Abstract
Purpose
Since 2006, the working group Cardiovascular Nuclear Medicine of the German Society of Nuclear Medicine, in cooperation with the working group Nuclear Cardiology of the German Cardiac Society, has been surveying the utilization and technical realization of myocardial perfusion scintigraphy (MPS) in Germany. This paper presents the results of the reporting year 2009.
Methods
A total of 291 centres participated in the inquiry, including 179 private practices (PP), 86 hospitals (HO) and 26 university hospitals (UH).
Results
MPS of 98,103 patients were reported. The MPS numbers per million population (pmp) were estimated at 2,360; 76% of the MPS were performed in PP, 17% in HO and 7% in UH. The ratio of MPS to coronary angiography to revascularization was 0.5 to 2.3 to 1. Data from 134 centres which participated in the surveys from 2005 to 2009 showed a decrease in MPS utilization of 2.2%. Nearly half of the MPS were requested by ambulatory care cardiologists. Of all MPS studies, 89% were conducted with 99mTc perfusion tracers. Ergometry was the preferred stress test (69%). Adenosine was used in 16%, adenosine + exercise in 7%, dipyridamole in 3%, dipyridamole + exercise in 5% and dobutamine in <1%. Gated single proton emission computed tomography (SPECT) acquisition was performed in 56% of all rest MPS and in 56% of all stress MPS. Both rest and stress MPS were ECG gated in 41%. Only 33% of the centres always performed a quantification of the perfusion studies, whereas 51% did not apply any quantification; 4% of the MPS studies were corrected for attenuation, and 17 centres used transmission sources of 12 CT-based systems.
Conclusion
A scan activity of 2,380 MPS pmp is in the upper third of the European range. The ratios to coronary angiography and to revascularization suggest that angiography dominates diagnosis and management of coronary artery disease (CAD). The clinical and technical realizations reveal that the predominant goals of further trainings to optimize MPS are in the field of gated SPECT and quantitative perfusion SPECT.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Myocardial perfusion scintigraphy (MPS) is a well-established diagnostic tool with an excellent database which provides effective diagnostic, prognostic and therapy-guiding information in patients with both known and suspected coronary artery disease (CAD) [1–3]. Data about the routine use and current practice of MPS studies are rare, but of growing interest in times of health economics. The last European survey was published in 2008 for the reporting year 2005 [4].
In order to obtain reliable information on technique, practice, utilization and development of MPS, the working group Cardiovascular Nuclear Medicine of the German Society of Nuclear Medicine, in cooperation with the working group Nuclear Cardiology of the German Cardiac Society, projected a regular survey in 2006 and here presents the results of the inquiry for the reporting year 2009. The results of the former surveys have been published in German elsewhere [5–8].
Germany is the most populous country in Europe; thus, the current German MPS survey may also represent typical European MPS features of daily routine practice.
The German healthcare system can be briefly characterized as follows: The system is decentralized, with private practice physicians providing ambulatory care, and independent, mostly nonprofit hospitals providing the majority of inpatient care. Outpatient services supplied to the public are largely the responsibility of independent physicians practising on a freelance basis under contract to the statutory health insurance companies. The level of reimbursement for specific services is based on a medical fee schedule and in detail determined through negotiations between regional physicians’ associations and sickness funds. Approximately 90% of the population is covered by statutory health insurance funds which provide a standardized level of coverage. Higher income employees can opt out of the standard plan in favour of private insurance.
Materials and methods
Based on the register of members of the Germany Society of Nuclear Medicine, registers of office-based nuclear medicine physicians of the 17 state chambers of physicians, the German Yellow Pages® and the German hospitals’ address book, in total 888 potential centres/persons practising nuclear medicine were identified.
A one-page questionnaire with a cover letter was sent by fax at the beginning of May 2010. In cases of no response a reminder was forwarded 4 weeks later. A second and last reminder was sent after the summer holidays. The survey was closed at the end of October 2010.
The questionnaire comprised: (1) number of patients studied with MPS, (2) number of stress and rest MPS, (3) stress techniques, (4) MPS radiopharmaceuticals, (5) MPS protocols, (6) utilization of gated single proton emission computed tomography (SPECT), (7) utilization of attenuation correction and finally (8) the referral structure.
The survey data were related to the figures of the National Association of Statutory Health Insurance Physicians (NASHIP) [Kassenärztliche Bundesvereinigung (KBV)], which represents the number of outpatient services of private practices and hospitals within the statutory health system, to reliably estimate the total MPS numbers. Unfortunately, data from private insurance companies are not available.
Due to the partially competitive relations among and within healthcare institutions (private practices and hospitals), the population size served by different centres may largely overlap. Furthermore, estimates of populations served are often vague. To avoid any bias with respect to these issues, the MPS numbers were only related to the total population size after adjustment to the NASHIP statistics.
Results
The first figures given in squared brackets refer to the reporting year 2008 (survey realized in 2009), followed by the figures of the reporting year 2005 (first survey realized in 2006).
Returns were obtained from 393 centres, with 102 responders not undergoing MPS studies. The data returned refer to 291 [310; 346] centres: 179 [191; 213] private practices (PP)—5 of them cardiologists with a focus on nuclear cardiology—86 [93; 99] hospitals (HO) and 26 [26; 34] university hospitals (UH).
Among the centres, 59 were new responders and 77 participating in the last inquiry chose not to respond this time.
MPS activity
The number of patients studied with MPS was 98,103 [98,947; 112,707]; 96,566 [96,508; 110,747] stress MPS and 85,577 [84,133; 95,878] rest MPS were conducted. In the case of 201Tl, the stress and the corresponding redistribution study were counted as one stress and one rest study; 76% [77%; 72%] of all patients were studied in PP, 17% [15%; 15%] in HO and 7% [8%; 13%] in UH. The average MPS patient number was 421 [398; 379] in PP, 190 [159; 170] in HO and 263 [312; 437] in UH.
The range of patient numbers was 1–3,673 [2–3,788; 5–3,577] in PP, 1–2,000 [1–1,400; 1–729] in HO and 10–965 [36–1,067; 32–1,215] in UH.
The NASHIP reports 132,412 stress MPS and 114,109 rest MPS in 2009 [9]. Given a 10% proportion of privately insured patients and 15% of hospital studies that are not covered by the NASHIP figures, it may be concluded that this survey represents about 50–55% of all MPS studies or that the “true” figures are about twice as high.
Therefore, the MPS figures were multiplied by 2 to reliably estimate the coronary angiography to MPS ratio and to calculate the population-based MPS activity. By this approach the ratios tend to be mildly overestimated.
The MPS patient numbers per million people (pmp) and the angiography to MPS ratios are shown in Table 1. On the regional basis of the German Federal States, the range of these data was 1,290–5,220 MPS pmp and 2.4–14 angiography/MPS.
MPS patient figures from 2005 to 2009
A total of 230 centres (142 PP, 67 HO, 21 UH) participated in both the 2008 and 2009 inquiries. Their MPS figures changed by −2.1% (PP −2.2%, HO −3.8%, UH +3.1%).
From 2005 to 2009 continuous data from 134 centres (80 PP, 36 HO, 18 UH) are available. They demonstrate an overall decrease of 2.2%, which was most obvious in UH (31.9%). However, the MPS patient figures increased by 1.5% in PP and by 4.5% in HO (Fig. 1).
Protocols and radiopharmaceuticals
The utilization of typical study protocols is given in Table 2 and Fig. 2. Furthermore, Table 2 lists the effective doses that result from the German diagnostic reference levels by implementation of the Euratom Directive [10, 11].
In 2009, 89% [88%; 80%] of the MPS studies were conducted with 99mTc radiopharmaceuticals. A 2-day protocol was realized in 63% [63%; 60%] of the stress-rest 99mTc MPS studies and accordingly a 1-day protocol in 37% [37%; 40%]. Only 18 [26; 54] centres exclusively applied 201Tl for MPS. Dual isotope imaging plays no role, as shown before, and was therefore not inquired [5].
Stress techniques
Utilization of the different stress techniques is summarized in Table 3 and Fig. 3. Dynamic exercise stress remains the most frequent stress test; 72% [68%] of pharmacological tests were conducted with adenosine, and 31% [22%] of these with adenosine and low-level exercise as an adjunct. Dipyridamole was used in 26% [29%] of all pharmacological tests and in 64% [64%] combined with exercise. In 2005, data of adenosine and dipyridamole were not requested.
Attenuation correction
Only 4% of the MPS studies reported were corrected for attenuation. This technique was most widely applied in UH (46%) vs19% in HO and 4% in PP; 17 centres used transmission sources and 12 CT-based systems. Three centres had both techniques available. Thirty-two centres applied prone-supine imaging in order to identify attenuation artefacts.
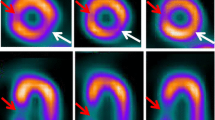
Quantitative scoring and gated SPECT
The frequency of quantification of SPECT perfusion images with summed stress, summed rest and summed difference scores is listed in Table 4 and Fig. 4. About 50% of the centres did not generate perfusion scores at all.
The utilization of gated SPECT as an important adjunct to myocardial perfusion SPECT showed a considerable increase (Table 5 and Fig. 5). Gated SPECT was most widely used in the UH.
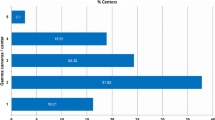
MPS referrals
The referral structure is shown in Table 6 and Fig. 6. Nearly half of the MPS were requested by ambulatory care cardiologists, who represent the major referral group.
Discussion
This survey gives an overview of the utilization of MPS as a diagnostic imaging tool in CAD and tracks the state of MPS practice in Germany in 2009. Representing about 20% of the European population, the German MPS figures may also reflect European MPS practice. It is important to consider that this survey represents average and routine use of MPS over a broad spectrum of users, not exclusively high-end users.
The representativeness of the survey was verified by the data from NASHIP, which covers reimbursed services of statutory outpatient care. Based on these numbers, about 50–55% of all MPS could be surveyed. Thus, the results of this survey can be regarded as representative.
The last European survey (reporting year 2005) was published in 2008 and included only 21 German centres [4]. The present survey is more representative and encompasses with 291 participants more centres than the European study.
The key issues of this survey are:
-
1.
In 2009 about 2,380 MPS pmp were performed in Germany. Comparing this figure with the 2005 European survey, the estimated 2,380 MPS pmp are in the upper third of the high utilization countries. It should be emphasized that the German and European MPS figures are in stark contrast to more than 30,000 MPS pmp reported in the USA in 2005 [4]. One reason is certainly the clear interdisciplinary cut between cardiology and nuclear medicine in Germany and other European countries. Only five ambulatory care cardiologists practice nuclear cardiology imaging themselves. Interestingly, these are high utilization centres with annual MPS rates of up to 3,600.
-
2.
An average coronary angiography to MPS ratio of 4.4 is substantially higher than the European ratio of 2.5. Furthermore, a large regional variation of 2–10 is found throughout Germany. A ratio of 0.5 to 0.6 MPS to each revascularization is low, but within the European range. The ratios relativize the high MPS utilization status and suggest that angiography dominates CAD diagnosis and that many interventions are performed without knowledge of myocardial perfusion. This trend is increasing over time and has remained unaltered despite the results of the COURAGE trial, which demonstrated no general benefit of a percutaneous intervention in patients with stable CAD to optimal medical therapy [12]. The COURAGE subanalysis revealed that the amount of ischaemia plays a dominant role in preventing cardiac events and led to the former results that an ischaemic burden > 10–12% (as defined by quantitative analysis) favours an interventional therapy [2, 13]. Therefore, functional imaging like MPS is of crucial importance guiding diagnosis and therapy in CAD.
Current numbers of stress echocardiograms are not available, but it is unlikely that they would have a basic impact on the angiography to functional imaging ratio. The same applies to the numbers of other noninvasive imaging techniques, such as CT angiography and cardiac MRI. They are certainly low because they are not yet reimbursed by the statutory health insurance companies.
The angiography to revascularization ratio of 2.3 indicates that patient preselection for angiography is crude and probably a consequence of the imbalance between functional and morphological imaging.
-
3.
The MPS figures reveal considerable shifts since 2005. The most striking drops were noticed in the UH, certainly motivated by a shift to preclinical outpatient diagnosis and a focus on new imaging technologies with direct access to cardiology departments. PP and HO showed mild increases in MPS activities from 2005 to 2009 and a higher patient number per centre. However, overall MPS activity is mildly declining. The key reasons for this, despite the excellent scientific MPS database, are an increasing pressure to save costs and a preference for angiography.
-
4.
About half of the MPS studies are directly requested by ambulatory care cardiologists, with only mild changes in the past 5 years, suggesting that MPS has a defined role in CAD diagnosis and management. Only 15% of MPS are related to inpatient diagnosis. This proportion has decreased since 2005 and thus demonstrates the shift from inpatient to outpatient diagnosis.
-
5.
201Tl MPS studies are further decreasing to currently 11%. This is a favourable trend in terms of radiation exposure for patients. Furthermore, the preferred use of 2-day 99mTc MPS studies, which allows the application of lower doses than with 1-day protocols, indicates another approach to lower radiation doses for patients. With regard to the ongoing discussion on radiation exposure for patients by MPS, the German/European data show that the doses are considerably lower than in the USA [14].
-
6.
A 13% proportion of stress-only MPS studies appears to be low. As about 40% of MPS are related to patients without known CAD or suspected CAD, a higher amount of stress-only studies could be expected, especially in private practices [6]. This will be one goal of further education regarding patients’ radiation exposure and healthcare costs.
-
7.
Ergometry is the most common stress test. The proportion of pharmacological stress tests is increasing. Adenosine is the leading agent because dipyridamole is not approved for MPS in Germany and can only be applied in single cases decided by the responsible nuclear medicine physician. The number of vasodilator stress tests combined with low-level ergometry should further increase, due to the lower rate of side effects and a better image quality [15]. The increasing rates of pharmacological tests suggest that more and more patients are unable to exercise maximally. In these patients pharmacological stress testing is superior and enables a reliable diagnostic approach to CAD. Pharmacological tests are more frequently conducted in HO and UH than in PP, indicating a higher proportion of elderly patients and patients with comorbidities in these centres.
-
8.
A measured attenuation correction with transmission sources or with CT is rarely realized and only implemented in 11% of the centres. The amount of CTs for attenuation is slightly higher than that of transmission sources. Prone-supine imaging is more widely applied for the detection of attenuation artefacts.
-
9.
Of all MPS studies, 56% are realized as gated SPECT. This proportion is still lower than the European average of 65% [4]. Starting with a proportion of only 35% in 2005, this constitutes favourable progress and a further motivation to continue training. Both the stress and the rest studies should be acquired as gated SPECT. This technique delivers additional information on prognosis, on detection of three-vessel disease, and increases specificity [16–18]. As ECG gating is not reimbursed in Germany, this issue may also contribute to the still incomplete penetration of gated acquisitions in MPS.
-
10.
Another issue of training in nuclear cardiology is the underuse of quantitative SPECT analysis which refers to all types of centres. Data from the European survey concerning this issue are not available. Quantitative perfusion SPECT—realized visually or automatically with normal databases—should be applied to meet the full potential of MPS for risk stratification and therapeutic management. The quantitative analysis helps guide the decision for medical or interventional therapy, it further facilitates the classification of MPS patients to risk groups and it is helpful in the assessment of perfusion disturbances in follow-up studies [13, 19].
Conclusion
The Germany survey on MPS in 2009 reflects the complex and competitive context of MPS in the field of cardiac imaging. Furthermore, this survey reveals the work which still needs to be done in order to implement and conduct MPS optimally, but it also demonstrates that steps ahead have already been taken.
References
Sharples L, Hughes V, Crean A, Dyer M, Buxton M, Goldsmith K, et al. Cost-effectiveness of functional cardiac testing in the diagnosis and management of coronary artery disease: a randomised controlled trial. The CECaT trial. Health Technol Assess 2007;11:iii-iv, ix-115.
Shaw LJ, Iskandrian AE. Prognostic value of gated myocardial perfusion SPECT. J Nucl Cardiol 2004;11:171–85.
Hesse B, Tägil K, Cuocolo A, Anagnostopoulos C, Bardiés M, Bax J, et al. EANM/ESC procedural guidelines for myocardial perfusion imaging in nuclear cardiology. Eur J Nucl Med Mol Imaging 2005;32:855–97.
Underwood SR, Wiener S. Myocardial perfusion scintigraphy in Europe 2005: a survey of the European Council on Nuclear Cardiology. Eur J Nucl Med Mol Imaging 2009;36:260–8.
Lindner O, Burchert W, Bengel FM, Zimmermann R, Vom Dahl J, Schäfer W, et al. Myocardial perfusion scintigraphy in Germany. Results of the 2005 query and current status. Nuklearmedizin 2007;46:49–55.
Lindner O, Burchert W, Bengel FM, Zimmermann R, Vom Dahl J, Schäfer W, et al. Myocardial perfusion scintigraphy 2006 in Germany. Results of the query and current status. Nuklearmedizin 2008;47:139–45.
Lindner O, Burchert W, Bengel F, Zimmermann R, Vom Dahl J, Schäfer W, et al. Myocardial perfusion scintigraphy 2007 in Germany—results of the query and current status. Nuklearmedizin 2009;48:131–7.
Lindner O, Burchert W, Bengel FM, Zimmermann R, Vom Dahl J, Schäfer W, et al. Myocardial perfusion scintigraphy 2008 in Germany—results of the fourth query. Nuklearmedizin 2010;49:65–72.
Mitteilung der KBV (Communication of the NASHIP). KBV Abrechnungsstatistik (Reimbursement Statistics of the NASHIP). 2010.
The Council of the European Union. Council Directive 97/43/Euratom of 30 June 1997 on health protection of individuals against the dangers of ionizing radiation in relation to medical exposure, and repealing Directive 84/466/Euratom. Off J Eur Commun 1997;180:22–7.
Bundesamt für Strahlenschutz (Federal Office for Radiation Protection). Bekanntmachung der diagnostischen Referenzwerte für radiologische und nuklearmedizinische Untersuchungen. 10 July 2003.
Boden WE, O’Rourke RA, Teo KK, Hartigan PM, Maron DJ, Kostuk WJ, et al. Optimal medical therapy with or without PCI for stable coronary disease. N Engl J Med 2007;356:1503–16.
Hachamovitch R, Hayes SW, Friedman JD, Cohen I, Berman DS. Comparison of the short-term survival benefit associated with revascularization compared with medical therapy in patients with no prior coronary artery disease undergoing stress myocardial perfusion single photon emission computed tomography. Circulation 2003;107:2900–7.
Berrington de Gonzalez A, Kim KP, Smith-Bindman R, McAreavey D. Myocardial perfusion scans: projected population cancer risks from current levels of use in the United States. Circulation 2010;122:2403–10.
Hashimoto A, Palmar EL, Scott JA, Abraham SA, Fischman AJ, Force TL, et al. Complications of exercise and pharmacologic stress tests: differences in younger and elderly patients. J Nucl Cardiol 1999;6:612–9.
Taillefer R, DePuey EG, Udelson JE, Beller GA, Latour Y, Reeves F. Comparative diagnostic accuracy of Tl-201 and Tc-99m sestamibi SPECT imaging (perfusion and ECG-gated SPECT) in detecting coronary artery disease in women. J Am Coll Cardiol 1997;29:69–77.
Sharir T, Bacher-Stier C, Dhar S, Lewin HC, Miranda R, Friedman JD, et al. Identification of severe and extensive coronary artery disease by postexercise regional wall motion abnormalities in Tc-99m sestamibi gated single-photon emission computed tomography. Am J Cardiol 2000;86:1171–5.
Hachamovitch R, Rozanski A, Hayes SW, Thomson LE, Germano G, Friedman JD, et al. Predicting therapeutic benefit from myocardial revascularization procedures: are measurements of both resting left ventricular ejection fraction and stress-induced myocardial ischemia necessary? J Nucl Cardiol 2006;13:768–78.
Hachamovitch R, Berman DS, Shaw LJ, Kiat H, Cohen I, Cabico JA, et al. Incremental prognostic value of myocardial perfusion single photon emission computed tomography for the prediction of cardiac death: differential stratification for risk of cardiac death and myocardial infarction. Circulation 1998;97:535–43.
Bruckenberger E. Herzbericht 2009 mit Transplantationschirurgie (22. Bericht); 2010.
Bruckenberger E. Herzbericht 2008 mit Transplantationschirurgie (21. Bericht); 2009.
Bruckenberger E. Herzbericht 2005 mit Transplantationschirurgie (18. Bericht); 2006.
ICRP Publication 80. Radiological protection in biomedical research. Ann ICRP vol 28/3, Pergamon Press; 1998.
Acknowledgements
The authors wish to thank all participating centres for their time and effort contributing to this survey. They also thank NASHIP for the delivery of MPS figures, and Mrs. Carola Thamar for revising this manuscript.
Conflicts of interest
None.
Author information
Authors and Affiliations
Consortia
Corresponding author
Additional information
Michael Schäfers and Wolfgang Burchert are Chairman/Vice-Chairman of the working group Cardiovascular Nuclear Medicine of the German Society of Nuclear Medicine
Wolfgang Burchert and Rainer Zimmermann are Chairman/Vice-Chairman of the working group Nuclear Cardiology of the German Cardiac Society
Rights and permissions
About this article
Cite this article
Lindner, O., Burchert, W., Bengel, F.M. et al. Myocardial perfusion scintigraphy in Germany in 2009: utilization and state of the practice. Eur J Nucl Med Mol Imaging 38, 1485–1492 (2011). https://doi.org/10.1007/s00259-011-1777-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00259-011-1777-1