Abstract
Purpose
Pathological data suggest that the rate of oestrogen receptor (ER) expression in uterine sarcoma is significantly lower than in leiomyoma. The present study aimed to investigate whether ER expression using ER imaging agents for positron emission tomography (PET), of which the most successful has been 16α-[18F]-fluoro-17β-oestradiol (FES), is able to add useful information to the differential diagnosis of uterine sarcoma and leiomyoma in patients with positive or equivocal findings on [18F]fluorodeoxyglucose (FDG) PET.
Methods
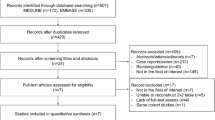
A total of 76 patients with suspected uterine sarcoma based on ultrasound and magnetic resonance imaging findings from 2007 to 2010 were enrolled. Twenty-four of the present patients were referred for FES PET because of FDG PET findings that showed equivocal or positive FDG uptake. PET images were quantitatively evaluated with reference to histopathological findings. Receiver-operating characteristic analysis was performed to determine the optimal cutoff value to differentiate uterine sarcoma and leiomyoma.
Results
Of the 24 patients, 11 had a final diagnosis of uterine sarcoma, while 13 had leiomyoma. The sensitivity, specificity and accuracy of an FDG to FES standardized uptake value (SUV) ratio greater than 2.0 were significantly higher using Cochran’s Q test (p = 0.024) when compared with FDG PET greater than 3.0 alone (90.9 vs 81.8%, 92.3 vs 84.6% and 91.3 vs 83.3%, respectively).
Conclusion
Additional FES PET findings confirmed uterine sarcoma in 91.3% of a selected group of patients with equivocal or positive FDG uptake.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Uterine leiomyoma is a common benign uterine tumour of mesenchymal origin. Most uterine leiomyomas are oestrogen receptor (ER)-expressing tumours that occur in 25–30% of women over 30 years of age [1]. On the other hand, mesenchymal tumours other than uterine leiomyomas, such as uterine sarcoma, are uncommon. They constitute only 3% of uterine malignancies, including carcinosarcoma (CS), leiomyosarcoma (LMS), endometrial stromal sarcoma (ESS) and adenosarcoma, and show less ER expression [2]. Despite representing a low fraction of uterine corpus cancers, sarcomas account for a disproportionately high fraction of deaths. The importance of properly diagnosing uterine sarcoma cannot be understated due to the possibility of conservative treatment of leiomyoma. The main problem encountered is that proper diagnosis may delay or prevent final histological tissue diagnosis [3–6]. Thus, differentiating uterine sarcoma from leiomyoma is an important clinical issue. As preoperative histological examination of uterine myometrial lesions may present practical difficulties and be associated with significant sampling errors, imaging plays an important role in the evaluation of myometrial lesions. The usefulness of magnetic resonance imaging (MRI) in the workup of uterine sarcoma is well known; however, even when using MRI, it is difficult to distinguish between a uterine sarcoma and leiomyoma, particularly when degeneration is evident [7–10].
Although increased uptake on positron emission tomography (PET) with [18F]fluorodeoxyglucose (FDG) has emerged as a promising oncological imaging tool, several reports have described significant FDG uptake in leiomyomas [11, 12]. In addition, a recent review concluded that FDG PET alone cannot be used to differentiate LMS from leiomyoma, as uterine leiomyoma rarely shows high FDG uptake and LMS rarely shows mild FDG uptake [13].
An encouraging experience in 25 patients with leiomyoma or LMS showed that ER expression coupled with glucose metabolism using ER imaging agents for PET, of which the most successful has been 16α-[18F]-fluoro-17β-oestradiol (FES) and FDG PET, is useful for differential diagnosis of leiomyoma and LMS [14]. A combination of FDG and FES findings could thus be useful for predicting uterine sarcoma. If it is difficult to exclude malignancy in cases of uterine leiomyoma with FDG uptake with a qualitative evaluation, intense FES uptake by the lesion on additional FES PET scanning can suggest that the lesion is a benign leiomyoma; however, this has not yet been systemically shown with prospective clinical trials.
The purpose of the present prospective study was to investigate whether regional uptake of FES can add useful information for the differential diagnosis of uterine sarcoma and leiomyoma.
Materials and methods
Subjects
Between April 2007 and October 2010, FDG PET was performed in 76 patients with uterine sarcoma-related symptoms and “suspected uterine sarcoma” according to the following imaging findings: (a) ultrasound exhibiting enlarged tumour and the characteristic “mosaic pattern” on ultrasonic power Doppler images [13] and (b) MRI exhibiting enlarged uterine tumour of mesenchymal origin showing heterogeneous high-signal intensity on T2-weighted images and/or the characteristic “enhancement” on contrast-enhanced MRI. All patients were seen by gynaecological oncological physicians at our outpatient clinic at Fukui University Hospital. Of these, 36 were enrolled for FES PET because of FDG PET findings that showed equivocal or positive FDG tracer uptake. We retrospectively reviewed clinical data from the 36 patients and obtained informed consent. Subsequently, 12 of the 36 patients were excluded for the following reasons: (a) they had abnormal endometrial cytology, (b) they did not wish to undergo surgery, (c) they had received hormonal replacement therapy or (d) they did not wish to undergo FES PET within 2 weeks prior to surgery. Thus, within 2 weeks before surgery, the images and clinical data from the 24 patients (mean age 51.3 ± 2.7 years; range 31–77 years) who underwent FES PET imaging were reviewed. Definitive diagnosis was determined by postoperative histopathological analysis (n = 24) (Table 1). This study was approved by the Institutional Review Board of our institution and informed consent was obtained from all participating patients.
FDG PET and FES PET
Two PET scans with FDG and FES were performed on 2 separate days within a 2-week period. A whole-body tomography scanner (Advance, General Electric Medical Systems), which permitted the simultaneous acquisition of 35 image slices in a two-dimensional acquisition mode with an inter-slice spacing of 4.25 mm, was used. Performance tests showed the intrinsic resolution of the scanner to be 4.0–5.3 mm in the axial direction and 4.6–5.7 mm in the transaxial direction.
FES was synthesized as reported elsewhere [15]. The specific activity was 100–200 GBq/μmol and radiochemical purity was greater than 99%. For each FES and FDG PET study, approximately 185 MBq of tracer was administered via the antecubital vein. Before tracer administration in each study, patients fasted for at least 4 h in order to avoid elevation of blood sugar levels in FDG PET and to reduce tracer excretion to the intestines in FES PET. Fifty minutes after tracer injection, the patient was positioned supine in the PET scanner, and a 16-min emission scan was started with 3-min scans at the pelvic region (two bed positions) and 2-min scans in each remaining region (five bed positions) in order to completely cover the head to inguinal regions. Post-injection transmission scans of 2 min at the pelvis and 1 min in other areas were performed after emission scans using a 68Ge/68Ga rod source for attenuation correction. PET data were reconstructed by the iterative reconstruction method, with selection of 14 subsets and 2 iterations. Reconstructed images were then converted into a semiquantitative image corrected based on injection dose and subject’s body weight [standardized uptake value (SUV)] for data analysis.
FDG PET and FES PET image analysis
FDG PET images were qualitatively evaluated by two reviewers who were blinded to all clinical data. An equivalent and slightly higher FDG accumulation than physiological liver uptake was considered to be an “equivocal” finding on FDG PET. FDG uptake that was clearly higher than the physiological liver uptake was defined as a “positive” FDG PET finding. Those patients with “equivocal” or “positive” findings on FDG PET were referred for FES PET.
Quantitative estimation of lesions on the FDG and FES PET images was performed. Attenuation-corrected PET images and MR images were displayed together on a picture archiving and communication system workstation. For quantitative analysis, circular regions of interest (ROIs) with a fixed size of 8 mm in diameter were drawn on the lesions in order to obtain local SUV. Individual MR images were referenced for placement of ROIs in the appropriate region after PET and MR images were coregistered (Body Guide, Advance Biologic Co., Toronto, Canada). ROIs were placed on the resliced MRI sections after coregistration of three images in each patient and the same ROIs were applied to the FES and FDG PET images. A total of four sagittal or coronal planes of 6-mm thickness were used to obtain the SUV at the centre of the tumour. Substantial partial volume effects on the mean SUV value were expected, and SUVs for each patient were thus averaged for the FDG and FES PET images. The ratio of mean FDG/FES SUVs for each lesion was also calculated [16].
Histopathological evaluation
The pathologist was blinded to all clinical data when reviewing the histopathology of surgically removed tumours. Uterine sarcomas were classified based on the World Health Organization histological classification system [17].
Statistical analysis
Quantitative estimation of uterine sarcomas was performed using SUV for FDG, FES and FDG to FES ratio. One-way analysis of variance (ANOVA) was used to determine whether there were significant differences in SUV between uterine sarcoma and leiomyoma. A p value of less than 0.05 was considered to indicate a statistically significant difference. Statistical analyses were performed using a software package (SPSS for Windows 11.5.1 J, SPSS Inc., Chicago, IL, USA). Receiver-operating characteristic (ROC) analysis was performed to determine the optimal cutoff value to differentiate uterine sarcoma and leiomyoma using PC software (MedCalc ver. 7.6.0.0, Mariakerke, Belgium). Sensitivity, specificity and accuracy were calculated with the optimal cutoff value considered positive, and differences in sensitivity and specificity among the imaging modalities were analysed using Cochran’s Q test [12]. The unpaired Student’s t test was used to test for significant differences in age, tumour size and SUV between uterine sarcoma and leiomyoma.
Results
Of the 24 study patients, final diagnoses were 11 uterine sarcomas and 13 leiomyomas. The characteristics of patients who underwent both FDG and FES PET, including histological subtype and tumour size, are summarized in Table 1, and the details of the 11 patients with uterine sarcoma are in listed Table 2. There were significantly older patients (p < 0.01) and a higher number of postmenopausal patients (p < 0.01) with uterine sarcoma than leiomyoma, but there was no significant difference in tumour size (p = 0.086) between uterine sarcoma and leiomyoma (Table 1). With regard to quantitative estimation of lesions on the FDG and FES PET images, there was significantly higher accumulation of FDG than FES accumulation in the patients with uterine sarcoma (p < 0.01). In contrast, there was significantly higher accumulation of FES than accumulation of FDG in patients with leiomyoma (p < 0.01). In addition, the FDG to FES SUV ratio was significantly different between uterine sarcoma and leiomyoma (p < 0.01) (Figs. 1 and 2, Table 3).
Box-and-whisker plots of tracer uptake in the two groups. Horizontal bars inside boxes indicate median values. Error bars indicate farthest points that are not outliers. Significant differences in FDG accumulation were observed between uterine sarcoma and leiomyoma (p < 0.01) a FES PET showed significant differences between the two groups (p < 0.01) b Box-and-whisker plots of the FDG to FES SUV ratio between the two groups. Significant differences were observed between uterine sarcoma and leiomyoma (p < 0.01) (c)
a FDG PET images (a), FES PET images (b) and sagittal T2-weighted MRI (c) of a 75-year-old woman with leiomyosarcoma. PET images showed positive FDG accumulation (SUV 10.5) (arrow) (a) and negative accumulation of FES (arrow) (SUV 1.0) (c) in the primary tumour lesion of the uterus. The FDG to FES ratio was 10.5. Sagittal T2-weighted MRI showed a uterine mass with heterogeneous high signal intensity (arrow). Postoperative histopathological results confirmed leiomyosarcoma. b FDG PET images (a), FES PET images (b) and axial T2-weighted MRI (c) of a 52-year-old woman with uncomplicated leiomyoma. PET images showed intense FDG uptake (SUV 6.2) (arrow) and intense FES uptake (SUV 8.2) (arrow) in the tumour, whereas the PET FDG to FES ratio was 0.75. Axial T2-weighted MRI showed a uterine mass with heterogeneous signal intensity (arrow). Postoperative histopathological results confirmed uncomplicated leiomyoma and adenomyosis
The optimal cutoff values to differentiate uterine sarcoma from leiomyoma were FDG SUV, FES SUV and FDG to FES SUV ratios more than 3, less than 2.5 and more than 2, respectively. There were two false-positive (leiomyoma with adenomyosis and haemorrhagic cellular variant leiomyoma) and two false-negative (low -grade ESS and LMS) results obtained for FDG SUV, four false-positive (three myxoid variant leiomyomas and one leiomyoma with adenomyosis) and two false-negative (two low-grade ESS) results obtained for FES SUV, and one false-negative (low-grade ESS) and one false-positive result (leiomyoma with adenomyosis) obtained for FDG/FES SUV. The sensitivity, specificity and accuracy that were calculated for each modality using optimal cutoff values that were considered malignant are summarized in Table 4. When an FDG to FES SUV ratio of 2.0 was the cutoff for uterine sarcoma, ROC analysis revealed 90.9% sensitivity and 92.3% specificity, respectively. When significance was found using Cochran’s Q test (p = 0.024), the sensitivity, specificity and accuracy of the FDG to FES SUV ratio was higher than that of FDG PET alone (90.9 vs 81.8%, 92.3 vs 84.6% and 91.3 vs 83.3%, respectively) (Table 4). Although, when the combination of FDG and FES indicated high accuracy for differentiating uterine sarcoma from leiomyoma, a false-negative case was found for one low-grade ESS and a false-positive case was found for one leiomyoma with adenomyosis. For the false-negative case, age was 38 years, tumour size was 2.5 cm, and FDG SUV was 2.9, FES SUV was 3.0 and FDG/FES was 0.9 (Table 3). For the false-positive case, age was 47 years, tumour size was 7 cm, and FDG SUV was 6.2, FES SUV was 1.79 and FDG/FES was 3.46.
Discussion
To our knowledge, this study is the first to demonstrate that additional FES PET findings can identify disease in patients with uterine sarcoma when FDG PET findings show equivocal or positive uptake. The high diagnostic accuracy with regional FDG/FES for uterine sarcoma supports the potential clinical use of additional PET imaging trials using FES in the workup of incidentally discovered “suspected uterine sarcoma” based on FDG PET findings.
FDG uptake on PET has been correlated with cells metabolizing glucose, but it is not specific for malignant transformation [11]. This lack of specificity is a potential problem in identifying malignant uterine sarcoma [12]. In the present FDG PET imaging analysis, FDG uptake of uterine sarcoma was significantly higher when compared with benign leiomyoma; however, there were some overlapping cases. It has previously been reported that increased FDG uptake is occasionally observed in some leiomyomas, and these overlapping cases have created some diagnostic and medical treatment problems [12]. In clinical settings, patients who receive a false-positive diagnosis may be subject to unnecessary worry and emotional trauma, particularly in cases of uterine masses for which preoperative histological diagnosis may present practical difficulties.
Additional FES PET has the potential to provide functional information about ER activity and to exclude malignancy in cases of benign leiomyoma with marked FDG accumulation. In an immunohistochemical study, almost 100% expression of ER was detected in leiomyomas, as uterine leiomyomas are defined as oestrogen-dependent benign tumours [18]. In the present study, there was a significantly higher accumulation of FES than FDG accumulation. In other words, leiomyoma showed FES accumulation, which could potentially provide functional information about ER activity.
With regard to ER expression in immunohistochemical studies, the criteria for considering whether there is positive ER expression have varied slightly between reports [18–22]. The prevalence of ER expression cited in the literature is almost 50% for LMS and 30–35% for CS [18–22]. Mittal and Demopoulos noted a significantly lower mean percentage of positive ER expression in LMS when compared with leiomyoma [21]. The rate of ER expression in uterine LMSs is thus lower than in leiomyomas, but some uterine LMSs still express ER. These observations suggest that patients with LMS can be managed medically with at least modest success using hormonal therapies, such as progestational agents and selective ER modulators. However, hormonal therapy is not effective in LMS patients. There have been a few reports of LMS cases responding to medroxyprogesterone, an aromatase inhibitor [22, 23]. This suggests that the immunohistochemical detection of ER in LMS represents nonfunctional ER expression. The two patients with low-grade ESS showed accumulation findings on FES PET. Several clinical observations have shown that ESS expresses ER and is sensitive to hormonal treatment, in contrast to LMS and CS [22, 24, 25]. A recent PET and immunohistochemistry study confirmed the relationship between FES uptake and expression of ERα in endometrial cancer [26]. Furthermore, it was reported that the FDG to FES ratio, which reflects glucose metabolism relative to ERα density, is significantly correlated with progesterone receptor B (PR-B) expression. This indicates that the FDG to FES ratio can be used as a functional ERα and PR index; PR production is regulated by the oestrogen-ER complex, and expression of PR suggests that regulation is functioning normally [27]. However, the expression of ER in ESS, particularly low-grade ESS, is thought to be normal and is commonly observed, and this makes the “FDG to FES SUV ratio greater than 2.0” a futile index in the diagnosis of ESS. In fact, in this study, one of the two ESS cases was a false-negative according to criteria for uterine sarcoma based on “FDG to FES SUV ratio greater than 2.0”. Thus, we should take into consideration the limitations of this index in the diagnosis of ESS.
In this study, all of the patients underwent hysterectomy and underwent FES PET within 2 weeks prior to surgery. Histopathological diagnosis of surgical specimens is the “gold standard”, and sarcomas such as low-grade ESS on preoperative endometrial Pap test have a differential diagnosis that includes a number of benign conditions, including normally shed endometrial cells, endometriosis and submucosal leiomyoma, and it is impossible to render a definitive diagnosis based on curettage material examinations [28]. Although the diagnosis of CS may be missed because endometrial biopsy or curettage does not adequately sample both the epithelial and stromal components of the tumour, appropriate preoperative referral is necessary because of the presence of a malignancy, and staging is accomplished at the time of hysterectomy [29]. However, Oda et al. reported that some cases were covered with marked necrosis and that the presence of a malignancy was not diagnosed [30]. In fact, in all three of the present CS cases, the presence of a malignancy was missed on preoperative endometrial Pap tests, despite abnormal genital bleeding. All preoperative endometrial Pap tests were covered with marked necrosis and the presence of malignancy was missed. In our two low-grade ESS patients, one patient was postmenopausal with abdominal pain, and her preoperative Pap smear showed benign cytology. The other patient was premenopausal with abnormal genital bleeding, and her preoperative Pap test and curettage material indicated benign cellular leiomyomas. This supports the notion that final diagnosis for uterine sarcomas requires hysterectomy specimens.
As for the timing of FES PET, our previous preliminary study indicated, in premenopausal patients, FES accumulation of uterine myometrium and some leiomyomas is slightly affected by the menstrual cycle [31]. This is the reason why patients underwent FES PET within 2 weeks prior to surgery.
Our study had a number of limitations. First, the present study did not aim to directly compare the performance of FDG PET and FES PET, but rather to assess the clinical utility of FES PET in a specific subset of uterine tumour patients showing equivocal or positive uptake on FDG PET. Second, the small sample size of 11 uterine sarcoma patients in this study, including LMS, CC and ESS, has to be regarded as a limitation. Although we cannot conclude with any certainly that a combination of FES PET and FDG PET is useful for preoperative diagnosis of uterine sarcomas, in these patients, it was clearly demonstrated that FES PET directly affects the diagnosis of uterine sarcomas. The role of FES PET appears to be detection of functional ER in the clinical diagnosis of uterine sarcomas; thus, FES PET may be used to assess the suitability of treatment with hormonal therapies (such as progestational agents, selective ER modulators and gonadotropin-releasing hormone agonists).
In conclusion, additional FES PET findings can decrease the number of false-positive FDG PET findings and may reduce unnecessary worry and emotional trauma. To decrease unnecessary surgery and to establish a noninvasive evaluation method for risk management in patients with uterine tumour, further PET studies with a larger patient population and long-term follow-up are necessary.
References
Adams Hillard PJ. Benign disease of the female reproductive tract. In: Berek JS, editor. Berek & Novak’s gynecology. 14th ed. Philadelphia: Lippincott Williams & Wilkins; 2006. p. 431–504.
Sutton GP, Stehman FB, Michael H, Young PC, Ehrlich CE. Estrogen and progesterone receptors in uterine sarcomas. Obstet Gynecol 1986;68:709–14.
Amant F, Coosemans A, Debiec-Rychter M, Timmerman D, Vergote I. Clinical management of uterine sarcomas. Lancet Oncol 2009;10:1188–98.
Milman D, Zalel Y, Biran H, Open M, Caspi B, Hagay Z, et al. Unsuspected uterine leiomyosarcoma discovered during treatment with a gonadotropin-releasing hormone analogue: a case report and literature review. Eur J Obstet Gynecol Reprod Biol 1998;76:237–40.
Wallach EE, Vlahos NF. Uterine myomas: an overview of development, clinical features, and management. Obstet Gynecol 2004;104:393–406.
Parker WH. Uterine myomas: management. Fertil Steril 2007;88:255–71.
Schwartz LB, Zawin M, Carcangiu ML, Lange R, McCarthy S. Does pelvic magnetic resonance imaging differentiate among the histologic subtypes of uterine leiomyomata? Fertil Steril 1998;70:580–7.
Sahdev A, Sohaib SA, Jacobs I, Shepherd JH, Oram DH, Reznek RH. MR imaging of uterine sarcomas. AJR Am J Roentgenol 2001;177:1307–11.
Kido A, Togashi K, Koyama T, Yamaoka T, Fujiwara T, Fujii S. Diffusely enlarged uterus: evaluation with MR imaging. Radiographics 2003;23:1423–39.
Tanaka YO, Nishida M, Tsunoda H, Okamoto Y, Yoshikawa H. Smooth muscle tumors of uncertain malignant potential and leiomyosarcomas of the uterus: MR findings. J Magn Reson Imaging 2004;20:998–1007.
Rohren EM, Turkington TG, Coleman RE. Clinical applications of PET in oncology. Radiology 2004;231:305–32.
Yoshida Y, Kurokawa T, Sawamura Y, Shinagawa A, Tsujikawa T, Okazawa H, et al. Comparison of 18F-FDG PET and MRI in assessment of uterine smooth muscle tumors. J Nucl Med 2008;49:708–12.
Kitajima K, Murakami K, Kaji Y, Sugimura K. Spectrum of FDG PET/CT findings of uterine tumors. AJR Am J Roentgenol 2010;195:737–43.
Tsujikawa T, Yoshida Y, Mori T, Kurokawa T, Fujibayashi Y, Kotsuji F, et al. Uterine tumors: pathophysiologic imaging with 16alpha-[18F]fluoro-17beta-estradiol and 18F fluorodeoxyglucose PET–initial experience. Radiology 2008;248:599–605.
Mori T, Kasamatsu S, Mosdzianowski C, Welch MJ, Yonekura Y, Fujibayashi Y. Automatic synthesis of 16 alpha-[(18)F]fluoro-17beta-estradiol using a cassette-type [(18)F]fluorodeoxyglucose synthesizer. Nucl Med Biol 2006;33:281–6.
Tsujikawa T, Yoshida Y, Kudo T, Kiyono Y, Kurokawa T, Kobayashi M, et al. Functional images reflect aggressiveness of endometrial cancer: estrogen receptor expression combined with 18FDG PET. J Nucl Med 2009;50:1598–604.
Gompel C, Silverberg SG. Pathology in gynecology and obstetrics. 4th ed. Philadelphia: Lippincott Williams & Wilkins; 1994. p. 163–283.
Bodner K, Bodner-Adler B, Kimberger O, Czerwenka K, Leodolter S, Mayerhofer K. Estrogen and progesterone receptor expression in patients with uterine leiomyosarcoma and correlation with different clinicopathological parameters. Anticancer Res 2003;23:729–32.
Leitao MM, Soslow RA, Nonaka D, Olshen AB, Aghajanian C, Sabbatini P, et al. Tissue microarray immunohistochemical expression of estrogen, progesterone, and androgen receptors in uterine leiomyomata and leiomyosarcoma. Cancer 2004;101:1455–62.
Zhai YL, Kobayashi Y, Mori A, Orii A, Nikaido T, Konishi I, et al. Expression of steroid receptors, Ki-67, and p53 in uterine leiomyosarcomas. Int J Gynecol Pathol 1999;18:20–8.
Mittal K, Demopoulos RI. MIB-1 (Ki-67), p53, estrogen receptor, and progesterone receptor expression in uterine smooth muscle tumors. Hum Pathol 2001;32:984–7.
Ioffe YJ, Li AJ, Walsh CS, Karlan BY, Leuchter R, Forscher C, et al. Hormone receptor expression in uterine sarcomas: prognostic and therapeutic roles. Gynecol Oncol 2009;115:466–71.
Uchida T, Nakakawaji K, Sakamoto J, Kojima H, Murakami H, Kato J, et al. The effectiveness of medroxyprogesterone in the treatment of multiple metastasizing leiomyosarcomas: report of a case. Surg Today 1996;26:138–41.
Tsujikawa T, Yoshida Y, Kiyono Y, Kurokawa T, Kudo T, Fujibayashi Y, et al. Functional oestrogen receptor alpha imaging in endometrial carcinoma using 16alpha-[(18)F]fluoro-17beta-oestradiol PET. Eur J Nucl Med Mol Imaging 2011;38(1):37–45.
Conneely OM, Lydon JP, De Mayo F, O’Malley BW. Reproductive functions of the progesterone receptor. J Soc Gynecol Investig 2000;7:S25–32.
Zhu XQ, Shi YF, Cheng XD, Zhao CL, Wu YZ. Immunohistochemical markers in differential diagnosis of endometrial stromal sarcoma and cellular leiomyoma. Gynecol Oncol 2004;92:71–9.
Kir G, Cetiner H, Karateke A, Gurbuz A, Bulbul D. Utility of MIB-1 and estrogen and progesterone receptor in distinguishing between endometrial stromal sarcomas and endometrial stromal nodules, highly cellular leiomyomas. Int J Gynecol Cancer 2005;15:337–42.
Policarpio-Nicolas ML, Cathro HP, Kerr SE, Stelow EB. Cytomorphologic features of low-grade endometrial stromal sarcoma. Am J Clin Pathol 2007;128:265–71.
Gregory S, John K, Aaron W, Carmen T. Corpus: mesenchymal tumors. In: Barakat RR, editor. Principles and practice of gynecologic oncology. 4th ed. Philadelphia: Lippincott Williams & Wilkins; 2009. p. 733–61.
Oda K, Okada S, Nei T, Shirai T, Takahashi M, Sano Y, et al. Cytodiagnostic problems in uterine sarcoma. Analysis according to a novel classification of tumor growth types. Acta Cytol 2004;48:181–6.
Tsuchida T, Okazawa H, Mori T, Kobayashi M, Yoshida Y, Fujibayashi Y, et al. In vivo imaging of estrogen receptor concentration in the endometrium and myometrium using FES PET—influence of menstrual cycle and endogenous estrogen level. Nucl Med Biol 2007;34:205–10.
Acknowledgments
This study was partly funded by the Research and Development Project Aimed at Economic Revitalization (Leading Project) from MEXT Japan, Grants-in-Aid for Scientific Research (Nos. 20790887 and 21390342) and the 21st Century Center of Excellence Program from the Japan Society for the Promotion of Science.
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Yoshida, Y., Kiyono, Y., Tsujikawa, T. et al. Additional value of 16α-[18F]fluoro-17β-oestradiol PET for differential diagnosis between uterine sarcoma and leiomyoma in patients with positive or equivocal findings on [18F]fluorodeoxyglucose PET. Eur J Nucl Med Mol Imaging 38, 1824–1831 (2011). https://doi.org/10.1007/s00259-011-1851-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00259-011-1851-8