Abstract
In the past few years, the introduction of novel PET tracers labelled with 68Ga has changed the diagnostic approach to neuroendocrine tumours (NET) in specialized centres. Although somatostatin analogue tracers labelled with 111In have represented the gold standard imaging modality for NET detection in past decades, the advantages offered by both labelling somatostatin analogues with 68Ga and using PET/CT tomography for image acquisition, account for the increasing use of these tracers in clinical practice. There are an increasing number of reports of the higher accuracy of 68Ga-DOTA peptide PET/CT for the detection of NET lesions as compared to morphological imaging procedures and somatostatin receptor scintigraphy. Moreover, the use of 68Ga-DOTA peptides offers the possibility to noninvasively evaluate NET cells for the presence of somatostatin receptor expression, with direct therapeutic implications. Several practical advantages also favour the use of 68Ga-DOTA peptides including the relatively easy and economic synthesis process and the fact that 68Ga labelling can be performed in centres without an on-site cyclotron. We describe the advantages and limitations of 68Ga-DOTA peptide PET/CT imaging for the assessment of gastroenteropancreatic NET referring to the available literature as well as to our experience, and finally highlight potential future perspectives.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Neuroendocrine tumours (NET) have historically been considered as rare tumours [1, 2]; however, recent incidence estimates suggest that they are more common than might be expected. An analysis of the Surveillance, Epidemiology, and End Results (SEER) database indicates an increase in the reported annual age-adjusted incidence of NETs from 1973 (1.09/100,000) to 2004 (5.25/100,000) [3].
Originating from neuroendocrine cells deriving from the neural crest [4], NET may arise in diverse anatomic locations and may be associated with symptoms resulting from the secretion of hormones or vasoactive peptides into the bloodstream. Based on the presence of hormone-related syndromes, NET may be classified into functional (33–50% of patients) and non-functional forms. Being part of the amine precursor uptake and decarboxylation cell system, NET can produce a large variety of substances since they take up, accumulate and decarboxylate amine precursors such as dihydroxy-phenylalanine (DOPA) and hydroxyl-tryptophane. Another typical feature of neuroendocrine cells is the expression of several receptors in high quantities [4].
Although NET may arise virtually anywhere in the human body, the most common location of NET primary lesions is the gastroenteropancreatic (GEP) tract, followed by the lungs. Less frequent sites include the skin, the adrenal glands, the thyroid and the genital tract [5]. Traditionally, GEP NET were classified based on their origin in the foregut (pancreas, stomach, duodenum), midgut (ileum, appendix) or hindgut (colon, rectum). However, the European Neuroendocrine Tumour Society and the American Joint Committee on Cancer have proposed also using the TNM staging system for NET of the foregut, midgut and hindgut [6, 7]. The use Ki67 levels to define the histological grade of NET has been proposed: low grade (grade 1), Ki67 <2%; intermediate grade (grade 2), Ki67 3% to 20%; high grade (grade 3), Ki67 >20% [6, 7]. The International Association for the Study of Lung Cancer has also recently recommended the use of the TNM staging system for pulmonary NET [8].
The small size of NET, their variable anatomical location and the slow metabolic rate of well-differentiated forms, have limited their detection using different imaging procedures. Traditionally, NET diagnostic work-up included morphological imaging procedures such as computed tomography (CT), ultrasonography (US) and magnetic resonance imaging (MRI) combined with functional imaging, namely whole-body somatostatin receptor scintigraphy (SRS) [9, 10]. As described by Chiti et al. in this issue, the introduction of SRS represented a milestone in the NET diagnostic flow-chart. In a study analysing more than 1,000 patients, Krenning et al. observed a higher accuracy of SRS as compared to other morphological imaging modalities [11] for the detection of both primary NET and their metastatic lesions.
Despite the high accuracy of SRS for the detection of NET, the recent introduction of novel somatostatin analogues labelled with 68Ga (68Ga-DOTA peptides) has completely revolutionized the traditional diagnostic approach to NET in specialized centres in Europe. The use of 68Ga-DOTA peptide PET/CT offers several advantages over SRS. From a technical point of view, the synthesis of 68Ga-DOTA peptides is relatively easy and economical, and can also be performed in centres without an on-site cyclotron. PET/CT imaging is less time-consuming than SRS (2 hours, instead of the 4 plus 24 hours acquisition). The possibility to semiquantify the activity in a given region of interest is another potential advantage of PET scanning over SRS and the SUVmax has recently been reported to be a prognostic factor [12]. Moreover, among the other advantages is the higher spatial resolution of the PET tomograph as compared to the gamma camera, providing better visualization of small lesions (<10 mm).
The synthesis of specific PET tracers for NET imaging has been pursued mainly as a consequence of the marginal role of FDG for the visualization of well-differentiated NET [13] and because of the difficulties in the synthesis of other PET tracers for NET imaging (e.g. 18F-DOPA).
68Ga-DOTA peptides are a group of PET tracers that specifically bind to somatostatin receptors (SST) that are over-expressed on NET cells. SST are G-protein-coupled receptors and are internalized after specific ligand binding [14], and six different types have been identified (SST1, 2A, 2B, 3, 4 and 5) in humans. Structurally 68Ga-DOTA peptides are made of an active part directly binding to SST (TOC, NOC, TATE), a chelate (DOTA) and the beta-emitting isotope (68Ga). The main difference among the various tracers (DOTA-TOC, DOTA-NOC, DOTA-TATE) is the variable affinity to SST subtypes [15]: while all can bind to SST2 and SST5, only DOTA-NOC also shows good affinity for SST3. However, there is currently no evidence of a clinical impact of these differences in receptor binding affinity, and therefore there is no indication suggesting the preferential use of one compound over the others. The labelling with 68Ga also presents advantages over other employed isotopes as reported by Antunes et al. [15] and DeCristoforo in this issue.
From the time of their first use in humans, the use of 68Ga-DOTA peptides has increased exponentially, and the number of papers describing their use in patients with NET has risen considerably in the past few years. At present, their use is limited to clinical trials in specialized centres.
68Ga-DOTA peptide synthesis
From a technical point of view, the synthesis process is relatively easy: 68Ga can be easily eluted from a commercially available 68Ge/68Ga generator without the need for an on-site cyclotron. The long half-life of the mother radionuclide 68Ge (270.8 days) makes it possible to use the generator for approximately 9–12 months depending on requirements. 68Ga (half-life 68 min) is a positron emitter with 89% positron emission and negligible gamma emission (1,077 keV) of 3.2% only. For labelling, the 68Ga eluate is first concentrated and purified using a microchromatography method [16]. Radiolabelling yields of >95% can usually be achieved within 15 min.
PET/CT imaging protocol using 68Ga-DOTA peptides
PET/CT image acquisition using 68Ga-DOTA peptides has recently been standardized [17]. PET/CT image acquisition starts at 60 min after intravenous injection of approximately 100 MBq (75–250 MBq) of the chosen radiolabelled peptide (68Ga-DOTA-TOC, 68Ga-DOTA-NOC, 68Ga-DOTA-TATE). The amount of injected radioactivity strictly depends on the daily production of the generator for each single elution (usually in the range 300–700 MBq), by the tomograph characteristics (the use of 3-D tomographs is recommended) and, of course, by the number of patients scanned per day. The discontinuation of somatostatin analogue treatment before the PET/CT scan is not mandatory and no clear evidence supports the need for discontinuing their use before scanning.
Considering that SST are widely dispersed within the human body, different organs may be imaged using 68Ga-DOTA peptides, including the liver, spleen, pituitary, thyroid, kidneys, adrenal glands, salivary glands, stomach wall and bowel. A potential pitfall in image interpretation is represented by the uptake of tracer in the pancreatic head. Tracer uptake in the exocrine pancreas (head) has been reported to be a relatively frequent finding (Gabriel et al. [18] with DOTA-TOC, 67.8%; Castellucci et al. [19] with DOTA-NOC, 31%) and is not necessarily associated with the presence of active disease. Its clinical significance, however, as well as the detailed mechanism of uptake in the pancreatic head, are still unclear. Among the causes of potential pitfalls in image interpretation, inflammation needs to be considered, since SST are expressed on activated lymphocytes, and therefore 68Ga-DOTA peptides may be falsely positive in inflamed areas. Moreover, an accessory spleen or physiological activity at the adrenal level may be other causes of false-positive reports.
Clinical use of 68Ga-DOTA peptides in GEP NET
As stated above, several papers report the higher diagnostic accuracy of 68Ga-DOTA peptide PET/CT as compared to conventional imaging procedures, SRS and other metabolic PET tracers used for NET imaging (18F-DOPA, 18F-FDG). However, most studies have included both patients with GEP and patients with non-GEP tumours, reporting overall sensitivity values. Indications for performing 68Ga-DOTA peptide studies in patients with GEP NET include: staging, restaging after surgery or therapy, identification of the site of the unknown primary tumour in patients with proven NET secondary lesions, and selection of patients eligible for therapy with either cold or hot (peptide receptor radionuclide therapy) somatostatin analogues.
The following discussion covers the most commonly employed DOTA peptides in clinical practice: 68Ga-DOTA-TOC, 68Ga-DOTA-NOC and 68Ga-DOTA-TATE.
68Ga-DOTA-TOC in GEP NET
The first 68Ga-DOTA peptide to be used in patients with NET was 68Ga-DOTA-TOC. Several studies showed a high tumour to non-tumour contrast and a higher sensitivity of 68Ga-DOTA-TOC PET/CT as compared to SRS [20, 21]. Hofmann et al. described a population of eight patients with pathologically proven NET (six with a GEP NET primary), and observed overall sensitivity for tumour detection with DOTA-TOC of 100% as compared to 85% of SRS [20]. The study with the largest patient population (84 patients with NET; 53 with a documented GEP primary) showed overall higher sensitivity (97%) for DOTA-TOC PET compared to CT (61%) and SRS (52%) for the detection of NET lesions, especially in patients with small tumours at the nodal or bone level [18]. The accuracy of 68Ga-DOTA-TOC for the detection of bone lesions was further investigated in detail in a recent study that compared PET data with conventional imaging findings and bone scintigraphy. In 51 patients with well-differentiated NET (35 with a GEP primary), PET with 68Ga-DOTA-TOC performed better than CT and bone scintigraphy for the early detection of secondary lesions in bones (sensitivity 97%, specificity 92%) [22].
68Ga-DOTA-NOC in GEP NET
68Ga-DOTA-NOC is also increasingly used in several centres in Europe and worldwide. DOTA-NOC shows good affinity not only for SST2 and SST5, but also (in contrast to DOTA-TOC) for SST3 [15]. Moreover, 68Ga-DOTA-NOC has been reported to have a more favourable dosimetry [23]. Similar to 68Ga-DOTA-TOC, 68Ga-DOTA-NOC has also been reported to show higher accuracy for the detection of NET lesions than both conventional imaging and SRS. In particular, 68Ga-DOTA-NOC shows good sensitivity for the visualization of small lesions, particularly at the nodal and bone levels [24], or in patients with an unusual anatomical location [25]. Fanti et al. reported that 68Ga-DOTA-NOC can be used for the evaluation of NET with uncommon presentations including tumours of the uterus, prostate, ovary, kidney, breast and ear, and paraganglioma [25].
Since NET may often present as lesions with small dimensions and may arise virtually anywhere in the human body, the detection of the primary tumour site in patients with proven NET secondary lesions is challenging for the clinician. In fact morphological conventional imaging procedures and SRS often fail to identify the primary tumour site. In a population of 59 patients, 68Ga-DOTA-NOC PET/CT was able to detect of the primary tumour in 35 patients with cancer of unknown primary (CUP; in 32 of the 35, the primary was a GEP tumour), with an overall detection rate of 59% [26].
Of course, the introduction of a more sensitive imaging procedure (such as PET/CT with 68Ga-DOTA peptides), although very appealing for both researchers and clinicians, may not always have a direct impact on the clinical management of patients. In fact in most patients the detection of a higher number of metastatic lesions in comparison to morphological imaging or SRS is not followed by a change in the therapeutic approach. On the contrary, the detection of unsuspected metastatic spread or local relapse, the identification of the site of the occult primary tumour or the confirmation or exclusion of SSR expression on tumour cells are all conditions that can modify the therapeutic approach. The clinical impact of DOTA-NOC PET/CT was evaluated in a population of 90 NET patients (62 with a GEP primary) [27], and overall the PET/CT findings affected either stage classification or therapy modifications in half the patients. It is interesting to note that as a consequence of being a receptor-based tracer, the most frequent clinical setting in which PET provided an impact on management was the therapeutic approach (initiation/continuation of hot or cold somatostatin analogues, in 36 of the 90 patients) followed by surgical indication/exclusion. Less frequent impacts on management included the initiation of radiotherapy, further diagnostic investigation and liver transplantation [25].
At present, 68Ga-DOTA-NOC is the only tracer studied with the aim of defining PET/CT-derived parameters to predict patient outcome. In fact the observations that well-differentiated NET show a slower growth rate, higher SST expression, higher 68Ga-DOTA-NOC uptake, higher response rate to somatostatin analogues and better outcome, have raised the issues of whether it is possible to define SUVmax values that may predict a more favourable outcome. In a population of 47 patients with NET (41 with a GEP primary), 68Ga-DOTA-NOC PET/CT SUVmax values were found to provide prognostic information [12]: patients with stable disease or partial response showed significantly higher SUVmax than those with progressive disease. In particular, the best SUVmax cut-off to differentiate between these two groups of patients was reported to range between 17.6 and 19.3 (SUVmax values higher than 19.3 permitted the selection of patients with slower disease progression). Interestingly the authors also reported higher SUVmax values in patients with a pancreatic primary as compared to those with other primary locations.
68Ga-DOTA-TATE in GEP NET
Compared to other 68Ga-DOTA peptides, 68Ga-DOTA-TATE shows an extremely selective affinity for SST2 [15, 28], the most common SST subtype on NET cells. Similar to 68Ga-DOTA-TOC and 68Ga-DOTA-NOC, 68Ga-DOTA-TATE has also been reported to be superior to SRS for NET lesion detection. In a population of 51 NET patients (37 with a GEP primary) with either negative (35) or equivocal (16) SRS, 68Ga-DOTA-TATE PET/CT identified significantly more lesions than SRS with a change in management in 36 patients [29].
Comparative studies: 68Ga-DOTA peptides vs. other PET tracers for NET detection
Considering the complex biology of NET cells, several compounds have been proposed for the imaging of NET. The most commonly used metabolic tracer to study well-differentiated NET is 18F-DOPA. To our knowledge there is only one study involving a direct comparison between 68Ga-DOTA-NOC and 18F-DOPA. In a limited patient population (13 patients, 11 with a GEP primary) a higher detection rate was found for 68Ga-DOTA-NOC [30]. Similarly, in a population of 25 patients (14 with a GEP primary), 68Ga-DOTA-TATE showed 54 out of 55 NET lesions in contrast to 29 lesions with 18F-DOPA (sensitivity 96% vs. 56%) [31].
18F-FDG may also play a role in the detection of NET lesions. Although the role of FDG is limited by the slow metabolic rate of NET cells, it should be remembered that NET may show variable degrees of differentiation between patients, in different lesions in the same patient and within different areas of the same tumour [32]. The detection of FDG uptake in lesions is clinically relevant since it depicts the presence of less-differentiated tumour cells that are associated with a worse prognosis and require a different therapeutic approach, including systemic chemotherapy. A few studies have compared the differential uptake patters of DOTA peptides (DOTA-TOC and DOTA-TATE) and FDG in non-GEP NET (lung NET and medullary thyroid carcinoma). Although the detailed analysis of non-GEP NET is beyond the scope of this review, it is relevant to observe that in non-GEP NET high uptake of 68Ga-DOTA peptides is seen in low-grade NET, while FDG uptake is seen in high-grade tumours [33, 34]. From a clinical point of view, 18F-FDG may be considered superior to 68Ga-DOTA peptides in patients with low-differentiated NET (low SST expression) or in forms of NET characterized by a low expression of SST (e.g. medullary thyroid carcinoma).
Our experience in more than 1,000 patients with NET studied by 68Ga-DOTA-NOC PET/CT
Krenning et al. [11] reported their experience on the use of SRS in more than 1,000 patients with NET, stating the many advantages of using SRS over CT. Although the introduction of PET/CT with 68Ga-DOTA peptides certainly represents a major advance in the diagnostic approach to patients with NET, offering higher accuracy for NET lesion detection and technical advantages, the role of SRS still needs to be underlined. Currently there is no evidence supporting the clinical advantages of performing PET/CT with 68Ga-DOTA peptides in patients with NET and an existing pathological SRS-documented metastatic disease. The presence of equivocal or negative SRS raises the issue as to whether it is appropriate to perform PET/CT with 68Ga-DOTA peptides in order to exclude (or confirm) the presence of lesions under 10 mm or to better investigate areas where octreotide physiologically shows a higher uptake (e.g. liver and bowel). It is easier to draw conclusions as to whether a technique is appropriate or not when dealing with a large patient population. Therefore, similar to the Rotterdam group, we decided to include a brief summary of the results we obtained using 68Ga-DOTA-NOC PET/CT at our centre in order to provide data on a large population of patients with NET.
In February 2007, we introduced 68Ga-DOTA-NOC PET/CT scanning as part of the diagnostic work-up of NET patients. All patients with NET were included in a study protocol to assess the accuracy of 68Ga-DOTA-NOC PET/CT for NET lesion detection. In particular, in all patients, data regarding the pathological confirmation of NET, conventional imaging studies (performed within a month of the PET/CT scan), laboratory data and clinical follow-up were recorded. In consideration of the very good results obtained in terms of diagnostic accuracy, economic burden and patient compliance, our Institution decided to discontinue SRS at the end of 2007 in favour of 68Ga-DOTA-NOC PET/CT. The study protocol for 68Ga-DOTA-NOC PET/CT in NET patients was approved by the local ethics committee. At the time of this report the study was on-going, and therefore still collecting data regarding both new patients with NET and clinical and imaging follow-up information following older studies.
Overall, we have studied 1,239 patients with either pathologically proven or suspected NET by 68Ga-DOTA-NOC PET/CT. Pathological confirmation was obtained by either surgical (819 of the 1,239 patients) or biopsy specimens (308 of 1239) while in 112 patients no tumour could be identified (108 suspected NET, 4 equivocal SRS). In the majority of patients (Table 1), the primary tumour arose from the GEP tract (670 patients, 54.1%) while among the patients with non-GEP NET (311, 25.1%), the lung was the most frequent primary site (158, 12.8%). Genetic syndromes accounted for the tumour in only a minority of the studied patients, including 62 with multiple endocrine neoplasia (MEN) and 3 with von Hippel-Lindau syndrome, while in 81 patients with CUP (6.5%) the site of the primary tumour could not be identified. Finally, in the remaining 112 patients studied for suspicion of NET, the presence of tumour was not confirmed either by PET or on follow-up.
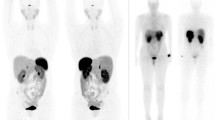
Indications for performing PET/CT (Table 2) included staging (Figs. 1 and 2), restaging (after surgery or therapy), identification of the site of the primary tumour, screening in MEN, equivocal conventional imaging, equivocal SRS, follow-up, suspected relapse or suspected NET.
Considering all patients (Table 3), PET was positive in 655, negative in 576 and equivocal in 8. Comparing the results with conventional imaging and follow-up data, 68Ga-DOTA-NOC PET/CT was true-positive in 652, true-negative in 524, false-positive in 9 and false-negative in 54 patients. Overall (Table 2), 68Ga-DOTA-NOC PET/CT showed good sensitivity (92%) and specificity (98%) for the detection of NET. The mean SUVmax of positive lesions was 22.8 ± 18.6 [2.2-150.0].
The most frequent cause of the false-positive PET findings (9 patients) was the presence of inflammation due to the expression of SST on activated lymphocytes. The causes of the false-negative PET findings (54 patients) included lesion size under 5 mm (14 patients; 7 gastric, 3 lung, 1 idiopathic diffuse neuroendocrine cell hyperplasia, 1 liver, 1 Merkel cell, 1 pancreas), lesions at sites of physiological 68Ga-DOTA-NOC uptake (6 pancreatic head, 1 pituitary), factors related to tumour biological characteristics that would account for low/variable SST expression (1 insulinoma, 1 phaeochromocytoma, and 10 moderate to low differentiation NET, including small cell lung cancer). In the remaining 21 patients studied for CUP, PET was negative and the site of the primary could not be identified. We frequently observed focal 68Ga-DOTA-NOC uptake at the head of the pancreas (56 patients, 4.5%) not related to the presence of tumour.
In our series, 68Ga-DOTA-NOC PET/CT was useful for the detection of the site of the primary tumour in patients with documented secondary NET lesions (Fig. 3). Among 105 patients studied for CUP, PET/CT allowed the detection of the primary tumour site in 24 (22.8%), confirmed the presence of secondary lesions in 60 but did not show the primary site, and was false-negative in 21.
68Ga-DOTA-NOC PET/CT images in a patient with multiple secondary NET lesions in the liver studied to identify the unknown primary site. A focal area of tracer uptake in the duodenum (SUVmax 17) is compatible with the primary tumour site. Multiple areas of uptake at the liver and nodal (paracaval) levels are also shown. Surgical excision of the identified primary lesion provided confirmation of the PET findings
Among the patients studied for suspected NET or suspected relapse, when the suspicion arose from the detection of increased levels of biochemical markers alone (66 and 22 patients, respectively), the majority of patients were true-negative (64 of 66 and 16 of 22, respectively). A high rate of true-negative results was also seen in patients presenting with chronic diarrhoea alone (4 of 5).
Conclusions and future perspectives on 68Ga-DOTA peptides PET/CT
68Ga-DOTA peptides PET/CT is increasingly used for the assessment of patients with well-differentiated NET in specialized centres in Europe. Several studies have shown the higher accuracy of 68Ga-DOTA peptides for the detection of NET lesions as compared to both conventional imaging and SRS. The advantages of the use of 68Ga-DOTA peptides are not merely limited to a better overall accuracy but also to the fact that they provide valuable data regarding the pattern of expression of SST on target lesions, which represents a useful non-invasive modality to select patients for therapy with either hot or cold somatostatin analogues. From a technical point of view it is also worth mentioning the relatively easy and economical synthetic process of these compounds that renders them suitable for use even in small centres without an on-site cyclotron.
The potential association of 68Ga-DOTA peptide PET/CT with PET/CT using metabolic tracers may prove valuable in patients presenting with intermediate- to high-grade tumours (18F-FDG) or for assessing response to therapy (18F-DOPA). However, further data are needed to further elucidate the role of the integrated use of metabolic and receptor-targeted tracers in the clinical management of patients with NET.
Considering the expression of a wide range of receptors on the surface of NET cells, further studies are needed to ascertain whether the use of alternative radiolabelled ligands, currently used only in the preclinical setting, may provide additional value in the management of patients with NET.
References
Modlin IM, Kidd M, Latich I, Zikusoka MN, Shapiro MD. Current status of gastrointestinal carcinoids. Gastroenterology. 2005;128(6):1717–51.
Taal BG, Visser O. Epidemiology of neuroendocrine tumours. Neuroendocrinology. 2004;80 Suppl 1:3–7.
Yao JC, Hassan M, Phan A, Dagohoy C, Leary C, Mares JE, et al. One hundred years after "carcinoid": epidemiology of and prognostic factors for neuroendocrine tumors in 35,825 cases in the United States. J Clin Oncol. 2008;26(18):3063–72.
Reubi JC. Neuropeptide receptors in health and disease: the molecular basis for in vivo imaging. J Nucl Med. 1995;36:1825–35.
Jensen RT. Endocrine tumors of the gastrointestinal tract and pancreas. In: Kasper DL, Braunwald E, Fauci AS, Hauser SL, Longo DL, Jameson JL, editors. Harrison’s principles of internal medicine. 16th ed. New York: McGraw-Hill; 2005. p. 2220–31
Rindi G, Klöppel G, Alhman H, Caplin M, Couvelard A, de Herder WW, et al. TNM staging of foregut (neuro)endocrine tumors: a consensus proposal including a grading system. Virchows Arch. 2006;449(4):395–401.
Rindi G, Klöppel G, Couvelard A, Komminoth P, Körner M, Lopes JM, et al. TNM staging of midgut and hindgut (neuro) endocrine tumors: a consensus proposal including a grading system. Virchows Arch. 2007;451(4):757–62.
Travis WD, IASLC Staging Committee. Reporting lung cancer pathology specimens. Impact of the anticipated 7th edition TNM classification based on recommendations of the IASLC Staging Committee. Histopathology. 2009;54(1):3–11.
Sundin A, Garske U, Orlefors H. Nuclear imaging of neuroendocrine tumours. Best Pract Res Clin Endocrinol Metab. 2007;21(1):69–85.
Ramage JK, Davies AH, Ardill J, Bax N, Caplin M, Grossman A, et al. Guidelines for the management of gastroenteropancreatic neuroendocrine (including carcinoid) tumours. Gut. 2005;54 Suppl 4:iv1–16.
Krenning EP, Kwekkeboom DJ, Bakker WH, Breeman WA, Kooij PP, Oei HY, et al. Somatostatin receptor scintigraphy with [111In-DTPA-D-Phe1]- and [123I-Tyr3]-octreotide: the Rotterdam experience with more than 1000 patients. Eur J Nucl Med. 1993;20(8):716–31.
Campana D, Ambrosini V, Pezzilli R, Fanti S, Labate AM, Santini D, et al. Standardized uptake values of (68)Ga-DOTANOC PET: a promising prognostic tool in neuroendocrine tumors. J Nucl Med. 2010;51(3):353–9.
Adams S, Baum R, Rink T, Schumm-Dräger PM, Usadel KH, Hör G. Limited value of fluorine-18 fluorodeoxyglucose positron emission tomography for the imaging of neuroendocrine tumors. Eur J Nucl Med. 1998;25:79–83.
Cescato R, Schulz S, Waser B, Eltschinger V, Rivier JE, Wester HJ, et al. Internalization of sst2, sst3, and sst5 receptors: effects of somatostatin agonists and antagonists. J Nucl Med. 2006;47(3):502–11.
Antunes P, Ginj M, Zhang H, Waser B, Baum RP, Reubi JC, et al. Are radiogallium-labelled DOTA-conjugated somatostatin analogues superior to those labelled with other radiometals? Eur J Nucl Med Mol Imaging. 2007;34(7):982–93.
Zhernosekov KP, Filosofov DV, Baum RP, Aschoff P, Bihl H, Razbash AA, et al. Processing of generator-produced 68Ga for medical application. J Nucl Med. 2007;48(10):1741–8.
Virgolini I, Ambrosini V, Bomanji JB, Baum RP, Fanti S, Gabriel M, et al. Procedure guidelines for PET/CT tumour imaging with 68Ga-DOTA-conjugated peptides: 68Ga-DOTA-TOC, 68Ga-DOTA-NOC, 68Ga-DOTA-TATE. Eur J Nucl Med Mol Imaging. 2010;37(10):2004–10.
Gabriel M, Decristoforo C, Kendler D, Dobrozemsky G, Heute D, Uprimny C, et al. [68Ga]DOTA-Tyr3-octreotide PET in neuroendocrine tumors: comparison with somatostatin receptor scintigraphy and CT. J Nucl Med. 2007;48(4):508–18.
Castellucci P, Pou Ucha J, Fuccio C, Rubello D, Ambrosini V, Montini GC, et al. Incidence of increased 68Ga-DOTANOC uptake in the pancreatic head in a large series of extrapancreatic NET patients studied with sequential PET/CT. J Nucl Med. 2011;52(6):886–90.
Hofmann M, Maecke H, Börner R, Weckesser E, Schöffski P, Oei L, et al. Biokinetics and imaging with the somatostatin receptor PET radioligand (68)Ga-DOTATOC: preliminary data. Eur J Nucl Med. 2001;28(12):1751–7.
Kowalski J, Henze M, Schuhmacher J, Mäcke HR, Hofmann M, Haberkorn U. Evaluation of positron emission tomography imaging using [68Ga]-DOTA-D Phe(1)-Tyr(3)-octreotide in comparison to [111In]-DTPAOC SPECT. First results in patients with neuroendocrine tumors. Mol Imaging Biol. 2003;5(1):42–8.
Putzer D, Gabriel M, Henninger B, Kendler D, Uprimny C, Dobrozemsky G, et al. Bone metastases in patients with neuroendocrine tumor: 68Ga-DOTA-Tyr3-octreotide PET in comparison to CT and bone scintigraphy. J Nucl Med. 2009;50(8):1214–21.
Pettinato C, Sarnelli A, Di Donna M, Civollani S, Nanni C, Montini G, et al. 68Ga-DOTANOC: biodistribution and dosimetry in patients affected by neuroendocrine tumors. Eur J Nucl Med Mol Imaging. 2008;35(1):72–9.
Ambrosini V, Tomassetti P, Castellucci P, Campana D, Montini G, Rubello D, et al. Comparison between [68Ga]DOTA-NOC and [18F]DOPA PET for the detection of gastro-entero-pancreatic and lung neuro-endocrine tumours. Eur J Nucl Med Mol Imaging. 2008;35(8):1431–8.
Fanti S, Ambrosini V, Tomassetti P, Castellucci P, Montini G, Allegri V, et al. Evaluation of unusual neuroendocrine tumours by means of [68Ga]DOTA-NOC PET. Biomed Pharmacother. 2008;62(10):667–71.
Prasad V, Ambrosini V, Hommann M, Hoersch D, Fanti S, Baum RP. Detection of unknown primary neuroendocrine tumours (CUP-NET) using (68)Ga-DOTA-NOC receptor PET/CT. Eur J Nucl Med Mol Imaging. 2010;37(1):67–77.
Ambrosini V, Campana D, Bodei L, Nanni C, Castellucci P, Allegri V, et al. 68Ga-DOTANOC PET/CT clinical impact in patients with neuroendocrine tumors. J Nucl Med. 2010;51(5):669–73.
Reubi JC, Schar JC, Waser B, Wenger S, Heppeler A, Schmitt JS, et al. Affinity profiles for human somatostatin receptor subtypes SST1-SST5 of somatostatin radiotracers selected for scintigraphic and radiotherapeutic use. Eur J Nucl Med. 2000;27:273–82.
Srirajaskanthan R, Kayani I, Quigley AM, Soh J, Caplin ME, Bomanji J. The role of 68Ga-DOTATATE PET in patients with neuroendocrine tumors and negative or equivocal findings on 111In-DTPA-octreotide scintigraphy. J Nucl Med. 2010;51(6):875–82.
Ambrosini V, Tomassetti P, Castellucci P, Campana D, Montini G, Rubello D, et al. Comparison between [68Ga]DOTA-NOC and [18F]DOPA PET for the detection of gastro-entero-pancreatic and lung neuro-endocrine tumours. Eur J Nucl Med Mol Imaging. 2008;35(8):1431–8.
Haug A, Auernhammer CJ, Wängler B, Tiling R, Schmidt G, Göke B, et al. Intraindividual comparison of [68Ga]DOTA-TATE and [18F]DOPA PET in patients with well-differentiated metastatic neuroendocrine tumours. Eur J Nucl Med Mol Imaging. 2009;36(5):765–70.
von Falck C, Boerner AR, Galanski M, Knapp WH. Neuroendocrine tumour of the mediastinum: fusion of 18F-FDG and 68Ga-DOTATOC PET/CT datasets demonstrates different degrees of differentiation. Eur J Nucl Med Mol Imaging. 2007;34(5):812.
Kayani I, Bomanji JB, Groves A, Conway G, Gacinovic S, Win T, et al. Functional imaging of neuroendocrine tumors with combined PET/CT using [68Ga]DOTATATE (DOTA-DPhe1, Tyr3-octreotate) and [18F]FDG. Cancer. 2008;112(11):2447–55.
Koukouraki S, Strauss LG, Georgoulias V, Eisenhut M, Haberkorn U, Dimitrakopoulou-Strauss A. Comparison of the pharmacokinetics of 68Ga-DOTATOC and [18F]FDG in patients with metastatic neuroendocrine tumours scheduled for 90Y-DOTATOC therapy. Eur J Nucl Med Mol Imaging. 2006;33(10):1115–22.
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ambrosini, V., Campana, D., Tomassetti, P. et al. 68Ga-labelled peptides for diagnosis of gastroenteropancreatic NET. Eur J Nucl Med Mol Imaging 39 (Suppl 1), 52–60 (2012). https://doi.org/10.1007/s00259-011-1989-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00259-011-1989-4