Abstract
Due to poor correlation between slice thickness and orientation, verification of medical imaging results by histology is difficult. Often validation of imaging findings of lesions suspicious for prostate cancer is driven by a subjective, visual approach to correlate in vivo images with histopathology. We describe fallacious assumptions in the correlation of imaging findings with pathology and identify the lack of accurate registration as a major obstacle in the validation of PET and PET/CT imaging in primary prostate cancer. Specific registration techniques that facilitate the most difficult part of the registration process—the mapping of pathology onto high-resolution imaging, preferably aided by the ex vivo prostate specimen—are discussed.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The American Cancer Society estimated that in 2012 about 241,740 men were newly diagnosed with prostate cancer in the U.S. [1]. Due to prostate-specific antigen screening and more frequent prostate biopsies, a significant stage and grade migration has occurred. As a result, many newly diagnosed prostate cancers are clinically insignificant (indolent) tumors. The identification of such disease poses the tremendous clinical, financial and ethical dilemma of possible overtreatment [2]. On the other hand, roughly 28,170 men died of prostate cancer in the U.S. in 2012 [1], indicating that the risk of prostate cancer-related death remains a great concern. Accordingly, there is considerable uncertainty as to the “best” course of prostate cancer management, one that will significantly reduce morbidity and mortality resulting from tumor progression, yet avoid significant therapeutic side effects and costs related to overtreatment.
From a clinician’s perspective the most important imaging task in the primary setting is not necessarily the identification of prostate cancer itself, but accurate staging and the ability to predict the presence of clinically significant (or relevant) disease. Given currently accepted criteria for local significant disease (Gleason score >6, extraprostatic extension, seminal vesicle and nodal disease involvement, tumor volume >0.5 ml [3, 4]), the identification of significant disease at an early stage is challenging for anatomic, functional and metabolic imaging alike. In addition as highlighted in this article, assessing the accuracy of imaging in identifying prostate cancer is difficult in itself, especially when considering the multifocality of primary prostate cancer [5]. As a result, there is considerable uncertainty about the performance of imaging in the setting of primary prostate cancer, particularly PET and PET/CT.
A recent review of 17 studies in over 500 patients showed the usefulness of 18F-choline and 11C-choline for the diagnosis of primary prostate cancer [6]. Reported sensitivities and specificities for prostate cancer detection varied widely (sensitivity range 66–100 %, specificity range 43–86 %). Most studies used absolute uptake measures (SUV, SUVmax) in characterizing disease. Other studies investigating tumor-to-background ratios have shown that normalization of tumor uptake may improve the likelihood of correct disease classification [7–9]. However, normalization may be a source of additional bias. Moreover, the assessment of efficacy requires a comparison of imaging findings with pathology as the gold standard. We examine here the current standard practice and emerging methods for comparing imaging findings obtained from the prostate gland with pathology.
Current standard practice
When examining methods for comparing PET imaging results with histological findings, there are four approaches of increasing complexity in the medical imaging literature:
-
1.
Lesion-based comparison of radiotracer uptake findings for each prostate lobe.
-
2.
Sector-based (also called template-based) approach for which the prostate is divided into specific sectors on imaging and pathology.
-
3.
Visual comparison of the entire three-dimensional (3-D) prostate volume with multiple discrete 2-dimensonal (2-D) slices, which requires whole-mount sectioning of prostatectomy specimen.
-
4.
Direct registration (or mapping) of the 3-D prostate imaging volume with stacked 2-D whole-mount histological slices stained with hematoxylin-eosin (HE).
The first approach simply assumes that any focally abnormal uptake on the PET image represents malignancy, and that the identified focus represents disease identified on pathology in the same lobe. Due to the lack of sufficient spatial information on pathology, this precludes the ability to assess the performance of a given imaging test unless the cancer involves the entire prostate lobe.
The second approach uses a sector-based comparison of PET imaging results with pathology by dividing the prostate volume into six (sextant) or more (usually 12) sectors taking into account anatomical regions (such as the apex, mid, base, peripheral and central/transitional zones). This method is current standard practice and is commonly applied for comparisons of pathology with imaging. The method mimics the pathologist’s approach for a systematic evaluation from both biopsies and prostatectomy specimens. For this comparison of imaging with pathology, a number of assumptions are made that are considered invalid.
Combining the sector-based analysis with whole-mount histology of the prostate specimen (third approach) improves spatial information content on pathology and improves comparability [10]. This approach, however, still has severe limitations as the classification into specific regions may be arbitrary due to an intrinsic lack of anatomical features (landmarks) that would clearly separate these zones, which is particularly true for low-resolution (PET) and low-contrast (CT) imaging. In addition, any deformations of the prostate specimen due to fixation and sectioning are not taken into account.
Furthermore, imaging studies that derive their pathological correlate from prostate biopsies are limited due to the inherent uncertainty of the biopsy location, even when using template-based biopsies. Also due to significant sampling errors, Gleason grades obtained from prostate biopsies may over- or underestimate the true Gleason grade obtained from a prostatectomy specimen [11], limiting the ability to accurately assess Gleason grading capabilities of in vivo imaging.
In this review, we examine the registration process and review recent progress in techniques for registering in vivo image volumes (MRI, PET) with multiple whole-mounted radical prostatectomy specimens (fourth approach).
Examination of fallacious assumptions for registration
We discuss here fallacious assumptions that have compromised the registration accuracy of histology and in vivo imaging modality combinations in many prior studies. All these assumptions ultimately result from assuming that the registration or mapping problem in this context is fundamentally less than a fully 3-D problem, i.e. 3-D histology “mapped” (alternatively “registered”) to 3-D medical imaging (3-D ↔ 3-D). Assuming that the registration of just the outer 2-D manifolds (3-D organ surfaces) between differing modalities such as histology and in vivo imaging accurately matches internal structures is fallacious. An associated 2-D corollary, i.e. assuming registration of 2-D internal structures of multimodality slices from 1-D manifolds (outer perimeters) is equally erroneous.
Finding correct outline correspondences requires more than implementing arbitrary and biased user assumptions of matching outline segments, such as overlaying evenly arc-segmented radial lines on both datasets each centered at some arbitrary point and forcing so-called “homologous” points that intersect at the outlines to be registered. Matching outlines involves finding truly matching tangential homologous line segments along the outlines, not just 2-D points which define a point-to-point homology with no regard to local tangents. Even so, the warping of the interior is not defined by matching points on the outline. Matching the outlines and expecting the rest of the registration to be correct requires that all deformations are proportionately radial about some unknown center point, clearly something that rarely exists in nature, if at all. Accurate internal registration by matching outlines would require the use of a 2-D finite element model (FEM) which assumes prior segmentation knowledge of the slice’s internal features and each segment’s elastic properties. But if the loci of such parameters were known, it would be possible to register them by geometric methods without using a FEM in the first place. However, neither option is typically feasible due to the missing joint spatial and elasticity information for FEM segments. Likewise, registration of just the outer 3-D surface shell (2-D manifold) cannot correct local volumetric deformations such as local nonzero divergences and curls that may occur within tissues due to fixation-related changes. Even if the outer 3-D shells were registered, the registration error would generally increase with distance inward away from the registered outer shell.
Prostate deformation
Assuming that a 3-D ex vivo radical prostatectomy specimen that has been formalin-fixed for histology sectioning has the same 3-D geometry as the 3-D in vivo medical images, such that the two can be registered at most by a simple 3-D rotate, translate, and isotropic scaling transformation is also fallacious. An associated, fallacious 2-D corollary assumes that a slice in 3-D in vivo imaging can be found, possibly by reformation of the 3-D medical imaging data, that matches a slice of histology such that the 2-D histology slice only needs a 2-D transformation to map its geometry onto the 2-D geometry of the corresponding “found” in vivo slice.
As can be expected, the in vivo configuration of the prostate will change with bladder and rectal filling. In addition, depending on technique, the use of a balloon for endorectal coil MRI can significantly change the configuration of the prostate gland. The mechanical deformation of the in vivo specimen in the process of surgical extraction alone is sufficient to understand the fallacy of the assumption. Surgical extraction of the prostate begins with transecting periprostatic tissues including vessels, urethra and bladder, resulting in significant deformation of the prostate. The surgeon uses manual or robotic probing to tear the prostate away from the supporting surrounding tissue, and finally the prostate is firmly grasped and extracted from the body cavity. At this point the geometry of the prostate is already altered far beyond a rigid body deformation due to the vascular and urethral pressure collapse, manual compression and tissue destruction. Orczyk et al. calculated an average 10 % loss in volume due to surgical resection alone as measured by in vivo and ex vivo MRI [12]. Further the dehydration of a tissue sample during formalin fixation yields differential shrinkage of internal tissue components (fat, muscle, collagen, calcifications, etc.) due to their initial differential water hydration states [13, 14].
While the previous paragraph describes 3-D deformations to the intact prostate, recall that preparation of 2-D histology slices requires the mechanical cutting of the fixed tissue volume into 2-D slices with a microtome, mounting the slice on a glass slide and staining the tissue. If a frozen sample is cut with a cryomicrotome, the result is referred to as the “butter” transform, where the cryostat is set at a temperature to keep the tissue sample sufficiently solid to cut nearly parallel slices without breaking the blade. If instead the sample is cut into slices after formalin fixation followed by paraffin embedding, the sample is still non-uniformly deformed due to the differential tensile strengths of the structures cut [13]. While torn slices are usually discarded, such slides may still be selected for the study because of the pathology they uniquely represent. The presence of these often random effects strongly suggests that it is important to map/register each 2-D slice back onto the geometry of the (frozen or paraffin-fixed) tissue block before it was microtomed, which can be captured in a picture taken of the block face ideally just before the section is cut (or even afterwards if the sections are very thin and thus very similar). Otherwise the alternative is to try to compensate for all of these random, fundamentally 2-D deformations after the slices have been bound into a volume where no geometrical truth exists. While several published papers justify ignoring these 2-D tasks while citing the need for laboriously assigning manually chosen point correspondences on each of the slices, it is the case that automatic registration algorithms possessing sufficiently large capture ranges can be successful with little or no manual intervention [15]. If torn tissue slides are discarded, their location needs to be preserved with null, nonregistration biasing entries so as to maintain the relatively correct spacing of the stack of histology slices to limit the required degrees of freedom (DOF) of the next registration step.
Prostatic motion
Assuming that in vivo acquisition motion artifacts can be safely ignored is problematic when performing MRI and PET due to extended volume collection durations. CT acquisitions in late generation machines are now sufficiently fast that motion artifacts can be avoided, but the same is not true for MRI and PET. It is worth noting that maximal cranial-caudal motion of an adult prostate has been measured at about 1 cm between full inspiration and full expiration [16–18]. However, under normal breathing conditions in a comfortable supine position, respiratory motion of the prostate appears to be less than 4 mm [19]. Immobilization in thermoplastic shells (for radiation treatment) may increase prostate motion synchronously with respiration, rather than prevent it [18]. These findings suggest that respiratory-gated PET acquisitions in list mode may provide better prostate registration with other modalities. However, preventing patient motion by optimizing patient comfort during imaging is most relevant. This is particularly true for endorectal coil MRI, as rectal and pelvic muscular contractions can significantly alter the position of the prostate [17].
Advances in registration techniques
Specialized registration techniques are needed to facilitate the registration of histology onto in vivo imaging. Histology information content is multiple levels of scale higher than that of MRI, which is typically the in vivo imaging modality obtained with the greatest contrast resolution to discern intraprostatic anatomy. Therefore, the limiting factor for registration accuracy is primarily the local information content of the in vivo imaging, independent of modality. CT has high spatiotemporal resolution but poor soft-tissue contrast resolution; thus the information content of its resulting imaging volume for soft tissues is limited primarily by the radiation dose and attenuation characteristics of the image volume. MRI has high intrinsic soft-tissue contrast resolution, but lesser spatiotemporal resolution, which can reduce the contrast resolution achieved due to tissue motion during acquisition. The soft-tissue contrast resolution of PET is dependent on the achievable target-to-background contrast of the selected tracer, but its spatiotemporal resolution is generally much worse than that of CT or MRI. Thus, in general we assume for imaging stationary soft tissue the following ordering of image volume information content (I) from each of the imaging modalities, i.e. I Histology » I MRI > I CT > I PET, where the ordering of the average information content of in vivo imaging modalities may be altered under different imaging conditions than those described above.
By combining appropriate modality parings, it is possible to match the needed DOF of warping with the appropriate mutual information (MI) content to improve the overall registration accuracy between histology and in vivo imaging. For example, when high DOF warping is needed for registration, appropriate modality pairings are required whose MI supports such DOF. A one-step registration performed by mapping an accurately formed histology volume to the in vivo MRI volume, which requires a large DOF due to the large bending energy differences between the two datasets, is not supported by the MI of the combination, specifically due the low information content of the in vivo MRI. Thus the use of intermediate stages of high information content imaging is required to provide support for the needed DOF necessary to ultimately map the two datasets. For example a high-resolution block face photo taken just before the slice of interest is cut with the microtome will provide sufficient information for the resulting histology slice to be deformed back into its en bloc geometry [20]. Note that the largely random 2-D deformations (including tearing) that occur during microtoming the tissue block cannot be corrected later by 3-D deformations unless the deformations persist systematically across many slices, i.e. are truly correlated in 3-D (which is extremely unlikely). Finally, it is clear that inclusion of more whole-mount sections/slices in the representation of the histology volume is beneficial due to the increased information content of the resulting histology volume. While pathologists typically sample and annotate between five and seven sections (each section is usually 0.4–0.5 cm in thickness) for clinical diagnosis, the inclusion of additional non-annotated slices will improve the following joint volumetric registration tasks.
The resulting stack of 2-D geometry-corrected histology slices, which represents a sampling of the prostatic volume en bloc, can be more accurately mapped to its in vivo geometry through the use of higher DOF warping. This can be achieved by first mapping the en bloc geometry to its ex vivo state as acquired by motionless, thin-slice, multiple signal-averaged anatomical T2-weighted MRI imaging begun immediately after the prostate is surgically removed. This imaging should be performed while the prostate specimen is supported ideally in a neutrally buoyant, formalin-containing solution so as to prevent further deformation of the ex vivo organ from its in vivo geometry [20]. If ex vivo imaging begins immediately after the fresh prostate specimen is placed in formalin, then only the surface of the prostate will be fixed within in the first hour, and the remainder of the prostate will not be crosslinked. If this is not possible (as in Fig. 1), then the imaging protocol must be changed to accommodate the imaging of the fixed prostate using a proton density weighted acquisition (long TR/short TE of 1,000–2,000/20–30 ms) at higher field strengths, i.e. 7 T. Either way the signal-to-noise ratio (SNR) and therefore the information content of the ex vivo, thin-slice MRI acquisition can be made far higher than that of the in vivo anatomical MRI due to repeated signal averaging supported by motionless imaging where the averaging time for the fixed specimen is on the order of eight to ten times that of the unfixed specimen [21].
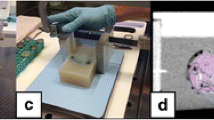
Registration process. a–c Formalin-fixed specimen (a) undergoes ex vivo MRI (b) in a custom-made prostate mold (c). d Gross sectioning is done in identical position at evenly spaced distances. e Tissue block face photos are obtained from these 3-mm sections. f After HE staining, the pathologist outlines prostate cancer lesions (blue dots) on whole-mount HE slices. g To demonstrate the process, the T2-weighted specimen MRI (TE 325 ms, TR 1,733 ms) volume obtained at a slice thickness of 0.15 mm is registered to a single 2-D HE slice. h The fusion image (50 % MRI and 50 % HE) demonstrates excellent registration between pathology and ex vivo MRI
The last step of mapping the histology volume now deformed to approximately the same geometry as the ex vivo prostate back to its in vivo geometry will only support low DOF due to the low SNR of the in vivo image. Warping methodologies that only support high DOF must choose appropriate penalty terms to penalize for higher local bending energies and/or are applied at sufficiently low spatial scales such that the resulting local bending energies are limited to prevent folding singularities in the resulting deformation.
The registration method described by Park et al. [20] allows registration without the use of extrinsic fiducial markers or unsubstantiated assumptions regarding geometric relationships between in vivo and ex vivo image sets and has been applied successfully in several clinical studies [8, 22–24]. The method, however, suffers from uncertainties related to variable geometry (slice thickness) of individual gross specimen sections regarding their location in the ex vivo specimen MRI.
To overcome this limitation, various dedicated sectioning devices have been developed that allow gross sectioning in defined fixed intervals and orientation [25, 26]. With the introduction of rapid prototyping technology, further improvements utilizing custom-made molds for the prostate specimen are now feasible [12, 25, 27–29]. Rapid prototyping allows conversion of a computer-generated 3-D model into a physical model. Acrylonitrile butadiene styrene plastics are common materials that can be used to print molds capable of holding the specimen in a defined position and shape for ex vivo imaging and gross sectioning. The mold is usually created on the basis of a 3-D representation of the prostate from in vivo high-resolution anatomical MRI [27, 28]. The design requires segmentation of the prostate surface and is usually performed on a stereo lithography computer-aided design (CAD) workstation. An advantage of this technique is that the mold can be manufactured prior to prostatectomy, with evenly spaced slits encouraging nearly parallel gross sectioning in a predefined orientation and direction [28]. In addition, the technique can be applied to sectioning of fresh (nonfixed) prostate specimens. Nevertheless, due to the differential compression of the ex vivo prostate during gross sectioning, the resulting sections have neither planar nor coplanar faces. Thus the exclusive use of such devices without additional nonlinear (warping) registration will not yield adequate results because the in vivo MRI and ex vivo sectioned 2-D manifold (identified as such because their shape may look more like that of a thick potato chip) still do not match, and only the appropriate use of nonlinear registration can account for the above-mentioned prostate deformations.
Additional ex vivo MRI of the prostate specimen has several advantages. First, image data can be acquired from a nonmoving object in exquisite resolution. Second, such image data allow independent verification of in vivo imaging features. Using this approach, Fan et al. were able to demonstrate that ex vivo MR imaging of the excised prostate specimen with a high-field-strength magnet (9.4 T) can have similarities to in vivo endorectal coil MR imaging at 1.5 T in both the peripheral and central zone, but their series comprised only nine prostates and they did not assess changes in image contrast which can occur within the prostate related to dehydration and/or fixation following prostatectomy [29]. Figure 1 displays the process of registration of ex vivo T2-weighted MRI of a prostatectomy specimen obtained at 3 T onto the whole mount pathology. Mold design was based on in vivo MRI. Figure 2 is a schematic of the entire registration process.
Once registration (mapping) of the in vivo 3-D MRI volume with a stack of warped 2-D histopathology slices is achieved, image information about any part of the gland—such as foci of cancer, benign hyperplastic nodules, or inflammation—can be transferred across all in vivo modalities, thus providing researchers with valuable spatial information about the significance of imaging features. Previously, we reported registration errors between pathology and in vivo MRI using MI registration techniques and ex vivo MRI (but without the use of custom molds) in the range 2.3–3.7 mm [20].
Many iterative and semiautomatic deformable registration algorithms have been developed to facilitate the comparison of imaging and histology, but credible estimates for registration errors for many methods have not been published. Since these methods do not rely on the intermediate data provided by ex vivo imaging, they appear to possess incomplete information to drive all the necessary deformations for accurate registration. However, with sufficient image information provided by both ex vivo and in vivo imaging, and volumetric histopathology, automated registration techniques can reduce the laborious and time-consuming registration task, and can improve the accuracy and applicability of registration techniques [30] in mapping histopathology back onto in vivo imaging.
Conclusion
The ability to unequivocally link specific in vivo prostate cancer imaging features to pathology is of great importance. This is especially true as clinical trials investigating the performance of imaging in primary prostate cancer are time-consuming and costly. The additional expenses related to advanced techniques for registration of in vivo imaging and pathology which require ex vivo imaging of the prostate specimen and possibly custom mold production are small in comparison to the overall costs of clinical trials. Employing advanced registration techniques will improve the impact of such research. One can also speculate that the total number of subjects needed to assess efficacy of imaging in primary prostate cancer could be reduced as a result of decreased bias and measurement errors. Employing advanced registration techniques may well be cost effective and is recommended for research applications. This is particularly true for primary prostate cancer, which often presents with multifocal disease of varying clinical significance.
References
American Cancer Society. Cancer facts and figures 2012. Atlanta: American Cancer Society; 2012
Bill-Axelson A, Holmberg L, Filen F, Ruutu M, Garmo H, Busch C, et al. Radical prostatectomy versus watchful waiting in localized prostate cancer: the Scandinavian prostate cancer group-4 randomized trial. J Natl Cancer Inst. 2008;100:1144–54.
Epstein JI, Chan DW, Sokoll LJ, Walsh PC, Cox JL, Rittenhouse H, et al. Nonpalpable stage T1c prostate cancer: prediction of insignificant disease using free/total prostate specific antigen levels and needle biopsy findings. J Urol. 1998;160:2407–11.
Epstein JI, Walsh PC, Carmichael M, Brendler CB. Pathologic and clinical findings to predict tumor extent of nonpalpable (stage T1c) prostate cancer. JAMA. 1994;271:368–74.
Karavitakis M, Ahmed HU, Abel PD, Hazell S, Winkler MH. Tumor focality in prostate cancer: implications for focal therapy. Nat Rev Clin Oncol. 2011;8:48–55.
Farsad M, Schwarzenbock S, Krause BJ. PET/CT and choline: diagnosis and staging. Q J Nucl Med Mol Imaging. 2012;56:343–53.
Li X, Liu Q, Wang M, Jin X, Yao S, Liu S, et al. C-11 choline PET/CT imaging for differentiating malignant from benign prostate lesions. Clin Nucl Med. 2008;33:671–6.
Piert M, Park H, Khan A, Siddiqui J, Hussain H, Chenevert T, et al. Detection of aggressive primary prostate cancer with 11C-choline PET/CT using multimodality fusion techniques. J Nucl Med. 2009;50:1585–93.
Chen J, Zhao Y, Li X, Sun P, Wang M, Wang R, et al. Imaging primary prostate cancer with 11C-choline PET/CT: relation to tumour stage, Gleason score and biomarkers of biologic aggressiveness. Radiol Oncol. 2012;46:179–88.
Mena E, Turkbey B, Mani H, Adler S, Valera VA, Bernardo M, et al. 11C-Acetate PET/CT in localized prostate cancer: a study with MRI and histopathologic correlation. J Nucl Med. 2012;53:538–45.
Cohen MS, Hanley RS, Kurteva T, Ruthazer R, Silverman ML, Sorcini A, et al. Comparing the Gleason prostate biopsy and Gleason prostatectomy grading system: the Lahey Clinic Medical Center experience and an international meta-analysis. Eur Urol. 2008;54:371–81.
Orczyk C, Mikheev A, Rosenkrantz A, Melamed J, Taneja SS, Rusinek H. Imaging of prostate cancer: A platform for 3D co-registration of in-vivo MRI ex-vivo MRI and pathology. Proc SPIE. 2012;8316:83162M
Jonmarker S, Valdman A, Lindberg A, Hellstrom M, Egevad L. Tissue shrinkage after fixation with formalin injection of prostatectomy specimens. Virchows Arch. 2006;449:297–301.
Schned AR, Wheeler KJ, Hodorowski CA, Heaney JA, Ernstoff MS, Amdur RJ, et al. Tissue-shrinkage correction factor in the calculation of prostate cancer volume. Am J Surg Pathol. 1996;20:1501–6.
Kim B, Boes JL, Frey KA, Meyer CR. Mutual information for automated unwarping of rat brain autoradiographs. Neuroimage. 1997;5:31–40.
Balter JM, Sandler HM, Lam K, Bree RL, Lichter AS, Ten Haken RK. Measurement of prostate movement over the course of routine radiotherapy using implanted markers. Int J Radiat Oncol Biol Phys. 1995;31:113–8.
Dinkel J, Thieke C, Plathow C, Zamecnik P, Prum H, Huber PE, et al. Respiratory-induced prostate motion: characterization and quantification in dynamic MRI. Strahlenther Onkol. 2011;187:426–32.
Malone S, Crook JM, Kendal WS, Szanto J. Respiratory-induced prostate motion: quantification and characterization. Int J Radiat Oncol Biol Phys. 2000;48:105–9.
Udrescu C, Jalade P, de Bari B, Michel-Amadry G, Chapet O. Evaluation of the respiratory prostate motion with four-dimensional computed tomography scan acquisitions using three implanted markers. Radiother Oncol. 2012;103:266–9.
Park H, Piert MR, Khan A, Shah R, Hussain H, Siddiqui J, et al. Registration methodology for histological sections and in vivo imaging of human prostate. Acad Radiol. 2008;15:1027–39.
Zachariah CR, Pitt D, Wassenar P, Clymer BD, Abduljalil AM, Knopp MV, et al. Quantification of formalin-fixed MS brain tissue parameters T1, T2*, PD and phase at 7T and comparison with histopathology. Proceedings of the Annual Meeting of the International Society for Magnetic Resonance in Medicine; 2010 May 1–7; Stockholm, Sweden. Berkeley: International Society for Magnetic Resonance in Medicine; 2010. p. 2073.
Park H, Meyer CR, Wood D, Khan A, Shah R, Hussain H, et al. Validation of automatic target volume definition as demonstrated for 11C-choline PET/CT of human prostate cancer using multi-modality fusion techniques. Acad Radiol. 2010;17:614–23.
Park H, Wood D, Hussain H, Meyer CR, Shah RB, Johnson TD, et al. Introducing Parametric Fusion PET/MRI of Primary Prostate Cancer. J Nucl Med Mol Imaging. 2012;53:546–51.
Garcia-Parra R, Wood D, Shah R, Siddiqui J, Hussain H, Park H, et al. Investigation on tumor hypoxia in resectable primary prostate cancer as demonstrated by 18F-FAZA PET/CT utilizing multimodality fusion techniques. Eur J Nucl Med Mol Imaging. 2011;38:1816–23.
Drew B, Jones EC, Reinsberg S, Yung AC, Goldenberg SL, Kozlowski P. Device for sectioning prostatectomy specimens to facilitate comparison between histology and in vivo MRI. J Magn Reson Imaging. 2010;32:992–6.
Chen LH, Ho H, Lazaro R, Thng CH, Yuen J, Ng WS, et al. Optimum slicing of radical prostatectomy specimens for correlation between histopathology and medical images. Int J Comput Assist Radiol Surg. 2010;5:471–87.
Shah V, Pohida T, Turkbey B, Mani H, Merino M, Pinto PA, et al. A method for correlating in vivo prostate magnetic resonance imaging and histopathology using individualized magnetic resonance-based molds. Rev Sci Instrum. 2009;80:104301.
Trivedi H, Turkbey B, Rastinehad AR, Benjamin CJ, Bernardo M, Pohida T, et al. Use of patient-specific MRI-based prostate mold for validation of multiparametric MRI in localization of prostate cancer. Urology. 2012;79:233–9.
Fan X, Haney CR, Agrawal G, Pelizzari CA, Antic T, Eggener SE, et al. High-resolution MRI of excised human prostate specimens acquired with 9.4T in detection and identification of cancers: validation of a technique. J Magn Reson Imaging. 2011;34:956–61.
Meyer CR, Wahl RL. Image fusion. In: Wahl RL, editor. Principle and practices of PET and PET/CT. 2nd ed. Philadelphia: Williams and Wilkins; 2009. p. 111–6.
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Meyer, C., Ma, B., Kunju, L.P. et al. Challenges in accurate registration of 3-D medical imaging and histopathology in primary prostate cancer. Eur J Nucl Med Mol Imaging 40 (Suppl 1), 72–78 (2013). https://doi.org/10.1007/s00259-013-2382-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00259-013-2382-2