Abstract
Purpose
Cardiac involvement in sarcoidosis is one of the leading causes of death associated with abnormalities of the conduction system. 18F-FDG PET is useful for detecting inflammatory lesions in cardiac sarcoidosis. However, the relationship between ECG abnormalities and focal 18F-FDG uptake has not been studied. The aim of this study was to evaluate the relationship between electrocardiogram (ECG) abnormalities and the location of elevated myocardial 18F-FDG uptake in patients with sarcoidosis.
Methods
Included in the study were 50 patients (56.3 ± 14.9 years old) with histologically proven sarcoidosis with suspected cardiac involvement based on ECG or echocardiography. All patients had fasted for at least 6 h and were given unfractionated heparin (50 IU/kg) intravenously to reduce the physiological 18F-FDG uptake in the myocardium. The left ventricle (LV) wall was divided into 17 segments by visual analysis. Obvious accumulation in each segment was defined as positive.
Results
Of the 50 patients, 33 showed some ECG abnormalities, including atrioventricular (AV) block in 13. Patients with abnormal ECG findings had a higher number of regions with 18F-FDG uptake than patients without ECG abnormality (3.48 ± 2.73 vs. 1.41 ± 2.09 regions, p = 0.0051). Among ECG abnormalities, the predictor for interventricular septum wall 18F-FDG involvement was AV block (p = 0.0025).
Conclusion
Patients with ECG abnormalities showed a higher number of abnormal 18F-FDG myocardial uptake regions than patients without ECG abnormalities. In particular, focal 18F-FDG uptake in the interventricular septum in cardiac sarcoidosis was associated with AV block. Therefore, determination of regional 18F-FDG distribution might contribute to patient management in cardiac sarcoidosis.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Sarcoidosis is a noncaseating granulomatous disease of unknown aetiology and multiorgan involvement, commonly found in young and middle-aged adults. The incidence of sarcoidosis varies widely due to differences in environmental risk factors and genetic factors [1, 2]. Cardiac involvement in sarcoidosis is associated with morbidity and death. Although the number of patients with cardiac involvement is considered to be limited, recent studies have indicated that it might be one of the major causes of death in sarcoidosis [3]. The severity of cardiac involvement depends on the location and extent of the granulomatous lesions [4, 5]. Clinical manifestations include left ventricular (LV) dysfunction and arrhythmia such as ventricular tachyarrhythmia and conduction disturbance [3, 6]. Previous studies have indicated the possibility of recovery from atrioventricular (AV) nodal dysfunction after steroid therapy [7–10]. However, most patients with advanced AV block are treated by permanent pacemaker implantation. Such a solution is a problem, especially in young patients [11, 12].
Recently diagnosis using 18F-FDG PET has been considered useful given its high sensitivity for cardiac lesion detection [13–17]. Accumulation of 18F-FDG is associated with an active inflammatory process, thus allowing the activity of inflammatory disease to be evaluated [18–20]. Takeda et al. found that cardiac 18F-FDG uptake was associated with conduction disturbance in a patient with cardiac sarcoidosis [9]. Being able to pinpoint the location of 18F-FDG uptake might provide great benefits in treatment planning, particularly when the lesion involves the conduction system [21]. To the best of our knowledge, there has been no study evaluating the relationship between the location of abnormal myocardial 18F-FDG uptake and ECG abnormalities. The aim of this study was to evaluate the association between cardiac segmental 18F-FDG uptake and ECG abnormalities in patients with sarcoidosis.
Materials and methods
Study population
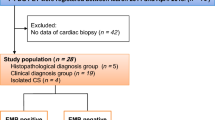
From January 2003 to March 2011, 67 patients with histologically proven sarcoidosis with suspected cardiac involvement because of ECG or echocardiographic abnormalities were prospectively involved in this study. Prior to the present study, none of the patients had been diagnosed as having cardiac involvement sarcoidosis. Cardiac involvement was defined based on the Japanese Ministry of Health and Welfare (JMHW) guidelines for diagnosing cardiac sarcoidosis (Table 1) [22].
We did not include patients with a history of coronary artery disease or any other known heart disease such as myocarditis or other cardiomyopathies in this study. To exclude patients with coronary artery disease, we performed additional evaluations, including stress myocardial perfusion imaging and coronary angiography in those with multiple coronary risk factors. Using echocardiography, we also excluded subjects with valvular heart disease and cardiomyopathy [23, 24]. We also excluded 17 patients who showed diffuse physiological cardiac 18F-FDG uptake [13]. Thus, we analysed 50 patients (11 men, 39 women; 56.3 ± 14.9 years old; Table 2). Of these 50 patients, 24 were diagnosed as having cardiac sarcoidosis based on JMHW diagnostic criteria, and the remaining 26 did not meet the diagnostic criteria for cardiac sarcoidosis.
The study protocol was approved by the ethics committee of Hokkaido University Graduate School of Medicine. Written informed consent was obtained from the patients prior to the study.
PET imaging
All patients fasted for at least 6 h before 18F-FDG PET studies to reduce physiological myocardial uptake of 18F-FDG [13]. In all patients unfractionated heparin (UFH; 50 IU/kg; Mochida, Tokyo) was injected intravenously 15 min prior to 18F-FDG injection also in order to reduce physiological myocardial 18F-FDG uptake [23]. Prior to 18F-FDG PET imaging, we checked contraindications to heparin use such as active bleeding, bleeding risk, and a history of heparin-induced thrombocytopenia. None of the patients in this study population had a contraindication to heparin use. PET imaging was performed using a Siemens ECAT EXACT HR+ scanner (Siemens/CTI, Knoxville, TN; n = 37) or a Biograph 64 TruePoint with TrueV PET/CT scanner (Siemens Japan; n = 13). Transmission scanning for PET or a low-dose CT scan for PET/CT was performed for attenuation correction. Scans were performed 45–60 min after administration of 218.9 ± 57.0 MBq of 18F-FDG. Blood samples were obtained before and 15 min after UFH administration to measure immunoreactive insulin (IRI) and free fatty acids (FFA). The fasting plasma glucose level was measured before 18F-FDG injection.
99mTc-MIBI imaging
Single photon emission computed tomography (SPECT) was performed 60 min after injection of 600 MBq of 99mTc-sestamibi (FUJI RI Pharma, Tokyo, Japan).
Data analysis
ECG data analysis
Resting 12-lead ECG and 24-h ambulatory ECGs were analysed by a cardiologist blinded to the clinical and 18F-FDG PET information. Findings such as right bundle branch block (RBBB), AV block, left-axis deviation, ventricular tachycardia, premature ventricular contraction (PVC) (grade >2 in Lown’s classification), and abnormal Q or ST-T changes were defined as abnormal based on the JMHW guidelines [22].
Transthoracic echocardiography
All patients underwent echocardiography using a 2.5 MHz echo-Doppler probe with a SONOS 5500 imaging system (Agilent Technologies, Andover, MA). The LV end-diastolic and end-systolic dimensions were analysed using M-mode or B-mode echocardiography. LV ejection fraction was obtained using the modified biplane Simpson’s method.
Findings such as abnormal wall motion, regional wall thinning or thickening, and dilatation of the LV were considered abnormal for transthoracic echocardiography (TTE) based on JMHW guidelines [22].
99mTc-MIBI imaging analysis
Two nuclear medicine physicians independently evaluated the myocardial perfusion images. In the event of discordant findings, the images were evaluated by a third observer. Myocardial perfusion distribution was assessed based on the American Society of Nuclear Cardiology (ASNC) imaging guidelines [25].
18F-FDG PET or PET/CT imaging analysis
Acquired images were resliced into a series of short-axis, horizontal long-axis and vertical long-axis images, and glucose metabolic activities in the LV myocardium were evaluated. The LV wall was divided into 17 segments based on ASNC imaging guidelines [26]. These segments were subdivided into five regions: anterior (3 segments), interventricular septum (5 segments), inferior (3 segments), lateral wall (5 segments), and apex (1 segment) [26]. Since each region contained a different number of segments, we calculated the percentage of segments in each region with positive 18F-FDG uptake as the total number of positive segments in each region/the total number of segments in each region. Uptake of 18F-FDG in the right ventricle (RV) wall was also evaluated using the same diagnostic criteria as for LV wall 18F-FDG uptake.
Two nuclear medicine physicians independently evaluated the myocardial 18F-FDG images. In the event of discordant findings, the images were evaluated by a third observer. Regional myocardial 18F-FDG uptake was first evaluated visually. Since there are no established criteria for visually positive myocardial 18F-FDG uptake under fasting conditions [16, 23, 27], we applied criteria for focally positive 18F-FDG uptake in PET imaging established for inflammation and oncology [28, 29]. 18F-FDG uptake was defined as positive if it was greater than that for a physiologically normal liver [28, 29]. A scan was defined as positive if focal 18F-FDG uptake was present in at least one segment [27]. In addition, standardized uptake values (SUVs) were used for semiquantitative analysis, but in order to avoid disparities in the results from the two scanners, SUVmax ratios were calculated in relation to the SUVmax in the liver of the same patient. These values were used in the analyses rather than direct comparison of SUVmax among the study population [30]. For the analysis of myocardial accumulation of 18F-FDG, spherical regions of interest for each of the five myocardial segments (apex, anterior, septal, and inferior and lateral wall) were placed to estimate the SUVmax [15].
Regional myocardial 18F-FDG uptakes, measured both visually and using semiquantitative analysis, were compared with ECG findings based on JMHW guidelines [22].
Statistical analysis
Means and standard deviations are provided as descriptive statistics for the data. For intragroup comparisons, the Wilcoxon signed-ranks test was applied to evaluate the difference in the total number of positive 18F-FDG uptake segments between ECG-abnormal and in ECG-normal patients. Fisher’s exact test was used to compare discrete data as appropriate. P values less than 0.05 were considered to represent statistically significant differences.
The Bonferroni correction was used in the assessment of the relationship between regional 18F-FDG uptake and ECG abnormalities. This analysis can be applied when several dependent or independent variables need to be compared. In this analysis, considering a type I error rate for multiple comparisons, p values of less than 0.01 (0.05/5) were considered to represent a statistically significant difference. Statistical calculations were carried out using statistical software (JMP version 9; SAS Institute, Cary, NC, USA).
Results
ECG abnormalities
In 33 patients there was at least one abnormal ECG finding, including RBBB in 15 patients, AV block in 13 patients, nonsustained ventricular tachycardia in 1 patient, PVC (Lown grade >2) in 13 patients, abnormal Q wave in 1 patient, and ST-T abnormalities in 3 patients (Table 3).
Blood sample data
Among 67 patients (50 with focal and 17 with diffuse 18F-FDG uptake), IRI was determined in 63 and FFA in 64. The blood sample volume was insufficient in four patients for the determination of IRI, and in three patients for the determination of FFA. FFA values were significantly increased after UFH administration in all patients both included and excluded (Table 4). No patients had side effects from UFH.
18F-FDG PET or PET/CT findings
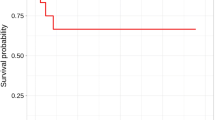
Of the 50 patients, 33 (66 %) showed abnormal 18F-FDG uptake in at least one segment in the LV wall. Focal uptake was frequently seen on the basal anteroseptal wall and lateral wall segments (Fig. 1). Patients who met the diagnostic criteria of the JMHW guidelines showed a higher 18F-FDG uptake frequency than patients who did not meet the diagnostic criteria (p < 0.0001; Table 2). The SUVmax ratio was significantly higher in the visually positive regions than in the visually negative regions (2.29 ± 0.94 vs. 0.83 ± 0.30, p < 0.0001). Patients with abnormal ECG had increased total numbers of segments of the LV wall showing abnormal 18F-FDG uptake compared with patients without ECG abnormalities (3.48 ± 2.73 segments vs. 1.41 ± 2.09 segments, p = 0.0051; Fig. 2). Table 5 summarizes the relationships between 18F-FDG uptake and ECG abnormalities. Among ECG abnormalities, only AV block predicted interventricular septum wall 18F-FDG uptake from both visual analysis (p = 0.0025) and SUVmax ratio using the Bonferroni correction (p = 0.0094; Table 5, Fig. 3). Patients with AV block also had a significantly higher proportion of segments showing abnormal 18F-FDG uptake in the interventricular septum wall (p = 0.0006). There was no significant relationship between the proportion of segments showing abnormal 18F-FDG uptake and the presence of other ECG abnormalities.
Representative findings in a 75-year-old woman. ECG shows complete AV block (a). Maximum intensity projection view of the 18F-FDG PET (b), axial views at cardiac level (c), short-axis view at basal level (d) are presented. 18F-FDG PET shows significant accumulation in interventricular septum wall at basal level. There are multiple lymph nodes showing abnormal uptake in supraclavicular, mediastinum, hilar, abdominal and inguinal regions (b)
In the RV wall analysis, 12 patients (24 %) had abnormal 18F-FDG uptake and a greater number of segments showing abnormal 18F-FDG uptake when compared to patients without RV uptake (p = 0.039). Patients with RV wall uptake showed a greater number of regional LV wall segments with abnormal 18F-FDG uptake than did patients without RV wall uptake (5.33 ± 2.74 vs. 1.97 ± 2.15 segments, p = 0.0002).
18F-FDG and 99mTc-MIBI findings
Of the 50 patients, 45 underwent rest 99mTc-sestamibi myocardial perfusion imaging to assess myocardial perfusion. In 30 patients with positive 18F-FDG uptake, 17 (56.7 %) showed some perfusion abnormalities. Conversely no patient with abnormal perfusion had a negative 18F-FDG uptake in the present study.
Discussion
Sarcoidosis patients with ECG abnormalities showed 18F-FDG uptakes in more regions in the LV wall than patients without ECG abnormalities. Among the ECG abnormalities, only AV block was associated with abnormal interventricular septum and RV wall 18F-FDG uptake. FFA significantly increased after heparin administration in all patients in proportion to the dose given [31]. FFA in excluded patients with diffuse 18F-FDG uptake also increased after heparin administration. Given that these findings agrees with those of previous studies and that these patients responded to heparin, the heparin response might not have been a factor in the diffuse 18F-FDG uptake.
In this study population, 24 patients met the diagnostic criteria of the JMHW. The remaining population had ECG or echocardiographic abnormalities but did not meet the criteria. The JMHW guidelines were issued in 1993 and the main category of diagnostic criteria was advanced pathophysiological conditions. Some have speculated that limiting patient populations to those with these criteria might lead to underestimation of cardiac involvement in patients with sarcoidosis [32]. Our group have reported the case of a patient with sarcoidosis who initially had positive 18F-FDG uptake and later met JMHW diagnostic criteria [14]. Therefore, we have included patients who did not meet these criteria. In fact, 15.4 % of patients (4/26) who did not meet the JMHW criteria showed ECG abnormalities and abnormal 18F-FDG uptake. These four patients showed PVC and ST-T abnormalities, PVC, RBBB, and second-degree AV block, respectively.
18F-FDG PET is used in the diagnosis of cardiac involvement in patients with sarcoidosis [13–17, 33]. In this study, the sensitivity of 18F-FDG PET was 95.8 % in patients who met JMHW criteria. Recently, Ohira et al. [13] and Youssef et al. [27] reviewed previous studies and found that the mean sensitivity of 18F-FDG PET for the diagnosis of cardiac sarcoidosis based on JMHW diagnostic criteria was 91 % with a range of 82 % to 100 %. The sensitivity of 18F-FDG PET reflects that determined by previous studies. In the current study, 56.7 % of regions with positive 18F-FDG uptake showed a perfusion abnormality. These findings might imply that 18F-FDG PET is more sensitive than perfusion imaging, a finding consistent with those of previous studies [13].
In the current study, the proportion of segments showing abnormal 18F-FDG uptake was lower in patients who did not meet the diagnostic criteria of the JMHW. However, our findings showed that there were some patients with 18F-FDG-positive segments in this population. We aimed to evaluate the relationships between ECG abnormalities and regional myocardial 18F-FDG uptake. Therefore, we also included patients who had ECG or echocardiographic abnormalities but who did not meet the diagnostic criteria of cardiac involvement in sarcoidosis based on the JMHW guidelines.
In this study, abnormal 18F-FDG uptake was frequently observed in the basal anteroseptal wall of the LV. Previous studies have shown that patients who die with active cardiac sarcoidosis granulomas frequently have localized masses in the basal portion of the interventricular septum or throughout the myocardium. The current findings agree with previous pathological reports [15, 16, 34–36]. We further showed the relationship between interventricular septum 18F-FDG uptake and ECG abnormalities, especially AV block. First-degree AV block is seen in the elderly and is nonspecific, so we also evaluated eight patients who showed second-degree or third-degree AV block. Almost all of the latter patients (seven of eight) showed more extensive septum wall 18F-FDG uptake than patients without second-degree and third-degree AV block (p = 0.0181).
Abnormal 18F-FDG uptake was seen in the RV in 24 % of patients. Previous studies have shown lower frequencies of involvement in the RV region than in the LV free wall [36, 37]. One small study of patients at autopsy showed that the frequency of involvement of the RV region was about half that of LV regions [38]. The current findings agree with those of the previous studies. Given the small number of patients with RV uptake in the current study, evaluating the clinical impact of RV uptake was difficult. Patients with RV 18F-FDG uptake frequently had ECG abnormalities; however, it was difficult to evaluate the relationship between RV uptake and specific ECG abnormalities given the small number of patients with RV uptake. The clinical impact of RV uptake should be the subject of future study.
Among sarcoidosis patients, cardiac involvement is the leading cause of death associated with conduction system abnormalities. About half of cardiac sarcoidosis patients have ECG abnormalities including rhythm abnormalities and repolarization [39]. ST alteration is known to occur frequently in hypertensive and diabetic patients, indicating interstitial and structural alterations in the myocardium. In this study, there was only one diabetic patient who had complete RBBB [40]. There were no hypertensive patients [41]. Thus, diabetes and hypertension had no impact on the current data. Kim et al. found AV block in 26–62 % of patients with cardiac sarcoidosis. In our study, 33 patients (66 %) showed ECG abnormalities. Among these patients, 13 (26 % of total patients) had AV block. Occurrence rates for each abnormality reflected those in the previous study [39]. Cardiac 18F-FDG uptake appears to be related to ECG abnormalities, a relationship which may represent a mechanistic link between cardiac sarcoidosis and cardiac death. Such a possibility remains to be followed up clinically.
Cardiac sarcoidosis is more common than was previously thought in young to middle-aged adults who have unexplained AV block requiring pacemaker implantation [42]. Kandolin et al. found that cardiac sarcoidosis patients who start immunosuppressive therapy earlier tend to have a reduced requirement for pacing [12]. This finding might imply that some cardiac sarcoidosis patients could avoid pacemaker implantation with early immunosuppressive intervention. Inflammatory regions might be reversible and treatable. 18F-FDG PET may be useful in determining the cause of arrhythmias in diagnosing cardiac sarcoidosis or in finding the causes of unexplained conduction abnormalities in patients. In future, 18F-FDG PET septum uptake may be among the diagnostic options for determining treatment indications in this population, and should be the subject of a future clinical trial. The current findings may indicate that 18F-FDG PET would be useful in managing AV block in patients with sarcoidosis. The uptake of 18F-FDG might also be useful in determining the requirement for device treatment. In this study population, we made clinical decisions based on the ACC/AHA/HRS guidelines [43] because no consensus for this treatment based on 18F-FDG uptake findings has been established. The usefulness of 18F-FDG PET in evaluating the indications for device therapy should be the subject of future clinical trials.
Limitations
The present study had methodological limitations. Of 50 patients, 37 were evaluated using PET and the remaining 13 were evaluated using PET/CT. PET/CT has better spatial resolution than PET. However, we defined as positive an obvious focal uptake that was higher than that of a normal liver, thereby allowing us to accurately detect abnormal regional uptake using PET as has been done in previous studies [15, 23]. Among the 50 patients, 37 fasted for more than 6 h and were given heparin, 6 fasted for more than 12 h and were given heparin, and 7 fasted for more than 18 h and were given a low-carbohydrate diet and heparin. The preparations were different in some patients. However, we evaluated only patients who had a sufficiently low physiological 18F-FDG myocardial uptake. Thus, the different preparations would have had a minimal impact on the 18F-FDG PET findings.
We did not compare focal 18F-FDG uptake and pathology findings. It is difficult to perform endomyocardial biopsies on all regions. However, it is known that myocardial biopsy shows lower sensitivity for the diagnosis of cardiac sarcoidosis [3, 39]. Given the limited sensitivity of myocardial biopsy, the JMHW guidelines have been used as the diagnostic standard [27]. Thus, the lack of myocardial biopsy should not be a major limitation. In the current study, all patients had at least biopsy-proven extracardiac sarcoidosis and we defined cardiac involvement based on the widely accepted JMHW guidelines. We have previously reported that focal 18F-FDG uptake is associated with active inflammation in patients with cardiac sarcoidosis [44]. Thus, focal 18F-FDG uptake might be associated with active sarcoid regions. In the current study, we lacked long-term follow-up data. Long-term follow-up data will be required in the future and their acquisition is currently underway. We included abnormal ECG and TTE findings based solely on the JMHW guidelines. Recently, new TTE findings, such as speckled myocardium, have been reported. In future studies, these findings should be compared with those for abnormal 18F-FDG uptake.
Conclusion
Regional 18F-FDG uptakes was more frequent in patients with sarcoidosis with ECG abnormalities than in patients without ECG abnormalities. Among ECG abnormalities, AV block was associated with interventricular septum 18F-FDG uptake.
References
Iannuzzi MC, Rybicki BA, Teirstein AS. Sarcoidosis. N Engl J Med. 2007;357:2153–65.
Rybicki BA, Major M, Popovich Jr J, Maliarik MJ, Iannuzzi MC. Racial differences in sarcoidosis incidence: a 5-year study in a health maintenance organization. Am J Epidemiol. 1997;145:234–41.
Doughan AR, Williams BR. Cardiac sarcoidosis. Heart. 2006;92:282–8.
Silverman KJ, Hutchins GM, Bulkley BH. Cardiac sarcoid: a clinicopathologic study of 84 unselected patients with systemic sarcoidosis. Circulation. 1978;58:1204–11.
Blankstein R, Naya M, Osborne M, Kim C, Murthy V, Kwong R, et al. Cardiac positron emission tomography enhances prognostic assessments of patients with suspected cardiac sarcoid. J Am Coll Cardiol. 2012;59:E1310.
Mehta D, Lubitz SA, Frankel Z, Wisnivesky JP, Einstein AJ, Goldman M, et al. Cardiac involvement in patients with sarcoidosis: diagnostic and prognostic value of outpatient testing. Chest. 2008;133:1426–35.
Valantine HA, Tazelaar HD, Macoviak J, Mullin AV, Hunt SA, Fowler MB, et al. Cardiac sarcoidosis: response to steroids and transplantation. J Heart Transplant. 1987;6:244–50.
Sugishita K, Togashi Y, Aizawa A, Asakawa M, Usui S, Ito N, et al. Postpartum complete atrioventricular block due to cardiac sarcoidosis: steroid therapy without permanent pacemaker. Int Heart J. 2008;49:377–84.
Takeda N, Yokoyama I, Hiroi Y, Sakata M, Harada T, Nakamura F, et al. Positron emission tomography predicted recovery of complete A-V nodal dysfunction in a patient with cardiac sarcoidosis. Circulation. 2002;105:1144–5.
Miyazaki S, Funabashi N, Nagai T, Uehara M, Kataoka A, Takaoka H, et al. Cardiac sarcoidosis complicated with atrioventricular block and wall thinning, edema and fibrosis in left ventricle: confirmed recovery to normal sinus rhythm and visualization of edema improvement by administration of predonisolone. Int J Cardiol. 2011;150:e4–10.
Dubrey SW, Falk RH. Diagnosis and management of cardiac sarcoidosis. Prog Cardiovasc Dis. 2010;52:336–46.
Kandolin R, Lehtonen J, Kupari M. Cardiac sarcoidosis and giant cell myocarditis as causes of atrioventricular block in young and middle-aged adults. Circ Arrhythmia Electrophysiol. 2011;4:303–9.
Ohira H, Tsujino I, Yoshinaga K. 18F-Fluoro-2-deoxyglucose positron emission tomography in cardiac sarcoidosis. Eur J Nucl Med Mol Imaging. 2011;38:1773–83.
Ohira H, Tsujino I, Sato T, Yoshinaga K, Manabe O, Oyama N, et al. Early detection of cardiac sarcoid lesions with 18F-fluoro-2-deoxyglucose positron emission tomography. Intern Med. 2011;50:1207–9.
Okumura W, Iwasaki T, Toyama T, Iso T, Arai M, Oriuchi N, et al. Usefulness of fasting 18F-FDG PET in identification of cardiac sarcoidosis. J Nucl Med. 2004;45:1989–98.
Yamagishi H, Shirai N, Takagi M, Yoshiyama M, Akioka K, Takeuchi K, et al. Identification of cardiac sarcoidosis with (13)N-NH(3)/(18)F-FDG PET. J Nucl Med. 2003;44:1030–6.
Manabe O, Oyama-Manabe N, Ohira H, Tsutsui H, Tamaki N. Multimodality evaluation of cardiac sarcoidosis. J Nucl Cardiol. 2012;19:621–4.
Bengel FM, Higuchi T, Javadi MS, Lautamaki R. Cardiac positron emission tomography. J Am Coll Cardiol. 2009;54:1–15.
Prior JO. Diabetes and vascular (18)f-fluorodeoxyglucose positron emission tomography uptake: another step toward understanding inflammation in atherosclerosis. J Am Coll Cardiol. 2012;59:2089–90.
Schindler TH, Schelbert HR, Quercioli A, Dilsizian V. Cardiac PET imaging for the detection and monitoring of coronary artery disease and microvascular health. JACC Cardiovasc Imaging. 2010;3:623–40.
Gyorik S, Ceriani L, Menafoglio A, Gallino A, Wyttenbach R. F-FDG PET scan as follow-up tool for sarcoidosis with symptomatic cardiac conduction disturbances requiring a pacemaker. BMJ Case Rep. 2009;2009:bcr2006070805.
Hiraga H, Hiroe M, Iwai K. Guidelines for diagnosis of cardiac sarcoidosis: study report on diffuse pulmonary diseases (in Japanese). Tokyo: The Japanese Ministry of Health and Welfare; 1993. p. 2.
Ishimaru S, Tsujino I, Takei T, Tsukamoto E, Sakaue S, Kamigaki M, et al. Focal uptake on 18F-fluoro-2-deoxyglucose positron emission tomography images indicates cardiac involvement of sarcoidosis. Eur Heart J. 2005;26:1538–43.
Ohira H, Tsujino I, Ishimaru S, Oyama N, Takei T, Tsukamoto E, et al. Myocardial imaging with 18F-fluoro-2-deoxyglucose positron emission tomography and magnetic resonance imaging in sarcoidosis. Eur J Nucl Med Mol Imaging. 2008;35:933–41.
American Society of Nuclear Cardiology. Updated imaging guidelines for nuclear cardiology procedures, part 1. J Nucl Cardiol. 2001;8:G5–G58.
Machac J, Bacharach SL, Bateman TM, Bax JJ, Beanlands R, Bengel F, et al. Positron emission tomography myocardial perfusion and glucose metabolism imaging. J Nucl Cardiol. 2006;13:e121–51.
Youssef G, Leung E, Mylonas I, Nery P, Williams K, Wisenberg G, et al. The use of 18F-FDG PET in the diagnosis of cardiac sarcoidosis: a systematic review and metaanalysis including the Ontario experience. J Nucl Med. 2012;53:241–8.
Laffon E, Adhoute X, de Clermont H, Marthan R. Is liver SUV stable over time in 18F-FDG PET imaging? J Nucl Med Technol. 2011;39:258–63.
Paquet N, Albert A, Foidart J, Hustinx R. Within-patient variability of (18)F-FDG: standardized uptake values in normal tissues. J Nucl Med. 2004;45:784–8.
Das CJ, Makharia GK, Kumar R, Tiwari RP, Sharma R, Malhotra A. PET/CT colonography: a novel non-invasive technique for assessment of extent and activity of ulcerative colitis. Eur J Nucl Med Mol Imaging. 2010;37:714–21.
Asmal AC, Leary WP, Thandroyen F, Botha J, Wattrus S. A dose–response study of the anticoagulant and lipolytic activities of heparin in normal subjects. Br J Clin Pharmacol. 1979;7:531–3.
Patel MR, Cawley PJ, Heitner JF, Klem I, Parker MA, Jaroudi WA, et al. Detection of myocardial damage in patients with sarcoidosis. Circulation. 2009;120:1969–77.
Tahara N, Tahara A, Nitta Y, Kodama N, Mizoguchi M, Kaida H, et al. Heterogeneous myocardial FDG uptake and the disease activity in cardiac sarcoidosis. JACC Cardiovasc Imaging. 2010;3:1219–28.
Ghosh P, Fleming HA, Gresham GA, Stovin PG. Myocardial sarcoidosis. Br Heart J. 1972;34:769–73.
Lie JT, Hunt D, Valentine PA. Sudden death from cardiac sarcoidosis with involvement of conduction system. Am J Med Sci. 1974;267:123–8.
Roberts WC, McAllister Jr HA, Ferrans VJ. Sarcoidosis of the heart. A clinicopathologic study of 35 necropsy patients (group 1) and review of 78 previously described necropsy patients (group 11). Am J Med. 1977;63:86–108.
Habersberger J, Manins V, Taylor AJ. Cardiac sarcoidosis. Intern Med J. 2008;38:270–7.
Nelson JE, Kirschner PA, Teirstein AS. Sarcoidosis presenting as heart disease. Sarcoidosis Vasculitis Diffuse Lung Dis. 1996;13:178–82.
Kim JS, Judson MA, Donnino R, Gold M, Cooper Jr LT, Prystowsky EN, et al. Cardiac sarcoidosis. Am Heart J. 2009;157:9–21.
American Diabetes Association. Diagnosis and classification of diabetes mellitus. Diabetes Care. 2010. 33 Suppl 1:S62–69.
Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo Jr JL, et al. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: the JNC 7 report. JAMA. 2003;289:2560–72.
Youssef G, Beanlands RS, Birnie DH, Nery PB. Cardiac sarcoidosis: applications of imaging in diagnosis and directing treatment. Heart. 2011;97:2078–87.
Epstein AE, DiMarco JP, Ellenbogen KA, Estes 3rd NA, Freedman RA, Gettes LS, et al. ACC/AHA/HRS 2008 Guidelines for Device-Based Therapy of Cardiac Rhythm Abnormalities: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Revise the ACC/AHA/NASPE 2002 Guideline Update for Implantation of Cardiac Pacemakers and Antiarrhythmia Devices): developed in collaboration with the American Association for Thoracic Surgery and Society of Thoracic Surgeons. Circulation. 2008;117:e350–408.
Koiwa H, Tsujino I, Ohira H, Yoshinaga K, Otsuka N, Nishimura M. Images in cardiovascular medicine: imaging of cardiac sarcoid lesions using fasting cardiac 18F-fluorodeoxyglucose positron emission tomography: an autopsy case. Circulation. 2010;122:535–6.
Acknowledgments
The authors thank Keiichi Magota, PhD, Hidehiko Omote, RT, Ken-ichi Nishijima, PhD, Daiske Abo, MSc, Kumi Ajiki, and Eriko Suzuki for their support during this study.
This study was supported in part by grants from the Ministry of Education, Science and Culture Japan (Category B, no. 23390294; Category Young Investigator, no. 23790826), the Hokkaido Heart Association for Research (H-23) (Sapporo, Japan), the Adult Vascular Disease Research Foundation (#H22-23) (Kyoto, Japan), and the North-Tech Research Foundation (#H23-S2-17, Sapporo, Japan). Dr.Yoshinaga is supported by an Imura Clinical Research Award (Adult Vascular Disease Research Foundation).
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Additional information
Clinical trial registration: UMIN000006533
Rights and permissions
About this article
Cite this article
Manabe, O., Ohira, H., Yoshinaga, K. et al. Elevated 18F-fluorodeoxyglucose uptake in the interventricular septum is associated with atrioventricular block in patients with suspected cardiac involvement sarcoidosis. Eur J Nucl Med Mol Imaging 40, 1558–1566 (2013). https://doi.org/10.1007/s00259-013-2460-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00259-013-2460-5