kidney disease, CVD cardiovascular disease, Diag diagnosis, EX exercise, VSA vasospastic angina)
References
Fallavollita JA, Malm BJ, Canty Jr JM. Hibernating myocardium retains metabolic and contractile reserve despite regional reductions in flow, function, and oxygen consumption at rest. Circ Res. 2003;92:48–55.
Braunwald E, Kloner RA. The stunned myocardium: prolonged, postischemic ventricular dysfunction. Circulation. 1982;66:1146–9.
Bolli R. Mechanism of myocardial “stunning”. Circulation. 1990;82:723–38.
Kloner RA, Jennings RB. Consequences of brief ischemia: stunning, preconditioning, and their clinical implications: part 2. Circulation. 2001;104:3158–67.
Villanueva FS, Lu E, Bowry S, Kilic S, Tom E, Wang J, et al. Myocardial ischemic memory imaging with molecular echocardiography. Circulation. 2007;115:345–52.
Dilsizian V. Metabolic adaptation to myocardial ischemia: the role of fatty acid imaging. J Nucl Cardiol. 2007;14:S97–9.
Tamaki N, Morita K, Kuge Y, Tsukamoto E. The role of fatty acids in cardiac imaging. J Nucl Med. 2000;41:1525–34.
Yoshinaga K, Tamaki N. Imaging myocardial metabolism. Curr Opin Biotechnol. 2007;18:52–9.
Tamaki N, Yoshinaga K. Novel iodinated tracers, MIBG and BMIPP, for nuclear cardiology. J Nucl Cardiol. 2011;18:135–43.
Kosnik JW, Zalenski RJ, Shamsa F, Harris R, Mittner J, Kozlowski J, et al. Resting sestamibi imaging for the prognosis of low-risk chest pain. Acad Emerg Med. 1999;6:998–1004.
Udelson JE, Beshansky JR, Ballin DS, Feldman JA, Griffith JL, Handler J, et al. Myocardial perfusion imaging for evaluation and triage of patients with suspected acute cardiac ischemia: a randomized controlled trial. JAMA. 2002;288:2693–700.
Asanuma T, Uranishi A, Masuda K, Ishikura F, Beppu S, Nakatani S. Assessment of myocardial ischemic memory using persistence of post-systolic thickening after recovery from ischemia. JACC Cardiovasc Imaging. 2009;2:1253–61.
Camici PG, Prasad SK, Rimoldi OE. Stunning, hibernation, and assessment of myocardial viability. Circulation. 2008;117:103–14.
Liedtke AJ. Alterations of carbohydrate and lipid metabolism in the acutely ischemic heart. Prog Cardiovasc Dis. 1981;23:321–36.
Taegtmeyer H, Woods A. Clinical trials report. Metabolic modulation as a principle for myocardial protection. Curr Hypertens Rep. 2003;5:443–4.
Schelbert HR, Henze E, Phelps ME, Kuhl DE. Assessment of regional myocardial ischemia by positron-emission computed tomography. Am Heart J. 1982;103:588–97.
Schwaiger M, Schelbert HR, Ellison D, Hansen H, Yeatman L, Vinten-Johansen J, et al. Sustained regional abnormalities in cardiac metabolism after transient ischemia in the chronic dog model. J Am Coll Cardiol. 1985;6:336–47.
Schwaiger M, Neese RA, Araujo L, Wyns W, Wisneski JA, Sochor H, et al. Sustained nonoxidative glucose utilization and depletion of glycogen in reperfused canine myocardium. J Am Coll Cardiol. 1989;13:745–54.
Taegtmeyer H, Dilsizian V. Imaging myocardial metabolism and ischemic memory. Nat Clin Pract Cardiovasc Med. 2008;5 Suppl 2:S42–8.
Tamaki N, Tadamura E, Kudoh T, Hattori N, Inubushi M, Konishi J. Recent advances in nuclear cardiology in the study of coronary artery disease. Ann Nucl Med. 1997;11:55–66.
Kawai Y, Tsukamoto E, Nozaki Y, Morita K, Sakurai M, Tamaki N. Significance of reduced uptake of iodinated fatty acid analogue for the evaluation of patients with acute chest pain. J Am Coll Cardiol. 2001;38:1888–94.
Tamaki N, Morita K, Kawai Y. The Japanese experience with metabolic imaging in the clinical setting. J Nucl Cardiol. 2007;14:S145–52.
Dilsizian V, Bateman TM, Bergmann SR, Des Prez R, Magram MY, Goodbody AE, et al. Metabolic imaging with beta-methyl-p-[(123)I]-iodophenyl-pentadecanoic acid identifies ischemic memory after demand ischemia. Circulation. 2005;112:2169–74.
Camici PG. Myocardial ischaemia and metabolic memory. Eur J Nucl Med Mol Imaging. 2006;33:4–5.
Knapp Jr FF, Kropp J. Iodine-123-labelled fatty acids for myocardial single-photon emission tomography: current status and future perspectives. Eur J Nucl Med. 1995;22:361–81.
Yamamichi Y, Kusuoka H, Morishita K, Shirakami Y, Kurami M, Okano K, et al. Metabolism of iodine-123-BMIPP in perfused rat hearts. J Nucl Med. 1995;36:1043–50
Hosokawa R, Nohara R, Fujibayashi Y, Okuda K, Ogino M, Hirai T, et al. Myocardial metabolism of 123I-BMIPP in a canine model with ischemia: implications of perfusion-metabolism mismatch on SPECT images in patients with ischemic heart disease. J Nucl Med. 1999;40:471–8.
Fujibayashi Y, Nohara R, Hosokawa R, Okuda K, Yonekura Y, Tamaki N, et al. Metabolism and kinetics of iodine-123-BMIPP in canine myocardium. J Nucl Med. 1996;37:757–61.
Thompson RC, Cullom SJ. Issues regarding radiation dosage of cardiac nuclear and radiography procedures. J Nucl Cardiol. 2006;13:19–23.
Inaba Y, Bergmann SR. Diagnostic accuracy of beta-methyl-p-[123I]-iodophenyl-pentadecanoic acid (BMIPP) imaging: a meta-analysis. J Nucl Cardiol. 2008;15:345–52.
Matsuo S, Nakajima K, Yamashina S, Sakata K, Momose M, Hashimoto J, et al. Characterization of Japanese standards for myocardial sympathetic and metabolic imaging in comparison with perfusion imaging. Ann Nucl Med. 2009;23:517–22.
Yoshinaga K, Matsuki T, Hashimoto A, Tsukamoto K, Nakata T, Tamaki N. Validation of automated quantitation of myocardial perfusion and fatty acid metabolism abnormalities on SPECT images. Circ J. 2011;75:2187–95.
Nohara R, Hosokawa R, Hirai T, Okuda K, Ogino M, Fujibayashi Y, et al. Effect of metabolic substrate on BMIPP metabolism in canine myocardium. J Nucl Med. 1998;39:1132–7.
Kataoka K, Nohara R, Hosokawa R, Hirai T, Okuda K, Li-Guang C, et al. Myocardial lipid metabolism in compensated and advanced stages of heart failure: evaluation by canine pacing model with BMIPP. J Nucl Med. 2001;42:124–9.
Hosokawa R, Nohara R, Fujibayashi Y, Okuda K, Ogino M, Hata T, et al. Myocardial kinetics of iodine-123-BMIPP in canine myocardium after regional ischemia and reperfusion: implications for clinical SPECT. J Nucl Med. 1997;38:1857–63.
Ito K, Sugihara H, Kawasaki T, Katoh S, Azuma A, Nakagawa M. Dynamic changes in cardiac fatty acid metabolism in the stunned human myocardium. Ann Nucl Med. 2001;15:343–50.
Kageyama H, Morita K, Katoh C, Tsukamoto T, Noriyasu K, Mabuchi M, et al. Reduced 123I-BMIPP uptake implies decreased myocardial flow reserve in patients with chronic stable angina. Eur J Nucl Med Mol Imaging. 2006;33:6–12.
Morimoto K, Tomoda H, Yoshitake M, Aoki N, Handa S, Suzuki Y. Prediction of coronary artery lesions in unstable angina by iodine 123 beta-methyl iodophenyl pentadecanoic acid (BMIPP), a fatty acid analogue, single photon emission computed tomography at rest. Angiology. 1999;50:639–48.
Suzuki A, Takada Y, Nagasaka M, Kato R, Watanabe T, Shimokata K, et al. Comparison of resting beta-methyl-iodophenyl pentadecanoic acid (BMIPP) and thallium-201 tomography using quantitative polar maps in patients with unstable angina. Jpn Circ J. 1997;61:133–8.
Kontos MC, Dilsizian V, Weiland F, DePuey G, Mahmarian JJ, Iskandrian AE, et al. Iodofiltic acid I 123 (BMIPP) fatty acid imaging improves initial diagnosis in emergency department patients with suspected acute coronary syndromes: a multicenter trial. J Am Coll Cardiol. 2010;56:290–9.
Iwado H, Iwado Y, Ohmori K, Mizushige K, Yukiiri K, Takagi Y, et al. Latent abnormal fatty acid metabolism in apparently normal perfusion during stress in patients with restenosis after coronary angioplasty: assessment by exercise stress thallium-201 and iodine-123-labeled 15-(p-iodophenyl)-3-R,S-methylpentadecanoic acid-dual myocardial single-photon emission computed tomography. Am J Cardiol. 2004;93:685–8.
Hatano T, Chikamori T, Usui Y, Morishima T, Hida S, Yamashina A. Diagnostic significance of positive I-123 BMIPP despite negative stress Tl-201 myocardial imaging in patients with suspected coronary artery disease. Circ J. 2006;70:184–9.
Yamabe H, Fujiwara S, Rin K, Ando M, Yokoyama M, Sakamoro T, et al. Resting 123I-BMIPP scintigraphy for detection of organic coronary stenosis and therapeutic outcome in patients with chest pain. Ann Nucl Med. 2000;14:187–92.
Nakajima K, Shimizu K, Taki J, Uetani Y, Konishi S, Tonami N, et al. Utility of iodine-123-BMIPP in the diagnosis and follow-up of vasospastic angina. J Nucl Med. 1995;36:1934–40.
Watanabe K, Ohta Y, Toba K, Ogawa Y, Aizawa Y, Tanabe N, et al. Abnormal fatty acid metabolism in patients with coronary vasospasm. Ann Nucl Med. 1999;13:33–41.
Watanabe K, Takahashi T, Miyajima S, Hirokawa Y, Tanabe N, Kato K, et al. Myocardial sympathetic denervation, fatty acid metabolism, and left ventricular wall motion in vasospastic angina. J Nucl Med. 2002;43:1476–81.
Kawai Y, Morita K, Nozaki Y, Ohkusa T, Sakurai M, Tamaki N. Diagnostic value of 123I-betamethyl-p-iodophenyl-pentadecanoic acid (BMIPP) single photon emission computed tomography (SPECT) in patients with chest pain. Comparison with rest-stress 99mTc-tetrofosmin SPECT and coronary angiography. Circ J. 2004;68:547–52.
Matsuki T, Tamaki N, Nakata T, Doi A, Takahashi H, Iwata M, et al. Prognostic value of fatty acid imaging in patients with angina pectoris without prior myocardial infarction: comparison with stress thallium imaging. Eur J Nucl Med Mol Imaging. 2004;31:1585–91.
Chikamori T, Fujita H, Nanasato M, Toba M, Nishimura T. Prognostic value of I-123 15-(p-iodophenyl)-3-(R, S) methylpentadecanoic acid myocardial imaging in patients with known or suspected coronary artery disease. J Nucl Cardiol. 2005;12:172–8.
Nakata T, Hashimoto A, Matsuki T, Yoshinaga K, Tsukamoto K, Tamaki N. Prognostic value of automated SPECT scoring system for coronary artery disease in stress myocardial perfusion and fatty acid metabolism imaging. Int J Cardiovasc Imaging. 2013;29:253–62.
Momose M, Miyake Y, Fukushima K, Nakajima T, Kondo C, Hagiwara N, et al. Prognostic value of (123)I-betamethyl-p-iodophenyl-pentadecanoic acid single-photon emission computed tomography in diabetic patients with suspected ischemic heart disease. Circ J. 2012;76:2633–9.
JCS Working Group; Tamaki N, Kumita S, Kusakabe K, Matsuzaki M, Nishimura T, Senda S, et al. Guidelines for clinical use of cardiac nuclear medicine (JCS 2010) – digest version. Circ J. 2012;76:761–7.
Takeishi Y, Fujiwara S, Atsumi H, Takahashi K, Sukekawa H, Tomoike H. Iodine-123-BMIPP imaging in unstable angina: a guide for interventional strategy. J Nucl Med. 1997;38:1407–11.
Fujiwara S, Takeishi Y, Atsumi H, Takahashi K, Tomoike H. Fatty acid metabolic imaging with iodine-123-BMIPP for the diagnosis of coronary artery disease. J Nucl Med. 1997;38:175–80.
Tateno M, Tamaki N, Yukihiro M, Kudoh T, Hattori N, Tadamura E, et al. Assessment of fatty acid uptake in ischemic heart disease without myocardial infarction. J Nucl Med. 1996;37:1981–5.
Nishimura M, Hashimoto T, Kobayashi H, Fukuda T, Okino K, Yamamoto N, et al. Myocardial scintigraphy using a fatty acid analogue detects coronary artery disease in hemodialysis patients. Kidney Int. 2004;66:811–9.
Nishimura M, Tsukamoto K, Tamaki N, Kikuchi K, Iwamoto N, Ono T. Risk stratification for cardiac death in hemodialysis patients without obstructive coronary artery disease. Kidney Int. 2011;79:363–71.
Nishimura M, Tsukamoto K, Hasebe N, Tamaki N, Kikuchi K, Ono T. Prediction of cardiac death in hemodialysis patients by myocardial fatty acid imaging. J Am Coll Cardiol. 2008;51:139–45.
Moroi M, Tamaki N, Nishimura M, Haze K, Nishimura T, Kusano E, et al. Association between abnormal myocardial fatty acid metabolism and cardiac-derived death among patients undergoing hemodialysis: results from a cohort study in Japan. Am J Kidney Dis. 2013;61:466–75.
Hirakata H, Nitta K, Inaba M, Shoji T, Fujii H, Kobayashi S, et al. Japanese Society for Dialysis Therapy guidelines for management of cardiovascular diseases in patients on chronic hemodialysis. Ther Apher Dial. 2012;16:387–435.
Tillisch J, Brunken R, Marshall R, Schwaiger M, Mandelkern M, Phelps M, et al. Reversibility of cardiac wall-motion abnormalities predicted by positron tomography. N Engl J Med. 1986;314:884–8.
Tamaki N, Kawamoto M, Tadamura E, Magata Y, Yonekura Y, Nohara R, et al. Prediction of reversible ischemia after revascularization. Perfusion and metabolic studies with positron emission tomography. Circulation. 1995;91:1697–705.
Yoshinaga K, Manabe O, Tamaki N. Physiological assessment of myocardial perfusion using nuclear cardiology would enhance coronary artery disease patient care: which imaging modality is best for evaluation of myocardial ischemia? (SPECT-side). Circ J. 2011;75:713–22; discussion 31.
Schelbert HR. 18F-deoxyglucose and the assessment of myocardial viability. Semin Nucl Med. 2002;32:60–9.
Machac J, Bacharach SL, Bateman TM, Bax JJ, Beanlands R, Bengel F, et al. Positron emission tomography myocardial perfusion and glucose metabolism imaging. J Nucl Cardiol. 2006;13:e121–51.
Camici P, Araujo LI, Spinks T, Lammertsma AA, Kaski JC, Shea MJ, et al. Increased uptake of 18F-fluorodeoxyglucose in postischemic myocardium of patients with exercise-induced angina. Circulation. 1986;74:81–8.
McFalls EO, Murad B, Liow JS, Gannon MC, Haspel HC, Lange A, et al. Glucose uptake and glycogen levels are increased in pig heart after repetitive ischemia. Am J Physiol Heart Circ Physiol. 2002;282:H205–11.
Camici P, Ferrannini E, Opie LH. Myocardial metabolism in ischemic heart disease: basic principles and application to imaging by positron emission tomography. Prog Cardiovasc Dis. 1989;32:217–38.
McNulty PH, Jagasia D, Cline GW, Ng CK, Whiting JM, Garg P, et al. Persistent changes in myocardial glucose metabolism in vivo during reperfusion of a limited-duration coronary occlusion. Circulation. 2000;101:917–22.
Araujo LI, McFalls EO, Lammertsma AA, Jones T, Maseri A. Dipyridamole-induced increased glucose uptake in patients with single-vessel coronary artery disease assessed with PET. J Nucl Cardiol. 2001;8:339–46.
Dilsizian V. 18F-FDG uptake as a surrogate marker for antecedent ischemia. J Nucl Med. 2008;49:1909–11.
He ZX, Shi RF, Wu YJ, Tian YQ, Liu XJ, Wang SW, et al. Direct imaging of exercise-induced myocardial ischemia with fluorine-18-labeled deoxyglucose and Tc-99m-sestamibi in coronary artery disease. Circulation. 2003;108:1208–13.
Dou KF, Yang MF, Yang YJ, Jain D, He ZX. Myocardial 18F-FDG uptake after exercise-induced myocardial ischemia in patients with coronary artery disease. J Nucl Med. 2008;49:1986–91.
Fink JC, Lodge MA, Smith MF, Hinduja A, Brown J, Dinits-Pensy MY, et al. Pre-clinical myocardial metabolic alterations in chronic kidney disease. Cardiology. 2010;116:160–7.
Gropler RJ, Siegel BA, Lee KJ, Moerlein SM, Perry DJ, Bergmann SR, et al. Nonuniformity in myocardial accumulation of fluorine-18-fluorodeoxyglucose in normal fasted humans. J Nucl Med. 1990;31:1749–56.
Ohira H, Tsujino I, Yoshinaga K. 18F-Fluoro-2-deoxyglucose positron emission tomography in cardiac sarcoidosis. Eur J Nucl Med Mol Imaging. 2011;38:1773–83.
Acknowledgments
The authors acknowledge Drs. Songji Zhao, Kenichi Nishijima and Yuji Kuge for their assistance in performing supporting basic experiments, and Keiichi Magota, PhD, and Yuuki Tomiyama, MSc, for technical assistance. The work of the authors presented in this article was supported in part by a grant from Nihon Medi-Physics Co., Ltd. (Tokyo, Japan).
Conflicts of Interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Yoshinaga, K., Naya, M., Shiga, T. et al. Ischaemic memory imaging using metabolic radiopharmaceuticals: overview of clinical settings and ongoing investigations. Eur J Nucl Med Mol Imaging 41, 384–393 (2014). https://doi.org/10.1007/s00259-013-2615-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00259-013-2615-4