Abstract
Purpose
Typically, 18F-FDG PET/CT and 18F-NaF PET/CT scans are done as two separate studies on different days to allow sufficient time for the radiopharmaceutical from the first study to decay. This is inconvenient for the patients and exposes them to two doses of radiation from the CT component of the examinations. In the current study, we compared the clinical usefulness of a combined 18F-FDG/18F-NaF PET/CT scan with that of a separate 18F-FDG-only PET/CT scan.
Methods
There were 62 patients enrolled in this prospective trial. All had both an 18F-FDG-alone PET/CT scan and a combined 18F-FDG/18F-NaF PET/CT scan. Of the 62 patients, 53 (85%) received simultaneous tracer injections, while 9 (15%) received 18F-NaF subsequent to the initial 18F-FDG dose (average delay 2.2 h). Images were independently reviewed for PET findings by two Board-Certified nuclear medicine physicians, with discrepancies resolved by a third reader. Interpreters were instructed to only report findings that were concerning for malignancy. Reading the 18F-FDG-only scan first for half of the patients controlled for order bias.
Results
In 15 of the 62 patients (24%) neither the 18F-FDG-only PET/CT scan nor the combined 18F-FDG/18F-NaF PET/CT scan identified malignancy. In the remaining 47 patients who had PET findings of malignancy, a greater number of lesions were detected in 16 of 47 patients (34%) using the combined 18F-FDG/18F-NaF PET/CT scan compared to the 18F-FDG-only PET/CT scan. In 2 of these 47 patients (4%), the 18F-FDG-only scan demonstrated soft tissue lesions that were not prospectively identified on the combined study. In 29 of these 47 patients (62%), the combined scan detected an equal number of lesions compared to the 18F-FDG-only scan. Overall, 60 of all the 62 patients (97%) showed an equal or greater number of lesions on the combined scan than on the 18F-FDG-only scan.
Conclusion
The current study demonstrated that 18F-FDG and 18F-NaF can be combined in a single PET/CT scan by administering the two radiopharmaceuticals simultaneously or in sequence on the same day. In addition to patient convenience and reduced radiation exposure from the CT component, the combined 18F-FDG/18F-NaF PET/CT scan appeared to increase the sensitivity for detection of osseous lesions compared to the 18F-FDG-only PET/CT scan in the studied population.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
PET/CT performed with 18F-FDG is now widely used for the evaluation of various malignancies, but 18F-FDG has known limitations in detecting blastic malignant skeletal lesions [1–3]. In the setting of performing whole body evaluations for malignancy, these blastic lesions have been imaged traditionally with bone scintigraphy performed with 99mTc-labeled MDP using gamma (Anger) cameras. These conventional planar images have limitations related to spatial resolution and lack of specificity [4, 5] that may be partially overcome with SPECT/CT [6, 7]. While newer technologies such as diffusion-weighted (DW) MRI appear promising for the whole-body evaluation of malignant bony lesions in both the primary setting [8, 9] and the metastatic setting [10, 11], they are still considered investigational and are not routinely available. More clinical trials are needed with these imaging modalities before they are accepted as the standard of care for clinical use.
18F-NaF is a positron-emitting radiopharmaceutical that was first used for bone imaging in the 1970s [12]. Its clinical use was previously limited due to logistic difficulties in delivering a radiopharmaceutical with a half-life of 109.74 min and the lack of PET scanners that can more effectively detect the 511 keV photons of 18F-NaF compared to the then more prevalent gamma cameras [13]. However, the improved availability of 18F-NaF and the increasingly widespread use of PET/CT has sparked renewed interest in PET/CT bone scans using 18F-NaF. In fact, in February 2011, the Federal Drug Administration approved a New Drug Application from the National Cancer Institute for 18F-NaF to be used for PET bone scans [14]. Furthermore, starting in February 2011, the Centers for Medicare and Medicaid Services started reimbursing for 18F-NaF PET/CT bone scans done through the National Oncologic PET Registry [15]. Such whole-body scans have the advantage of reduced imaging time, improved image resolution which may allow detection of smaller lesions, as well as enabling better lesion localization and specificity through the use of the available CT. Previous studies have demonstrated the superiority of 18F-NaF bone scintigraphy compared to planar 99mTc-MDP bone scintigraphy [16–19].
Typically, 18F-FDG PET/CT and 18F-NaF PET/CT scans are done as two separate studies on different days to allow sufficient time for the radiopharmaceutical from the first study to decay. This is inconvenient for patients and exposes them to two doses of radiation from the CT component of the scans. We have demonstrated the feasibility of administering both 18F-FDG and 18F-NaF in a single combined PET/CT scan, with similar performance for lesion detection compared to either scan done separately [20]. In the current study, we compared the clinical usefulness of a combined 18F-FDG/18F-NaF PET/CT scan with that of a separate 18F-FDG PET/CT scan. We also investigated whether the combined scanning can be performed in sequence with delayed administration of 18F-NaF subsequent to the initial 18F-FDG injection.
Materials and methods
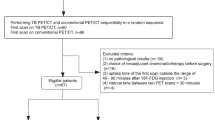
All patients were scanned at the Apollo Gleneagles PET/CT Centre in Hyderabad, India, under the immediate supervision of one of the coauthors of this study (J.E.R.). Approval from the local hospital ethics committee was obtained for this prospective trial. In addition, the Institutional Review Board at Stanford University approved the data transfer and local analysis. From July through December of 2009, consecutive patients with a history of histologically confirmed cancer were asked to participate in this study by their oncologists and subsequently referred for the 18F-FDG PET/CT and the combined 18F-FDG/18F-NaF PET/CT scans. All cancer types were included in the study in order to simulate actual clinical experience. The initial treatment strategy (formal diagnosis and initial staging) was the indication for imaging in 30% of the patients, while the remaining 70% were referred for subsequent treatment strategy (including treatment monitoring, restaging and detection of suspected recurrence). This classification was based on the National Coverage Determination for 18F-FDG PET for Oncologic Conditions from the Centers for Medicare & Medicaid Services [21]. During the study accrual period, 66 patients were recruited after informed consent had been obtained. Four of these 66 patients were removed because they did not complete both the 18F-FDG-only and the combined 18F-FDG/18F-NaF PET/CT scans, leaving 62 evaluable patients for the final analysis. The 62 evaluable patients were 22–74 years of age (average: 52.6 ± 12.7 years), with an almost 3:1 ratio of women (45, 73%) to men (17, 27%).
All scans were acquired on a Siemens Biograph 16 PET/CT scanner (Siemens, Erlangen, Germany). For the 18F-FDG-only scan, patients were injected intravenously (i.v.) with 555 MBq (15 mCi) of 18F-FDG after a minimum of 6 h of fasting and confirmation of a serum glucose level less than 150 mg/dl. All 18F-FDG scans were performed with both oral contrast agent (Telebrix; Guerbet, Telebrix; Guerbet, Gorinchem, The Netherlands) and i.v. contrast agent (Omnipaque; GE Healthcare, Princeton, NJ). For the combined scans, 53 of the 62 patients (85%) received simultaneous i.v. injection of 185 MBq (5 mCi) of 18F-NaF and 555 MBq (15 mCi) of 18F-FDG for a second PET/CT scan that was done the following day. The remaining 9 patients (15%) had the combined scan done after sequential i.v. tracer administration of 185 MBq (5 mCi) of 18F-NaF subsequent (average 133 ± 16 min) to the initial 18F-FDG dose used for the 18F-FDG-only scan, without reinjection of 18F-FDG for this second scan. The combined PET/CT studies were performed without oral or i.v. contrast agent in both the simultaneous and subsequent injection groups.
Images were displayed and interpreted on a dedicated workstation using Xeleris software (GE Healthcare, Haifa, Israel). All scans were independently reviewed by two of the three Board-Certified nuclear medicine physicians (A.I., F.I.L., E.S.M.) who were blinded to the patient’s history, diagnosis, and findings on the other imaging studies. Discrepancies were resolved by a consensus image interpretation with the third reader. The scans were evaluated qualitatively for positive findings, and interpreters were instructed to only report findings that were likely to represent malignancy. For this trial, visual analysis was used for the interpretation of the scans instead of quantitative analysis (i.e., standardized uptake value cut-offs). For the combined PET/CT scans, areas of focally increased skeletal uptake were read as malignant unless a benign etiology such as degenerative bone disease was identified at the same location on the corresponding CT images. For the 18F-FDG-only PET/CT scans, focal 18F-FDG uptake less than the mediastinal blood pool was considered benign, uptake equal to the mediastinal blood pool was considered uncertain, and uptake greater than mediastinal blood pool was considered malignant. Prior work has shown the validity of this approach [22, 23].
Results
Patients with a variety of malignancies were included, the most common being breast cancer, that accounted for 34 of the 62 patients (55%). Other cancers reported in the studied cohort included prostate (6, 10%), lung (6, 10%), sarcoma (2, 3%), lymphoma (2, 3%), and miscellaneous such as gastric, colorectal, cervical, endometrial, renal, and head and neck cancers (9, 14%). Three of the 62 patients (5%) had a malignancy of unknown primary. The high percentage of breast cancer patients included in the study contributed to the gender skew mentioned above.
For the 18F-FDG-only scans, the average radiopharmaceutical dose was 499.5 ± 22.2 MBq (13.5 ± 0.6 mCi), with a range of 266.4–740 MBq (7.2–20.0 mCi). The average uptake time was 59.9 ± 0.7 min with a range of 55–70 min. For the combined scans done with simultaneous injections, the average 18F-FDG dose was 529.1 ± 18.5 MBq (14.3 ± 0.5 mCi) with a range of 370–740 MBq (10.0–20.0 mCi), and the average 18F-NaF dose was 192.4 ± 7.4 MBq (5.2 ± 0.2 mCi) with a range of 370–740 MBq (4.0–8.0 mCi). The average uptake time was 61.3 ± 0.8 min, with a range of 55–70 min. For the nine cocktail scans done with subsequent 18F-NaF injections, the average 18F-FDG dose was 569.8 ± 66.6 MBq (15.4 ± 1.8 mCi) with a range of 432.9–740 MBq (11.7–20.0 mCi), and the average 18F-NaF dose was 214.6 ± 33.3 MBq (5.8 ± 0.9 mCi) with a range of 166.5–292.3 MBq (4.5–7.9 mCi). The average uptake time for the 18F-FDG in this subgroup was 192 ± 24 min with a range of 159–226 min, while the average uptake time for the 18F-NaF was 60 ± 1.7 min, with a range of 55–65 min (Table 1).
In 15 of the 62 patients (24%), malignancy was not identified by the 18F-FDG-only PET/CT scan or the combined 18F-FDG/18F-NaF PET/CT scan. In the remaining 47 patients who had PET findings of malignancy, a greater number of lesions were detected in 16 patients (34%) by the combined 18F-FDG/18F-NaF PET/CT than by the 18F-FDG-only PET/CT scan. In 5 of these 16 patients the 18F-FDG-only scan was negative for metastases; therefore, their staging was changed from M0 to M1. There were nine breast, two rectal, two prostate, one lung, and two cancers of unknown primary in the subgroup of 16 patients with more lesions detected on the combined scan. All of the additionally detected lesions on the cocktail study were in the skeleton, as expected, with specific regions involved including the rib cage (five patients), spine (four patients), pelvis (four patients), skull (three patients), sternum (three patients), femur (one patient), humerus (one patient), and scapula (one patient). Examples of these findings are shown in Figs. 1 and 2.
A 32-year-old man with rectal cancer referred for subsequent treatment strategy (restaging). a, b Maximum intensity projection PET/CT images. The image obtained after combined 18F-NaF/18F-FDG administration (b) demonstrates focally increased uptake compatible with L1 osseous metastasis (arrow) that is not clearly identified on the image from the 18F-FDG-only scan (a). c Transaxial CT image shows a sclerotic lesion in the L1 vertebra (arrowhead). d The PET image from the combined 18F-NaF/18F-FDG scan shows increased radiopharmaceutical uptake (arrowhead). e The same lesion (arrowhead) did not show uptake on the 18F-FDG-only scan
A 52-year-old woman with breast cancer referred for subsequent treatment strategy (detection of suspected recurrence; last chemo- and radiation therapy 2 years prior to the scans). a, b Maximum intensity projection images. The image obtained after combined 18F-NaF/18F-FDG administration (b) demonstrates multiple foci of increased uptake compatible with osseous metastases that are not clearly identified on the image from the 18F-FDG-only scan (a). c–e Transaxial images of selected lesions (arrowheads) in the L4 vertebra, left sacrum and left femur: CT (c), 18F-FDG-only PET (d), and combined 18F-NaF/18F-FDG PET (e). The lesions are more prominent on the combined scan
In 29 of the 47 patients with PET findings (62%), the combined scan detected the same number of lesions as the 18F-FDG-only scan. In 2 of these 47 patients (4%), the 18F-FDG-only scan demonstrated lesions that were not identified on the combined PET/CT scan. In one of these patients, the 18F-FDG-only scan showed a mediastinal lymph node that was not identified on the combined scan. However, this patient had multiple positive mediastinal lymph nodes and the overall impression of the study, as well as the staging of the patient, would not have been changed by this missed lesion. In the second patient, right cardiophrenic and retroperitoneal lymph nodes were apparent on the 18F-FDG-only scan and were only faintly visualized and not prospectively called on the combined scan. These findings are presented in Figs. 3 and 4.
A 59-year-old woman with breast cancer referred for subsequent treatment strategy (detection of suspected recurrence; last chemo- and radiation therapy 2 years prior to the scans). 18F-FDG-only PET/CT scan (transaxial CT, PET and fused PET/CT images; top row) shows uptake in mediastinal lymph nodes (arrowheads). Combined 18F-FDG and 18F-NaF PET/CT scan (transaxial CT, PET and fused PET/CT images; bottom row) shows very mild uptake in mediastinal lymph nodes (arrowheads)
A 70-year-old man with prostate cancer referred for subsequent treatment strategy (restaging). 18F-FDG-only PET/CT scan (transaxial CT, PET and fused PET/CT images; top row) shows uptake in retroperitoneal lymph nodes (arrows). Combined 18F-FDG and 18F-NaF PET/CT scan (transaxial CT, PET and fused PET/CT; bottom row) shows very mild uptake in retroperitoneal lymph nodes (arrows). Liver lesions are apparent on both scans (arrowheads)
Subgroup analysis showed no significant differences between combined scans done by simultaneous vs. subsequent injections in terms of changing the overall impression or staging of the patient. For the group who received simultaneous tracer injections, in 15 of the 53 studies (28%) there were more lesions on the combined scan than on the 18F-FDG-alone scan, compared to 1 of 9 pairs of scans (11%) in the subsequent group. Equal number of lesions was seen on both scans in 36 of 53 pairs (68%) in the simultaneous injection group vs. 8 of 9 pairs (89%) in the subsequent group. Both patients in whom the 18F-FDG-only scan showed more lesions than the combined study received simultaneous injections in addition to the 18F-FDG-only scan.
Overall, 60 of the 62 patients included in the study (97%) had an equal or greater number of lesions identified on the combined 18F-FDG/18F-NaF PET/CT scan than on the 18F-FDG-only scan.
Discussion
Previous studies have demonstrated limitations of 18F-FDG PET/CT for the detection of blastic osseous malignant lesions. Therefore, these have been better evaluated with gamma cameras using bone-seeking agents such as 99mTc-diphosphonates [16, 24, 25]. Several recent studies have also demonstrated the advantages of 18F-NaF PET/CT over planar or SPECT bone scans in terms of image resolution, sensitivity and specificity (by adding CT) [26]. 18F-FDG PET/CT and bone scans are typically done as two separate studies on different days, although previous studies have already demonstrated the feasibility of combined 18F-FDG and 18F-NaF in a single study, both as PET-only imaging [27] and as PET/CT [20].
Our study confirms that combined 18F-NaF/18F-FDG PET/CT imaging can be successfully performed as a single examination and that this combination increases the sensitivity for skeletal the detection of metastases when compared to 18F-FDG PET/CT alone. Another benefit of this approach is improved convenience for the patients and increased efficiency for the utilization of the PET/CT camera time. It is worth noting that overall an equivalent or greater number of lesions was detected in 97% of the patients using combined 18F-NaF/18F-FDG PET/CT compared to 18F-FDG-only PET/CT. As anticipated, all of the additionally detected lesions were in the skeleton.
One of the limitations of this study is that clinical confirmation of malignancy for all detected lesions was not feasible. This may be an area of improvement for future studies. Although pathological confirmation of all of these lesions may not be needed and may in fact be impractical/unethical, future studies could consider correlations between the newly found lesions and other noninvasive, whole-body imaging modalities such as DW MRI [28–31]. Another limitation of this study is that a separate interpretation of the CT component of the PET/CT scans was not done. Published data suggest that combining the information from 18F-FDG and CT independently can improve diagnostic accuracy [32].
In order to evaluate the clinical utility of combined 18F-FDG/18F-NaF PET/CT for detection of malignancy, it is important to discuss further the two patients in whom the 18F-FDG-only scan demonstrated lesions that were not seen on the combined scan. In the first patient, there was a mediastinal lymph node that was initially missed on the combined scan, although in retrospect the lesion was faintly visible. Despite this, the overall impression of the study and the patient’s clinical staging was not altered, since there were several other hypermetabolic mediastinal lymph nodes identified on the combined scan. In the second patient, the 18F-FDG-only study demonstrated hypermetabolic cardiophrenic and retroperitoneal lymph nodes that did not show sufficient 18F-FDG uptake above the background in order to be called positive on the combined scan. However, the missed lesions did not change the clinical or radiographic stage and no change in treatment would have resulted from their detection. These lesions were also not biopsy-proven for malignancy.
An important observation is that when findings between the 18F-FDG-only and combined scans are discrepant in favor of the 18F-NaF/18F-FDG PET/CT scan (i.e., more lesions detected on the combined scan), the impact on staging may be significant. Of the 16 patients who had more findings on the combined scans, 5 would have had their clinical staging changed from M0 to M1, as the 18F-FDG-only scans in these 5 patients were negative for metastatic lesions. While these were not biopsy-proven, the discrepant lymph nodes detected only on the 18F-FDG scans were also not biopsy-proven to represent metastatic disease. The cause of these conflicting observations should be further evaluated in future studies, and technical aspects such as alterations in image reconstruction for the combined scans from intense 18F-NaF uptake in osseous lesions should be considered. The validation of the combined technique is complicated by the fact that there is currently no good gold standard in the evaluation of bone scan-positive (either with 18F-NaF or with 99mTc-MDP) but 18F-FDG-negative lesions short of a bone biopsy, which is impractical to perform in all patients. In addition, the patient’s clinical examination is also a poor marker of disease progression as patients’ self-report of bone pain is not always indicative of worsening disease [33, 34].
Another limitation of the study is that semiquantitative analysis of radiopharmaceutical uptake such as standardized uptake value measurements was not performed. Semiquantitative analysis of 18F-NaF PET/CT scans is still an evolving field that has no standardized procedures and lacks validation [35]. Issues such as the effect of 18F-NaF on bone and soft tissue uptake of 18F-FDG when given simultaneously also have not been explored. An analysis of these issues was beyond the scope of the current study. While this kind of analyses should certainly be addressed in future evaluations, the conclusions regarding the clinical utility of cocktail scans drawn from this study remain valid. Oral and i.v. contrast agents were given for the 18F-FDG-only scan but not for the combined scan, in order to limit exposure of the patients to contrast agent. However, evidence for the superior sensitivity of the cocktail study remains legitimate because contrast agent administration is expected to only increase the relative detection ability of the 18F-FDG-only scan.
We acknowledge that some of the lesions identified on the combined scan due to the addition of 18F-NaF may have represented treatment-related changes (i.e., bone repair), and not active metastases, as our patient population included a large number of patients referred for subsequent treatment strategy. Scan indications for the 18 patients who had discrepant findings between the combined and the 18F-FDG-only scans are listed in Table 2. Of these 18 patients, 15 (83%) were referred for subsequent treatment strategy. While this may represent a limitation of the study, our goal was to demonstrate that improved lesion detection and sensitivity can be achieved by using the combined administration and imaging of 18F-NaF and 18F-FDG. Our goal was not to document the performance of 18F-NaF or 18F-FDG for detection of true-positive lesions, but this may be a question for future studies. Of these 15 subsequent treatment strategy patients, 3 with discrepant findings had had their last therapy more than 2 years (2007, 2003, 1998) prior to the scans, making reactive bone uptake less likely as a cause of false-positive lesions. Additional lesions were also identified in the 3 patients presenting for initial treatment strategy. Both patients with cancer of unknown primary who presented for initial treatment strategy had more lesions detected on the combined scan, suggesting that the combined method may be useful in this particular patient population. While the findings are more convincing for the participants in the initial treatment strategy group, further studies are needed to document the usefulness of combined imaging with 18F-NaF/18F-FDG for the cancer patients referred for subsequent treatment strategy.
Patients with all cancer types were included in this study to facilitate patient accrual, as well as to simulate an actual clinical experience. However, since 18F-FDG PET/CT is infrequently done for the evaluation of prostate cancer, including such patients may have created a study population that is not representative of actual patient distribution and may distort the findings regarding the clinical relevance of combined 18F-NaF/18F-FDG imaging. To address this issue, a subanalysis was done which excluded the six patients with prostate cancer. In the remaining 56 non-prostate cancer patients, 14 (25%) did not show malignancy on either scan. Of the remaining 42 pairs of scans, 27 (64%) demonstrated equal findings, while 14 (33%) showed more lesions on the combined scan. As one of the two patients with missed lesions had prostate cancer, only one patient would have had 18F-FDG-avid lesions not prospectively identified on the combined scan. These results with the prostate cancer patients excluded are comparable to the results obtained from the entire study population. A valid argument can be made that the combined scan may not be useful in the evaluation of patients with lung cancer. Indeed, Krüger et al. have reported data suggesting that 18F-FDG PET/CT is superior to 18F-NaF PET/CT and 99mTc-MDP bone scintigraphy in the detection of osteolytic bone metastases in patients with non-small-cell lung cancer [36]. Various organizations publish clinical guidelines, such as those from the National Comprehensive Cancer Network (NCCN). These guidelines do not always recommend the use of both 18F-FDG PET/CT and bone scintigraphy; however, guidelines frequently change based on emerging data from clinical trials and the role of various imaging modalities is frequently reviewed. Therefore, future research projects, including on combined 18F-FDG/18F-NaF PET/CT are warranted.
Subgroup analysis of the data demonstrated that administering the 18F-NaF subsequent to the initial 18F-FDG dose can allow successful combined imaging. Taking into account the small number of patients in the subsequent group (n = 9), there were no clinically significant differences in lesion detection for the combined scans between those done with 18F-NaF given simultaneously and those done with 18F-NaF given subsequently after the initial 18F-FDG injection. Our preliminary results suggest that the two methods may be equally effective. If validated in future research, this could translate into added clinical flexibility. For instance, a study can first be done with 18F-FDG, with 18F-NaF given subsequently if there are equivocal osseous lesions seen after initial review of the images or if the clinical suspicion for bone metastases remains high despite a negative 18F-FDG scan.
In terms of exposure of the patients to radiation, the combined 18F-FDG/18F-NaF PET/CT scan reduces the doses compared to performing two separate scans [20]. Using dosimetry data used in the pilot study, patients with 18F-FDG PET/CT and 18F-NaF PET/CT as two separate scans would receive a total of approximately 41.5 mSv (4,150 mrem), i.e., 0.03 mSv/MBq (110 mrem/mCi) from 18F-FDG, 0.03 mSv/MBq (100 mrem/mCi) from 18F-NaF, and 10 mSv (1,000 mrem) from each of the low-dose CT scans. In comparison, patients with these two scans as a single combined scan would receive approximately 31.5 mSv (3,150 mrem) because only one low-dose CT is needed instead of two. This represents a 26% decrease in patient radiation exposure. Further reduction in radiation exposure can be achieved by optimizing the doses of 18F-FDG and 18F-NaF administered in the combined study, and this could be an area of research for future trials.
Conclusion
The current study demonstrated that whole-body 18F-FDG and 18F-NaF PET/CT imaging can be combined into a single study by administering both radiopharmaceuticals simultaneously or subsequently on the same day. In addition to patient convenience and reduced radiation dose to the patients from the CT scan, the combined 18F-FDG/18F-NaF PET/CT scans appear to increase the sensitivity for detection of osseous lesions compared to the separate 18F-FDG PET/CT scans in the studied population. Further research is needed to identify and validate the specific indications of the combined 18F-FDG/18F-NaF PET/CT. The potential reduction in health-care costs should also be further evaluated. It is possible that other tracer cocktails may be of even greater clinical value, as the combination of PET radiopharmaceuticals for a single examination continues to evolve in the future.
References
Huyge V, Garcia C, Vanderstappen A, Alexiou J, Gil T, Flamen P. Progressive osteoblastic bone metastases in breast cancer negative on FDG-PET. Clin Nucl Med. 2009;34(7):417–20.
Nakai T, Okuyama C, Kubota T, Yamada K, Ushijima Y, Taniike K, et al. Pitfalls of FDG-PET for the diagnosis of osteoblastic bone metastases in patients with breast cancer. Eur J Nucl Med Mol Imaging. 2005;32(11):1253–8.
Cook GJ, Houston S, Rubens R, Maisey MN, Fogelman I. Detection of bone metastases in breast cancer by 18FDG PET: differing metabolic activity in osteoblastic and osteolytic lesions. J Clin Oncol. 1998;16(10):3375–9.
Chua S, Gnanasegaran G, Cook G. Miscellaneous cancers (lung, thyroid, renal cancer, myeloma, and neuroendocrine tumors): role of SPECT and PET in imaging bone metastases. Semin Nucl Med. 2009;39(6):416–30.
Schirrmeister H, Glatting G, Hetzel J, Nüssle K, Arslandemir C, Buck AK, et al. Prospective evaluation of the clinical value of planar bone scans, SPECT, and (18)F-labeled NaF PET in newly diagnosed lung cancer. J Nucl Med. 2001;42(12):1800–4.
Savelli G, Maffioli L, Maccauro M, De Deckere E, Bombardieri E. Bone scintigraphy and the added value of SPECT (single photon emission tomography) in detecting skeletal lesions. Q J Nucl Med. 2001;45(1):27–37.
Bybel B, Brunken R, DiFilippo F, Neumann D, Wu G, Cerqueira M. SPECT/CT imaging: clinical utility of an emerging technology. Radiographics. 2008;28(4):1097–113.
Eftekhari F. Imaging assessment of osteosarcoma in childhood and adolescence: diagnosis, staging, and evaluating response to chemotherapy. Cancer Treat Res. 2009;152:33–62.
James SL, Panicek DM, Davies AM. Bone marrow oedema associated with benign and malignant bone tumours. Eur J Radiol. 2008;67(1):11–21.
Schmidt G, Reiser M, Baur-Melnyk A. Whole-body MRI for the staging and follow-up of patients with metastasis. Eur J Radiol. 2009;70(3):393–400.
Bäuerle T, Semmler W. Imaging response to systemic therapy for bone metastases. Eur Radiol. 2009;19(10):2495–507.
Blau M, Nagler W, Bender MA. Fluorine-18: a new isotope for bone scanning. J Nucl Med. 1962;3:332–4.
Dasgeb B, Mulligan M, Kim C. The current status of bone scintigraphy in malignant diseases. Semin Musculoskelet Radiol. 2007;11(4):301–11.
National Cancer Institute. New drug for use in bone scans approved; provides an alternative to radioactive tracer that is currently in short supply. http://www.cancer.gov/newscenter/pressreleases/SodiumFluoride18. Updated 1 Feb 2011. Accessed 27 Oct 2011.
National Oncologic PET Registry. NOPR Update: NOPR announcement regarding coverage change implementation. http://www.cancerpetregistry.org/news.htm#FEB022011. Updated 1 Feb 2011. Accessed 27 Oct 2011.
Fogelman I, Cook G, Israel O, Van der Wall H. Positron emission tomography and bone metastases. Breast Dis. 2005;35(2):135–42.
Hetzel M, Arslandemir C, König HH, Buck AK, Nüssle K, Glatting G, et al. F-18 NaF PET for detection of bone metastases in lung cancer: accuracy, cost-effectiveness, and impact on patient management. J Bone Miner Res. 2003;18(12):2206–14.
Petrén-Mallmin M, Andréasson I, Ljunggren O, Ahlström H, Bergh J, Antoni G, et al. Skeletal metastases from breast cancer: uptake of 18F-fluoride measured with positron emission tomography in correlation with CT. Skeletal Radiol. 1998;27(2):72–6.
Schirrmeister H, Guhlmann A, Elsner K, Kotzerke J, Glatting G, Rentschler M, et al. Sensitivity in detecting osseous lesions depends on anatomic localization: planar bone scintigraphy versus 18F PET. J Nucl Med. 1999;40(10):1623–9.
Iagaru A, Mittra E, Yaghoubi S, Dick DW, Quon A, Goris ML, et al. Novel strategy for a cocktail 18F-fluoride and 18F-FDG PET/CT scan for evaluation of malignancy: results of the pilot-phase study. J Nucl Med. 2009;50(4):501–5.
Centers for Medicare and Medicaid Services. National Coverage Determination (NCD) for Positron Emission Tomogtaphy (FDG) for Oncologic Conditions (220.6.17). 2010; https://www.cms.gov/medicare-coverage-database/details/ncd-details.aspx. Accessed Sep 01, 2011.
Christensen JA, Nathan MA, Mullan BP, Hartman TE, Swensen SJ, Lowe VJ. Characterization of the solitary pulmonary nodule: 18F-FDG PET versus nodule-enhancement CT. AJR Am J Roentgenol. 2006;187(5):1361–7.
Juweid ME, Stroobants S, Hoekstra OS, Mottaghy FM, Dietlein M, Guermazi A, et al. Use of positron emission tomography for response assessment of lymphoma: consensus of the Imaging Subcommittee of International Harmonization Project in Lymphoma. J Clin Oncol. 2007;25(5):571–8.
Gallowitsch H-J, Kresnik E, Gasser J, Kumnig G, Igerc I, Mikosch P, et al. F-18 fluorodeoxyglucose positron-emission tomography in the diagnosis of tumor recurrence and metastases in the follow-up of patients with breast carcinoma: a comparison to conventional imaging. Invest Radiol. 2003;38(5):250–6.
Moon DH, Maddahi J, Silverman DH, Glaspy JA, Phelps ME, Hoh CK. Accuracy of whole-body fluorine-18-FDG PET for the detection of recurrent or metastatic breast carcinoma. J Nucl Med. 1998;39(3):431–5.
Grant F, Fahey F, Packard A, Davis R, Alavi A, Treves T. Skeletal PET with 18F-fluoride: applying new technology to an old tracer. J Nucl Med. 2008;49(1):68–78.
Hoegerle S, Juengling F, Otte A, Altehoefer C, Moser EA, Nitzsche EU. Combined FDG and [F-18]fluoride whole-body PET: a feasible two-in-one approach to cancer imaging? Radiology. 1998;209(1):253–8.
Messiou C, Cook G, deSouza NM. Imaging metastatic bone disease from carcinoma of the prostate. Br J Cancer. 2009;101(8):1225–32.
Takenaka D, Ohno Y, Matsumoto K, Aoyama N, Onishi Y, Koyama H, et al. Detection of bone metastases in non-small cell lung cancer patients: comparison of whole-body diffusion-weighted imaging (DWI), whole-body MR imaging without and with DWI, whole-body FDG-PET/CT, and bone scintigraphy. J Magn Reson Imaging. 2009;30(2):298–308.
Kwee T, Takahara T, Ochiai R, Koh DM, Ohno Y, Nakanishi K, et al. Complementary roles of whole-body diffusion-weighted MRI and 18F-FDG PET: the state of the art and potential applications. J Nucl Med. 2010;51(10):1549–58.
Nakanishi K, Kobayashi M, Nakaguchi K, Kyakuno M, Hashimoto N, Onishi H, et al. Whole-body MRI for detecting metastatic bone tumor: diagnostic value of diffusion-weighted images. Magn Reson Med Sci. 2007;6(3):147–55.
Taira A, Herfkens R, Gambhir S, Quon A. Detection of bone metastases: assessment of integrated FDG PET/CT imaging. Radiology. 2007;243(1):204–11.
Blomqvist C, Elomaa I, Virkkunen P, Porkka L, Karonen SL, Risteli L, et al. The response evaluation of bone metastases in mammary carcinoma. The value of radiology, scintigraphy, and biochemical markers of bone metabolism. Cancer. 1987;60(12):2907–12.
Hird A, Chow E, Zhang L, Wong R, Wu J, Sinclair E, et al. Determining the incidence of pain flare following palliative radiotherapy for symptomatic bone metastases: results from three Canadian cancer centers. Int J Radiat Oncol Biol Phys. 2009;75(1):193–7.
Segall G, Delbeke D, Stabin M, Even-Sapir E, Fair J, Sajdak R, et al. SNM practice guideline for sodium 18F-fluoride PET/CT bone scans 1.0. J Nucl Med. 2010;51(11):1813–20.
Krüger S, Buck A, Mottaghy F, Hasenkamp E, Pauls S, Schumann C, et al. Detection of bone metastases in patients with lung cancer: 99mTc-MDP planar bone scintigraphy, 18F-fluoride PET or 18F-FDG PET/CT. Eur J Nucl Med Mol Imaging. 2009;36(11):1807–12.
Acknowledgments
This research was supported in part by NCI ICMIC CA114747 (S.S.G.) and clinical studies were supported in part by the Doris Duke Foundation and Canary Foundation (S.S.G.). We would also like to thank Mr. Atul Gada (senior technologist) whose help and support was immense.
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lin, F.I., Rao, J.E., Mittra, E.S. et al. Prospective comparison of combined 18F-FDG and 18F-NaF PET/CT vs. 18F-FDG PET/CT imaging for detection of malignancy. Eur J Nucl Med Mol Imaging 39, 262–270 (2012). https://doi.org/10.1007/s00259-011-1971-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00259-011-1971-1