Abstract
Prosthetic joint replacement surgery is performed with increasing frequency. Overall the incidence of prosthetic joint infection (PJI) and subsequently prosthesis revision failure is estimated to be between 1 and 3%. Differentiating infection from aseptic mechanical loosening, which is the most common cause of prosthetic failure, is especially important because of different types of therapeutic management. Despite a thorough patient history, physical examination, multiple diagnostic tests and complex algorithms, differentiating PJI from aseptic loosening remains challenging. Among imaging modalities, radiographs are neither sensitive nor specific and cross-sectional imaging techniques, such as computed tomography and magnetic resonance imaging, are limited by hardware-induced artefacts. Radionuclide imaging reflects functional rather than anatomical changes and is not hampered by the presence of a metallic joint prosthesis. As a result scintigraphy is currently the modality of choice in the investigation of suspected PJI. Unfortunately, there is no true consensus about the gold standard technique since there are several drawbacks and limitations inherent to each modality. Bone scintigraphy (BS) is sensitive for identifying the failed joint replacement, but cannot differentiate between infection and aseptic loosening. Combined bone/gallium scintigraphy (BS/GS) offers modest improvement over BS alone for diagnosing PJI. However, due to a number of drawbacks, BS/GS has generally been superseded by other techniques but it still may have a role in neutropenic patients. Radiolabelled leucocyte scintigraphy remains the gold standard technique for diagnosing neutrophil-mediated processes. It seems to be that combined in vitro labelled leucocyte/bone marrow scintigraphy (LS/BMS), with an accuracy of about 90%, is currently the imaging modality of choice for diagnosing PJI. There are, however, significant limitations using in vitro labelled leucocytes and considerable effort has been devoted to developing alternative radiotracers, such as radiolabelled HIGs, liposomes, antigranulocyte antibodies and fragments, as well as more investigational tracers such as radiolabelled antibiotics, antimicrobial peptides, bacteriophages and thymidine kinase. On the other hand, positron emission tomography (PET) is still growing in the field of PJI imaging with radiotracers such as 18F-fluorodeoxyglucose (FDG), 18F-FDG white blood cells and 18F-fluoride. But unfortunately this superb tomographic technique will only receive full acceptance when specific PET uptake patterns can be successfully developed. The emergence of hybrid modality imaging using integrated single photon emission computed tomography (SPECT) and PET with computed tomography (SPECT/CT and PET/CT) may also have a contributing role for more accurate assessment of joint replacement complications, especially combined with new radiotracers such as 68Ga and 64Cu. Finally, in searching for infection-specific tracers, currently there is no such diagnostic agent available.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
As life expectancy increases, prosthetic joint replacement is becoming a more frequently used procedure to improve quality of life of the aging population. Total joint arthroplasty is one of the most reliable and cost-effective surgical procedures performed [1]. Complications of prosthetic joint surgery such as heterotopic ossification, fracture and dislocation are relatively uncommon. Aseptic or mechanical loosening and polyethylene wear is nowadays the major cause of arthroplasty failure, which can occur in more than one quarter of patients [2]. Although occurring infrequently, prosthetic joint infection (PJI) nevertheless is a serious complication of joint replacement surgery that results in substantial morbidity and decline in functional outcome. Moreover, it is associated with significant clinical, psychological and financial costs. Furthermore, surgeons are faced with an increasingly complex mix, with a higher prevalence of immunocompromised patients, increased co-morbidities and antibiotic-resistant bacteria, along with several known patient-related and surgical risk factors [3].
Classifications, pathogenesis and clinical scenarios
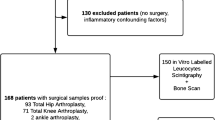
Classification schemes encompass the pathophysiological and pathogenetic pathway of the development of PJI and on the other hand a distinction between early, delayed and late presentation may be clinically useful. Some of the currently used classifications are explained in Table 1 and Fig. 1 [1, 4].
Causes of infection associated with prosthetic joints. There are two basic pathogenetic concepts of PJI. PJI related to surgery including a small number of otherwise non-virulent bacteria contaminating the implant during surgery and persisting as a biofilm despite a functional immune system and antimicrobial treatment. Secondly, haematogenous PJI whereby bacteria invade into the sterile encapsulated joint space through a process of bacteraemia, acquired from any remote infectious process in the body elsewhere. Commonly and less frequently isolated microorganisms are shown (adapted with permission from [132])
Today’s prosthesis, a combination of metal (cobalt-chromium or titanium) and plastic (ultrahigh molecular weight polyethylene), can be attached to native bone in numerous ways. In aseptic and septic conditions, initially, the prosthetic implant is surrounded by a bone and fibrous tissue membrane, leading to osseous integration. Only rarely does bone directly interface with the metal or plastic of the prosthesis; usually it is separated by a thin layer of reactive fibrous tissue situated between the host and the implant or its anchoring cement, known as the “membrane” by orthopaedic surgeons. Even well-fixed implants may have these membranes, but in a failed prosthetic joint, this membrane becomes thickened by inflammatory cells, collagen and blood vessels. In infection, in which microbial colonization of the prosthesis occurs at the time of implantation or thereafter (e.g. as a result of haematogenous seeding), a low inoculum appears to be sufficient. The presence of a foreign body, the prosthetic joint, and the formation of a biofilm contribute to the susceptibility to infection. The responsible pathogens attach to the devices by proteinaceous cell wall and capsular polysaccharide-associated adhesins and remain subsequently protected from antibiotics and the host immune response by secreted biofilms.
The clinical scenarios of PJI depend upon the time of infection, similar to the pathogenesis, summarized in Table 1 [4].
More recent studies reported a shift from acute/early to more chronic/late PJI, reflecting changes in surgical practice, including the use of prophylactic antibiotics and improvements in the operating room environment [3].
Preoperative workup
Preoperative diagnosis of PJI relies on clinical history, physical examination and investigations including serum markers of inflammation [white blood cell count, C-reactive protein (CRP) and erythrocyte sedimentation rate (ESR)], joint aspiration and several imaging modalities (Table 2).
A thorough evaluation of medical and surgical history as well as physical examination is an excellent screening tool for PJI and helps guide subsequent diagnostic evaluation.
Establishing the presence of acute infection or, in the presence of a sinus tract communicating with the prosthesis, chronic infection, is rather uncomplicated. Furthermore, the diagnosis of PJI is straightforward in some patients in whom joint aspiration is diagnostic and the clinical signs of infection are obvious. The most challenging diagnostic situation, however, is a persistent slight elevation of the CRP level or persistent pain after surgery. In these circumstances, the distinction between delayed infection and failure related to prosthetic wear debris can be very difficult.
Acute phase reactants must be interpreted cautiously in patients with coexistent chronic inflammatory rheumatic diseases that can produce the same response. In addition, a normal ESR or CRP level does not completely rule out a low-grade infection, although false-negative results may occur in patients who have been treated with antibiotics or present with indolent delayed-onset infection [5].
If blood cultures are not positive, joint aspiration may allow confirmation of the diagnosis [6].
Finally, due to substantial lack of any definite preoperative tests for detecting PJI with high certainty, a variety of imaging modalities (such as radiological and nuclear medicine techniques) have been developed for further evaluation of the suspected PJI [2].
Imaging techniques and features
Nuclear medicine compared to radiographic techniques
Plain radiographs should always be performed for the evaluation of the painful arthroplasty. Radiographic findings such as radiolucency, osteolysis and migration are observed in both infection and aseptic loosening and, therefore, they may be neither sensitive nor specific for diagnosing PJI. Periosteal new bone formation or an adjacent soft tissue collection are highly suggestive of infection but are infrequently present. In the early stages of infection plain radiographs will be normal in appearance. Plain radiographs, therefore, have the greatest utility when serial studies are performed over time. They often demonstrate loosening of the prosthesis in delayed-(onset) infections, but signs of loosening are usually absent in patients with early-(onset) and acute-(onset) haematogenous infections. Finally, conventional radiographs can rule out other conditions such as dislocation and periprosthetic fractures [7].
Ultrasonography may detect the presence of periprosthetic collections and joint effusions around the prosthesis and can be used to guide joint aspiration and drainage procedures. It is especially helpful in prosthetic hip infection in which effusion cannot be clinically diagnosed [7].
Cross-sectional imaging techniques, such as computed tomography and magnetic resonance imaging, are of limited value in the presence of metallic prosthetic implants owing to beam hardening and dephasing artefacts [7]. Nevertheless, advances in multidetector CT and several MRI techniques have improved the image quality by further minimizing metallic artefacts. MRI displays greater resolution for periprosthetic soft tissue abnormalities than CT or radiography. On the other hand, CT is useful in detecting joint effusion, sinus tracts, soft tissue abscesses, bone erosion and periprosthetic lucency, especially in the case of total hip arthroplasty. In addition, similarly to ultrasonography, it may assist in guiding joint aspiration and selecting the surgical approach [4, 7].
Radionuclide imaging, which is, in general, not affected by metallic hardware, is the current imaging modality of choice for evaluation of suspected joint replacement infection [2]. The two oldest radionuclide imaging modalities used for this purpose are bone scintigraphy (BS) and gallium citrate scintigraphy [8] (Table 3).
Bone scintigraphy
BS is widely available, relatively inexpensive, easily performed and rapidly completed. Uptake of bone-seeking tracers such as 99mTc-labelled diphosphonates MDP or HDP, which accumulate on the surface of the bone mineral matrix, depends on blood flow and especially on the rate of new bone formation [9]. The main reason is that accumulation of labelled diphosphonates occurs inconsistently in periosteal new bone. Moreover, uptake of those bone-seeking radiopharmaceuticals is also well known in areas of sterile inflammation, such as osteolysis induced by polyethylene wear debris. Also, any cause of accelerated new bone formation, including postoperative physiological bone remodelling, as well as pathological conditions such as fracture, heterotopic ossification, aseptic loosening and infection all may present as increased periprosthetic activity on BS. Subsequently, tracer uptake around the prosthesis greater than the background level can occur as a physiological response for several months following joint replacement. Therefore, any new bony uptake (focal or diffuse) around a prosthesis can be caused by both septic and aseptic loosening. Persistent uptake more than 12 months after surgery is usually abnormal; however, in clinical practice, tracer uptake is known to persist for an even longer period of time. In general BS is highly sensitive but not very specific as it cannot differentiate between infection and aseptic loosening (Figs. 2 and 3).
a Infected 3-year-old cementless revised left hip prosthesis. There is diffusely increased activity around the femoral component of the prosthesis. Intraoperative cultures grew S. aureus. b Aseptically loosened 4-year-old cementless left hip prosthesis. There is diffusely increased activity around the femoral component of the prosthesis. Compare with a. Periprosthetic uptake patterns on bone scans do not reliably differentiate between infection and aseptic loosening
a Aseptically loosened 6-year-old knee prostheses. Note the striking bony uptake around the left knee prosthesis, compared to the right. b One-year-old infected right knee prosthesis. Intraoperative cultures grew S. hominis. Periprosthetic uptake pattern is virtually indistinguishable from that in Fig. 3a
Moreover, the data in the literature about its diagnostic efficiency show a considerable variability and to some extent, this inconsistency is caused by several factors, such as (1) the use of different scan interpretation criteria (quantitative analysis versus qualitative approach), (2) performing a three-phase study instead of only a delayed bone scan, (3) the type of prosthesis (knee versus hip, cemented versus cementless, old versus new ones) affecting both the degree and the pattern of periprosthetic bone uptake, and last but not least, (4) the fact that during the first year after implantation, when nearly two thirds of all PJIs occur, periprosthetic bony uptake is so variable that only a completely normal BS, which in clinical practice is uncommon, provides us useful information [10–19]. Nonetheless, BS is more sensitive than plain radiographs [20]. Lieberman et al. suggested, therefore, that BS is useful only when conventional radiography is inconclusive [21]. Others have suggested that the role of BS should be limited to that of a screening test, or that it should be performed as a part of a combined study with gallium or labelled leucocyte scintigraphy (Table 4).
Sequential bone/gallium scintigraphy
In an effort to enhance the radionuclide diagnosis of PJI, 67Ga-citrate scintigraphy (GS) often is improved in addition to BS and the two studies are interpreted together using standardized criteria [22–24]. Since both gallium and diphosphonates are bone-seeking radiopharmaceuticals, 67Ga-citrate is not accurate enough to image PJI. Similar to diphosphonates, gallium also accumulates not only in infection, but also in the postoperative patient, in heterotopic or periosteal new bone formation, aseptic loosening, fractures and even granulomatous reaction to prosthetic cement [24, 25]. Images are therefore interpreted by established criteria comparing congruity of the spatial distribution and intensity of the two scans. Although sequential BS/GS, with an accuracy ranging from 65 to 80%, provides somewhat better results than BS alone, it seems to be of limited value for diagnosing PJI, also in combination with a number of drawbacks inherent to 67Ga-citrate [14, 24, 26, 27] (Fig. 4).
a Bilaterally infected 10-year-old cementless hip prostheses. The distribution of activity on the bone and gallium images is spatially incongruent and the combined study is (true) positive for infection. Intraoperative cultures grew S. aureus. b Aseptically loosened 3-year-old cemented left total hip replacement. Periprosthetic uptake on the gallium study is similar in distribution to that on the bone scan, but is much more intense and the combined study is (false) positive for infection. Combined bone/gallium imaging is only slightly more accurate than bone imaging alone for diagnosing PJI
Labelled leucocyte scintigraphy (LS)
Targeting leucocytes that migrate to sites of infection and inflammation may represent the single most important achievement in radionuclide diagnosis of infection to date. Commonly used tracers include 111In-oxine and 99mTc-hexamethyl propyleneamine oxime (HMPAO). The introduction of in vitro labelled autologous leucocytes has dramatically improved the accuracy of the radionuclide diagnosis of PJI [28–30]. Labelled leucocytes do not accumulate at sites of increased bone turnover or remodelling in the absence of infection. Uptake of labelled cells depends on intact chemotaxis, the number and type of cells labelled, and the principal cellular component of a given inflammatory response [31]. Since circulating neutrophils are predominantly labelled and neutrophils are inconsistently present in the infected prosthetic joint, LS is the gold standard for imaging this purpose. Moreover, at least in theory, LS is particularly well suited to distinguish between the infected prosthesis and the inflamed aseptically loosened prosthesis, in which neutrophils are generally absent [31–34] (Fig. 5).
Some investigators reported that the technique was sensitive, but not specific, while other investigators found that the test was specific, but not sensitive. These relatively unsatisfactory results reported for LS, performed as the only radionuclide imaging technique, have been attributed to several factors, such as (1) the presence of a chronic or low-grade infection with fastidious microorganisms and the presence of a biofilm around the infected prosthesis (decreasing its sensitivity) [35, 36], (2) the possible negative influence of administered antibiotics (decreasing its sensitivity) [37], (3) the non-specific inflammation in the neighbouring soft tissues (decreasing its specificity), (4) the interfering problem of ectopic bone marrow present in the appendicular skeleton, particularly induced by prosthetic surgery (decreasing its specificity) [38–41], and last but not least (5) the inability to develop a generally accepted acquisition protocol in combination with the lack of a satisfactory analysis method for interpretation of the images [2, 42, 43].
Moreover, the cell labelling technique is labour intensive, requires appropriately trained staff and there is handling of blood products which entails a risk for contamination. Finally, in neutropenic patients there may also be too few leucocytes available for harvesting and for labelling.
Conventional radionuclide imaging: enhanced techniques
Therefore, to overcome those limitations of in vitro LS, for many years, a combination of two or even three radiopharmaceuticals and/or modifications of the scanning protocol have (largely) been adopted in clinical practice (Table 4).
Leucocyte/bone scintigraphy
The combination of BS and LS did not significantly improve accuracy, as expected. Diagnostic criteria for a positive study were non-congruent bone and leucocyte uptake, either in spatial distribution or in intensity [44] (Fig. 6).
In the largest retrospective study on suspected hip prostheses comprising 116 patients, Teller et al. found, besides a lower sensitivity of 64% and a moderate high specificity of 78%, that a positive 111In LS only increased the likelihood of infection from 14 to 30%, although negative results decreased the likelihood to 7% [45].
Leucocyte/bone marrow scintigraphy (BMS)
Because leucocyte uptake around prostheses can be secondary to bone marrow displacement or activation by surgery, the combination of LS and BMS with 99mTc-sulphur colloid has been introduced [46]. The principal of combined LS/BMS is thus based on the fact that LS and BMS both reflect radiotracer accumulation in the reticuloendothelial system of the marrow [38]. While the distribution of marrow activity is similar on LS and BMS in normal individuals and in those with underlying marrow abnormalities, on the other hand in osteomyelitis, LS and BMS are not similar due to the fact that infection stimulates uptake of leucocytes but suppresses uptake of sulphur colloid. Therefore, LS and BMS are spatially incongruent in PJI [31] (Fig. 7).
a Aseptically loosened right hip replacement. The distribution of activity around the prosthesis on the labelled leucocyte (left) and sulphur colloid (right) images is spatially congruent, and the combined study is negative for infection. b Infected right hip replacement. There is activity around the femoral component on the labelled leucocyte study (left). On the bone marrow image (right), however, activity is present only distal to the tip of the prosthesis. The distribution of activity on the labelled leucocyte and sulphur colloid images is spatially incongruent (arrows), and the combined study is positive for infection
Over the years the results of LS/BMS, with few exceptions, have been remarkably consistent, with reported accuracies ranging from 86 to 98%. In most of the LS/BMS series reported to date, leucocytes have been labelled with 111In-oxine. Recent data, however, suggest that comparable results can be achieved using leucocytes labelled with 99mTc-HMPAO [11, 46–51].
Late leucocyte scintigraphy
Some investigators have found that the accuracy of LS for diagnosing PJI is improved by performing early and late imaging. Larikka et al. reported improved sensitivity (83 vs 50% and 100 vs 87% for hip and knee prostheses, respectively) and specificity (100 vs 90% and 82 vs 77% for hip and knee prostheses, respectively) by comparing early (4–6 h) and late (20–24 h) 99mTc LS [35, 36]. Fernandez et al. came to similar conclusions, in a study with 49 prosthetic joint implants. Those results show again an improvement of specificity (87 vs 72%) and also a greater inter-observer reproducibility, for 4-h/24-h compared to 4-h 99mTc LS [52] (Fig. 8).
Serial time point or multiphase leucocyte scintigraphy
Other investigators have used dual or serial time point LS as a surrogate for BMS. The hypothesis is that early leucocyte images reflects white blood cell uptake in marrow, since neutrophil uptake in the bone marrow, as in the spleen, is immediate and the result of extensive physiological margination in sinusoids, while the late leucocyte images reflect white blood cell uptake in infection [53, 54]. Subsequently, incongruence between early and late images, analogous to conventional LS/BMS, is indicative of infection.
Pelosi et al. studied the accuracy of a serial time point (50 min, 4 h and 20 h) imaging protocol with 99mTc LS in 78 patients suspected of having infected hip-knee arthroplasties. They found that the accuracy of the technique, using visual analysis, was about 75%. Using semi-quantitative analysis, considering a 10% up ratio positive for infection, the accuracy improved to about 95% [55]. Simonsen et al. retrospectively reviewed 76 painful hip prostheses studied with 99mTc LS and found in agreement with Pelosi et al. that serial (LS) imaging improved the accuracy of the technique [56].
In vivo labelled leucocyte scintigraphy or antigranulocyte scintigraphy (AGS)
Reducing or eliminating the need for a separate bone marrow study would be an improvement over combined LS/BMS, but there are other limitations to the technique as well, responsible in some part to the fact that LS/BMS is not widely used in clinical practice and the poor availability of sulphur colloid in Europe. Considerable efforts, therefore, have been devoted to developing in vivo methods of labelling leucocytes with promising results (Table 4).
Granuloscint/Scintimun® and sulesomab/LeukoScan® are a murine whole monoclonal G1 immunoglobulin and, on the other hand, a 50-kDa fragment antigen binding (Fab′) portion, that bind respectively to the non-specific cross-reacting antigen (NCA) 95 and NCA 90 present on activated leucocytes [57]. The technique involves injection of a prepared agent (kit) into the patient relying on in vivo trafficking of leucocytes. Therefore, similarly to in vitro labelled leucocytes, both radiopharmaceuticals are proposed as promising agents for imaging of inflammation and infection. The results of these agents for diagnosing PJI, however, have been variable [58–63].
Similarly to in vitro LS, some investigators have also made adaptations to the scanning protocol of AGS, in order to improve the specificity of this modality [64–67] (Fig. 9).
Infected left knee replacement after revision of the tibial component 1 year earlier. Antigranulocyte antibody scintigraphy: on the early image (30 min p.i.) there is faint focal labelled granulocyte activity at the proximal tibia (arrow) and mild diffuse labelled granulocyte activity in the synovium of the knee joint; but on the 20-h image, there is persistent but now intense focal uptake at the proximal tibia (arrow), probably localized in the soft tissues near the prosthesis itself, indicating an infected knee prosthesis
SPECT/CT bone, leucocyte and gallium imaging modalities
The main drawback of radionuclide imaging is the limited spatial resolution and subsequently the poor anatomical detail compared to morphological modalities, such as CT and MRI [7, 68].
A complicated matter in conventional nuclear medicine studies is the absence of anatomical landmarks for delineating the pathological process and for differentiating soft tissue from bone infection, for example differentiating soft tissue involvement from deep-seated prosthesis infection. It is well known that single photon emission computed tomography (SPECT) enables more exact localization of the radiotracer uptake than is afforded by planar imaging alone, resulting in greater specificity [69]. Van Acker et al. and Vanquickenborne et al. investigated the possible role of performing LS SPECT and/or BS SPECT in the setting of the painful knee arthroplasty as well as infected hip prostheses. In both reports, they concluded that performing LS/BS with additional SPECT did indeed increase the accuracy in detecting PJI [70, 71] (Fig. 10).
LS SPECT/CT, performed at 4 h p.i., shows pathological activity at the prosthesis proximal part, the presence of a chronic fistulization in the upper thigh (arrow) and an abscess collection near the distal part of the femoral shaft (dashed arrow), indicating a chronic infected hip prosthesis. Combining SPECT/CT fusion images enhances the exact localization and, in particular in this case, the extent of the inflamed tissues, probably more accurately than SPECT alone. Subsequently, the orthopaedic surgeon can be prepared for an extended treatment strategy. Finally, note the presence of metal artefacts, generated on the low-dose CT
These difficulties have been overcome, to a great extent, with the introduction of in-line SPECT/CT systems [72, 73]. The contribution of SPECT/CT with LS or 67Ga-citrate scintigraphy has been evaluated in a variety of clinical indications, demonstrating a definite added value in distinguishing physiological uptake of labelled leucocytes from infectious processes and defining the precise anatomical location of infection in up to 85% of cases [72, 74].
First clinical studies with this integrated hybrid machine in the field of infection and inflammation and in some part of PJI imaging are very promising. In patients with osteomyelitis, LS SPECT/CT can also detect areas of tracer accumulation in surrounding soft tissues, thus defining the precise extent of infection with ensuing relevant clinical impact on patient management. Horger et al. were the first to demonstrate in patients with suspected chronic post-traumatic osteomyelitis imaged with 99mTc-AGS SPECT/CT, compared to SPECT, that the specificity improved substantially (89 vs 78%) while the sensitivity remained equal. They concluded that 99mTc-AGS SPECT/CT was therefore of clinical relevance in selecting patients for surgery [75].
In another study, Filippi and Schillaci investigated the value of additional SPECT/CT to 99mT LS in 28 patients with suspected bone (n = 15) and joint infections (n = 13). They showed that SPECT/CT allowed a correct diagnosis of prosthesis versus soft tissue involvement in five of seven patients with a hip prosthesis. In two of six patients with knee prostheses SPECT/CT correctly localized leucocyte uptake in the synovium and therefore could reliably exclude a PJI [76].
18F-Fluorodeoxyglucose positron emission tomography: current role in PJI
In recent years, 18F-fluorodeoxyglucose positron emission tomography (FDG PET) has been used successfully for assessing a multitude of malignant disorders. FDG, however, also accumulates at the sites of infection and inflammation, including those of the musculoskeletal system [77].
FDG PET has a number of advantages over conventional radionuclide imaging modalities such as LS/BMS or BS/GS of showing no physiological bone marrow uptake [78, 79]. In addition, the PET technique inherently provides high-quality images with improved spatial resolution and imaging is completed within a reasonably short time of 2–3 h [79]. In addition, PET/CT combines PET with a low or conventional dose CT scan and provides excellent anatomical correlation of any areas of uptake which increases the accuracy compared to PET alone. Therefore, FDG PET and PET/CT are emerging as important imaging modalities in the management of patients with painful arthroplasty [80].
Published results on the role of FDG PET for diagnosing PJI are however inconclusive due to several factors, such as (1) the lack of uniform interpretation criteria used (quantitative versus qualitative approach by means of standardized uptake values or SUV), (2) different FDG uptake patterns and interpretation criteria, (3) the fact of generating artefacts inherent to the material used as well as introduced by the PET technique and the coregistered CT portion, (4) the important role of activated leucocytes in the inflamed prosthesis, such as neutrophils and macrophages, and the fact that glucose consumption can be even higher in activated macrophages, and (5) the postoperative remodelling conditions involved in arthroplasty surgery and subsequently a-specific FDG periprosthetic uptake up to 6 months after insertion, similarly to conventional tracers [16, 17, 43, 49, 70, 71, 81–86] (Figs. 11, 12 and 13, Table 4).
Qualitative analysis of FDG uptake according to the classification system of Reinartz et al. demonstrate several patterns differentiating PJI (type 5) from aseptic loosening (type 4), physiological remodeling (types 2–3), and normal findings (type 1, no uptake, not shown), in patients scanned with an interval of 6 months after hip arthroplasty (adapted with permission from [17])
Infected 4-month-old right knee replacement. Patient with persistent elevated inflammatory parameters after recent total knee arthroplasty was sent for both dedicated PET/CT (a) and LS (b). Both studies were rather congruent, namely diffuse pathological uptake around the soft tissues and the knee joint, probably indicating an acute infected knee arthroplasty. Intraoperative findings revealed gross purulence and cultures grew S. aureus. Note again, similarly to SPECT/CT, the presence of metal-induced CT artefacts. Performing a PET/CT study was, in this particular case, not contributive
Investigational/experimental tracers
Interleukin-8
Small diffusible molecules, such as small proteins and peptides, which can readily cross the activated endothelium, are used for the development of new tracers including radiolabelled chemokines and cytokines, respectively targeting circulating and migrating neutrophils, lymphocytes and mononuclear cells [87]. One of them is the acute phase cytokine, interleukin-8 (IL-8). Initial clinical investigations with 99mTc-labelled IL-8 in patients with various infections have recently been reported. The sensitivity, specificity and accuracy were 83, 100 and 90%, respectively, and there were no adverse events [88]. These results are encouraging, but the value of this agent in PJI is not known.
111 In-Biotin scintigraphy is based on the non-specific accumulation of biotin at sites of infection, partly linked to increased transcapillary leakage of macromolecules and to interstitial oedema at these sites [89]. On the other hand biotin, known as vitamin H, is a compound of low molecular weight and it is suggested that biotin is partly utilized by growing bacteria at the site of infection according to the rate of their metabolism [90, 91]. Therefore, biotin is now used as a single agent as 111In-biotin for imaging infection and inflammation [92].
Annexin V scintigraphy
Radiolabelled annexin V is a marker of apoptosis and cellular stress or activation and has already been used as a non-invasive tracer for detection of acute, subacute and chronic inflammation in several animal models and humans. In a preliminary study of seven patients undergoing revision surgery for hip (n = 5) or knee (n = 2) prostheses, Lorberboym et al. reported for the first time on 99mTc-recombinant annexin V scintigraphy [93]. They found four true-positive, two true-negative and one false-positive annexin V images. They also found that annexin V uptake in the periprosthetic region is more common and intense in infected prostheses than in aseptic loosening [93].
Infection-specific tracers
Among the myriad of radionuclide imaging techniques currently available, none truly is specific for infection, and the search continues for new and better agents [94]. Radiolabelled antibiotics have been investigated for their potential as “infection-specific” tracers [95]. Initially there were promising results with 99mTc-Ciprofloxacin for diagnosing prosthetic hip and knee infection [96–98].
In contrast, results of in vitro binding, animal and clinical studies reported that 99mTc as well as 18F-Cipro was not specific for bacterial infections and that, although it was sensitive, the technique could not reliably differentiate the infected from the aseptically loosened joint replacement [99–102]. Recently this non-specificity was demonstrated in a single-centre, phase II, prospective clinical trial comparing 99mTc-Cipro versus combined LS/BMS [103] (Fig. 14).
Aseptically loosened left hip replacement. There is diffuse periprosthetic activity (arrows) on the Tc-ciprofloxacin image and the study is false-positive for infection (same patient as illustrated in Fig. 11)
Antimicrobial peptides play a critical role in the biological defence system of multicellular organisms [104]. They are produced by various cells, including phagocytes, endothelial and epithelial cells and bind to the bacterial cell membrane. Their expression may be constant or induced on contact with microbial organisms; they also may be transported to sites of infection by leucocytes [105]. Radiolabelled synthetic fragments of ubiquicidin (UBI), a naturally occurring human antimicrobial peptide that targets bacteria, possess the ability to differentiate infection from sterile inflammation [106]. Moreover, it seems to be that the amount of radiolabelled UBI 29-41 uptake depends on the number of viable bacteria present at the site of infection, but results of recent data, performed in animal models of several infections (including PJI), are more controversial [107–111]. Nevertheless, first studies of this agent for diagnosing PJI in humans are encouraging [112].
Another application of a potential infection-specific imaging agent is the introduction of radiolabelled bacteriophages which are specific for bacterial species. The binding mechanism consists of the attachment of the phages to specific surface receptors or domains located on the surface of the bacterium and, subsequently, by transferring their genetic material into the host cell dedicated to phage replication/reproduction [113].
Recently, four 99mTc-labelled bacteriophages against different microorganisms as potential infection-specific imaging tracers were developed. Unfortunately, only one radiolabelled bacteriophage showed any specificity for its host bacteria, indicating this approach needs major evaluation before further studies can be considered [114].
Finally, another approach is the use of enzymatic substrates of bacterial enzymes. These ligands allow the non-invasive detection of bacteria or viruses by targeting thymidine kinase (TK), whose substrate is distinct from that of the major human TK. Because those uracil nucleoside derivatives are incorporated into bacteria rather than into inflammatory cells, it should be specific for the infectious process, as shown in a pilot study of musculoskeletal bacterial infection in humans [115].
Future applications of hybrid imaging with new radiotracers
Following the introduction of new infection imaging agents, such as antigranulocyte antibodies and fragments, ciprofloxacin and biotin, SPECT/CT has demonstrated definite advantages over single-modality imaging [75, 116].
Although 111In-biotin SPECT/CT has been reported to have a high diagnostic value in imaging spinal infections, Graute et al. were the first investigators to evaluate the value of 99mTc-AGS SPECT/CT in a homogeneous series of patients with suspected low-grade PJI [117]. In a retrospective study of 31 consecutive patients (mainly knee implants), they found that AGS SPECT/CT made a contribution to the final diagnosis in 7 of 31 patients (23%), compared to only 4 cases (13%) for SPECT alone. Thus, they concluded that additional SPECT/CT could provide accurate anatomical as well as precise information on the extent of the infection. Finally, the number of false-positive studies (planar and SPECT) was reduced to six cases when performing additional SPECT/CT, resulting in a moderate positive predictive value of 57%.
In a preliminary study of using PET/CT in hip prosthesis infections, Chen et al. reported a high sensitivity (100%) but a variable specificity (50–87.5%) in predicting residual infection after insertion of an interim spacer [118]. Although the limitations of FDG in imaging arthroplasty are known, on the other hand given the high negative predictive value, they concluded that PET/CT can be used to rule out persistent infections [118].
The labelling of leucocytes with 18F-FDG has also been investigated in a variety of infections throughout the body with high sensitivity and specificity [119]. Although the results of 18F-FDG-labelled WBCs in initial clinical investigations, including PJI, were encouraging, there are several disadvantages inherent to this procedure [120]. First of all, the labelling efficiency and stability of FDG-labelled leucocytes is significantly less than that for SPECT ligands (such as 111In-oxine and 99mTc-HMPAO) and it is evident that blood glucose levels affect this labelling procedure. Furthermore, 18F is far from ideal as a radiolabel, quite apart from the instability of 18F-FDG-labelled leucocytes, its half-life of 110 min does not allow sufficient time for imaging of leucocyte migration [121]. For this reason, in the future 64Cu, which has an optimal half-life of 12.7 h, seems to be more suitable [122].
FDG is not the only tracer used in PET imaging nowadays. In a small study of 14 painful knee arthroplasties, Sterner et al. showed a 100% sensitivity for the detection of early aseptic loosening in total knee arthroplasty using the bone-seeking tracer 18F-fluoride [123]. In a recent prospective study, using 18F-fluoride PET in 65 hip prosthetic joints, Kobayashi et al. found a sensitivity and specificity of 95 and 98% for all cases and a sensitivity and specificity of 95 and 88% for surgically treated cases, by using a new uptake pattern classification system for discerning aseptic from septic loosening (Fig. 15). They concluded for the first time that fluoride PET has considerable potential as a method to differentiate septic from aseptic loosening following total hip arthroplasty, since the uptake pattern classification system is relatively simply performed [124]. This first rather large-scale study of fluoride PET suggests a potential role in imaging the failed prosthetic joint but, nevertheless, more studies are warranted in the future.
Qualitative analysis of Fluoride uptake according to the classification system of Kobayashi et al demonstrate several patterns differentiating PJI (type 3, major uptake) from aseptic loosening (type 2, minor uptake), and normal findings (type 1, no uptake, not shown), in patients scanned with an interval of 1 year after hip arthroplasty; subtypes are defined as follows: (A) uptake localized on the cup side; (B) uptake localized on the stem side; (C) uptake localized on both the cup and stem sides (adapted with permission from [124])
Radiolabelled targeting of inflammatory cells such as macrophages has shown some promise. For example, Kropholler et al. used PET to monitor macrophage migration into inflamed areas in rheumatoid arthritis using the ligand PK11195 coupled to a PET tracer, 11C, which binds to benzodiazepine receptors on macrophages [125].
The same limitation, as for 18F-FDG, would apply to 68Ga, a generator-produced radiometal with a half-life comparable to 18F-FDG, namely 68 min. Nevertheless, the availability of this PET tracer from a 68Ge/68Ga generator makes it attractive to use in busy nuclear medicine departments, particularly those with limited access to cyclotrons. Furthermore, the addition of targeting small vascular adhesion molecules (VCAM), a vascular peptide protein 1 (VAP-P1), or even transferrin to 68Ga allows specific targeting of molecules of inflammation and infection instead of trafficking white blood cells, such as expressed in osteomyelitis [126–128].
Finally, there are numerous other PET radiotracers under development that may have applications in inflammatory disorders, such as [11C]choline and [18F]fluorothymidine (FLT) PET, which are currently used as markers of cellular proliferation.
Summary
Over the past 20 years, radionuclide imaging has improved the accuracy of the diagnosis of PJI [30]. Sequential bone/gallium scintigraphy, the first generation of scintigraphic imaging techniques introduced for this purpose, has been replaced by combined leucocyte/bone marrow scintigraphy [2]. Despite an accuracy of about 90%, the technique is expensive, time consuming, labour intensive, not widely available and potentially hazardous [80]. Unfortunately, data on FDG PET are rather inconsistent and suggest no additional benefit to conventional nuclear medicine modalities, e.g. combined leucocyte/bone marrow scintigraphy, for the diagnosis of PJIs [129]. Although hybrid imaging is entering the field of PJI imaging, today data are however still limited and further studies are needed to verify if this new modality may really become clinically relevant in the near future [130]. Finally, in order to replace combined leucocyte/bone marrow imaging for the differentiation between aseptic and septic prosthetic loosening, agents that can differentiate infection from aseptic inflammation must be developed [131].
Take home messages: PJI imaging
Introduction |
• Infection imaging became widespread in 1971 with the introduction of 67Ga-citrate, despite the significant limitations of this agent |
• Development of radiolabelled leucocytes with 111In or 99mTc improves infection imaging compared with 67Ga, but these agents also localize to inflammatory regions, despite the cumbersome ‘in vitro’ labelling technique |
• A multitude of techniques have been tried to improve PJI imaging, meeting with limited success |
Established imaging agents for PJI: enhanced methods |
• 99mTc or 111In LS/BS: high negative predictive value, but limited specificity in discerning PJI from aseptic loosening |
• 99mTc or 111In LS/BMS: high accuracy in diagnosing PJI, but contemporary bone marrow imaging adds to the complexity of the study, and sulphur colloid is not widely available in Europe (alternative agent is nanocolloid) |
• Serial phase 99mTc LS imaging: 1-h LS image as a surrogate marker for bone marrow image has the potential to replace sulphur colloid scan (if validated in larger homogeneous trials) |
• Antigranulocyte antibody and fragment scintigraphy: high negative predictive value, but limited specificity in discerning PJI from aseptic loosening; can be improved by serial time point imaging and/or adding nanocolloid |
Investigational agents for PJI |
• Since the late 1980s a wide variety of diagnostic agents have been tried in an attempt to improve infection imaging, such as: |
- Nanocolloids/HIGs/liposomes: no translation into clinical practice—not commercially available |
- Chemotactic peptides: LTB4 lack of human studies |
- Cytokines: IL-8 first study in infection is promising, but not commercially available |
- Ciprofloxacin and/or quinolone family: sensitive technique for the inflamed prosthesis, but limited specificity in discerning PJI from aseptic loosening |
- Biotin: first studies in infections are promising, but the value of this agent in PJI is not known |
- Ubiquicidin: data on the role of this agent for diagnosing PJI in humans are encouraging, but still very limited |
- Bacteriophage: no studies in humans are available |
- Thymidine kinase: pilot study of musculoskeletal bacterial infection in humans is very promising, but the value of this agent in PJI is not known |
• For more than two decades, several authors have promoted PET as an optimal PJI imaging modality |
- 18F-FDG: pooled average sensitivity and specificity are 84%, more accurate for hip than for knee prostheses; lack of consensus on FDG uptake patterns specific for PJI |
- 18F-FDG-labelled WBCs: comparable results to in vitro leucocyte scintigraphy, cumbersome ‘in vitro’ labelling technique |
- 68Ga: experimental data are promising, but the value of this agent in PJI is not known |
- 64Cu-labelled WBCs: experimental data are promising, but human studies are lacking |
- 18F-Fluoride: fluoride uptake pattern allowed discerning PJI from aseptic loosening, has to be further validated |
Hybrid imaging modalities: new bright future! |
• Since the late 1990s new SPECT/CT and PET/CT have been developed |
- Those superb dual-imaging modalities are very promising for imaging the failed prosthetic implant, especially in combination with the current and future diagnostic agents |
• But superiority above single-imaging modality has still to been proven in further trials |
Future perspective |
• Future work must concentrate on the development of a truly infection-specific imaging agent that works well with the improved SPECT/CT and PET/CT devices |
References
Anguita-Alonso P, Hanssen AD, Patel R. Prosthetic joint infection. Expert Rev Anti Infect Ther 2005;3:797–804.
Love C, Marwin SE, Palestro CJ. Nuclear medicine and the infected joint replacement. Semin Nucl Med 2009;39:66–78.
Bauer TW, Parvizi J, Kobayashi N, Krebs V. Diagnosis of periprosthetic infection. J Bone Joint Surg Am 2006;88:869–82.
Zimmerli W, Trampuz A, Ochsner PE. Prosthetic-joint infections. N Engl J Med 2004;351:1645–54.
Berbari E, Mabry T, Tsaras G, Spangehl M, Erwin PJ, Murad MH, et al. Inflammatory blood laboratory levels as markers of prosthetic joint infection: a systematic review and meta-analysis. J Bone Joint Surg Am 2010;92:2102–9.
Parvizi J, Ghanem E, Menashe S, Barrack RL, Bauer TW. Periprosthetic infection: what are the diagnostic challenges? J Bone Joint Surg Am 2006;88 Suppl 4:138–47.
Palestro CJ, Love C, Miller TT. Infection and musculoskeletal conditions: imaging of musculoskeletal infections. Best Pract Res Clin Rheumatol 2006;20:1197–218.
Palestro CJ, Love C. Radionuclide imaging of musculoskeletal infection: conventional agents. Semin Musculoskelet Radiol 2007;11:335–52.
Love C, Din AS, Tomas MB, Kalapparambath TP, Palestro CJ. Radionuclide bone imaging: an illustrative review. Radiographics 2003;23:341–58.
Maurer AH, Chen DC, Camargo EE, Wong DF, Wagner Jr HN, Alderson PO. Utility of three-phase skeletal scintigraphy in suspected osteomyelitis: concise communication. J Nucl Med 1981;22:941–9.
Palestro CJ, Swyer AJ, Kim CK, Goldsmith SJ. Infected knee prosthesis: diagnosis with In-111 leukocyte, Tc-99m sulfur colloid, and Tc-99m MDP imaging. Radiology 1991;179:645–8.
Levitsky KA, Hozack WJ, Balderston RA, Rothman RH, Gluckman SJ, Maslack MM, et al. Evaluation of the painful prosthetic joint. Relative value of bone scan, sedimentation rate, and joint aspiration. J Arthroplasty 1991;6:237–44.
Schauwecker DS. The scintigraphic diagnosis of osteomyelitis. AJR Am J Roentgenol 1992;158:9–18.
Itasaka T, Kawai A, Sato T, Mitani S, Inoue H. Diagnosis of infection after total hip arthroplasty. J Orthop Sci 2001;6:320–6.
Segura AB, Muñoz A, Brulles YR, Hernandez Hermoso JA, Díaz MC, Bajen Lazaro MT, et al. What is the role of bone scintigraphy in the diagnosis of infected joint prostheses? Nucl Med Commun 2004;25:527–32.
Stumpe KD, Nötzli HP, Zanetti M, Kamel EM, Hany TF, Görres GW, et al. FDG PET for differentiation of infection and aseptic loosening in total hip replacements: comparison with conventional radiography and three-phase bone scintigraphy. Radiology 2004;231:333–41.
Reinartz P, Mumme T, Hermanns B, Cremerius U, Wirtz DC, Schaefer WM, et al. Radionuclide imaging of the painful hip arthroplasty: positron-emission tomography versus triple-phase bone scanning. J Bone Joint Surg Br 2005;87:465–70.
Nagoya S, Kaya M, Sasaki M, Tateda K, Yamashita T. Diagnosis of peri-prosthetic infection at the hip using triple-phase bone scintigraphy. J Bone Joint Surg Br 2008;90:140–4.
Gratz S, Höffken H, Kaiser JW, Behr TM, Strosche H, Reize P. Nuclear medical imaging in case of painful knee arthroplasty. Radiologe 2009;49:59–67.
Magnuson JE, Brown ML, Hauser MF, Berquist TH, Fitzgerald Jr RH, Klee GG. In-111-labeled leukocyte scintigraphy in suspected orthopedic prosthesis infection: comparison with other imaging modalities. Radiology 1988;168:235–9.
Lieberman JR, Huo MH, Schneider R, Salvati EA, Rodi S. Evaluation of painful hip arthroplasties. Are technetium bone scans necessary? J Bone Joint Surg Br 1993;75:475–8.
Rosenthall L, Lisbona R, Hernandez M, Hadjipavlou A. 99mTc-PP and 67Ga imaging following insertion of orthopedic devices. Radiology 1979;133:717–21.
Schauwecker DS, Park HM, Mock BH, Burt RW, Kernick CB, Ruoff III AC, et al. Evaluation of complicating osteomyelitis with Tc-99m MDP, In-111 granulocytes, and Ga-67 citrate. J Nucl Med 1984;25:849–53.
Merkel KD, Brown ML, Fitzgerald Jr RH. Sequential technetium-99m HMDP-gallium-67 citrate imaging for the evaluation of infection in the painful prosthesis. J Nucl Med 1986;27:1413–7.
Palestro CJ. The current role of gallium imaging in infection. Semin Nucl Med 1994;24:128–41.
Gómez-Luzuriaga MA, Galán V, Villar JM. Scintigraphy with Tc, Ga and In in painful total hip prostheses. Int Orthop 1988;12:163–7.
Kraemer WJ, Saplys R, Waddell JP, Morton J. Bone scan, gallium scan, and hip aspiration in the diagnosis of infected total hip arthroplasty. J Arthroplasty 1993;8:611–6.
Thakur ML, Lavender JP, Arnot RN, Silvester DJ, Segal AW. Indium-111-labeled autologous leukocytes in man. J Nucl Med 1977;18:1014–21.
Peters AM, Danpure HJ, Osman S, Hawker RJ, Henderson BL, Hodgson HJ, et al. Clinical experience with 99mTc-hexamethylpropylene-amineoxime for labelling leucocytes and imaging inflammation. Lancet 1986;2:946–9.
Palestro CJ, Love C, Bhargava KK. Labeled leukocyte imaging: current status and future directions. Q J Nucl Med Mol Imaging 2009;53:105–23.
Love C, Tomas MB, Marwin SE, Pugliese PV, Palestro CJ. Role of nuclear medicine in diagnosis of the infected joint replacement. Radiographics 2001;21:1229–38.
Merkel KD, Brown ML, Dewanjee MK, Fitzgerald Jr RH. Comparison of indium-labeled-leukocyte imaging with sequential technetium-gallium scanning in the diagnosis of low-grade musculoskeletal sepsis. A prospective study. J Bone Joint Surg Am 1985;67:465–76.
Datz FL, Thorne DA. Effect of chronicity of infection on the sensitivity of the In-111-labeled leukocyte scan. AJR Am J Roentgenol 1986;147:809–12.
Krznaric E, Roo MD, Verbruggen A, Stuyck J, Mortelmans L. Chronic osteomyelitis: diagnosis with technetium-99m-d, l-hexamethylpropylene amine oxime labelled leucocytes. Eur J Nucl Med 1996;23:792–7.
Larikka MJ, Ahonen AK, Junila JA, Niemelä O, Hämäläinen MM, Syrjälä HP. Extended combined 99mTc-white blood cell and bone imaging improves the diagnostic accuracy in the detection of hip replacement infections. Eur J Nucl Med 2001;28:288–93.
Larikka MJ, Ahonen AK, Junila JA, Niemelä O, Hämäläinen MM, Syrjälä HP. Improved method for detecting knee replacement infections based on extended combined 99mTc-white blood cell/bone imaging. Nucl Med Commun 2001;22:1145–50.
Datz FL, Thorne DA. Effect of antibiotic therapy on the sensitivity of indium-111-labeled leukocyte scans. J Nucl Med 1986;27:1849–53.
King AD, Peters AM, Stuttle AW, Lavender JP. Imaging of bone infection with labelled white blood cells: role of contemporaneous bone marrow imaging. Eur J Nucl Med 1990;17:148–51.
Seabold JE, Nepola JV, Marsh JL, Hawes DR, Justin EP, Ponto JA, et al. Postoperative bone marrow alterations: potential pitfalls in the diagnosis of osteomyelitis with In-111-labeled leukocyte scintigraphy. Radiology 1991;180:741–7.
Palestro CJ, Roumanas P, Swyer AJ, Kim CK, Goldsmith SJ. Diagnosis of musculoskeletal infection using combined In-111 labeled leukocyte and Tc-99m SC marrow imaging. Clin Nucl Med 1992;17:269–73.
Scher DM, Pak K, Lonner JH, Finkel JE, Zuckerman JD, Di Cesare PE. The predictive value of indium-111 leukocyte scans in the diagnosis of infected total hip, knee, or resection arthroplasties. J Arthroplasty 2000;15:295–300.
Palestro CJ. Nuclear medicine, the painful prosthetic joint, and orthopedic infection. J Nucl Med 2003;44:927–9.
Reinartz P. FDG-PET in patients with painful hip and knee arthroplasty: technical breakthrough or just more of the same. Q J Nucl Med Mol Imaging 2009;53:41–50.
Johnson JA, Christie MJ, Sandler MP, Parks Jr PF, Homra L, Kaye JJ. Detection of occult infection following total joint arthroplasty using sequential technetium-99m HDP bone scintigraphy and indium-111 WBC imaging. J Nucl Med 1988;29:1347–53.
Teller RE, Christie MJ, Martin W, Nance EP, Haas DW. Sequential indium-labeled leukocyte and bone scans to diagnose prosthetic joint infection. Clin Orthop Relat Res 2000;373:241–7.
Mulamba L, Ferrant A, Leners N, de Nayer P, Rombouts JJ, Vincent A. Indium-111 leucocyte scanning in the evaluation of painful hip arthroplasty. Acta Orthop Scand 1983;54:695–7.
Palestro CJ, Kim CK, Swyer AJ, Capozzi JD, Solomon RW, Goldsmith SJ. Total-hip arthroplasty: periprosthetic indium-111-labeled leukocyte activity and complementary technetium-99m-sulfur colloid imaging in suspected infection. J Nucl Med 1990;31:1950–5.
Joseph TN, Mujtaba M, Chen AL, Maurer SL, Zuckerman JD, Maldjian C, et al. Efficacy of combined technetium-99m sulfur colloid/indium-111 leukocyte scans to detect infected total hip and knee arthroplasties. J Arthroplasty 2001;16:753–8.
Love C, Marwin SE, Tomas MB, Krauss ES, Tronco GG, Bhargava KK, et al. Diagnosing infection in the failed joint replacement: a comparison of coincidence detection 18F-FDG and 111In-labeled leukocyte/99mTc-sulfur colloid marrow imaging. J Nucl Med 2004;45:1864–71.
El Espera I, Blondet C, Moullart V, Saidi L, Havet E, Mertl P, et al. The usefulness of 99mTc sulfur colloid bone marrow scintigraphy combined with 111In leucocyte scintigraphy in prosthetic joint infection. Nucl Med Commun 2004;25:171–5.
Fuster D, Duch J, Soriano A, Garcia S, Setoain X, Bori G, et al. Potential use of bone marrow scintigraphy in suspected prosthetic hip infection evaluated with 99mTc-HMPAO-leukocytes. Rev Esp Med Nucl 2008;27:430–5.
Fernandez P, Monet A, Matei C, De Clermont H, Guyot M, Jeandot R, et al. 99mTc-HMPAO labelled white blood cell scintigraphy in patients with osteoarticular infection: the value of late images for diagnostic accuracy and interobserver reproducibility. Eur J Clin Microbiol Infect Dis 2008;27:1239–44.
Aktolun C, Ussov WY, Arka A, Glass D, Gunasekera RD, Peters AM. Technetium-99m and indium-111 double labelling of granulocytes for kinetic and clinical studies. Eur J Nucl Med 1995;22:330–4.
Dutton JA, Bird NJ, Skehan SJ, Peters AM. Evaluation of a 3-hour indium-111 leukocyte image as a surrogate for a technetium-99m nanocolloid marrow scan in the diagnosis of orthopedic infection. Clin Nucl Med 2004;29:469–74.
Pelosi E, Baiocco C, Pennone M, Migliaretti G, Varetto T, Maiello A, et al. 99mTc-HMPAO-leukocyte scintigraphy in patients with symptomatic total hip or knee arthroplasty: improved diagnostic accuracy by means of semiquantitative evaluation. J Nucl Med 2004;45:438–44.
Simonsen L, Buhl A, Oersnes T, Duus B. White blood cell scintigraphy for differentiation of infection and aseptic loosening: a retrospective study of 76 painful hip prostheses. Acta Orthop 2007;78:640–7.
Meller J, Liersch T, Oezerden MM, Sahlmann CO, Meller B. Targeting NCA-95 and other granulocyte antigens and receptors with radiolabeled monoclonal antibodies (Mabs). Q J Nucl Med Mol Imaging 2010;54:582–98.
Hotze AL, Briele B, Overbeck B, Kropp J, Gruenwald F, Mekkawy MA, et al. Technetium-99m-labeled anti-granulocyte antibodies in suspected bone infections. J Nucl Med 1992;33:526–31.
Boubaker A, Delaloye AB, Blanc CH, Dutoit M, Leyvraz PF, Delaloye B. Immunoscintigraphy with antigranulocyte monoclonal antibodies for the diagnosis of septic loosening of hip prostheses. Eur J Nucl Med 1995;22:139–47.
Devillers A, Garin E, Polard JL, Poirier JY, Arvieux C, Girault S, et al. Comparison of Tc-99m-labelled antileukocyte fragment Fab′ and Tc-99m-HMPAO leukocyte scintigraphy in the diagnosis of bone and joint infections: a prospective study. Nucl Med Commun 2000;21:747–53.
Ryan PJ. Leukoscan for orthopaedic imaging in clinical practice. Nucl Med Commun 2002;23:707–14.
Vicente AG, Almoguera M, Alonso JC, Heffernan AJ, Gomez A, Contreras PI, et al. Diagnosis of orthopedic infection in clinical practice using Tc-99m sulesomab (antigranulocyte monoclonal antibody fragment Fab′2). Clin Nucl Med 2004;29:781–5.
Pakos EE, Trikalinos TA, Fotopoulos AD, Ioannidis JP. Prosthesis infection: diagnosis after total joint arthroplasty with antigranulocyte scintigraphy with 99mTc-labeled monoclonal antibodies–a meta-analysis. Radiology 2007;242:101–8.
Klett R, Kordelle J, Stahl U, Khalisi A, Puille M, Steiner D, et al. Immunoscintigraphy of septic loosening of knee endoprosthesis: a retrospective evaluation of the antigranulocyte antibody BW 250/183. Eur J Nucl Med Mol Imaging 2003;30:1463–6.
Rubello D, Casara D, Maran A, Avogaro A, Tiengo A, Muzzio PC. Role of anti-granulocyte Fab′ fragment antibody scintigraphy (LeukoScan) in evaluating bone infection: acquisition protocol, interpretation criteria and clinical results. Nucl Med Commun 2004;25:39–47.
Gratz S, Behr TM, Reize P, Pfestroff A, Kampen WU, Höffken H. (99m)Tc-Fab′ fragments (sulesomab) for imaging septically loosened total knee arthroplasty. J Int Med Res 2009;37:54–67.
Sousa R, Massada M, Pereira A, Fontes F, Amorim I, Oliveira A. Diagnostic accuracy of combined 99mTc-sulesomab and 99mTc-nanocolloid bone marrow imaging in detecting prosthetic joint infection. Nucl Med Commun 2011;32:834–9.
Mariani G, Bruselli L, Kuwert T, Kim EE, Flotats A, Israel O, et al. A review on the clinical uses of SPECT/CT. Eur J Nucl Med Mol Imaging 2010;37:1959–85.
Weon YC, Yang SO, Choi YY, Shin JW, Ryu JS, Shin MJ, et al. Use of Tc-99m HMPAO leukocyte scans to evaluate bone infection: incremental value of additional SPECT images. Clin Nucl Med 2000;25:519–26.
Van Acker F, Nuyts J, Maes A, Vanquickenborne B, Stuyck J, Bellemans J, et al. FDG-PET, 99mtc-HMPAO white blood cell SPET and bone scintigraphy in the evaluation of painful total knee arthroplasties. Eur J Nucl Med 2001;28:1496–504.
Vanquickenborne B, Maes A, Nuyts J, Van AF, Stuyck J, Mulier M, et al. The value of (18)FDG-PET for the detection of infected hip prosthesis. Eur J Nucl Med Mol Imaging 2003;30:705–15.
Bar-Shalom R, Yefremov N, Guralnik L, Keidar Z, Engel A, Nitecki S, et al. SPECT/CT using 67Ga and 111In-labeled leukocyte scintigraphy for diagnosis of infection. J Nucl Med 2006;47:587–94.
Schillaci O. Hybrid imaging systems in the diagnosis of osteomyelitis and prosthetic joint infection. Q J Nucl Med Mol Imaging 2009;53:95–104.
Bunyaviroch T, Aggarwal A, Oates ME. Optimized scintigraphic evaluation of infection and inflammation: role of single-photon emission computed tomography/computed tomography fusion imaging. Semin Nucl Med 2006;36:295–311.
Horger M, Eschmann SM, Pfannenberg C, Storek D, Dammann F, Vonthein R, et al. The value of SPET/CT in chronic osteomyelitis. Eur J Nucl Med Mol Imaging 2003;30:1665–73.
Filippi L, Schillaci O. Usefulness of hybrid SPECT/CT in 99mTc-HMPAO-labeled leukocyte scintigraphy for bone and joint infections. J Nucl Med 2006;47:1908–13.
de Winter F, Vogelaers D, Gemmel F, Dierckx RA. Promising role of 18-F-fluoro-D-deoxyglucose positron emission tomography in clinical infectious diseases. Eur J Clin Microbiol Infect Dis 2002;21:247–57.
Guhlmann A, Brecht-Krauss D, Suger G, Glatting G, Kotzerke J, Kinzl L, et al. Chronic osteomyelitis: detection with FDG PET and correlation with histopathologic findings. Radiology 1998;206:749–54.
de Winter F, van de Wiele C, Vogelaers D, de Smet K, Verdonk R, Dierckx RA. Fluorine-18 fluorodeoxyglucose-position emission tomography: a highly accurate imaging modality for the diagnosis of chronic musculoskeletal infections. J Bone Joint Surg Am 2001;83-A:651–60.
Zhuang H, Yang H, Alavi A. Critical role of 18F-labeled fluorodeoxyglucose PET in the management of patients with arthroplasty. Radiol Clin North Am 2007;45:711–8. vii.
Zhuang H, Duarte PS, Pourdehnad M, Maes A, Van Acker F, Shnier D, et al. The promising role of 18F-FDG PET in detecting infected lower limb prosthesis implants. J Nucl Med 2001;42:44–8.
Zhuang H, Chacko TK, Hickeson M, Stevenson K, Feng Q, Ponzo F, et al. Persistent non-specific FDG uptake on PET imaging following hip arthroplasty. Eur J Nucl Med Mol Imaging 2002;29:1328–33.
Delank KS, Schmidt M, Michael JW, Dietlein M, Schicha H, Eysel P. The implications of 18F-FDG PET for the diagnosis of endoprosthetic loosening and infection in hip and knee arthroplasty: results from a prospective, blinded study. BMC Musculoskelet Disord 2006;7:20.
Stumpe KD, Romero J, Ziegler O, Kamel EM, von Schulthess GK, Strobel K, et al. The value of FDG-PET in patients with painful total knee arthroplasty. Eur J Nucl Med Mol Imaging 2006;33:1218–25.
Pill SG, Parvizi J, Tang PH, Garino JP, Nelson C, Zhuang H, et al. Comparison of fluorodeoxyglucose positron emission tomography and (111)indium-white blood cell imaging in the diagnosis of periprosthetic infection of the hip. J Arthroplasty 2006;21:91–7.
García-Barrecheguren E, Rodríguez FM, Toledo Santana G, Valentí Nín JR, Richter Echevarría JA FDG-PET: a new diagnostic approach in hip prosthetic replacement. Rev Esp Med Nucl 2007;26:208–20.
Kumar V. Radiolabeled white blood cells and direct targeting of micro-organisms for infection imaging. Q J Nucl Med Mol Imaging 2005;49:325–38.
Bleeker-Rovers CP, Rennen HJ, Boerman OC, Wymenga AB, Visser EP, Bakker JH, et al. 99mTc-labeled interleukin 8 for the scintigraphic detection of infection and inflammation: first clinical evaluation. J Nucl Med 2007;48:337–43.
Hnatowich DJ, Virzi F, Rusckowski M. Investigations of avidin and biotin for imaging applications. J Nucl Med 1987;28:1294–302.
Shoup TM, Fischman AJ, Jaywook S, Babich JW, Strauss HW, Elmaleh DR. Synthesis of fluorine-18-labeled biotin derivatives: biodistribution and infection localization. J Nucl Med 1994;35:1685–90.
Erba PA, Cataldi AG, Tascini C, Leonildi A, Manfredi C, Mariani G, et al. 111In-DTPA-Biotin uptake by Staphylococcus aureus. Nucl Med Commun 2010;31:994–7.
Lazzeri E, Erba P, Perri M, Tascini C, Doria R, Giorgetti J, et al. Scintigraphic imaging of vertebral osteomyelitis with 111in-biotin. Spine (Phila Pa 1976) 2008;33:E198–204.
Lorberboym M, Feldbrin Z, Hendel D, Blankenberg FG, Schachter P. The use of 99mTc-recombinant human annexin V imaging for differential diagnosis of aseptic loosening and low-grade infection in hip and knee prostheses. J Nucl Med 2009;50:534–7.
Buscombe JR. The future of infection imaging. Q J Nucl Med Mol Imaging 2006;50:99–103.
Vinjamuri S, Hall AV, Solanki KK, Bomanji J, Siraj Q, O’Shaughnessy E, et al. Comparison of 99mTc infecton imaging with radiolabelled white-cell imaging in the evaluation of bacterial infection. Lancet 1996;347:233–5.
Sonmezoglu K, Sonmezoglu M, Halac M, Akgün I, Türkmen C, Onsel C, et al. Usefulness of 99mTc-ciprofloxacin (infecton) scan in diagnosis of chronic orthopedic infections: comparative study with 99mTc-HMPAO leukocyte scintigraphy. J Nucl Med 2001;42:567–74.
Larikka MJ, Ahonen AK, Niemelä O, Junila JA, Hämäläinen MM, Britton K, et al. Comparison of 99mTc ciprofloxacin, 99mTc white blood cell and three-phase bone imaging in the diagnosis of hip prosthesis infections: improved diagnostic accuracy with extended imaging time. Nucl Med Commun 2002;23:655–61.
Larikka MJ, Ahonen AK, Niemelä O, Puronto O, Junila JA, Hämäläinen MM, et al. 99m Tc-ciprofloxacin (Infecton) imaging in the diagnosis of knee prosthesis infections. Nucl Med Commun 2002;23:167–70.
Sarda L, Saleh-Mghir A, Peker C, Meulemans A, Crémieux AC, Le Guludec D. Evaluation of (99m)Tc-ciprofloxacin scintigraphy in a rabbit model of Staphylococcus aureus prosthetic joint infection. J Nucl Med 2002;43:239–45.
Dumarey N, Blocklet D, Appelboom T, Tant L, Schoutens A. Infecton is not specific for bacterial osteo-articular infective pathology. Eur J Nucl Med Mol Imaging 2002;29:530–5.
Sarda L, Crémieux AC, Lebellec Y, Meulemans A, Lebtahi R, Hayem G, et al. Inability of 99mTc-ciprofloxacin scintigraphy to discriminate between septic and sterile osteoarticular diseases. J Nucl Med 2003;44:920–6.
Langer O, Brunner M, Zeitlinger M, Ziegler S, Müller U, Dobrozemsky G, et al. In vitro and in vivo evaluation of [18F]ciprofloxacin for the imaging of bacterial infections with PET. Eur J Nucl Med Mol Imaging 2005;32:143–50.
Fuster D, Soriano A, Garcia S, Piera C, Suades J, Rodríguez D, et al. Usefulness of 99mTc-ciprofloxacin scintigraphy in the diagnosis of prosthetic joint infections. Nucl Med Commun 2011;32:44–51.
Nibbering PH, Welling MM, van den Broek PJ, van Wyngaarden KE, Pauwels EK, Calame W. Radiolabelled antimicrobial peptides for imaging of infections: a review. Nucl Med Commun 1998;19:1117–21.
Lupetti A, Welling MM, Pauwels EK, Nibbering PH. Radiolabelled antimicrobial peptides for infection detection. Lancet Infect Dis 2003;3:223–9.
Welling MM, Lupetti A, Balter HS, Lanzzeri S, Souto B, Rey AM, et al. 99mTc-labeled antimicrobial peptides for detection of bacterial and Candida albicans infections. J Nucl Med 2001;42:788–94.
Nibbering PH, Welling MM, Paulusma-Annema A, Brouwer CP, Lupetti A, Pauwels EK. 99mTc-Labeled UBI 29-41 peptide for monitoring the efficacy of antibacterial agents in mice infected with Staphylococcus aureus. J Nucl Med 2004;45:321–6.
Sarda-Mantel L, Saleh-Mghir A, Welling MM, Meulemans A, Vrigneaud JM, Raguin O, et al. Evaluation of 99mTc-UBI 29-41 scintigraphy for specific detection of experimental Staphylococcus aureus prosthetic joint infections. Eur J Nucl Med Mol Imaging 2007;34:1302–9.
Akhtar MS, Khan ME, Khan B, Irfanullah J, Afzal MS, Khan MA, et al. An imaging analysis of (99m)Tc-UBI (29-41) uptake in S. aureus infected thighs of rabbits on ciprofloxacin treatment. Eur J Nucl Med Mol Imaging 2008;35:1056–64.
Salber D, Gunawan J, Langen KJ, Fricke E, Klauth P, Burchert W, et al. Comparison of 99mTc- and 18F-ubiquicidin autoradiography to anti-Staphylococcus aureus immunofluorescence in rat muscle abscesses. J Nucl Med 2008;49:995–9.
Brouwer CP, Gemmel FF, Welling MM. Evaluation of 99mTc-UBI 29-41 scintigraphy for specific detection of experimental multidrug-resistant Staphylococcus aureus bacterial endocarditis. Q J Nucl Med Mol Imaging 2010;54:442–50.
Arteaga de Murphy C, Gemmel F, Balter J. Clinical trial of specific imaging of infections. Nucl Med Commun 2010;31:726–33.
Rusckowski M, Gupta S, Liu G, Dou S, Hnatowich DJ. Investigations of a (99m)Tc-labeled bacteriophage as a potential infection-specific imaging agent. J Nucl Med 2004;45:1201–8.
Rusckowski M, Gupta S, Liu G, Dou S, Hnatowich DJ. Investigation of four (99m)Tc-labeled bacteriophages for infection-specific imaging. Nucl Med Biol 2008;35:433–40.
Diaz Jr LA, Foss CA, Thornton K, Nimmagadda S, Endres CJ, Uzuner O, et al. Imaging of musculoskeletal bacterial infections by [124I]FIAU-PET/CT. PLoS One 2007;2:e1007.
Lazzeri E, Erba P, Perri M, Doria R, Tascini C, Mariani G. Clinical impact of SPECT/CT with In-111 biotin on the management of patients with suspected spine infection. Clin Nucl Med 2010;35:12–7.
Graute V, Feist M, Lehner S, Haug A, Müller PE, Bartenstein P, et al. Detection of low-grade prosthetic joint infections using 99mTc-antigranulocyte SPECT/CT: initial clinical results. Eur J Nucl Med Mol Imaging 2010;37:1751–9.
Chen SH, Ho KC, Hsieh PH, Lee MS, Yen TC. Potential clinical role of 18F FDG-PET/CT in detecting hip prosthesis infection: a study in patients undergoing two-stage revision arthroplasty with an interim spacer. Q J Nucl Med Mol Imaging 2010;54:429–35.
Dumarey N, Egrise D, Blocklet D, Stallenberg B, Remmelink M, del Marmol V, et al. Imaging infection with 18F-FDG-labeled leukocyte PET/CT: initial experience in 21 patients. J Nucl Med 2006;47:625–32.
Rini JN, Palestro CJ. Imaging of infection and inflammation with 18F-FDG-labeled leukocytes. Q J Nucl Med Mol Imaging 2006;50:143–6.
Rini JN, Bhargava KK, Tronco GG, Singer C, Caprioli R, Marwin SE, et al. PET with FDG-labeled leukocytes versus scintigraphy with 111In-oxine-labeled leukocytes for detection of infection. Radiology 2006;238:978–87.
Bhargava KK, Gupta RK, Nichols KJ, Palestro CJ. In vitro human leukocyte labeling with (64)Cu: an intraindividual comparison with (111)In-oxine and (18)F-FDG. Nucl Med Biol 2009;36:545–9.
Sterner T, Pink R, Freudenberg L, Jentzen T, Quitmann H, Bockisch A, et al. The role of [18F]fluoride positron emission tomography in the early detection of aseptic loosening of total knee arthroplasty. Int J Surg 2007;5:99–104.
Kobayashi N, Inaba Y, Choe H, Ike H, Fujimaki H, Tezuka T, et al. Use of F-18 fluoride PET to differentiate septic from aseptic loosening in total hip arthroplasty patients. Clin Nucl Med 2011;36:e156–61.
Kropholler MA, Boellaard R, Elzinga EH, van der Laken CJ, Maruyama K, Kloet RW, et al. Quantification of (R)-[11C]PK11195 binding in rheumatoid arthritis. Eur J Nucl Med Mol Imaging 2009;36:624–31.
Mäkinen TJ, Lankinen P, Pöyhönen T, Jalava J, Aro HT, Roivainen A. Comparison of 18F-FDG and 68Ga PET imaging in the assessment of experimental osteomyelitis due to Staphylococcus aureus. Eur J Nucl Med Mol Imaging 2005;32:1259–68.
Lankinen P, Mäkinen TJ, Pöyhönen TA, Virsu P, Salomäki S, Hakanen AJ, et al. (68)Ga-DOTAVAP-P1 PET imaging capable of demonstrating the phase of inflammation in healing bones and the progress of infection in osteomyelitic bones. Eur J Nucl Med Mol Imaging 2008;35:352–64.
Ujula T, Salomäki S, Virsu P, Lankinen P, Mäkinen TJ, Autio A, et al. Synthesis, 68Ga labeling and preliminary evaluation of DOTA peptide binding vascular adhesion protein-1: a potential PET imaging agent for diagnosing osteomyelitis. Nucl Med Biol 2009;36:631–41.
Kwee TC, Kwee RM, Alavi A. FDG-PET for diagnosing prosthetic joint infection: systematic review and metaanalysis. Eur J Nucl Med Mol Imaging 2008;35:2122–32.
van der Bruggen W, Bleeker-Rovers CP, Boerman OC, Gotthardt M, Oyen WJ. PET and SPECT in osteomyelitis and prosthetic bone and joint infections: a systematic review. Semin Nucl Med 2010;40:3–15.
Gemmel F, Dumarey N, Welling M. Future diagnostic agents. Semin Nucl Med 2009;39:11–26.
Del Pozo JL, Patel R. Infection associated with prosthetic joints. N Engl J Med 2009;361:787–94.
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Gemmel, F., Van den Wyngaert, H., Love, C. et al. Prosthetic joint infections: radionuclide state-of-the-art imaging. Eur J Nucl Med Mol Imaging 39, 892–909 (2012). https://doi.org/10.1007/s00259-012-2062-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00259-012-2062-7