Abstract
Purpose
The purpose of the study was to investigate the associations between uptake of 111In-DTPA-trastuzumab, tumour HER2 density and response to trastuzumab (Herceptin) of human breast cancer (BC) xenografts in athymic mice.
Materials and methods
The tumour uptake of 111In-DTPA-trastuzumab in athymic mice bearing BC xenografts with increasing HER2 density (0 to 3+) was evaluated. Specific uptake ratios were established in biodistribution (SUR) and imaging studies (ROI-SUR) using 111In-labeled mouse IgG (111In-DTPA-mIgG). Further corrections were made for circulating radioactivity using tumour-to-blood ratios defined as a localization index (LI) and region-of-interest localization index (ROI-LI), respectively. Mice were treated with trastuzumab (Herceptin). A tumour growth inhibition index (TGI) was calculated and relative TGIs calculated by dividing the TGI of control by that of trastuzumab-treated mice.
Results
Strong, nonlinear associations with HER2 density were obtained if the uptake of 111In-DTPA-trastuzumab was corrected for nonspecific IgG localization (i.e., SUR; r 2 = 0.99) and circulating radioactivity (i.e., LI; r 2 = 0.87), but without these corrections, the association between HER2 density and tumour uptake was poor (r 2 = 0.22). There was a strong association between ROI-SUR and ROI-LI values and HER2 expression (r 2 = 0.90 and r 2 = 0.95, respectively. All tumours were imaged. Relative TGI values were associated with increasing uncorrected tumour uptake of 111In-DTPA-trastuzumab but not always with HER2 density (i.e., MCF-HER2-18 cells with trastuzumab-resistance).
Conclusion
HER2 expression (0 to 3+) can be differentiated using 111In-DTPA-trastuzumab, but requires correction of tumour uptake for nonspecific IgG localization and circulating radioactivity. The uncorrected uptake of 111In-DTPA-trastuzumab was associated with tumour response to trastuzumab.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Trastuzumab (Herceptin®) is a humanized IgG1 monoclonal antibody (mAb) which exploits the overexpression of the HER2 transmembrane receptor tyrosine kinase found in about 20% of cases of breast cancer (BC). This immunotherapeutic agent has clinical benefit in patients with metastatic HER2-positive disease both as a single agent and in combination with chemotherapy [1, 2]. Trastuzumab has also recently been approved as an adjuvant treatment for early stage BC based on improved disease-free and overall survival as well as decreased risk of recurrence [3]. Patients are selected for trastuzumab-based therapies by assessment of tumour HER2 overexpression by immunohistochemical (IHC) staining or probing HER2 gene amplification using fluorescence in situ hybridization (FISH) [4]. Despite pre-selection of patients with HER2-positive tumours, only a minority respond to the drug as a single agent (12–35%) [5]. Response rates improve to 40–60% when trastuzumab is combined with anthracyclines or taxanes [2, 6].
Inherent in the restriction of trastuzumab to patients with tumours that overexpress HER2 is the assumption that tumour uptake of the drug is proportional to HER2 density and that uptake is directly correlated with therapeutic response. Indeed, Phase II clinical trials of trastuzumab revealed that the overall response rate to trastuzumab was higher in those with HER2 highly overexpressing tumours (IHC score 3+) compared to those with moderate HER2 density (IHC score 2+), presumably due to higher tumour uptake [2]. Molecular imaging using radiolabeled forms of trastuzumab could potentially probe the level of tumour HER2 expression as well as directly visualize the delivery of the drug to tumours (at least administered in a single radiotracer dose) and thus may be useful for predicting patient response to trastuzumab [7]. This premise was previously examined by Behr et al. in a study of 20 patients with metastatic BC, who found that 11 patients with tumour uptake of 111In-DTPA-trastuzumab responded to trastuzumab, whereas only one patient without tumour uptake benefited [8]. Many forms of trastuzumab (i.e., IgG, Fab and scFv fragments), as well as anti-HER2 affibodies, minibodies and diabodies, labeled with single γ-photon-emitters (e.g., 111In, 99mTc, 131I) or positron-emitters (e.g., 68Ga, 124I and 89Zr) have been investigated for imaging HER2-positive tumours both preclinically [9–17] and clinically [8, 18–19]. However, a limitation of these studies was that they did not attempt to define the quantitative associations between radiopharmaceutical uptake and tumour HER2 density, especially for tumours with a wide range of receptor expression (i.e., IHC scores 0 to 3+), nor did they examine the relationship between these parameters and tumour response to trastuzumab. Our objective was therefore to conduct the first preclinical study, to our knowledge, investigating these important associations for 111In-DTPA-trastuzumab, in a panel of human BC xenografts in athymic mice with widely varying HER2 expression. HER2 density was characterized by radioligand binding assays as well as by more clinically relevant tests (i.e., IHC and FISH) to allow interpretation of the results in the clinical context of patient tumour characteristics. 111In-DTPA-trastuzumab IgG was used for these studies because it was believed that it would be the most representative of trastuzumab and, therefore, the most suitable for establishing these associations.
Materials and methods
Breast cancer cells
Human breast cancer (BC) cells (MDA-MB-231, MDA-MB-361, SK-Br-3 and BT-20) were purchased from the American Type Culture Collection (ATCC, Manassas, VA, USA). A variant of BT-474 cells with stable bimodal (assessed by repeated HER2 characterization after multiple cell passages) and overall low (1+) HER2 expression was used. To distinguish this BT-474 variant from those reported that have higher HER2 density [9], these cells were annotated as BT-474HET. Stably transfected MCF/HER2-18 cells were donated by Dr. Mien-Chie Hung (MD Anderson Cancer Center, Houston, TX, USA) [20]. Cells were cultured in the recommended media supplemented with 10–20% fetal bovine serum (FBS, Sigma-Aldrich). MCF/HER2-18 cells were supplemented with G418 sulphate (0.5 mg/mL; Geneticin®, Invitrogen, Carlsbad, CA, USA).
Preparation and characterization of 111In-DTPA-trastuzumab
Trastuzumab (Herceptin®, Hoffman-La Roche, Mississauga, ON, USA) or nonspecific mouse IgG (mIgG; Sigma-Aldrich Product I5381) was derivatized with a fourfold excess of diethylenetriaminepentaacetic acid (DTPA) dianhydride (Sigma-Aldrich) [21]. The conjugation efficiency and DTPA substitution level were calculated as described previously [9]. DTPA-trastuzumab was purified and reconcentrated to 10 mg/mL in 1 mol/L CH3COONa buffer by ultrafiltration on a Microcon YM-30 device (Amicon, Billerica, MA, USA). DTPA-trastuzumab was labeled with 111InCl3 (MDS Nordion, Kanata, ON), to a specific activity of 0.02–1 MBq/μg. 111In-DTPA-trastuzumab was purified on a Sephadex G-50 mini-column (Sigma-Aldrich). The final radiochemical purity was >97% measured by instant thin layer-silica gel chromatography (ITLC-SG) [9] and size-exclusion high performance liquid chromatography (SE-HPLC) performed on a BioSep SEC-S2000 column (300 × 7.8 mm; Phenomenex, Torrance, CA, USA) eluted with 100 mM NaH2PO4 buffer, pH 7.0 at a flow rate of 0.8 mL/min using a Series 200 pump (PerkinElmer, Wellesley, MA, USA) interfaced with a diode array detector (PerkinElmer) set at 280 nm and a Radiomatic 610TR flow scintillation analyzer (PerkinElmer).
The immunoreactive fraction (IRF) of 111In-DTPA-trastuzumab was measured by the Lindmo method [22]. Briefly, 10 ng of 111In-DTPA-trastuzumab was incubated with 9.3 × 105 to 3.0 × 107 SK-Br-3 cells/mL in 500 μl of serum-free cell culture media for 3 h at room temperature. Cells were rinsed three times to remove unbound radioactivity. The cell pellets containing bound 111In-DTPA-trastuzumab were counted in a γ-counter (Wizard 3, PerkinElmer). Nonspecific binding was estimated in the presence of 100-fold excess of unlabeled trastuzumab. Bound/total radioactivity was plotted vs. the inverse of cell concentration. The IRF was obtained from the inverse of the intercept on the ordinate as reported by Lindmo [22].
Saturation receptor-binding assays
The HER2 receptor density (average number of receptors/cell) on BC cells and the dissociation constants (K d) for 111In-DTPA-trastuzumab were measured in radioligand saturation receptor-binding assays. Approximately 5 × 104 HER2 overexpressing SK-Br-3 or MCF/HER2-18 cells were plated overnight in 24-well plates (Sarstedt, Montreal, QC). The adherent cells were then incubated in serum-free culture media with increasing concentrations of 111In-DTPA-trastuzumab (0–150 nmol/L, 0.02 MBq/µg) in a total volume of 500 μL for 3 h at 4˚C. Unbound radioactivity was removed, and the cells were rinsed twice with ice-cold phosphate-buffered saline (PBS), pH 7.0. The cells were dissolved in 0.1 mol/L NaOH and the cell-bound radioactivity counted in a γ-counter. K d values and the concentration of 111In-DTPA-trastuzumab required to saturate the receptors (B max) were calculated by fitting a plot of cell-bound 111In-DTPA-trastuzumab (nmol) vs. the concentration of unbound radioligand (nmol/L, corrected for IRF) to a one-site saturation binding model using Prism® Ver. 4.0 software (GraphPad Software, San Diego, CA, USA). This model fitting corrects the total binding for nonspecific binding by assuming that it is proportional to radioligand concentration. B max values (nmol) were converted to the number of HER2 receptors/cell. The HER2 expression of MDA-MB-231, BT-20, MDA-MB-361 and BT-474HET cells were measured in one-point binding assays performed by incubating 4 × 105 cells/well in six-well plates with 2 mL of 60 nmol/L of 111In-DTPA-trastuzumab sufficient to saturate the receptors. These assays were conducted in the presence (nonspecific binding) or absence (total binding) of a 100-fold molar excess of unlabeled trastuzumab. B max was similarly calculated and converted to the number of receptors/cell.
Immunohistochemistry
Immunohistochemistry (IHC) staining for HER2 was performed in triplicate on human BC cell lines. Cell pellets were coated in 3% agar, and the agar blocks were fixed in 10% neutral buffered formalin for 24 h before being paraffin-embedded. Sections (4 μm) were dewaxed and rehydrated prior to antigen retrieval. Endogenous peroxidase and biotin activities were blocked using 3% H2O2 and an avidin/biotin blocking kit, respectively (Vector Laboratories, Burlington, ON). Sections were then blocked for 15 min with 10% normal serum and incubated with a mouse anti-c-erbB-2 monoclonal antibody (CB11; Novocastra Laboratories, Newcastle, UK; 1/100) for 1 h at room temperature (RT), followed by an anti-mouse biotinylated secondary antibody (Vector Laboratories) for 30 min and a horseradish peroxidase-conjugated ultrastreptavidin labeling reagent (ID Labs™, London, ON) for 30 min. Sections were washed twice with PBS and the reaction product was visualized using NovaRed solution (Vector Laboratories) and counterstained lightly with Mayer’s hematoxylin. Finally, sections were dehydrated, cleared in xylene, and mounted in Permount (Fisher Scientific, Ottawa, ON). Negative control sections were prepared with omission of the primary anti-c-erbB-2 antibody. All slides were scored based on the percentage of moderate-to-strongly staining cells with complete membrane staining.
Fluorescence in situ hybridization
Fluorescence in situ hybridization (FISH) was performed on BC cells using the PathVysion HER-2 probe (Abbott Molecular, Des Plaines, IL, USA) according to the manufacturer’s instructions. The kit consists of a HER-2 gene DNA probe labeled with SpectrumOrange, which maps to 17q11.2–q12, and a CEP17 chromosome 17-specific alpha-satellite DNA probe labeled with SpectrumGreen. Fluorescence signals were detected with the Leica DMLB fluorescence microsope (Leica Microsystems, Wetzlar, Germany) using DAPI, FITC and Texas Red filters. Representative cells were imaged digitally using the CytoVision (Applied Imaging, San Jose, CA, USA) image capturing system. Sixty nuclei were scored for each cell line. A HER2:CEP17 ratio of ≥ 2.2 was considered HER-2 amplified [4].
Tumour and normal tissue uptake of 111In-DTPA-trastuzumab
The tumour and normal tissue uptake of 111In-DTPA-trastuzumab were determined in female athymic CD1nu/nu mice (Charles River, Wilmington, MA, USA) bearing s.c. MDA-MB-361 BC xenografts. Mice were inoculated s.c. in the right thigh with 1 × 107 cells in 100 μL of growth medium mixed with 100 μL of Matrigel (BD Biosciences) at 24 h after s.c. implantation of a 0.72 mg, 60-day sustained-release 17β-estradiol pellet (Innovative Research of America, Sarasota, FL, USA). Once the tumours had reached an average volume of 240 mm3, groups of four mice received an i.v. (tail vein) injection of 111In-DTPA-trastuzumab or 111In-DTPA-mIgG (10 μg, 0.2–0.4 MBq) in 200 μL of sodium chloride injection USP. One group of mice received an 80-fold excess of unlabeled trastuzumab 24 h prior to injection of 111In-DTPA-trastuzumab to assess the specificity of tumour uptake. At 72 h post-injection (p.i.), the mice were sacrificed, and the tumour, blood and normal tissues were collected, weighed and their radioactivity counted in a γ-counter. This time point has been shown to produce optimal tumour-to-background ratios for 111In-DTPA-trastuzumab IgG [9, 10]. Tumour and normal tissue uptake were expressed as mean ± SD percent injected dose/g (% i.d./g).
Associations between tumour uptake and HER2 density
In order to evaluate the association between HER2 density (average number of receptors/cell) and the tumour uptake of 111In-DTPA-trastuzumab (or 111In-DTPA-IgG), groups of three to four athymic mice were inoculated s.c. with 1 × 107 MDA-MB-231, BT-20, MDA-MB-361, BT-474HET or MCF/HER2-18 BC cells to establish tumour xenografts with varying HER2 expression (0 to 3+). Mice implanted with MDA-MB-361, BT-474HET and MCF/HER2-18 tumour xenografts were pre-inoculated with a sustained-release 17β-estradiol pellet. Tumour and blood concentrations of radioactivity at 72 h p.i. were measured by γ-counting as described earlier. Tumour uptake was expressed as % i.d./g or by a specific uptake ratio (SUR), which was defined as the uptake (% i.d./g) of 111In-DTPA-trastuzumab divided by that of 111In-DTPA-mIgG. In addition, blood concentrations of radioactivity were used to establish a localization index (LI), which was defined as the tumour/blood (T/B) ratio of 111In-DTPA-trastuzumab divided by that of 111In-DTPA-mIgG.
Tumour imaging with 111In-DTPA-trastuzumab
Imaging was performed at 72 h p.i. of 10 µg (7–10 MBq) of 111In-DTPA-trastuzumab or 111In-DTPA-mIgG in tumour-bearing athymic mice using a small field-of-view clinical γ-camera (ADAC Model TransCam, ADAC Laboratories, Milpitas, CA) fitted with a 4-mm pinhole collimator. Planar images were collected into a 256 × 256 × 16 acquisition matrix for a total of 250,000 counts. Region of interest (ROI) analysis was performed and counts in tumour ROIs reported as the mean ± SD percent injected dose per pixel (% i.d./pixel). Specific tumour uptake was defined as an ROI uptake ratio (ROI–SUR) calculated by dividing the mean tumour counts (% i.d./pixel) for 111In-DTPA-trastuzumab by that of 111In-DTPA-mIgG. To account for blood pool radioactivity, an ROI localization index (ROI-LI) was defined as the mean ratio of tumour/heart (mediastinal radioactivity) counts for 111In-DTPA-trastuzumab divided by that of 111In-DTPA-mIgG. The principles of Laboratory Animal Care (NIH Publication No. 86-23, revised 1985) were followed, and all animal studies were conducted under a protocol approved by the Animal Care Committee at the University Health Network (No. 989.2) in accordance with Canadian Council on Animal Care (CCAC) guidelines.
Tumour response to trastuzumab
Groups of six to eight athymic mice bearing BC xenografts (110 ± 70 mm3) were randomly assigned to treatment with trastuzumab or PBS (control group). A second group of control mice bearing MDA-MB-361 tumours were treated with nonspecific human IgG (hIgG; Sigma-Aldrich Product I4506). Mice were administered trastuzumab intraperitoneally (i.p.) with a loading dose of 4 mg/kg followed by weekly doses of 2 mg/kg for 4 weeks, diluted in PBS to a final volume of 100 µL. We previously determined that trastuzumab is rapidly absorbed from an i.p. injection in mice within 24 h (unpublished data). Tumours were measured weekly using calipers and tumour volume calculated using the formula: length × width 2 × 0.5. Tumour growth was normalized to the initial tumour volume (tumour growth index; TGI) and the mean TGI was compared for trastuzumab treated vs. control mice and between groups of mice implanted with the different BC xenografts. The TGI of PBS controls was divided by the TGI of trastuzumab-treated xenografts (relative TGI) for comparisons with HER2 density or uptake of 111In-DTPA-trastuzumab.
Statistical analysis
Tumour uptake of 111In-DTPA-trastuzumab or 111In-DTPA-mIgG was compared between xenograft models using one-way parametric ANOVA using the Bonferroni correction for multiple comparisons (P < 0.05). Scatterplots were generated for comparisons between tumour uptake, SUR, ROI-SUR, LI, and ROI-LI and HER2 density. These were fitted to a one-site nonlinear association model using GraphPad Prism 4.0 and r 2 values calculated. Correlations between biodistribution (SUR and LI) and imaging (ROI-SUR and ROI-LI) results were made using Pearson’s correlation (P < 0.05). All other statistical comparisons were made using Student’s t test (P < 0.05).
Results
Preparation and characterization of 111In-DTPA-trastuzumab
Under the conditions used, trastuzumab was derivatized with 1.4 ± 0.3 DTPA groups per IgG molecule (n = 10). DTPA-derivatized trastuzumab was labeled with 111InCl3 to a final radiochemical purity of >97%. SE-HPLC analysis showed one major peak (t R = 7.8 min) corresponding to monomeric 111In-DTPA-trastuzumab IgG with minimal (<10%) evidence of intermolecular cross-linking (t R = 7.1 min; results not shown). The IRF of 111In-DTPA-trastuzumab at infinite antigen (HER2) excess was 0.64 ± 0.04.
Saturation receptor-binding assays
111In-DTPA-trastuzumab demonstrated saturable binding to HER2-overexpressing SK-Br-3 and MCF/HER2–18 cells which was displaceable by a 100-fold excess of unlabeled trastuzumab (results not shown). The K d was 1.7 ± 0.8 × 10–9 mol/L and 1.2 ± 0.5 × 10–9 mol/L for SK-Br-3 and MCF/HER2–18 cells, respectively (not significantly different; P > 0.05). B max values expressed as the number of HER2 receptors/cell and the correlation with IHC and FISH results are summarized in Table 1. HER2 density ranged from 5.4 ± 0.7 × 104 receptors/cell for MDA-MB-231 cells to 1.3 ± 0. × 106 receptors/cell for SK-Br-3 cells. The overall HER2 density of BT-474HET cells was 1.3 ± 0.7 × 105 receptors/cell, although IHC and FISH confirmed that there was a bimodal distribution. MCF/HER2-18 cells displayed 1.2 ± 0.1 × 106 HER2 receptors/cell and were used to establish tumour xenografts that exhibit high HER2 expression (3+), since SK-Br-3 cells are not tumourigenic. Based on the number of receptors per cell, BC cells were assigned relative HER2 expression scores of 0 to 3+ (Table 1) to relate these to more commonly used IHC staining scores that were previously assigned to cells with known HER2 densities (0: 20,000; 1+: 100,000; 2+: 500,000 and 3+: 2,000,000) [23–25].
Immunohistochemistry
Greater than 10% tumour cells with moderate-to-strong, complete membrane staining by IHC (Fig. 1a and Table 1) was considered clinically HER2-positive [26]. MDA-MB-231 and BT-20 cell lines had <1% and 0%, respectively, of immunopositive cells. MDA-MB-361 cells were 45% positive and MCF/HER2-18 cells were 38% positive. BT-474HET cells showed 5% staining, while SK-Br-3 cells had 98% of HER2-positive cells. Using the applied criteria, IHC classified MDA-MB-231, BT-20 and BT-474HET cells as HER2-negative and MDA-MB-361, MCF/HER2–18 and SK-Br-3 cells as HER2-positive.
Characterization of HER2 expression in a panel of human breast cancer cells lines. a Immunohistochemical (IHC) staining of the cells [I. MDA-MB-231, II. BT-474HET, III. BT-20, IV. MDA-MB-361, V. MCF/HER2–18 and VI. SK-Br-3; percentages of HER2-positive cells are shown]. b Corresponding fluorescence in situ hybridization (FISH) results [HER2:CEP17 ratios are indicated]
Fluorescence in situ hybridization
FISH (Fig. 1b and Table 1) revealed that MDA-MB-231 and BT-20 cells were not HER2 gene-amplified (HER2:CEP17 ratios <2.2), whereas MDA-MB-361 and SK-Br-3 cells exhibited gene amplification ratios of >5 and >3, respectively. FISH confirmed that BT-474HET cells harbored HER2 gene-amplified (ratio of >3) and non gene-amplified (ratio of 1) cells. Despite high surface HER2 expression, MCF/HER2-18 cells did not exhibit gene amplification detected by FISH (ratio of 0.7). This may be explained by poor hybridization of the PathVysion HER-2 probe to the transfected HER2 cDNA, which is only 4.6 kb (comprising only the coding region of HER2) in contrast to its more efficient hybridization to the HER2 amplicon that is greater than 280 kb [27].
Tumour and normal tissue uptake of 111In-DTPA-trastuzumab
The tumour and normal tissue uptake of 111In-DTPA-trastuzumab at 72 h p.i. in athymic mice bearing HER2 2+ MDA-MB-361 BC xenografts is shown in Table 2. Tumour accumulation of radioactivity for mice receiving 111In-DTPA-trastuzumab was more than fourfold higher than for those injected with 111In-DTPA-mIgG (23.4 ± 1.6 vs. 5.5 ± 0.6% i.d./g; P < 0.001). Moreover, pre-injection of an 80-fold excess of unlabeled trastuzumab (800 µg) 24 h prior to 111In-DTPA-trastuzumab decreased tumour uptake 3.3-fold (7.0 ± 2.9 vs. 23.4 ± 1.6% i.d./g, respectively; P < 0.001; Table 2). Tumour uptake of 111In-DTPA-trastuzumab following blocking with unlabeled trastuzumab was not significantly different than that of 111In-DTPA-mIgG (5.5 ± 0.6% i.d./g; P > 0.05). The highest normal tissue concentrations of radioactivity for 111In-DTPA-trastuzumab as well as 111In-DTPA-mIgG were found in the blood, spleen, liver and kidneys (Table 2). Uptake in these tissues was comparable with previous reports for 111In-DTPA-trastuzumab IgG [10, 15].
Associations between tumour uptake and HER2 density
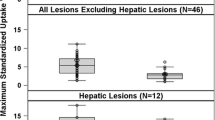
The relationships between tumour uptake of radioactivity for 111In-DTPA-trastuzumab (uncorrected or expressed as SUR or LI) and HER2 density (average number of receptors/cell; Table 1) are shown in Fig. 2. The association between the uncorrected radioactivity and HER2 expression level was poor (r 2 = 0.22; Fig. 2a). The highest tumour uptake (23.4 ± 1.6% i.d./g) was observed for MDA-MB-361 xenografts which displayed 2+ HER2 expression. Lower accumulation of 111In-DTPA-trastuzumab was found in MDA-MB-231, BT-20 and BT-474HET tumours (11.4 ± 1.4, 9.0 ± 1.7% and 13.7 ± 1.5% i.d./g, respectively) with fewer HER2 receptors (0 or 1+). However, the uptake of 111In-DTPA-trastuzumab in highly HER2-positive (3+) MCF/HER2-18 tumours (13.6 ± 3.0% i.d./g) was similar to that in MDA-MB-231, BT-20 or BT-474HET xenografts. In addition, there were significant differences (ANOVA; P < 0.0001) in the uptake of 111In-DTPA-mIgG between the various BC xenografts (Table 3), but no associations were found between these differences and HER2 expression (Fig. 2a).
Associations between HER2 expression levels in a panel of human breast cancer xenografts and tumour uptake of 111In-DTPA-trastuzumab or 111In-DTPA-mIgG at 72 h post-injection. a Tumour uptake expressed as percent injected dose/g [% i.d./g; mean ± SD (n = 4)]. b Tumour uptake expressed as specific uptake ratios (SUR). c Tumour uptake expressed as localization indices (LI)
In contrast to the poor relationship found between the uncorrected tumour uptake of 111In-DTPA-trastuzumab and HER2 density (Fig. 2a), there was a strong, nonlinear association of the SUR values with HER2 expression (r 2 = 0.99; Fig. 2b). SUR values incorporated differences in nonspecific IgG uptake estimated using 111In-DTPA-mIgG, but it was noted that there were also significant differences (ANOVA; P < 0.005) in the blood concentrations of radioactivity between groups of mice injected with 111In-DTPA-trastuzumab or 111In-DTPA-mIgG (Table 3). These differences in the level of circulating radioactivity may affect tumour uptake of the radiopharmaceuticals; therefore, a second LI was established. The association between LI and HER2 density was slightly weaker than the relationship between SUR and HER2 expression (r 2 = 0.99; Fig. 2b), but remained strong (r 2 = 0.87; Fig. 2c).
Tumour imaging with 111In-DTPA-trastuzumab
Tumour as well as normal tissue uptake of radioactivity in the liver, spleen, kidneys and excreted into the bladder were observed on images of mice at 72 h p.i. of 111In-DTPA-trastuzumab or 111In-DTPA-mIgG (Fig. 3). In all BC xenografts (except MDA-MB-231), there was significantly higher uptake of radioactivity in mice injected with 111In-DTPA-trastuzumab than in those receiving 111In-DTPA-mIgG. ROI-SUR values ranged from 0.9 ± 0.3 for MDA-MB-231 tumours (P = 0.42) to 2.8 ± 0.4 for MDA-MB-361 xenografts (P = 0.001) and 2.3 ± 0.8 for MCF/HER2-18 tumours (P = 0.045). There was a poor association between the uncorrected uptake of 111In-DTPA-trastuzumab (% i.d./pixel) and HER2 expression level (r 2 = 0.09; Fig. 4a). However, there was a strong, nonlinear association between ROI-SUR values with HER2 density (r 2 = 0.90; Fig. 4b). This association improved slightly using ROI-LI values (r 2 = 0.95; Fig. 4c) that incorporated differences in blood pool (mediastinal) radioactivity. The accuracy in measuring the relative tumour uptake of 111In-DTPA-trastuzumab and 111In-DTPA-mIgG or blood pool radioactivity on the images was shown by the strong and significant correlation between ROI-SUR and SUR values (r = 0.92, P = 0.03; Fig. 5a) and between ROI-LI and LI values (r = 0.97, P = 0.006; Fig. 5b).
Posterior whole-body planar images of representative athymic mice implanted s.c. in the right hind leg with human breast cancer xenografts (white arrow) at 72 h post-injection of 111In-DTPA-trastuzumab (top row) or 111In-DTPA-mIgG (bottom row). The relative expression of the tumours are: I MDA-MB-231 (0), II BT-474HET (1+), III. BT-20 (1+), IV. MDA-MB-361 (2+), and V. MCF/HER2–18 (3+). Also visualized on the images are the liver (large arrowhead) and kidneys (small arrowhead)
Associations between HER2 expression levels of a panel of human breast cancer xenografts and tumour uptake of 111In-DTPA-trastuzumab or 111In-DTPA-mIgG at 72 h post-injection, determined by ROI analysis. a Tumour uptake expressed as percent injected dose/pixel [% i.d./pixel; mean ± SD (n = 3)]. b Tumour uptake expressed as region-of-interest specific uptake ratios (ROI-SUR). c Tumour uptake expressed as region-of-interest localization indices
Tumour response to trastuzumab
Tumour growth was strongly inhibited by trastuzumab in mice bearing s.c. MDA-MB-361 xenografts with 2+ HER2 expression. TGIs in these trastuzumab-treated mice were significantly lower than in controls treated with PBS (0.5 ± 0.2 vs. 6.9 ± 3.1, respectively; P < 0.002) or those administered hIgG (5.3 ± 2.7; P < 0.004). There were no significant tumour growth-inhibitory effects of trastuzumab on MDA-MB-231 or BT-20 xenografts with lower levels of HER2 (0 and 1+, respectively). TGIs for mice with these tumours treated with trastuzumab were 1.0 ± 0.6 and 1.6 ± 0.8, respectively; these were not significantly different than those for PBS-treated controls (2.5 ± 2.0 and 1.5 ± 1.0, respectively; P > 0.05). MCF/HER2-18 xenografts with 3+ HER2 expression were not growth-inhibited by trastuzumab compared to PBS-treated controls (1.4 ± 0.5 vs. 2.6 ± 2.5, respectively; P > 0.10). A comparison of these trastuzumab treatment outcomes with the uncorrected tumour uptake of 111In-DTPA-trastuzumab (Table 3) revealed that the greatest response was observed for MDA-MB-361 tumours that accumulated the highest concentration of the radiopharmaceutical. MDA-MB-231 and BT-20 tumours with 0 and 1+ HER2 expression, as well as MCF/HER2-18 xenografts (3+) exhibited two- to threefold lower uptake of 111In-DTPA-trastuzumab than MDA-MB-361 tumours and were unresponsive.
Discussion
Molecular imaging has great potential to probe the levels of therapeutically important targets in malignancies such as HER2 [7], but the associations between tumour uptake of the radiopharmaceuticals and the target receptor density, as well as the relationship between these parameters and therapeutic outcome must be established. In this study, we showed that there was a strong, nonlinear association between HER2 density (average number of receptors/cell) on BC cells forming tumour xenografts in athymic mice, and the accumulation of 111In-DTPA-trastuzumab corrected for nonspecific IgG localization (using SUR and ROI-SUR values) or circulating radioactivity (using LI and ROI-LI values). This strong association was found in biodistribution studies (r 2 = 0.87–0.99; Fig. 2) as well as in region-of-interest (ROI) analysis of images (r 2 = 0.90–0.95; Fig. 4). In contrast, only a poor association was found between the uncorrected tumour uptake of 111In-DTPA-trastuzumab and the HER2 expression of BC cells in these studies (r 2 = 0.09–0.22). Cai et al. [28] recently reported the correlation between the uptake of 64Cu-labeled cetuximab and EGFR expression in a panel of tumour xenografts in athymic mice but did not correct for nonspecific IgG localization or blood flow and obtained a poorer correlation (r 2 = 0.80 for % i.d./g and r 2 = 0.64 for tumour/muscle ratios) than we obtained by applying these corrections. The uptake of 111In-DTPA-trastuzumab was specific as revealed by the fourfold significantly lower accumulation of 111In-DTPA-mIgG in MDA-MB-361 tumours (2+ HER2 expression) and the threefold significantly lower uptake of 111In-DTPA-trastuzumab following HER2 receptor blocking by pre-administration of an 80-fold excess of unlabeled trastuzumab (Table 2).
The non-linear associations found between SUR or LI and ROI-SUR or ROI-LI and HER2 density may be due to the limited and small mass (10 µg) of 111In-DTPA-trastuzumab administered; this mass may have been insufficient to saturate all of the receptors on the 3+ MCF/HER2-18 cells. This nonlinearity may also reflect quantitative differences among the tumours in receptor-independent processes that control the uptake of immunoglobulins [29]. Notably, the accumulation of 111In-DTPA-trastuzumab in MCF/HER2-18 tumours was twofold significantly lower than in MDA-MB-361 xenografts (Table 3), despite their twofold higher HER2 density (Table 1). Furthermore, the uptake of nonspecific 111In-DTPA-mIgG was two- to threefold lower in MCF/HER2-18 tumours than in other BC xenografts (Table 3). Nonlinearity in tumour uptake of 111In-DTPA-trastuzumab could similarly occur in patients administered the low masses (5 mg) used for imaging studies [19, 30] and/or due to physiological limitations in delivery of IgGs to lesions [29]. Underestimation of the level of HER2 expression in tumours may occur if a linear relationship between tumour uptake of 111In-DTPA-trastuzumab and HER2 density is assumed. In addition, differences in the proportion of nonspecific IgG uptake or differences in the levels of circulating radioactivity may affect tumour uptake. Correction for these effects in patients may be difficult, but could potentially be achieved in a single study by imaging using 111In-DTPA-trastuzumab and 99mTc-labeled human IgG (hIgG) [31, 32]. Analogous approaches have been used for correction of the tumour uptake of 131I-anti-carcinoembryonic antigen (CEA) monoclonal antibodies in patients for contributions due to blood pool, using 99mTc-human serum albumin [33, 34]. However, differences in the radiochemistry of 99mTc- and 111In-labeled hIgG may contribute to inaccuracies in estimating nonspecific IgG localization, thus requiring two separate studies with 111In-DTPA-trastuzumab and 111In-labeled hIgG which may not be feasible. Alternatively, antibody fragments (e.g., Fab or scFv) of trastuzumab which may have a lower proportion of nonspecific tumour uptake than the intact IgG, could be used to evaluate HER2 expression without these corrections [9, 12]. Nonetheless, the results of our study support the premise that provided that appropriate corrections are applied, four relatively broad but therapeutically important levels of HER2 expression (0, 1, 2 or 3+) could potentially be differentiated in patients by imaging with 111In-DTPA-trastuzumab.
Our study further revealed an association between the uncorrected accumulation of 111In-DTPA-trastuzumab in BC xenografts and response to trastuzumab, irrespective of the HER2 expression level. The greatest response was found in MDA-MB-361 tumours with intermediate (2+) HER2 density; these tumours had a two- to threefold higher uptake of 111In-DTPA-trastuzumab than in the other xenografts, including MCF/HER2-18 (3+) tumours. These results agreed with the report by Behr et al. in which the uncorrected tumour uptake of 111In-DTPA-trastuzumab on SPECT images was associated with response to trastuzumab in BC patients [8]. Our results examining MDA-MB-231, BT-20 and MDA-MB-361 tumours with 0, 1+ or 2+ HER2 expression, respectively, also agreed with current eligibility criteria for trastuzumab in which only patients with tumours with at least 2+ HER2 density are expected to benefit [2–6]. The discordant therapeutic response for HER2 3+ MCF/HER2-18 tumours treated with trastuzumab may be due to low uptake of trastuzumab, perhaps predicted by their twofold lower accumulation of 111In-DTPA-trastuzumab (Table 3) and/or the presence of trastuzumab-resistance mechanisms in these cells [i.e. insulin-like growth factor-1 receptors (IGF-1R)] [35, 36]. Some clinical studies have found an association between IGF-1R expression and a lack of response to trastuzumab [37]. Thus, a similar discordant result may occur in patients between response to trastuzumab, tumour uptake of 111In-DTPA-trastuzumab on images and HER2 overexpression in tumour biopsies. Additional molecular imaging probes that elaborate resistance pathways would be helpful [38]. Further examination of a larger panel of tumour xenografts with 0 to 3+ HER2 expression may be required to fully understand the associations between tumour uptake of 111In-DTPA-trastuzumab, HER2 density and response to trastuzumab.
Ultimately, the use of molecular imaging to assess the level of HER2 expression (0 to 3+) in tumours or for predicting therapeutic outcome will depend on the ability to detect lesions. Clinically, SPECT has limitations in quantifying radionuclide uptake in tissues, including a low γ-photon detection efficiency as well as attenuation by overlying tissues (particularly for deep-seated lesions), contributions from scattered γ-photons and partial volume effects [39, 40]. One study found that only 45% of known lesions in 15 BC patients were detected by SPECT using 111In-DTPA-trastuzumab; but occult lesions were found in 13 patients [19]. In addition, the regional detection rate was higher at 73% (Dr. Pieter Jager, personal communication, November 2007), indicating that many patients had at least one lesion imaged and characterized as HER2-positive. These findings suggest that imaging with 111In-DTPA-trastuzumab may be valuable for making therapeutic decisions even if not all lesions are detected. Furthermore, several investigators have reported that 111In concentrations in tissues in patients or animals can be accurately quantified by SPECT provided that the limitations are addressed [41, 42]. Encouragingly, we found strong correlations between ROI-SUR and SUR values (r = 0.92, P = 0.03; Fig. 5a) and between ROI-LI and LI values (r = 0.97, P = 0.006; Fig. 5b), indicating that reliable estimates of 111In concentrations, at least in small animal tumour xenograft models are possible. Nonetheless, the sensitivity of detection of HER2-positive tumours as well as accurate quantification of tumour and normal tissue concentrations of radiolabeled trastuzumab would be substantially improved by PET. A recent study reported visualization of HER2-positive tumours using trastuzumab labeled with the positron-emitter, 89Zr [18].
Conclusion
We conclude that imaging with 111In-DTPA-trastuzumab may be valuable for assessing relative HER2 expression in lesions (i.e., 0 to 3+) in BC patients, provided that appropriate corrections are applied for nonspecific IgG tumour localization as well as circulating radioactivity. The uncorrected tumour uptake of the radiopharmaceutical was associated with response to treatment with trastuzumab (Herceptin) in the limited panel of tumour xenografts examined, but it is important to recognize that compensatory trastuzumab-resistance mechanisms (e.g., IGF-1R overexpression) can cause discordance between HER2 density, tumour uptake of 111In-DTPA-trastuzumab on the images, and response to the drug. Evaluation of a larger panel of tumour xenografts expressing 0 to 3+ HER2 density is warranted to fully understand these relationships.
References
Vogel CL, Cobleigh MA, Tripathy D, Gutheil JC, Harris LN, Fehrenbacher L, et al. Efficacy and safety of trastuzumab as a single agent in first-line treatment of HER2-overexpressing metastatic breast cancer. J Clin Oncol. 2002;20:719–26.
Slamon DJ, Leyland-Jones B, Shak S, Fuchs H, Paton V, Bajamonde A, et al. Use of chemotherapy plus a monoclonal antibody against HER2 for metastatic breast cancer that overexpresses HER2. N Engl J Med. 2001;344:783–92.
Plosker GL, Keam SJ. Trastuzumab: a review of its use in the management of HER2-positive metastatic and early-stage breast cancer. Drugs. 2006;66:449–75.
Wolff AC, Hammond EH, Schwartz JN, Hagerty KL, Allred DC, Cote RJ, et al. American society of clinical oncology/college of American pathologist guideline recommendations for human epidermal growth factor receptor 2 testing in breast cancer. J Clin Oncol. 2007;25:118–45.
Vogel C. Trastuzumab monotherapy. Breast Cancer Res Treat. 2003;81 Suppl 1:S67–8.
Marty M, Cognetti F, Maraninchi D, Snyder R, Mauriac L, Tubiana-Hulin M, et al. Randomized phase II trial of the efficacy and safety of trastuzumab combined with docetaxel in patients with human epidermal growth factor receptor 2-positive metastatic breast cancer administered as first-line treatment: the M77001 study group. J Clin Oncol. 2005;23:4265–74.
McLarty K, Reilly RM. Molecular imaging as a tool for targeted and personalized cancer therapy. Clin Pharmacol Ther. 2007;81:420–4.
Behr TM, Béhé M, Wörmann B. Trastuzumab and breast cancer. N Engl J Med. 2001;345:995–6.
Tang Y, Wang J, Scollard DA, Mondal H, Holloway C, Kahn HJ, et al. Imaging of HER2/neu-positive BT-474 human breast cancer xenografts in athymic mice using 111In-trastuzumab (Herceptin) Fab fragments. Nucl Med Biol. 2005;32:51–8.
Garmestani K, Milenic DE, Plascjak PS, Brechbiel MW. A new and convenient method for purification of 86Y using a Sr(II) selective resin and comparison of biodistribution of 86Y and 111In labeled Herceptin. Nucl Med Biol. 2002;29:599–606.
Tang Y, Scollard D, Chen P, Wang J, Holloway C, Reilly RM. Imaging of HER2/neu expression in BT-474 human breast cancer xenografts in athymic mice using 99mTc-HYNIC-trastuzumab (Herceptin) Fab fragments. Nucl Med Commun. 2005;26:427–32.
Orlova A, Rosik D, Sandström M, Lundqvist H, Einarsson L, Tolmachev V. Evaluation of [111/114mIn]CHX-A″-DTPA-ZHER2:342, an Affibody ligand conjugate for targeting of HER2-expressing malignant tumours. Q J Nucl Med Mol Imaging. 2007;51:314–23.
Smith-Jones PM, Solit DB, Akhurst T, Afroze F, Rosen N, Larson SM. Imaging the pharmacodynamics of HER2 degradation in response to Hsp90 inhibitors. Nat Biotechnol. 2004;22:701–6.
Niu G, Cai W, Chen X. Molecular imaging of human epidermal growth factor receptor 2 (HER-2) expression. Front Biosci. 2008;13:790–805.
Lub-de Hooge MN, Kosterink JG, Perik PJ, Nijnuis H, Tran L, Bart J, et al. Preclinical characterisation of 111In-DTPA-trastuzumab. Br J Pharmacol. 2004;143:99–106.
Robinson MK, Doss M, Shaller C, Narayanan D, Marks JD, Adler LP, et al. Quantitative immuno-positron emission tomography imaging of HER2-positive tumor xenografts with an iodine-124 labeled anti-HER2 diabody. Cancer Res. 2005;65:1471–8.
Olafsen T, Tan GJ, Cheung CW, Yazaki PJ, Park JM, Shively JE, et al. Characterization of engineered anti-p185HER-2 (scFv-CH3)2 antibody fragments (minibodies) for tumor targeting. Protein Eng Des Sel. 2004;17:315–23.
Dijkers E, Lub-de Hooge MN, Kosterink JG, Jager PL, Brouwers AH, Perk LR, et al. Characterization of 89Zr-trastuzumab for clinical HER2 immunoPET imaging [abstract 3508]. J Clin Oncol. 2007;25:18S.
Perik PJ, Lub-De Hooge MN, Gietema JA, van der Graaf WT, de Korte MA, Jonkman S, et al. Indium-111-labeled trastuzumab scintigraphy in patients with human epidermal growth factor receptor 2-positive metastatic breast cancer. J Clin Oncol. 2006;24:2276–82.
Benz CC, Scott GK, Sarup JC, Johnson RM, Tripathy D, Coronado E, et al. Estrogen-dependent, tamoxifen-resistant tumorigenic growth of MCF-7 cells transfected with HER2/neu. Breast Cancer Res Treat. 1992;24:85–95.
Cornelissen B, Hu M, McLarty K, Costantini D, Reilly RM. Cellular penetration and nuclear importation properties of 111In-labeled and 123I-labeled HIV-1 tat peptide immunoconjugates in BT-474 human breast cancer cells. Nucl Med Biol. 2007;34:37–46.
Lindmo T, Boven E, Cuttitta F, Fedorko J, Bunn PA Jr. Determination of the immunoreactive fraction of radiolabeled monoclonal antibodies by linear extrapolation to binding at infinite antigen excess. J Immunol Methods. 1984;72:77–89.
Leonard DS, Hill AD, Kelly L, Dijkstra B, McDermott E, O’Higgins NJ. Anti-human epidermal growth factor receptor 2 monoclonal antibody therapy for breast cancer. Br J Surg. 2002;89:262–71.
Horton J. Her2 and trastuzumab in breast cancer. Cancer Control. 2001;8:103–10.
Ross JS, Fletcher JA, Bloom KJ, Linette GP, Stec J, Symmans WF, et al. Targeted therapy in breast cancer: the HER-2/neu gene and protein. Mol Cell Proteomics. 2004;3:379–98.
Hanna W, O’Malley FP. Updated recommendations from the HER2/neu consensus meeting - Toronto, Ontario, September 2001. Current Oncology. 2002;9 Suppl. 1:S18–9.
Kauraniemi P, Kallioniemi A. Activation of multiple cancer-associated genes at the ERBB2 amplicon in breast cancer. Endocr Relat Cancer. 2006;13:39–49.
Cai W, Chen K, He L, Cao Q, Koong A, Chen X. Quantitative PET of EGFR expression in xenograft-bearing mice using 64Cu-labeled cetuximab, a chimeric anti-EGFR monoclonal antibody. Eur J Nucl Med Mol Imaging. 2007;34:850–8.
Jain RK. Physiological barriers to delivery of monoclonal antibodies and other macromolecules in tumors. Cancer Res. 1990;50 Suppl. 3:814–9.
de Korte MA, de Vries EG, Lub-de Hooge MN, Jager PL, Gietema JA, van der Graaf WT, et al. 111Indium-trastuzumab visualises myocardial human epidermal growth factor receptor 2 expression shortly after anthracycline treatment but not during heart failure: a clue to uncover the mechanisms of trastuzumab-related cardiotoxicity. Eur J Cancer. 2007;43:2046–51.
Wong DW, Eisenman JI, Wade W Jr. Detection of acute infection/inflammation with Tc-99m labeled intact polyvalent human IgG. Nucl Med Biol. 1995;22:513–9.
Nijhof MW, Oyen WJ, van Kampen A, Claessens RA, Meer JW, Corstens FH. Evaluation of infections of the locomotor system with indium-111 labeled human IgG scintigraphy. J Nucl Med. 1997;38:1300–5.
Hine KR, Bradwell AR, Reeder TA, Drolc Z, Dykes PW. Radioimmunodetection of gastrointestinal neoplasms with antibodies to carcinoembryonic antigen. Cancer Res. 1980;40:2993–6.
Goldenberg DM, Kim EE, DeLand FH, Bennett S, Primus FJ. Radioimmunodetection of cancer with radioactive antibodies to carcinoembryonic antigen. Cancer Res. 1980;40:2984–92.
Jerome L, Alami N, Belanger S, Page V, Yu Q, Paterson J, et al. Recombinant human insulin-like growth factor binding protein 3 inhibits growth of human epidermal growth factor receptor-2-overexpressing breast tumors and potentiates herceptin activity in vivo. Cancer Res. 2006;66:7245–52.
Lu Y, Zi X, Zhao Y, Mascarenhas D, Pollak M. Insulin-like growth factor-I receptor signaling and resistance to trastuzumab (Herceptin). J Natl Cancer Inst. 2001;93:1852–7.
Harris LN, You F, Schnitt SJ, Witkiewicz A, Lu X, Sgroi D, et al. Predictors of resistance to preoperative trastuzumab and vinorelbine for HER2-positive early breast cancer. Clin Cancer Res. 2007;13:1198–207.
Cornelissen B, McLarty K, Kersemans V, Reilly RM. The level of insulin growth factor-1 receptor expression is directly correlated with the tumor uptake of 111In-IGF-1(E3R) in vivo and the clonogenic survival of breast cancer cells exposed in vitro to trastuzumab (Herceptin). Nucl Med Biol 2008;35:645–53.
King M, Farncombe T. An overview of attenuation and scatter correction of planar and SPECT data for dosimetry studies. Cancer Biother Radiopharm. 2003;18:181–90.
Bailey DL, Parker JA. Single-photon emission computed tomography. In: Ell PJ, Gambhir SS, editors. Nuclear medicine in clinical diagnosis and treatment, vol. 2. 3rd ed. Amsterdam: Elsevier Limited; 2004; p. 1815–1826.
Kanwar B, Gao DW, Hwang AB, Grenert JP, Williams SP, Franc B, et al. In vivo imaging of mucosal CD4+ T cells using single photon emission computed tomography in a murine model of colitis. J Immunol Methods. 2008;329:21–30.
Wiseman GA, White CA, Stabin M, Dunn WL, Erwin W, Dahlbom M, et al. Phase I/II 90Y-Zevalin (yttrium-90 ibritumomab tiuxetan, IDEC-Y2B8) radioimmunotherapy dosimetry results in relapsed or refractory non-Hodgkin’s lymphoma. Eur J Nucl Med. 2000;27:766–77.
Acknowledgments
This research was supported by grants from the Ontario Cancer Research Network (No. 03-NOV-0428) with funds from the Province of Ontario. K.M. is the recipient of the MDS Nordion Graduate and an Ontario Graduate Scholarship and is a Canadian Institutes of Health Research Strategic Training Fellow in the Excellence in Radiation Research for the 21st Century (EIRR21) Program. Parts of this research were presented at the Canadian Breast Cancer Research Alliance Reasons for Hope Conference, Montreal, PQ, May 6–8, 2006. The authors are grateful to Dr. Pieter Jager, McMaster University, for his review of the manuscript and helpful comments.
Conflict of Interest Statement
The authors have no known conflict of interest with submission of this manuscript for publication. Dr. Raymond Reilly has a Materials Transfer Agreement with Genentech, Inc. for a separate project. All sources of support relating to these studies have been acknowledged.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
McLarty, K., Cornelissen, B., Scollard, D.A. et al. Associations between the uptake of 111In-DTPA-trastuzumab, HER2 density and response to trastuzumab (Herceptin) in athymic mice bearing subcutaneous human tumour xenografts. Eur J Nucl Med Mol Imaging 36, 81–93 (2009). https://doi.org/10.1007/s00259-008-0923-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00259-008-0923-x