Abstract
Purpose
Huntington disease (HD) mutation increases gain-of-toxic functions contributing to glutamate-mediated excitotoxicity. Riluzole interferes with glutamatergic neurotransmission, thereby reducing excitotoxicity, enhancing neurite formation in damaged motoneurons and increasing serum concentrations of BDNF, a brain cortex neurotrophin protecting striatal neurons from degeneration.
Methods
We investigated metabolic and volumetric differences in distinct brain areas between 11 riluzole-treated and 12 placebo-treated patients by MRI and 18F-fluoro-2-deoxy-d-glucose (FDG) PET scanning, according to fully automated protocols. We also investigated the influence of riluzole on peripheral growth factor blood levels.
Results
Placebo-treated patients showed significantly greater proportional volume loss of grey matter and decrease in metabolic FDG uptake than patients treated with riluzole in all cortical areas (p<0.05). The decreased rate of metabolic FDG uptake correlated with worsening clinical scores in placebo-treated patients, compared to those who were treated with riluzole. The progressive decrease in metabolic FDG uptake observed in the frontal, parietal and occipital cortex correlated linearly with the severity of motor scores calculated by Unified Huntington Disease Rating Scale (UHDRS-I) in placebo-treated patients. Similarly, the rate of metabolic changes in the frontal and temporal areas of the brain cortex correlated linearly with worsening behavioural scores calculated by UHDRS-III in the placebo-treated patients. Finally, BDNF and transforming growth factor beta-1 serum levels were significantly higher in patients treated with riluzole.
Conclusion
The linear correlation between decreased metabolic FDG uptake and worsening clinical scores in the placebo-treated patients suggests that FDG-PET may be a valuable procedure to assess brain markers of HD.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Huntington’s disease (HD) is caused by a CAG repeat expansion mutation in the huntingtin (HTT) gene, resulting in brain damage primarily involving the striatum [1] and, more extensively, several cortical regions [2, 3]. The abnormal elongated protein huntingtin is widely expressed in all body tissues, eventually reaching toxic levels [4]. Further toxicity is attributed to the effect of mutant HTT on other proteins, including neurotrophins such as brain-derived neurotrophic factor (BDNF) [5–7], which are protective and underexpressed in the presence of mutant HTT [5–7]. Other growth factors such as glial cell line-derived neurotrophic factor (GDNF), neurotrophic growth factor, and cytokines such as transforming growth factor (TGF beta-1), play a role in neurodegenerative diseases and, possibly, in HD, sometimes showing dysregulation in brain and periphery [8–10].
The transcription of some neurotrophic factors is mediated by metabotropic glutamate receptors [11], which are strictly related to excitotoxicity in HD. The excitotoxic hypothesis relates increased huntingtin toxicity to glutamate release in the cortex through a cascade of events, causing cell dysfunction and death in the striatum and several cortical regions [12]. Indeed, the progressive cortical dysfunction and degeneration associated with abnormal RNA expression in motor cortical areas [13] contributes to the progression of patients’ disability [2, 3]. Studies on cortical areas have demonstrated abnormal progressive glucose metabolism in HD [2, 14, 15], thus proving that neuronal stress occurs in vivo as has been shown in vitro [16]. Therefore, early damage to several brain cortical areas associated with progressive striatum atrophy gives support to the hypothesis that the wide spectrum of clinical signs and symptoms of HD may relate to widespread damage to the cortex [3, 17].
Riluzole interferes with glutamatergic neurotransmission, thereby reducing excitotoxicity, enhancing neurite formation in damaged motoneurons [18], and increasing serum concentrations of BDNF [19, 20]. In a previous longitudinal prospective study set up to analyse the magnitude of volumetric and metabolic brain changes in riluzole-treated patients in comparison to placebo-treated patients (100 mg/day riluzole versus placebo), we have demonstrated that brain grey matter volume and glucose metabolism after about 2 years are protected in patients receiving the drug compared to patients receiving placebo [20].
In the present study we investigated metabolic and volumetric differences in distinct brain areas between 11 riluzole-treated patients and 12 placebo-treated patients by MRI and FDG PET scanning, according to our fully automated protocols [2]. We also sought to determine whether these changes were related to clinical markers in the two groups of patients. Finally, we investigated the influence of riluzole on peripheral growth factor blood levels.
Materials and methods
Subjects
All 23 patients [20] underwent genetic testing after providing informed consent and after neurological examination, including motor, psychiatric, cognitive and functional assessments, by a physician with expertise in HD [20, 21]. Subjects’ consent was obtained according to the Declaration of Helsinki (Br Med J 1991;302:1194). Age at onset of symptoms was calculated according to the initial neurological manifestations [20, 21]. Motor symptoms and behavioural and cognitive changes were assessed clinically with the unified HD rating scale (UHDRS) [22]. All patients were matched for age, gender, mutation size, and disease stage, according to a previously published strategy (Table 1) [20]. Of the 23 patients enrolled, 11 received blinded treatment with the neuroprotective agent, as previously described [20].
Two MRI and PET scans were obtained for each patient and a mean interval of 24 months elapsed between scanning sessions [2, 20]. Serum BDNF, GDNF and TGF beta-1 levels were measured after the second MRI and PET scans in different cohorts of riluzole-treated patients, placebo-treated patients and healthy control subjects, according to a previously described method [6, 20]. Serum samples from all subjects were collected and stored at IRCCS Neuromed, after informed consent had been obtained. Of the 23 patients enrolled, 11 received blinded treatment with the neuroprotective agent [20].
MRI studies
MRI protocols included two interleaved sets of 15 slices covering the entire brain obtained at 1.5 T (Magnetom, Siemens, Erlangen, Germany), sampling the brain at a total of 30 levels. Each of the two sets was composed of two conventional spin-echo sequences, generating 15 T1-weighted (TR/TE 600/15 ms) and N(H)/T2-weighted (TR/TE1–TE2 2200/15–90 ms) images (25 cm FOV, 256×256 acquisition matrix, 4 mm thick axial slices). MRI segmentation procedure and statistical analysis were performed as described previously [2, 23]. In brief, brain compartments were segmented with a fully automated postprocessing procedure kindly provided by Dr. Bruno Alfano of the Biostructure and Bioimaging Institute of the CNR. For each MRI study, total intracranial volume and absolute volumes (in millilitres) of the grey matter (GM), white matter (WM), and cerebrospinal fluid (CSF), and the intracerebroventricular volume (ICV) and corresponding fractional volumes (f GM = GM/ICV, f WM = WM/ICV, and f CSF = CSF/ICV) were calculated to allow comparison of data from subjects with different head sizes. Each compartment (f GM, f WM, and f CSF) was then corrected for age-related changes by adjusting variables to the mean age of the subjects studied in years), according to the corresponding rates of yearly decline (for fGM, 0.013‰ per year) or yearly increase (for fCSF, 0.015‰ per year), as measured in the database of normal volunteers [2, 23].
PET data acquisition
All subjects underwent static 18F-FDG PET after receiving a 300-MBq injection of 18F-FDG while resting with eyes closed and ears plugged to reduce background noise. About 30 min after tracer injection, images were acquired with an ECAT EXACT 47 scanner (CTI/Siemens). After 5 min of transmission scanning with a 68Ge rod source, emission scanning was performed for 25 min in two-dimensional mode. Emission scans were reconstructed using the back-projection method with a Shepp-Logan filter (cut-off frequency 0.35), resulting in 47 slices with a 128×128 matrix (pixel size 1.8 mm) and an interplane separation of 3.125 mm. The attenuation effects were corrected using measured transmission images.
PET image transformation and statistical analysis
PET images were converted into Analyze format using ImageJ software (http://rsb.info.nih.gov/ij/). Integrated analysis of PET studies and coregistered segmented MR images was performed with software that included a correction for partial-volume effects and a region-of-interest module [24]. Partial-volume effects were corrected according to the methods of Muller-Gartner et al. [25]. Regions of interest were defined in the normalized space of Talairach using the automated voxel-identification routine of the Talairach Daemon software [26, 27]. The regions of interest encompassed the major GM structures (frontal, parietal, occipital and temporal lobes, basal ganglia, and cerebellum). In order to apply this region-of-interest set to each subject’s image dataset in the original space, we applied to the ROI set in the Montreal Neurological Institute space the parameters for normalization of the subject’s PET image onto the PET template space of statistical parametric mapping. Data were normalized by mean global counts.
Statistics
The rate of volume and metabolic change over time was calculated for GM and FDG-PET uptake according to the following formula: rate of change = (delayed scan)−(baseline scan)/(delayed scan)×100/(time between scans). Differences in the rate of change between riluzole-treated and placebo-treated patients were compared using t statistics, controlling for age and sex. The linear dependence of PET-normalized data on UHDRS I and UHDRS III score was determined by a simple regression model. A significance level of p≤0.05 was chosen. Statistical analysis was performed with the JMP statistical software package (SAS, Cary, NC).
Results
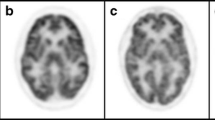
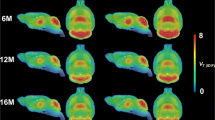
After a mean interval of 24 months we observed brain volumetric structural and metabolic changes in several cortical areas both in the 11 riluzole-treated patients and in the 12 placebo-treated patients (Table 1 and Fig. 1). Placebo-treated patients showed significantly greater proportional volume loss of fGM and decrease in metabolic FDG uptake than patients treated with riluzole in all cortical areas (p<0.05). All subjects showed a similar mean clinical score at UHDRS I and III (Table 1) associated with their HD stage. However, the decreased rate of metabolic FDG changes observed in several areas of the frontal, parietal and occipital cortex in placebo-treated patients correlated linearly with the severity of the UHDRS I score, rating motor performance (Fig. 2). The same rate of metabolic change in the frontal and temporal areas of the brain cortex in placebo-treated patients correlated linearly with worsening UHDRS III score, rating the severity of behavioural manifestations (Fig. 3). Differences in the distribution of longitudinal metabolic changes in the brain cortex in both placebo-treated and riluzole-treated patients are shown in Fig. 4. Serum levels of BDNF and TGF beta-1, but not those of GDNF, were significantly increased in patients treated with riluzole (Fig. 5). No significant differences in the changes in the clinical scores were detected between the riluzole-treated and placebo-treated patients, nor were they correlated with metabolic brain changes.
Linear correlation between the rate of decrease in FDG uptake in cortical brain areas and worsening UHDRS-I motor scores in placebo-treated patients: a parietal cortex; b occipital cortex; c cingulate. Regression equations are: a y = −0.25x + 6.38 (r 2 = 0.45, p = 0.027); b y = −0.21x + 8.64 (r 2 = 0.34, p = 0.046); c y = −0.16x + 1.24 (r 2 = 0.43, p = 0.021)
Linear correlation between the rate of decrease in FDG uptake in cortical brain areas and worsening UHDRS-III behavioural scores in placebo-treated patients: a frontal lobe; b temporal lobe. Regression equations are: a y = −0.31x + 1.87 (r 2 = 0.48, p = 0.012); b y = −0.27x + 3.46 (r 2 = 0.53, p = 0.008)
Neurotrophin serum levels in riluzole-treated patients, placebo-treated patients and healthy control subjects. a Increased levels of BDNF in riluzole-treated patients compared with placebo-treated patients (p<0.05) and control subjects. b Unchanged levels of GDNF in riluzole-treated patients. c Increased levels of TGF beta-1 in riluzole-treated patients compared with placebo-treated patients (p<0.05) and control subjects
Discussion
We sought to determine whether riluzole could be neuroprotective in HD, adopting a strategy that combined imaging, clinical and biochemical data from a relatively small but well-characterized cohort of patients, longitudinally followed-up for 2 years [20]. Considering that follow-up is relatively restricted in most pharmacological studies (not exceeding 3–4 years), we compared the worsening (instead of the improvement) in metabolic and structural brain changes in riluzole-treated patients to those in placebo-treated patients matched by age, gender, mutation size, and disease stage. We believe that the short follow-up as in this and other studies [20, 28] may have resulted in failure to detect improvements in clinical scores. Moreover, to be neuroprotective and to be extended to the presymptomatic life stage, an HD phase where no visible symptoms are manifesting, a drug needs to at least interfere with biological markers reflecting HD neuropathology. In our study we unequivocally demonstrated that glucose metabolism and brain structure were preserved in those patients who received riluzole, an antiglutamatergic agent that increases blood levels of the neurotrophins BDNF and TGF beta-1. The missing increase in GDNF is not surprising, as this neurotrophin strictly depends on BDNF [29] and TGF beta-1 [30] to exert its neurotrophic potential.
An interesting finding of the current study is the linear correlation between the progressive metabolic glucose consumption and the severity of UHDRS scores, internationally validated rating scales [22], in patients who did not receive riluzole. This finding corroborates the potential role of FDG-PET as a valid examination to test brain markers of HD, and gives strength to the hypothesis that riluzole interferes with progressive brain hypometabolism in patients with HD. Even more interestingly, increasing motor scores in placebo-treated patients were related to metabolic changes extensively occurring in the whole cortical brain area, particularly the parietal cortex [3], whilst metabolic changes in the frontal and temporal areas correlated with increasing scores of behavioural manifestations (particularly obsessive behaviour was related to the frontal and temporal areas and apathy to temporal hypometabolism). This finding is in line with the hypothesis that parietal areas might influence motor manifestations [3] whilst psychiatric manifestations may depend on frontal [31] and temporal dysfunction [32]. A potential beneficial effect on symptoms might perhaps be highlighted after several years of treatment, and this may explain why a previous large study over 4 years failed to highlight such improvement [28].
These findings offer strength to the hypothesis that antiglutamatergic drugs do represent a neuroprotective strategy in HD and that riluzole should be seriously considered as a well-tolerated pharmacological therapy with the potential to be extended to subjects at the presymptomatic stage [33]. For instance, the discovery of distinct brain and peripheral markers that highlight the progression from one stage to another would certainly represent a crucial step in determining the best treatment [34].
References
Vonsattel JP, Myers RH, Stevens TJ, Ferrante RJ, Bird ED, Richardson EP Jr. Neuropathological classification of Huntington’s disease. J Neuropathol Exp Neurol 1985;44:559–77. doi:10.1097/00005072-198511000-00003.
Ciarmiello A, Cannella M, Lastoria S, Simonelli M, Frati L, Rubinsztein DC, et al. Brain white-matter volume loss and glucose hypometabolism precede the clinical symptoms of Huntington’s disease. J Nucl Med 2006;47:215–22.
Rosas HD, Salat DH, Lee SY, Zaleta AK, Pappu V, Fischl B, et al. Cerebral cortex and the clinical expression of Huntington’s disease: complexity and heterogeneity. Brain 2008;131:1057–68. doi:10.1093/brain/awn025.
Beal MF, Kowall NW, Ellison DW, Mazurek MF, Swartz KJ, Martin JB. Replication of the neurochemical characteristics of Huntington’s disease by quinolinic acid. Nature 1986;321:168–71. doi:10.1038/321168a0.
Gauthier LR, Charrin BC, Borrell-Pages M, Dompierre JP, Rangone H, Cordelières FP, et al. Huntingtin controls neurotrophic support and survival of neurons by enhancing BDNF vesicular transport along microtubules. Cell 2004;118:127–38. doi:10.1016/j.cell.2004.06.018.
Ciammola A, Sassone J, Cannella M, Calza S, Poletti B, Frati L, et al. Low brain-derived neurotrophic factor (BDNF) levels in serum of Huntington’s disease patients. Am J Med Genet B Neuropsychiatr Genet 2007;144B:574–7. doi:10.1002/ajmg.b.30501.
Zuccato C, Ciammola A, Rigamonti D, Leavitt BR, Goffredo D, Conti L, et al. Loss of huntingtin-mediated BDNF gene transcription in Huntington’s disease. Science 2001;293:493–8. doi:10.1126/science.1059581.
Schaub RT, Anders D, Golz G, Göhringer K, Hellweg R. Serum nerve growth factor concentration and its role in the preclinical stage of dementia. Am J Psychiatry 2002;159:1227–9. doi:10.1176/appi.ajp.159.7.1227.
Tesseur I, Zou K, Esposito L, Bard F, Berber E, Can JV, et al. Deficiency in neuronal TGF-beta signaling promotes neurodegeneration and Alzheimer’s pathology. J Clin Invest 2006;116:3060–9. doi:10.1172/JCI27341.
Pérez-Navarro E, Arenas E, Reiriz J, Calvo N, Alberch J. Glial cell line-derived neurotrophic factor protects striatal calbindin-immunoreactive neurons from excitotoxic damage. Neuroscience 1996;75:345–52. doi:10.1016/0306-4522(96)00336-3.
Bruno V, Battaglia G, Casabona G, Copani A, Caciagli F, Nicoletti F. Neuroprotection by glial metabotropic glutamate receptors is mediated by transforming growth factor-beta. J Neurosci 1998;18:9594–600.
Browne SE, Beal MF. Oxidative damage in Huntington’s disease pathogenesis. Antioxid Redox Signal 2006;8:2061–73. doi:10.1089/ars.2006.8.2061.
Hodges A, Strand AD, Aragaki AK, Kuhn A, Sengstag T, Hughes G, et al. Regional and cellular gene expression changes in human Huntington’s disease brain. Hum Mol Genet 2006;15:965–77. doi:10.1093/hmg/ddl013.
Feigin A, Ghilardi MF, Huang C, Ma Y, Carbon M, Guttman M, et al. Preclinical Huntington’s disease: compensatory brain responses during learning. Ann Neurol 2006;59:53–9. doi:10.1002/ana.20684.
Squitieri F, Ciarmiello A, Di Donato S, Frati L. The search for cerebral biomarkers of Huntington’s disease: a review of genetic models of age at onset prediction. Eur J Neurol 2006;13:408–15. doi:10.1111/j.1468-1331.2006.01264.x.
Giorgini F, Guidetti P, Nguyen Q, Bennett SC, Muchowski PJ. A genomic screen in yeast implicates kynurenine 3-monooxygenase as a therapeutic target for Huntington disease. Nat Genet 2005;37:526–31. doi:10.1038/ng1542.
Squitieri F, Berardelli A, Nargi E, Castellotti B, Mariotti C, Cannella M, et al. Atypical movement disorders in the early stages of Huntington’s disease: clinical and genetic analysis. Clin Genet 2000;58:50–6. doi:10.1034/j.1399-0004.2000.580108.x.
Bergerot A, Shortland PJ, Anand P, Hunt SP, Carlstedt T. Co-treatment with riluzole and GDNF is necessary for functional recovery after ventral root avulsion injury. Exp Neurol 2004;187:359–66. doi:10.1016/j.expneurol.2004.02.003.
Katoh-Semba R, Asano T, Ueda H, Morishita R, Takeuchi IK, Inaguma Y, et al. Riluzole enhances expression of brain-derived neurotrophic factor with consequent proliferation of granule precursor cells in the rat hippocampus. FASEB J 2002;16:1328–30.
Squitieri F, Ciammola A, Colonnese C, Ciarmiello A. Neuroprotective effects of riluzole in Huntington’s disease. Eur J Nucl Med Mol Imaging 2008;35:221–2. doi:10.1007/s00259-007-0615-y.
Squitieri F, Gellera C, Cannella M, Mariotti C, Cislaghi G, Rubinsztein DC, et al. Homozygosity for CAG mutation in Huntington disease is associated with a more severe clinical course. Brain 2003;126:946–55. doi:10.1093/brain/awg077.
Huntington Study Group. The Unified Huntington’s Disease Rating Scale: reliability and consistency. Mov Disord 1996;11:136–42. doi:10.1002/mds.870110204.
Alfano B, Brunetti A, Covelli EM, Quarantelli M, Panico MR, Ciarmiello A, et al. Unsupervised, automated segmentation of the normal brain using a multispectral relaxometric magnetic resonance approach. Magn Reson Med 1997;37:84–93. doi:10.1002/mrm.1910370113.
Quarantelli M, Berkouk K, Prinster A, Landeau B, Svarer C, Balkay L, et al. Integrated software for the analysis of brain PET/SPECT studies with partial-volume-effect correction. J Nucl Med 2004;45:192–201.
Muller-Gartner HW, Links JM, Prince JL, Bryan RN, McVeigh E, Leal JP, et al. Measurement of radiotracer concentration in brain gray matter using positron emission tomography: MRI-based correction for partial volume effects. J Cereb Blood Flow Metab 1992;12:571–83.
Rousset OG, Ma Y, Evans AC. Correction for partial volume effects in PET: principle and validation. J Nucl Med 1998;39:904–11.
Research Imaging Center, University of Texas Health Science Center at San Antonio. Talairach Daemon Client download. http://www.talairach.org/client.html. Accessed 26 Feb 2009.
Landwehrmeyer GB, Dubois B, de Yébenes JG, Kremer B, Gaus W, Kraus PH, et al. Riluzole in Huntington’s disease: A 3-year, randomized controlled study. Ann Neurol 2007;62:262–72. doi:10.1002/ana.21181.
Giehl KM, Schütte A, Mestres P, Yan Q. The survival-promoting effect of glial cell line-derived neurotrophic factor on axotomized corticospinal neurons in vivo is mediated by an endogenous brain-derived neurotrophic factor mechanism. J Neurosci 1998;18:7351–60.
Krieglstein K, Henheik P, Farkas L, Jaszai J, Galter D, Krohn K, et al. Glial cell line-derived neurotrophic factor requires transforming growth factor-beta for exerting its full neurotrophic potential on peripheral and CNS neurons. J Neurosci 1998;18:9822–34.
Paradiso S, Turner BM, Paulsen JS, Jorge R, Ponto LL, Robinson RG. Neural bases of dysphoria in early Huntington’s disease. Psychiatry Res 2008;162:73–87. doi:10.1016/j.pscychresns.2007.04.001.
Lehto SM, Kuikka J, Tolmunen T, Valkonen-Korhonen M, Joensuu M, Saarinen PI, et al. Temporal cortex dopamine D2/3 receptor binding in major depression. Psychiatry Clin Neurosci 2008;62:345–8. doi:10.1111/j.1440-1819.2008.01814.x.
Squitieri F, Cannella M, Frati L. Molecular medicine: predicting and preventing Huntington’s disease. Neurol Sci 2008;29:205–7. doi:10.1007/s10072-008-0969-3.
Squitieri F, Cannella M, Simonelli M, Sassone J, Martino T, Venditti E, et al. Distinct brain volume changes correlating with clinical stage, disease progression rate, mutation size and age at onset prediction as early biomarkers of brain atrophy in Huntington’s disease. CNS Neurosci Ther 2009;15:1–11.
Acknowledgments
We thank Dr. Jenny Sassone for providing help in setting up the ELISA analysis of patients’ serum. We also thank the European Huntington’s Disease (EURO-HD) Network, the patients’ family association ‘Associazione Italiana Corea di Huntington-Neuromed’, the Italian Society of Hospital Neurologists (S.N.O., ‘lascito Gobessi’) and the Italian Health Ministry (COFIN 2006; finalizzato ex art.56 2007), for their support to F.S. The financial support of Telethon-Italy to F.S. (grant no. GGP06181) is gratefully acknowledged.
Author information
Authors and Affiliations
Corresponding authors
Rights and permissions
About this article
Cite this article
Squitieri, F., Orobello, S., Cannella, M. et al. Riluzole protects Huntington disease patients from brain glucose hypometabolism and grey matter volume loss and increases production of neurotrophins. Eur J Nucl Med Mol Imaging 36, 1113–1120 (2009). https://doi.org/10.1007/s00259-009-1103-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00259-009-1103-3