Abstract
Purpose
For the treatment of cancer, the therapeutic potential of short-range, low-energy Auger-electron emitters, such as 125I, is getting progressively wider recognition. The potency of Auger-electron emitters is strongly dependent on their location in close vicinity to DNA. We have developed a new two-step targeting strategy to transport 125I into cancer-cell nuclei using PEG-stabilized tumour-cell targeting liposomes named “Nuclisome-particles”.
Methods
In the present study, epidermal growth factor (EGF) was used as a tumour-cell-specific agent to target the EGF-receptor (EGFR) and the liposomes were loaded with 125I-Comp1, a recently synthesized daunorubicin derivative.
Results
As analysed with cryo-TEM, the derivative precipitates inside liposomes at a drug-to-lipid molar ratio of 0.05:1. Receptor-specific uptake in cultured U-343MGaCl2:6 tumour cells of EGFR-targeting liposomes increased with time while non-specific and receptor-blocked uptake remained low. Nuclisome-particles were able to target single U-343MGaCl2:6 cells circulating in human blood during 4 h, with low uptake in white blood cells, as demonstrated in an ex vivo system using a Chandler loop. Autoradiography of targeted cells indicates that the grains from the radiolabelled drug are mainly co-localized with the cell nuclei. The successful targeting of the nucleus is shown to provide high-potency cell killing of cultured U-343MGaCl2:6 cells. At the concentration used, Nuclisome-particles were up to five orders of magnitude more effective in cell killing than EGFR-targeting liposomes loaded with doxorubicin.
Conclusion
The results thus provide encouraging evidence that our two-step targeting strategy for tumour cell DNA has the potential to become an effective therapy against metastasizing cancer cells in the bloodstream.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The efficacy of conventional cancer chemotherapy is often limited by side-effects such as bone marrow suppression, mucositis, cardiac-, neuro-, and nephro-toxicity, which preclude therapeutic drug levels from being reached at the tumour site [1]. Targeted drug delivery via liposomes attempts to minimize those dose-limiting side-effects by encapsulating the cytotoxic agent into lipid bilayer vesicles (liposomes) and attaching tumour-specific ligands to the liposome membrane (targeting liposomes). Tumour cells expressing the targeted surface marker are envisioned to actively internalize the liposomes and interaction of the drug with healthy tissue is thus foreseen to be minimised.
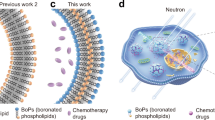
Despite some progress, existing strategies using targeting liposomes loaded with anticancer drugs have had so far only limited success in the treatment of cancer [2, 3]. Besides the tumour-cell targeting approach, our strategy includes a second targeting step to further direct the anti-tumour agent, in this case an Auger-emitting radionuclide, to its most potent site of action—the tumour-cell DNA. The aim of the second step is to boost the biological effect of Auger-emitting nuclides. The biological Auger effect is caused by local energy absorption of multiple low-energy electrons creating a complex double-strand break (DSB) in the DNA [4]. Due to this local effect, with most of the energy deposited within a few cubic nanometres around the site of decay, it is insufficient to target just the tumour cells—the DNA itself needs to be targeted. In fact, to obtain full effect, the radionuclide needs to decay within the DNA molecule either incorporated into the backbone or placed in between the strands.
Potential targets for targeting liposomes are the human epidermal growth factor receptors, essential mediators of cell proliferation and differentiation. The ErbB family comprises EGFR, HER2, HER3, and HER4 [5]. EGFR is a 170-kDa transmembrane glycoprotein normally expressed in epithelial, mesenchymal, and neuronal tissues [6]. The activation of the EGFR oncogene is involved in malignant transformation and tumour growth through cellular proliferation, inhibition of apoptosis, and promotion of angiogenesis and metastasis [7, 8]. EGFR can mediate the activation of the other members of the ErbB family emphasising its major role in tumour progression [9]. Deregulation and overexpression of the receptors are associated with the development of several malignant disorders including cancer of the lung, breast, colon, prostate, as well as squamous-cell cancer of the head and neck [7]. The EGFR ligand EGF is a single-chain 6-kDa polypeptide consisting of 53 amino acids that exerts a wide variety of biological effects, including the promotion of proliferation and differentiation of mesenchymal and epithelial cells [10]. Binding of EGF to EGFR but not any other member of the ErbB receptor family rapidly induces the clustering of ligand-receptor complexes in coated pits, followed by internalization of the complexes, and ultimately lysosomal degradation of both EGF and its receptor [11]. This rapid behaviour of the ligand-receptor complex, as well as the frequent and significant occurrence of overexpression of the receptor in many malignancies, makes the EGF-EGFR system a suitable model to analyse targeting liposomes. We have chosen this model system to demonstrate the efficacy of our concept. In ongoing studies we are, however, developing targeting liposomes also against other targets, such as HER2.
We have previously reported on PEG-stabilised EGFR-targeting liposomes as promising candidates for delivery of anti-tumour agents to cells overexpressing the EGFR [12, 13]. To further boost the therapeutic effect, we have in this study encapsulated a 125I-labelled amino-benzyl derivative of daunorubicin (125I-Comp1), which has previously been synthesised in one of our laboratories [14], into EGFR-targeting liposomes (Nuclisome-particles). The drug 125I-Comp1 has recently been shown to accumulate in tumour-cell nuclei, bind tumour-cell DNA, cause DNA double-strand breaks and cause substantial tumour-cell growth inhibition [15]. In the present study, we investigated the specificity of EGFR-targeting Nuclisome-particles towards tumour cells, their translocation into the cell nucleus, and their tumour cell growth inhibitory effect.
Materials and methods
Materials
1,2-distearoyl-sn-glycero-3-phosphatidylcholine (DSPC) and 1,2-distearoyl-sn-glycero-3-phosphatidylethanol-amine-N-[methoxy(polyethylene glycol)-2000] (DSPE-PEG2000) were purchased from Avanti Polar Lipids Inc. (Alabaster, AL). The N-hydroxysuccinimidyl ester of DSPE-PEG3400 (DSPE-PEG3400-NHS) was purchased from Shearwater Polymers (Huntsville, AL). 3H-labelled cholesterylhexadecyl ether (3H-CHE) was obtained from Perkin-Elmer Life Sciences Inc. (Boston, MA). Mouse EGF was obtained from Chemicon International, Inc. (Temecula, CA). Doxorubicin HCl (Dox), bovine serum albumin (BSA), Na-azide, Hoechst 33345, citric acid, N-[2-hydroxyethyl]piperazine-N'-[2-ethanesulfonic acid] (HEPES), cholesterol, chloramine-T, sodium metabisulfite, and Sephadex G-50, were purchased from Sigma-Aldrich Chemical Company (St. Louis, MO). Sepharose CL-4B, Sephadex G-25, Sephadex G-150 and 125I were purchased from Amersham Biosciences (Uppsala, Sweden). Quicksafe A scintillation fluid was obtained from Zinsser Analytic (Scintvaruhuset, Uppsala, Sweden). Triton X-100 was purchased from Fluka Chemie GmbH (Buchs, Switzerland). Formaldehyde, Mayer Hematoxylin and Pertex were obtained from Histolab Products AB (Göteborg, Sweden). Other chemicals were purchased from common sources.
The anthracycline derivative
The amino-benzyl derivative of daunorubicin was synthesized as its formate salt as described previously [14]. The biological characterisation of the compound has recently been published [15] and is referred to as Comp1. Figure 1 shows the molecular structures of Dox, daunorubicin and Comp1.
Radiolabelling of Comp1
Eighty micrograms of Comp1 in 40 μl of methanol was radiolabelled with 125I. In brief, 30 MBq of 125I was added to Comp1 in solution. Ten microlitres of Chloramine-T (4 mg/ml in methanol) was then added and mixed for 5 min at room temperature. The reaction was terminated by adding 10 μl of sodium metabisulfite (8 mg/ml in dH2O). 125I-Comp1 was separated from Comp1 on a System Gold HPLC (Beckman Coulter, Inc., Fullerton, CA, USA) equipped with an Ultrasphere C18 (5 µm, 4.6 mm × 25 cm inner diameter) reverse-phase column (Beckman Coulter) [15]. The column was eluted at a flow rate of 1 ml/min, with acetonitrile containing 0.05% formic acid and dH2O containing 0.05% formic acid as the mobile phases. For elution program and monitoring see [15]. Forty fractions were collected (1 min/fraction) and measured with a scintillation detector (Mini-instruments LTD, Essex, UK). Fractions containing 125I-Comp1 were pooled and the solvent was evaporated. The crystallised compound was reconstituted in an aqueous solution of 127I-Comp1 to a total I-Comp1 concentration of 0.4 mM. This radioactive composition, with mixture of 125I-Comp1 and 127I-Comp1 has a ratio of about 1:270. For clarity, when using pure non-radioactive iodinated compound without any addition of 125I-Comp1 the compound is referred to as 127I-Comp1.
Preparation of liposomes
Liposomes composed of DSPC, cholesterol, and DSPE-PEG2000 at a molar ratio of 57:40:3 were prepared by the lipid film hydration method [16]. Cholesterol and lipids were dissolved in chloroform, the solvent was evaporated under a gentle stream of nitrogen gas and the lipid film was dried under vacuum overnight. The lipid film was hydrated with 300 mM citrate buffer (pH 4) for 1 h with intermediate vortex mixing at a lipid concentration of 25 mM at a temperature of 60°C. The lipid dispersion was repetitively frozen in liquid nitrogen and thawed at a temperature of 60°C five times before extrusion. Liposomes were extruded ten times through two stacked polycarbonate membranes filters (Whatman Inc. Nucleopore, Newton, MA) with a pore size of 100 nm at RT using an Avanti Mini-extruder (Avanti Polar Lipids Inc., Alabaster, AL).
Drug encapsulation
125I-Comp1, 127I-Comp1 or Dox were encapsulated into liposomes using the pH-gradient driven loading protocol by Mayer et al. [17]. The pH gradient across the liposome membrane was generated by exchanging the extravesicular 300 mM citrate buffer (pH 4) with Hepes Buffered Saline (HBS, 20 mM pH 7.4, 150 mM NaCl) on a Sephadex G-25 column. Dox was dissolved at a concentration of 1 mM in HBS while 125I-Comp1 and 127I-Comp1 were dissolved in dH2O at a concentration of 0.4 mM. Preheated drug solution was added to liposomes at a 0.05 drug-to-lipid molar ratio. The mixtures were incubated for 15 min in a water bath at a temperature of 60°C with intermitted vortex mixing to allow efficient drug loading. Drug loading is close to 100% of the added Comp1 and hence one liposome contains about 5,000 molecules of drug giving less than 20 molecules of 125I-Comp1 for this liposome composition.
Cryogenic transmission electron microscopy (Cryo-TEM)
The procedure has been described in detail elsewhere [18–20]. In brief, liposomes loaded with Dox, 127I-Comp1 or Comp1 were transferred onto a copper grid coated with a perforated polymer film and vitrified by submersion in liquid ethane and into a Zeiss EM 920 A transmission electron microscope (Carl Zeiss Inc., Oberkochen, Germany). Samples were exposed to an electron density of 5–15 e-/Å2 and images were taken in zero-loss bright field mode with an acceleration voltage of 80 kV. Image sections were carefully chosen to represent a typical impression of all images.
Determination of drug retention
Liposomes loaded with Dox or 127I-Comp1 were incubated in HBS or culture media. At selected time points, aliquots were withdrawn in triplicate and non-encapsulated drug was removed on a Sephadex G-50 mini-column with HBS in a centrifugal field of 680 × g for 2 min. The volume of the eluent was adjusted to 1 ml with HBS and 1 ml of 1% Triton X-100 solution was added. Samples were heated to a temperature of 90°C and cooled down to room temperature. The fluorescence intensity of samples was determined at an excitation wavelength of 468 nm and an emission wavelength of 589 nm. The percentage of encapsulated drug after incubation and separation of free drug was determined relative to the amount of encapsulated drug before incubation using standard curves of the respective drug.
Conjugation of EGF to liposomes
The procedure for conjugating EGF to PEG-stabilized liposomes has been described and optimized previously [12, 13]. In brief, NHS-PEG3400- DSPE was hydrated for 5 min at a temperature of 60°C with mouse EGF (containing only one primary amine) in PBS at molar ratio of 0.1:2 and thereafter stirred for 1 h at RT. The NHS-DSPE-PEG3400 concentration was approximately 0.2 mM. Non-conjugated EGF was removed on a Sephadex G-150 column with HBS as the mobile phase. The purified EGF-PEG3400-DSPE was mixed with drug-loaded liposomes at a 1:33 lipid molar ratio at a temperature of 60°C for 1 h. After incubation, unincorporated EGF-PEG3400-DSPE was separated from liposomes on a Sepharose CL-4B column with HBS as eluent and fractions containing EGF-liposome-drug were pooled. The procedure to label EGF with 125I and liposomes with 3H-CHE has been described elsewhere [12].
Cell culture
U-343MGaCl2:6 cells overexpressing EGFR (5 × 105 receptors/cell) were obtained from the Department of Pathology, Uppsala University, Uppsala, Sweden [21]. Cells were grown in Nunclone 75 cm2 cell culture flasks (Nunc, Roskilde, DK) as monolayer cultures using Ham’s F-10 medium supplemented with 10% fetal calf serum, glutamine (2 mM), streptomycin (100 μg/ml), and penicillin (100 IU/ml) (all by Biochrom AG, Berlin, Germany) at a temperature of 37°C in humidified air with 5% CO2. Cells were harvested using trypsin/EDTA solution (0.25%/0.02% in PBS, Biochrom AG, Berlin, Germany).
Tumour-cell uptake of liposomes
A volume of 0.5 ml of EGF-coupled 3H-labelled liposomes or 3H-labelled liposomes at lipid concentrations of 0.2 µmol/ml (1.5 × 106 cpm/ml) in culture medium was added to 8 × 105 U-343 cells in 35-mm Petri dishes. To block EGFR from liposome uptake, 0.5 ml of medium containing EGF (1 mg/ml) was added while non-blocked cells received 0.5 ml of culture medium. Cell dishes were incubated in triplicates for 1, 2, 4, and 24 h. At each time point, the incubation medium was removed and cells were washed six times with cold serum-free media. To remove membrane-bound liposomes, 0.5 ml of 0.1 M glycine-HCl solution (pH 2.5) was added to each dish and cells were incubated for 6 min at a temperature of 4°C. To lyse cells, 0.5 ml of 1 M NaOH solution was added to cell dishes and cells were incubated for 1 h at a temperature of 37°C. The radioactivity of both solutions was determined using a liquid scintillation counter (1214 RackBeta, Perkin-Elmer, MA, USA). Samples containing NaOH were neutralized by adding 1 ml of 1 M HCl to avoid chemiluminescence.
To imitate circulating tumour cells in vivo, an ex vivo human blood vasculature system (Chandler loop) was set up. Medical plastic tubing (Raumedic AG, Münchberg, Germany) was cut into 0.3-m-long pieces and ends were joined with designed non-clothing connectors tightly pushed into the lumen of the tubing. Each loop was filled with 5 ml of freshly obtained human blood, approximately 106 U-343 cells, and either 125I-labelled EGF-coupled liposomes, EGF-coupled 3H-labelled liposomes, or EGF-coupled liposomes containing- 125I-Comp1 (totally 1 µmol lipid). The blood volume inside the Chandler loops was circulated for 2–4 h at a temperature of 37°C. Blood was thereafter transferred into 50-ml tubes containing 40 ml of lysis buffer (0.15 M NH4Cl, 0.1 mM KHCO3, 0.1 mM Na2EDTA pH 7.2–7.4). The tubes were kept in darkness for 15 min and were thereafter centrifuged at 335 × g for 10 min to remove the haemoglobin. The cell pellets, which contain white blood cells and tumour cells, were then washed once with ice-cold washing buffer (dH2O containing 1% bovine serum albumin and 0.05–0.1% Na-azide in dH2O) and then re-suspended in 0.5 ml of fresh washing buffer. Cells were stained with Hoechst 33342 (1:100/vol:vol) and thereafter separated using a fluorescent-activated cell sorter (FACSVantageSE, Becton Dickinson, San Jose, USA) according to DNA contents and size. After cell sorting, the radioactivity of the tumour cell fraction and the white blood cell fraction (WBC) was determined using either gamma counter (1480 Wallac Wizard, Perkin Elmer, Wellesley, MA, USA) or liquid scintillation counter.
Growth curves
Approximately 3 × 106 U-343 cells were transferred to glass flasks coated with silicon to prevent cell adhesion. EGFR-targeting and non-targeting liposomes containing Dox (0.25 μmol lipid), 127I-Comp1 (0.25 μmol lipid) or 125I-Comp1 (targeting: 0.25 μmol lipid, 0.1 MBq/ml; non-targeting: 0.125 μmol lipid, 0.1 MBq/ml) were added with culture media to total volume of 10 ml. Flasks were constantly rotated at a temperature of 37°C and an atmosphere containing 5% CO2. After 4 h, the cells were centrifuged for 5 min at 175 × g. The supernatant was removed and the procedure was repeated twice. Cells were re-suspended in complete culture medium, the cell number was determined with a cell counter (Coulter Z2 cell Counter, Beckman, CA, USA) and cells were re-seeded in triplicates, allowed to grow in an incubator, and counted again once a week. Only a part of the cells were propagated to keep a suitable number of cells in the culture. This was corrected for when constructing the growth curves. To determine the number of surviving cells, data were analyzed using non-linear regression analysis when cells had resumed exponential growth. Growth curve assay was used to enable comparison with earlier published results using this assay and has been shown to correlate well with clonogenic cell survival [22].
Autoradiography
Cells remaining after seeding were centrifuged at 225 × g for 5 min. Pellets were transferred into 4% formaldehyde in 10 mM phosphate buffer and fixated at a temperature of 4°C for 1 week before embedding into Historesin (for details see [15]). Cell pellets were dehydrated in ethanol and submerged three times for 20 min in Historesin infiltration solution (Leica Instruments GmbH, Heidelberg, Germany). Pellets were embedded overnight in Historesin with an activator. The Historesin block was sliced, and 4-µm-thick sections were transferred onto glass slides. Slides were submerged in Kodak NTB photo emulsion (Eastman Kodak Co., Rochester, NY, USA) and dried before storage in darkness at a temperature of 4°C. After 6 days of exposure, slides were submerged in Kodak D19 (Eastman Kodak Co.) solution for 3 min. Slides were transferred into 0.1% acetic acid for 10 s and fixed for 5 min using Kodak fixer (Eastman Kodak Co.). Slides were washed extensively with water, and cell nuclei were stained for 3 min with Mayer Hematoxylin. Slides were again washed with water for 5 min and mounted using Pertex. Cells were inspected with a light microscope (Nikon Eclipse E400; Nikon Corporation, Tokyo, Japan), and images of representative cells were then captured.
Results
Cryo-TEM
Cryo-TEM images of liposomes loaded with Dox, Comp1, or 127I-Comp1 confirmed that drugs precipitated inside liposomes (Fig. 2). The precipitate of 127I-Comp1 was distinct from that of both Dox and Comp1.
Drug retention in liposomes
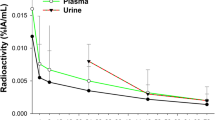
Dox and 127I-Comp1 remained encapsulated within liposomes when incubated in HBS at a temperature of 37°C for 24 h (Fig. 3a). Increasing the temperature to 60°C for 1 h decreased the retained amount of Dox to 66% while for 127I-Comp1 as much as 94% remained (Fig. 3a). When incubated in culture medium at a temperature of 37°C, the retention of the encapsulated drug was less compared to that in HBS (Fig. 3b) with minor differences between Dox and 127I-Comp1. At 24 and 48 h, 89% and 87% of 127I-Comp1 remained encapsulated as compared to 84% and 81% for Dox.
Tumour-cell uptake of liposomes
The uptake of EGF-coupled 3H-labelled liposomes by cultured human tumour cells increased with time (Fig. 4a). The accumulation was primarily intracellular since less than 10% of the radioactivity was associated with the acid solution (membrane-bound fraction) after 24 h (data not shown). This accumulation was receptor-specific since the uptake could be blocked with excess amounts of EGF (Fig. 4a). The uptake of non-targeting 3H-labelled liposomes was low, further supporting the fact that EGF-coupled 3H-labelled liposomes are specifically taken up by EGFR overexpressing tumour cells.
a Uptake of EGF-coupled 3H-labelled liposomes and 3H-labelled liposomes by U-343 cells incubated for up to 24 h with 0.2 µmol lipid/ml (1.5 × 106 cpm/ml). Cellular uptake of 3H was analysed after thorough washing. The data represent the sum of membrane-bound (less than 10%) and internalized radioactivity (see Methods). 106 cells were harvested. EGFR was blocked with 100-times excess of EGF. Error bars indicate maximum variations (n = 3). b Uptake of 125I-EGF-coupled liposomes (6 × 105 cpm added), EGF-coupled 3H-labelled liposomes (23 × 105 cpm added) and EGF-coupled liposome containing 125I-Comp1 (5 × 105 cpm added) by white blood cells (WBC) and U-343 tumour cells in an ex vivo human blood system [28]. Totally, 1 µmol of lipid was added in each setup
EGFR-targeting liposomes were also capable of locating single tumour cells circulating in human blood (Fig. 4b). Although the concentration of white blood cells is much higher (~5 million cells/ml) than the concentration of tumour cells (0.2 million cells/ml) it is clear that the uptake per cell was more than 20 times higher in tumour cells as compared to white blood cells. This result applies to all the different parts of the targeting liposome; the targeting agent (EGF), the liposome, and the daunorubicin derivative (125I-Comp1), as can be seen in (Fig. 4b).
Growth curves
Control cells and cells treated with non-targeting liposomes encapsulating Dox and targeting and non-targeting liposomes encapsulating 127I-Comp1 grew at an exponential rate when seeded after 4 h of incubation in roller flasks (Fig. 5). When treated with EGF-coupled Dox-loaded liposomes tumour-cell growth was delayed considerably. Only about 10% of the initial cells survived the treatment as determined by extrapolating growth curves from time points when cells had reached exponential growth (10–20 days post treatment). Treatment with non-targeting liposomes loaded with 125I-Comp1 had a similar effect on tumour cell growth
Growth curves of U-343 cells incubated for 4 h with a non-targeting and b EGFR-targeting liposomes loaded with either Dox, 127I-Comp1, or 125I-Comp1. Untreated control cells were incubated only with medium. For targeting liposomes with 125I-Comp1 (Nuclisome-particles) a concentration of 0.055 Bq 125I per cell was achieved, while for nontargeting liposomes only 0.015 Bq 125I per cell was measured. Cell densities of living cells were determined using a Z2 Coulter counter and corrected for cell loss after each sub-cultivation. To determine the number of surviving cells data were analysed using non-linear regression analysis (GraphPad Software, San Diego, CA) when cells had resumed exponential growth. Exponential growth was reached at day 14 for Liposome-125I-Comp1 and EGF-Liposome-Dox, and day 56 for EGF-Liposome-125I-Comp1. Error bars indicate maximum variations (n = 3)
.
EGFR-targeting liposomes loaded with 125I-Comp1 (Nuclisome-particles) delayed tumour cell growth by more than 40 days (Fig. 5). Extrapolation from the growth curve indicated that only a small number of the initial cells survived the Nuclisome-treatment. Two important points should be noted. First, the growth delay was gained from the Auger-emitting nuclide 125I, since EGF-liposome loaded with 127I-Comp1 caused no growth delay at all. Second, the efficacy of 125I-Comp1 encapsulated into EGFR-targeting liposomes was 105 times greater than that of Dox encapsulated into EGFR-targeting liposomes.
Autoradiography
The intracellular localization of radionuclides after 4-h incubation of targeting and non-targeting liposomes loaded with 125I-Comp1 together with U-343 cells in roller flasks was analysed using autoradiography. Following incubation with EGFR-targeting liposomes, most of the high grain density from the labelled compound was co-localized with the haematoxylin-stained cell nuclei (Fig. 6a) whereas low grain density, indicative of poor cellular uptake, was observed after incubation with non-targeting liposomes (Fig. 6b)
Representative autoradiography images of Hematoxylin-stained cultured human U-343 glioma cells incubated for 4 h at 37°C with equal amounts of a EGF-coupled liposomes containing 125I-Comp1 or b liposomes containing 125I-Comp1. Cells were embedded into a historesin block and 4-µm-thick sections were transferred onto glass slides. A Kodak NTB photo emulsion was exposed for 6 days and nuclei were stained with Meyer Hematoxylin. The magnification was 1,000-fold
.
Discussion
Radionuclides have a minor but important role in targeted cancer therapy. Beta-emitters such as 90Y, 131I and 177Lu are most commonly employed but the therapeutic potential of short-range, low-energy Auger-electron emitters, such as 125I, is getting progressively wider recognition. Auger emitters have to be delivered selectively into tumour cell nuclei since their radiotoxic properties are operative only in close vicinity to DNA. To enable specific tumour cell DNA delivery of 125I we developed a new strategy built on the use of Nuclisome-particles, i.e., targeting liposomes loaded with a radionuclide-labelled DNA-binding compound to specifically transport liposomes to tumour cells in a first step and to deliver radionuclides into DNA in a second step.
The anthracycline derivative Comp1 was, together with several other derivatives, specially designed and synthesised for loading into liposomes intended for tumour-cell-specific nuclear delivery [14]. The biological evaluation of the compounds per se indicated that Comp1 possessed the most promising properties regarding DNA-binding and ability to produce DNA double-stand breaks when labelled with the Auger-electron emitter 125I [15]. The aim of the present study was to investigate whether this novel radiolabelled compound could be used in a targeting liposome system to boost the therapeutic effect. The golden standard for liposomal drug delivery, Dox-loaded liposomes, where chosen as a suitable comparison. Both Dox and 127I-Comp1 form an intra-vesicular precipitate when loaded at high enough drug-to-lipid molar ratio and this effectively prevents rapid release of the compounds [17]. Interestingly, there is an apparent difference between the precipitates formed by the different compounds (Fig. 2). Dox forms rod-shaped precipitates that are broad and clearly contrasted. Comp1 forms similar shapes but they seem thinner and less contrasted. More obvious is the difference in structure found for 127I-Comp1. The iodinated compound forms spherical precipitates. The difference in precipitate structure between iodinated and non-iodinated Comp1 has important consequences for the design of the liposome-loading procedure. It is not realistic to load the liposomes with pure 125I-Comp1 in the high amounts needed to obtain precipitate. Thus, addition of non-radiolabelled Comp1 is required. The dissimilar precipitate structures disclosed by cryo-TEM suggest that 127I-Comp1, rather than non-iodinated Comp1, should be chosen for this purpose. Therefore, 125I-Comp1 was purified after radio-iodination to remove non-iodinated Comp1 and mixed with 127I-Comp1 prior to liposome loading.
No significant difference between 127I-Comp1 and Dox was observed regarding drug retention at 37°C after pH-gradient loading. When incubated at 60°C in HBS, 127I-Comp1 showed, however, a superior retention. Although the difference was less pronounced, a similar trend was observed in culture medium at 37°C. In conclusion, drug retention data suggest that 127I-Comp1 is equally or better retained inside the liposomes as compared to Dox.
To take advantage of any targeting principle, receptor specificity is a minimum requirement. Results of this study confirm our previous data [12, 13] and suggest that EGF-coupled liposomes posses a high tumour-cell specificity. When EGF-receptors were blocked with excess amount of ligand and when liposomes were administered without targeting agent, the tumour-cell uptake was low in comparison to uptake of EGF-liposomes in unblocked cells. Several mechanisms may, either alone or in combination, be responsible for the cytoplasmic release of the radiolabelled compound after receptor-mediated uptake of the liposomes. The full details of how liposome encapsulated substances are released from lysosomes still remain to be revealed. Lower pH and/or other environmental conditions in the lysosome might increase the permeability of the liposomes and thus promote fast leakage of the entrapped substance. Once released from the liposomes, the substance molecules are able to partition into and diffuse over the lysosome membrane, enter into the cytosol, and find their way to the cell nucleus.
This receptor specificity was further manifested by the tumour-cell uptake experiment in blood ex vivo. All three parts of the liposome conjugate, the targeting agent, the liposome, and the drug, exhibited a substantial uptake in tumour cells while the uptake in WBC was minor. The most relevant ratio between tumour cells and WBC is that of 125I-Comp1. The uptake of 125I in tumour cells was almost 35-times higher than that in WBC which leads to a significant difference in delivered radiation dose. The results from ex vivo experiments thus clearly demonstrate the ability of Nuclisome-particles to deliver a DNA-binding Auger-electron emitter to circulating tumour cells.
The tumour-cell killing efficiency of targeting Nuclisome-particles was remarkable in comparison with all other liposome formulations (Fig. 5). At the investigated concentration, neither non-targeting nor EGFR-targeting liposomes loaded with 127I-Comp1 had any effect on cultured tumour cells. Further, liposome-Dox, similar to the liposomes used in clinics today for treatment of Kaposi’s sarcoma and breast cancer, have no effect on cell growth at the investigated concentration. The increased efficacy achieved by adding EGF as the targeting agent to liposome-Dox confirms the previously reported efficacy enhancement by targeting Dox-loaded liposomes [23]. The small effect achieved by non-targeting liposomes encapsulating 125I-Comp1 might be a result of the minor leakage that occurs during incubation in culture medium. Since 125I-Comp1 is more effective than Dox per se, as shown earlier [15], this can explain why liposome-125I-Comp1 have some effect but not liposome-Dox.
When comparing the survival data obtained with EGFR-targeting liposomes loaded with 125I-Comp1 and 127I-Comp1, respectively, it is evident that the dramatic effect of the former derives from 125I solely. When Comp1 is labelled with 127I no growth disturbing effect is seen. At the same concentration, a clear growth inhibition is seen for compound labelled with 125I. This could be an Auger effect of 125I on tumour-cell DNA, which originates from multiple low-energy short-range Auger electrons. These electrons deposit the majority of energy within a few nm3 around the site of decay and therefore cause cell-killing only when located in close proximity to DNA. The autoradiography images of cells incubated with EGF-coupled liposomes containing 125I-Comp1 shows that 125I-Comp1 could be DNA associated since ARG-grains were co-localized with the nuclei of tumour cells. The sub-cellular distribution of ARG-tracks was similar to the distribution of tracks from 125I-Comp1 per se as shown previously [15]. In the same study, 125I-Comp1 was proven with several techniques to bind DNA and to generate about 0.5 double-strand breaks per decay when bound to extracted chromosomal DNA.
Several recently reported approaches [24, 25] are based on nuclear localization sequences (NLS) to transport Auger-electron emitting nuclides from cytoplasmatic compartments to the nucleus. The efficiency of the Auger-electron emitting nuclide is thereby increased by approximately one order of magnitude [24]. Our approach differs somewhat since our aim is to target the tumour-cell DNA. The Auger effect, with a high electron density causing complex DNA damages, can only be manifested when the decay occurs within a few nanometres from DNA. The dramatic effect shown by 125I-Comp1 could well be due to DNA association and hence the significant radiotoxic effect. The additional boost seen from the Auger emitter decreases the administration need compared to conventional liposomes loaded with Dox. This will probably also decrease the cytotoxic effect of the compound regardless of Auger effect, and may thus be seen as an advantage due to the narrow therapeutic index of anthracyclines.
Targeting Nuclisome-particles have the potential to become an effective anti-tumour agent and the most important application could well be disseminated single tumour cells in the circulation. The elimination of these circulating cells is desirable since they eventually can give rise to metastases. The use of cytotoxic drugs might not be adequate due to common lack of proliferation and consequently there is a need to develop more specific adjuvant therapy [26]. An important advantage of targeting liposomes in such applications is the massive amount of compound deliverable by means of only a few receptor interactions. The ability to deliver such quantities is also important since the pharmacokinetics of the liposomes might be a limiting factor. Furthermore, the restricted dose distribution of Auger-electron emitters to only targeted cells will probably minimize irradiation of bone marrow. Actually, assuming that an Auger-electron emitting nuclide like 125I is bound to tumour-cell DNA, the dose to normal tissue could be negligible when delivering a therapeutic dose to the tumour cells [27]. Targeting Nuclisome-particles are therefore attractive for in vivo tumour targeting evaluation.
References
Chabner BA, Meyers CE. In: DeVita Jr VT, HSaRSA, editors. Cancer: principles and practice of oncology. Philadelphia, Toronto: J.B. Lippincott Company; 1982. p. 156–97.
Sapra P, Allen TM. Ligand-targeted liposomal anticancer drugs. Prog Lipid Res. 2003;42:439–62.
Fenske DB, Chonn A, Cullis PR. Liposomal nanomedicines: an emerging field. Toxicol Pathol. 2008;36:21–9.
Elmroth K, Stenerlow B. DNA-incorporated 125I induces more than one double-strand break per decay in mammalian cells. Radiat Res. 2005;163:369–73.
Yarden Y, Sliwkowski MX. Untangling the ErbB signalling network. Nat Rev Mol Cell Biol. 2001;2:127–37.
Yano S, Kondo K, Yamaguchi M, Richmond G, Hutchison M, Wakeling A, et al. Distribution and function of EGFR in human tissue and the effect of EGFR tyrosine kinase inhibition. Anticancer Res. 2003;23:3639–50.
El-Rayes BF, LoRusso PM. Targeting the epidermal growth factor receptor. Br J Cancer. 2004;91:418–24.
Ranson M, Sliwkowski MX. Perspectives on anti-HER monoclonal antibodies. Oncology. 2002;63(Suppl 1):17–24.
Spano JP, Fagard R, Soria JC, Rixe O, Khayat D, Milano G. Epidermal growth factor receptor signaling in colorectal cancer: preclinical data and therapeutic perspectives. Ann Oncol. 2005;16:189–94.
Lee J. Formulation development of epidermal growth factor. Pharmazie. 2002;57:787–90.
Baulida J, Kraus MH, Alimandi M, Di Fiore PP, Carpenter G. All ErbB receptors other than the epidermal growth factor receptor are endocytosis impaired. J Biol Chem. 1996;271:5251–7.
Kullberg EB, Nestor M, Gedda L. Cell–cell targeted epidermal growth factor liposomes loaded with boronated acridine: uptake and processing. Pharm Res. 2003;20:229–36.
Kullberg EB, Wei Q, Capala J, Giusti V, Malmstrom PU, Gedda L. EGF-receptor targeted liposomes with boronated acridine: growth inhibition of cultured glioma cells after neutron irradiation. Int J Radiat Biol. 2005;81:621–9.
Ghirmai S, Mume E, Tolmachev V, Sjoberg S. Synthesis and radioiodination of some daunorubicin and doxorubicin derivatives. Carbohydr Res. 2005;340:15–24.
Ickenstein LM, Edwards K, Sjoberg S, Carlsson J, Gedda L. A novel 125I-labeled daunorubicin derivative for radionuclide-based cancer therapy. Nucl Med Biol. 2006;33:773–83.
Hope MJ, Bally MB, Webb PR, Cullis PR. Production of large unilamellar vesicles by a rapid extrusion procedure. Characterization of size distribution, trapped volume and ability to maintain a membrane potential. Biochim Biophys Acta. 1985;812:55–65.
Mayer LD, Bally MB, Cullis PR. Uptake of adriamycin into large unilamellar vesicles in response to a pH gradient. Biochim Biophys Acta. 1986;857:123–6.
Bellare JR, Davis HT, Scriven LE, Talmon Y. Controlled environment vitrification system: an improved sample preparation technique. J Electron Microsc Tech. 1988;10:87–111.
Dubochet J, Adrian M, Chang JJ, Homo JC, Lepault J, McDowall AW, et al. Cryo-electron microscopy of vitrified specimens. Q Rev Biophys. 1988;21:129–228.
Vinson PK. In: Baily GW, editor. Proceedings of the 45th annual meeting of the Electron Microscopy Society of America. San Francisco: San Francisco Press; 1987. p. 644–5.
Westermark B, Magnusson A, Heldin CH. Effect of epidermal growth factor on membrane motility and cell locomotion in cultures of human clonal glioma cells. J Neurosci Res. 1982;8:491–507.
Steffen AC, Gostring L, Tolmachev V, Palm S, Stenerlow B, Carlsson J. Differences in radiosensitivity between three HER2 overexpressing cell lines. Eur J Nucl Med Mol Imaging. 2008;35:1179–91. doi:10.1007/s00259-007-0713-x.
Park JW, Hong K, Kirpotin DB, Colbern G, Shalaby R, Baselga J, et al. Anti-HER2 immunoliposomes: enhanced efficacy attributable to targeted delivery. Clin Cancer Res. 2002;8:1172–81.
Chen P, Wang J, Hope K, Jin L, Dick J, Cameron R, et al. Nuclear localizing sequences promote nuclear translocation and enhance the radiotoxicity of the anti-CD33 monoclonal antibody HuM195 labelled with 111In in human myeloid leukemia cells. J Nucl Med. 2006;47:827–36.
Ginj M, Hinni K, Tschumi S, Schulz S, Maecke HR. Trifunctional somatostatin-based derivatives designed for targeted radiotherapy using auger electron emitters. J Nucl Med. 2005;46:2097–103.
Ring A, Smith IE, Dowsett M. Circulating tumour cells in breast cancer. Lancet Oncol. 2004;5:79–88.
Lundqvist H, Stenerlöw B, Gedda L. The Auger effect in molecular targeting therapy: Springer Sciences + Business Media B.V; 2008.
Christensen K, Larsson R, Emanuelsson H, Elgue G, Larsson A. Coagulation and complement activation. Biomaterials. 2001;22:349–55.
Acknowledgements
We thank the following colleagues for their various contributions to the Nuclisome project: Dr. Eskender Mume, Dr. Senait Ghirmai, Dr. Vladimir Tolmachev, Prof. Hans Lundqvist, Dr. Jan Grawé, Dr. Cecilia Winander, Dr. Per Wessman and Mr. Göran Karlsson. Financial support was kindly provided by The Swedish Cancer Society (grants 07 0664 and 05 6593) and the Swedish Research Council (grant 621-2005-5581).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Fondell, A., Edwards, K., Ickenstein, L.M. et al. Nuclisome: a novel concept for radionuclide therapy using targeting liposomes. Eur J Nucl Med Mol Imaging 37, 114–123 (2010). https://doi.org/10.1007/s00259-009-1225-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00259-009-1225-7