Abstract
Introduction
The purpose of the EANM Dosimetry Committee Series on “Standard Operational Procedures for Pre-therapeutic Dosimetry” (SOP) is to provide advice to scientists and clinicians on how to perform pre-therapeutic and/or therapeutic patient-specific absorbed dose assessments.
Material and Methods
This particular SOP gives advice on how to tailor the therapeutic activity to be administered for systemic treatment of differentiated thyroid cancer (DTC) such that the absorbed dose to the blood does not exceed 2 Gy (a widely accepted limit for bone marrow toxicity). The methodology of blood-based dosimetry has been developed in the 1960s and refined in a series of international multi-centre trials in the framework of the introduction of new diagnostic and therapeutic tools, e.g. recombinant human thyroid-stimulating hormone in the management of DTC.
Conclusion
The intention is to guide the user through a series of measurements and calculations which the authors consider to be the best and most reproducible way at present.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The purpose of this EANM Dosimetry Committee Series on “Standard Operational Procedures for Pre-therapeutic Dosimetry” (SOP) is to provide recommendations to scientists and clinicians on how to perform pre-therapeutic and/or peri-therapeutic patient-specific absorbed dose assessments.
The intention is to guide the user through a series of measurements and calculations which the authors consider to be the best and most reproducible way at the moment. There might be different procedures that also lead to the same or similar results.
This paper is the first in a series of disease- and patient-specific “how to” procedures intended to summarise the methodology for assessing absorbed dose in targeted radionuclide therapy. The aim of the paper is to provide supplementary and comprehensive information to the corresponding medically oriented disease-specific guidelines provided by the “Therapy Committee” of the EANM.
This SOP gives recommendations on how to tailor the therapeutic activity to be administered for the systemic treatment of differentiated thyroid cancer (DTC) such that the absorbed dose to the blood does not exceed 2 Gy (a widely accepted limit for bone marrow toxicity) and, at 48 h after administration, the whole-body retention does not exceed 4.4 or 3 GBq in the absence or presence of iodine-avid diffuse lung metastases, respectively [1, 2]. For the blood absorbed dose estimate procedure, low activities of 131I NaI will be administered pre-therapeutically followed by a series of blood and whole-body measurements.
The use of 123I NaI for this specific pre-therapeutic procedure might be possible. However, there are no published data on the advantages/disadvantages when using this isotope for blood and bone marrow absorbed dose assessments.
The methodology of blood-based dosimetry has been developed and refined in a series of international multi-centre trials in the framework of the introduction of new diagnostic and therapeutic tools, e.g. recombinant human thyroid-stimulating hormone in the management of DTC [3, 4].
Motivation
Radioiodine therapy is used in common practice for the treatment of DTC to ablate remnant thyroid tissue after surgery and to treat iodine-avid metastases. An overview of the treatment procedures, benefits and risks related to DTC treatment with radioiodine can be found in the textbook by Schlumberger and Pacini [5]. Guidance on how patients with DTC should be treated and on general patient management issues are compiled in a new version of the EANM guidelines on the treatment of thyroid cancer (Luster et al. 2008, in preparation).
One of the possible concepts for treating advanced stages of thyroid cancer is based on the individual calculation of the activity to be administered delivering an absorbed dose to the blood of 2 Gy. The rationale for using a dosimetry-based approach is to replace the conventional fixed activity regime by a modern setting which allows the administered therapeutic activity to be increased avoiding undesired side effects. Using this strategy, the absorbed dose to iodine-avid tissue (remnants/metastases) can be optimised without inducing toxicity, which is in contrast to a fixed activity approach which can induce peripheral blood changes and long-term consequences (e.g. haematological disorders) [6, 7].
Blood, as a surrogate of the organ at risk, i.e. the red bone marrow, was considered as the critical organ in the approach originally reported by Benua and Leeper [1, 2]. The blood is irradiated either from the β particles emitted from activity in the blood itself or from penetrating γ radiation originating from activity dispersed throughout the remainder of the body. In the original work of Benua et al. [1], no serious haematological side effects were observed in the sub-group of patients that received 2 Gy or less to the blood. The maximum treatment activity, therefore, is calculated as the amount of 131I that would deliver an absorbed dose of 2 Gy to the blood compartment. A summary of the methodologies used until 2003 can be found in the review article by van Nostrand [8].
There is some evidence that the distribution volume of 131I as calculated from blood activity measurements is about 20 to 30 l with almost identical concentrations in blood and inner organs [9], and the radioiodine concentration is similar in blood and in red marrow [10]. The blood absorbed dose assessment, therefore, allows an estimate for the radiation absorbed dose that will be delivered to the haematopoietic system of the individual patient during the therapy.
For the application of the blood-based method, only two compartments need to be monitored for radioactivity: blood and whole body. Five blood samples are recommended to determine radioiodine kinetics in the blood over time. The activity in the whole body should be monitored by conjugate views of whole-body imaging with a dual-headed gamma camera or by conjugate whole-body counting with a probe using a fixed geometry. Details of the sampling frequency of the data and of the calculation process can be found in the “Standard operational procedures” section of this guideline.
The strengths of the blood-based approach are:
-
determination of the maximal safe activity of radioiodine for each patient individually;
-
identification of patients for whom empiric fixed activities are not safe [11];
-
the potential to administer higher activities once instead of multiple administrations of lower activities in a “fractionated” therapy to avoid changes in tumour/lesion biokinetics after multiple therapies that have been observed, e.g. by Samuel et al. [12];
-
a long history of use in several institutions [2];
-
an expected increase in the probability of curing patients in an advanced stages of the disease with fewer courses of therapy.
Limitations that need to be mentioned are:
-
a benefit of the strategy is plausible but no valid clinical data exist on improved response and/or outcome rates;
-
the absorbed dose to the tumour is not known. Higher activities might be administered without achieving a higher therapeutic effect when using this methodology;
-
the current debate regarding the issue of ‘stunning’ argues that diagnostic administrations of 131I could alter tumour/lesion biokinetics and, consequently, the absorbed dose in a subsequent treatment [13, 14];
-
increased cost and inconvenience, although this may be outweighed by rendering further treatments unnecessary.
Patient-specific blood-based dosimetry is easy to perform both pre-therapeutically and peri-therapeutically and allows the therapeutic activity for selected patients to be increased without risk of severe side effects.
The presented model might not to be applied in the presence of extended metastatic bone involvement, as the blood-based absorbed dose calculation could underestimate the absorbed dose to the red marrow.
It should be carefully applied in patients affected by diffuse lung micro-metastases because the critical organ could be the lung itself instead of the haematopoietic red marrow. In this case, the criteria set by Sgouros et al. [15] or Song et al. [16] should be considered before therapy.
Standard operational procedures
Timelines
The suggested timelines can be found in Table 1.
In the case of oral administration, the patient must endure the time until finalisation of the 2-h task without micturition. Therefore, the patient’s urinary bladder should be emptied immediately before the tracer activity is administered. The whole-body activity measurement at nominal 2 h (10 min in the case of intravenous administration) is intended to be the baseline quantification with 100% of the administered activity and must be performed before any activity excretion. The nominal 2-h whole-body activity measurement should be initiated earlier if the patient is unable to wait for 2 h. In case of intravenous administration, the first scan or probe count and the first blood sample must be collected within 10 min of the injection time.
Micturition is mandatory before all subsequent whole-body measurements (6, 24 and 96 h). It should be assured that the patients have one to two bowel movements a day during the diagnostic investigation and therapy to reduce artefacts due to 131I retained in the intestine and colon.
Dates and times of administration, blood sampling and activity measurements should be documented.
Preparation of 131I standard and tracer activity
The assay instrumentation (e.g. dose calibrator) used to quantify the tracer activity must be accurately calibrated for 131I and quality checked according to acknowledged quality control procedures.
The tracer activity necessary for a reliable assessment of the whole-body residence time depends on the equipment used (see the “Pre-therapeutic quantification of whole-body retention” section). Also, the potential risk of dramatically changing the iodine kinetics in target tissue induced by diagnostic procedures should be considered. Such a change has been observed after the diagnostic administration of only 74 MBq 131I NaI [14]. An analysis of the published dosimetry data shows that no changes are to be expected if the absorbed dose to iodine-avid tissue is kept below approximately 5 Gy [13]. An absorbed dose of 5 Gy to normal thyroid tissue is imparted for euthyroid persons after the administration of 15 MBq 131I NaI under the assumption of a typical thyroid tissue uptake of 1.5%/g [17].
It is good practice to prepare a radioiodine source to be used as a standard for quality control. If whole-body activity is measured with a gamma camera, the source should be scanned either separately or together with the patient; the standard activity should be about 5% of the tracer activity. The standard must be measured separately and its activity might need to be higher if a probe is used for whole-body activity determination.
The exact dose calibrator readings for standard and tracer activities must be recorded before the administration. In the case of administration of liquid 131I NaI, the residual activity must be quantified as well to determine the activity administered. The dose calibrator accuracy must be tested by a certified source and documented as part of the quality assurance procedures.
Pre-therapeutic quantification of whole-body retention
A dual-headed gamma camera with high-energy collimators and crystal thickness of 5/8 in. or more is recommended for the whole-body activity measurements (see the “Whole-body scan conjugate-view imaging” section). However, a spectroscopic probe with a large crystal might be used as well (see the “Probe measurements” section).
As whole-body activity typically contributes only 20–25% to the blood absorbed dose and later time points (assessments) usually suffer from high inaccuracy, whole-body measurements up to 96 h post-administration will be sufficient for most of the patients. However, an additional measurement after 144 h should be considered if the uncorrected whole-body retention after 96 h exceeds 5%.
Whole-body scan conjugate-view imaging
The activity in the whole body should be deduced from whole-body scan data, preferably by a dual-headed gamma camera. The case of intravenous administration, the first scan should be started within 10 min from the injection. Both camera heads must be equipped with high-energy collimators.
Tracer activity and scan duration should be chosen taking into account the camera detection efficiency. The geometric mean of the anterior and posterior net counts of the activity to administer should exceed 105 with the selected scan speed. A camera with crystal thickness of at least 5/8 in. gives the better conditions because of its increased efficiency for detecting 360 keV photons. With such a camera, (a) the net count rate (detection efficiency) of a non-attenuated point source should exceed 50 counts per second (cps) per MBq of 131I and (b) the net count rate per MBq of 131I in the field of view should be at least twice as high as the overall background count rate in the 131I energy window. An activity as low as 10–15 MBq 131I NaI will provide sufficient count statistics.
Established scintillation camera quality control procedures should be performed before the first imaging of the patient to prove that the camera meets common quality standards.
No other patients or active sources nearby should be allowed to affect the measured count rates. The normal background counts per pixel for the chosen settings should be measured at least once in a background scan with the patient being absent and no active source nearby.
The verification of a normal background count rate in the 131I energy window before each whole-body scan of the patient might be performed by a static 1 min acquisition; however, it is recommended to re-run the background scan before each patient scan.
For the scintigram, position the patient supine on the table with arms down by the side and the head at the upper border of the field of view. Take care that the patient lies comfortable and entirely (bottom to top and side to side) within the field of view. Note should be made of the positioning so that reproducible patient positions are achieved/assured for each whole-body scan (essential to ease region drawing on later scans with low count rates).
After the patient is comfortably positioned with feet together, position the standard source at the lower end of the field of view. Take care that the source is entirely within the field of view and as far apart from the patient’s legs as possible. Alternatively, the standard can be scanned separately using the same camera settings. This could facilitate the deduction of the activity.
Auto-contouring should be deactivated if the camera system features this option. The upper (anterior) and lower (posterior) scintillation camera heads should be positioned at a minimum distance from the patient and table, respectively. It should be ensured that for the upper head, the separation is appropriate for the full length of the whole-body scan with a minimal distance approach without touching the patient at any point. Using variable distances might not change the overall sensitivity of the system; it might, however; introduce unwanted errors by the variable spatial resolution of the system.
It is preferable to use the same camera, collimators and camera settings for all scans of the same patient. A valid cross-calibration of the systems must be assured if different systems are used.
Probe measurements
A spectroscopic probe, e.g. a sodium iodide detector with a crystal of at least 3 × 3 in. should be used. Choose a distance between probe and patient of 2 m or more for the count rate to be insensitive to small distance variations and redistribution of the radioiodine within the patient’s body. A partial shielding to reduce background is recommended. However, the aperture must allow a non-shielded view of the entire patient.
Allow adequate measuring times to achieve reliable results. For a partially shielded 3 × 3 in. NaI detector, for example, typical background count rate in a 15% energy window at 364 keV is about 5 cps and detection efficiency for a point source at a 2-m distance is about 50 cps/MBq of 131I. Tracer activity and count duration should be chosen depending on the detection efficiency. The net counts of the activity to be administered should exceed 105 for the selected acquisition duration to assure sufficient count statistics at the later time points.
Conjugate view (anterior and posterior) count rate measurements are strongly recommended to reduce sensitivity to activity redistribution within the patient.
All measurements attributed to an individual patient should be performed with the same probe at a well-defined location featuring low background radiation level. No other patients or active sources nearby should be able to affect the measured count rates. Verification of a normal background count rate before each patient measurement with the patient being absent is mandatory. Allow for adequate measuring times to achieve good counting statistics in the background count (counting time not shorter than in the patient acquisition) if background correction of the patient’s measurement is not performed by a spectroscopic peak fitting technique but simply by subtraction of the measured background count rate.
An exactly reproducible measuring geometry is essential for achieving a reliable activity–time curve of the whole-body 131I retention. The longitudinal position of the probe should be at the height of the tip of the sternum during the measurement. A setup with the patient lying under a detector fixed to the ceiling is preferable, although not all patients tolerate several minutes of lying in a prone position [18]. A horizontal spacer should be used to ensure a fixed and reproducible measuring distance if the patients are measured in an upright position (standing).
Blood sampling
Blood sampling should be performed for 1 week after the administration. In radioiodine therapy for DTC, the absorbed dose to the blood is mainly caused by beta radiation originating from activity in the blood. Usually, about 75–80% of the radiation absorbed dose deposited must be attributed to this contribution. Late blood sampling is required to reduce the potential risk of underestimating the blood absorbed dose in the presence of an unrecognised long-lived component in iodine kinetics.
The activity in the blood is determined in a well counter from aliquots of heparinised blood samples.
Whole blood samples (about 2 ml) are collected at 2, 6, 24, 96 and 144 h post-administration.
In the case of oral administration, wait for 2 h post-administration to take the first blood sample even if the initial whole-body measurement had to be shifted to earlier times because the patient was unable to wait for the 2-h time point without micturition.
In the case of intravenous administration, the first sample must be drawn within 10 min from the contralateral arm.
All blood samples should be stored until the last sample has been collected.
Data extraction
Whole-body retention
If a scintillation camera was utilised to measure whole-body activities, draw regions of interest (ROI) around the patient’s whole body (adjacent to whole-body contour, unaffected by the activity in the standard) and the standard activity in the 2-h anterior scan image and reflect them to the posterior image. Draw ROIs also on the background images. Copy the ROI from the first images to the corresponding images of the latter scans and check that patient and standard are well within their regions in each image. Use the corresponding background scan to determine the mean background counts per pixel (BKGcts/pix). Extract whole-body counts (WBcts), the number of pixels (WBpix) in the whole-body ROI and calculate the whole-body net counts (WBnet) by background subtraction according to: \({\text{WB}}_{{\text{net}}} \;{\text{ = }}\;{\text{WB}}_{{\text{cts}}} \; - \;{\text{WB}}_{{\text{pix}}} \; \times \;{\text{BKG}}_{{{{\text{cts}}} \mathord{\left/ {\vphantom {{{\text{cts}}} {{\text{pix}}}}} \right. \kern-\nulldelimiterspace} {{\text{pix}}}}} \).
If a probe was used, WBnet is the background corrected signal count rate.
For all further calculations, the geometric mean of corresponding net counts for conjugate views \(\sqrt {{\text{WB}}_{{\text{net anterior}}} \times {\text{WB}}_{{\text{net posterior}}} } \) will be used:
All geometric mean counts are normalised to the first data point (first data point is 100%) to calculate the activity as a function of time (R(t)) for the whole body.
Blood retention
Aliquots of 1 ml should be prepared from each blood sample. The pipette tip should be left in the test sample whenever a blood aliquot is prepared. The detection limit of the well counter used should be lower than 1 Bq of 131I per ml. The counter must be accurately calibrated for 131I.
We recommend performing all well counter measurements including a background count with no activity consecutively in a single contiguous session. Allow adequate measuring times to achieve good counting statistics. A statistical error of <5% can be achieved under typical conditions.
Correct the raw counts per minute of each aliquot for the background counts per minute and deduce the corresponding activity concentration values from the well counter calibration factor for 131I. Correct each result for physical decay between corresponding time points of blood sampling and measurement to determine the blood activity at the sampling time.
All blood activities are normalised to the administered activity to calculate the retention per millilitre of blood.
Absorbed dose calculation
Residence times
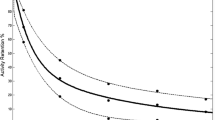
The curves describing the activity in blood and total body as a function of time after the administration usually are multi-exponential. Most of the activity is rapidly excreted with an effective half-life of typically half a day, but smaller fractions are retained in accumulating tissues (remnant, tumour and gastrointestinal tract). Unless the slowly excreted component is negligible, bi-exponential fitting is adequate to determine the function describing the activity as a function of time for whole body and blood.
where R(t) is the fraction of the administered activity A 0 as a function of time t and A 1, A 2, λ 1 and λ 2 are the fit constants.
An objective criterion for the goodness of the fit such as the minimisation of χ 2 should be used.
The residence times for the whole body and activity concentration in blood, τ total body [h] and τ millilitre of blood [h], are calculated by integrating the respective retention functions \({\text{R}}\left( t \right){\text{ }} = {\text{ }}{{A\left( t \right)} \mathord{\left/ {\vphantom {{A\left( t \right)} {A_0 }}} \right. } {A_0 }}\) from zero to infinity:
With the time lines suggested above, underestimation of the residence times due to unrecognised compartments is expected to induce <10% uncertainty in the determined blood absorbed dose [4]. However, the appearance of an additional component with long half-life after the activity assessments cannot be excluded. It is recommended to estimate upper limits for both residence times (τ LIMIT) by integrating the corresponding retention functions R(t) from zero to the last data point taken at time T and adding the integral from the last data point to infinity using physical decay only (λ phys = 0.0036 h−1):
As half-lives exceeding 6 days are seldom observed in thyroid cancer patients, the sampling can be considered to be sufficient, i.e. an overall 10% uncertainty of the residence time calculation will be achieved if the calculated upper limits exceed τ millilitre of blood and τ total body by <15% and 30%, respectively.
Blood absorbed dose calculation
According to the generally accepted MIRD formalism, the mean absorbed dose to the blood \(\left( {\overline D _{{\text{blood}}} } \right)\) per unit administered activity (A 0) is determined by the sum of contributions of blood self-irradiation and penetrating radiation from the whole body:
To estimate the first term, Benua et al. [1, 2] neglected the gamma component and assumed beta radiation absorption of 187 keV per decay corresponding to an absorbed dose of 3 × 10−11 Gy·ml/(Bq·s) = 108 Gy·ml/(GBq·h). The value is in reasonable agreement with Monte Carlo simulation of blood self-irradiation [19].
The S value for penetrating radiation from the whole body was approximated by \(S_{{\text{blood}} \leftarrow \gamma \;{\text{total body}}} \; \approx S_{{\text{total body}} \leftarrow \gamma \;{\text{total body}}} \) (note that only the γ contribution is considered here) and calculated according to a method described in [19] to be \(S_{{\text{blood}} \leftarrow \gamma \;{\text{total body}}} \; = \;{{0.00589 \times \overline g } \mathord{\left/ {\vphantom {{0.00589 \times \overline g } {{{{\text{wt}}\;{\text{Gy}}} \mathord{\left/ {\vphantom {{{\text{wt}}\;{\text{Gy}}} {\left( {{\text{GBq}}\,{\text{h}}} \right)}}} \right. \kern-\nulldelimiterspace} {\left( {{\text{GBq}}\,{\text{h}}} \right)}}}}} \right. \kern-\nulldelimiterspace} {{{{\text{wt}}\;{\text{Gy}}} \mathord{\left/ {\vphantom {{{\text{wt}}\;{\text{Gy}}} {\left( {{\text{GBq}}\,{\text{h}}} \right)}}} \right. \kern-\nulldelimiterspace} {\left( {{\text{GBq}}\,{\text{h}}} \right)}}}}\) where wt represents the patient’s weight in kg and \(\overline g \) is a geometrical factor (tabulated in [20]) dependent on the weight and height of the patient. The S value may be replaced by a term independent of \(\overline g \) based on the Monte Carlo simulation [21]:\(S_{{\text{blood}} \leftarrow \gamma \;{\text{total body}}} \; = \;0.0188 \times {{{\text{wt}}^{{\raise0.7ex\hbox{${ - 2}$} \!\mathord{\left/ {\vphantom {{ - 2} 3}}\right.\kern-\nulldelimiterspace}\!\lower0.7ex\hbox{$3$}}} \,{\text{Gy}}} \mathord{\left/ {\vphantom {{{\text{wt}}^{{\raise0.7ex\hbox{${ - 2}$} \!\mathord{\left/ {\vphantom {{ - 2} 3}}\right.\kern-\nulldelimiterspace}\!\lower0.7ex\hbox{$3$}}} \,{\text{Gy}}} {\left( {{\text{GBq h}}} \right)}}} \right. \kern-\nulldelimiterspace} {\left( {{\text{GBq h}}} \right)}}\). Both terms provide identical results for almost every patient within an error margin of 5%; blood absorbed dose is changed by <2%.
The mean blood absorbed dose per unit administered tracer activity can be calculated by:
The activity to be administered for a blood absorbed dose of 2 Gy is:
Red marrow absorbed dose calculation
The historical use of the blood absorbed dose model and related toxicity were investigated and validated in the early clinical studies by Benua et al. [1], and they were safely employed for more than three decades [2, 11, 22]. The scientific development leading to the Sgouros’ blood model for red marrow absorbed dose calculation in the case of labelled monoclonal antibodies for radioimmunotherapy is based on the hypothesis that the activity is transported within the red marrow by the plasma [23]. It is of importance to unify the methodology of dosimetry of the most critical organ (i.e. the red marrow) to proceed towards a standardisation of the different dosimetric methods. Unfortunately, the Sgouros’ model cannot be simply translated to radioiodine therapy because the initial distribution volume of the iodine ion is much larger than that of monoclonal antibodies [9, 10].
However, under the conservative assumption that the activity concentrations within the haematopoietic tissue and the blood are identical in radioiodine treatments [10], a red marrow-based approach for the determination of the maximum activity to be administered has been proposed [24].
The data collection for this method follows exactly the ones described in the previous sections. The only difference is that Eq. 5 is replaced by the following expression for the red marrow absorbed dose per unit activity:
where the S value is linearly scaled to the patient’s whole-body weight.
According to this equation, the red marrow absorbed dose is less than the blood absorbed dose (generally from −10% to −30%) for fixed τ millilitre of blood and τ total body.
The most recently published paper for red marrow absorbed dose calculation [25] employs non-linear scaling of the S values to the individual patient’s weight. According to this more accurate and complex model, the red marrow absorbed dose is even lower (for fixed τ millilitre of blood and τ total body). However, no systematic clinical validation of the red marrow absorbed dose vs. toxic effect has yet been undertaken for radioiodine treatments.
Recommendation for the absorbed dose calculation
At present, we recommend that the maximum administered activity should be computed using Eq. 5 (i.e. the blood absorbed dose) for the sake of caution. Nevertheless, in view of standardisation, both the blood and the red marrow absorbed doses should be reported in future publications. This will allow a better comparison between studies using different therapeutic approaches and/or radiopharmaceuticals.
References
Benua RS, Cicale NR, Sonenberg M, Rawson RW. Relation of radioiodine dosimetry to results and complications in treatment of metastatic thyroid cancer. Am J Roentgenol Radium Ther Nucl Med 1962;87:171–82.
Benua RS, Leeper RD. A method and rationale for treating metastatic thyroid carcinoma with the largest safe dose of I-131. Frontiers in thyroidology, vol 2. New York: Plenum Medical; 1986. p. 1317–21.
Luster M, Sherman SI, Skarulis MC, Reynolds JR, Lassmann M, Hänscheid H, et al. Comparison of radioiodine biokinetics following the administration of recombinant human thyroid stimulating hormone and after thyroid hormone withdrawal in thyroid carcinoma. Eur J Nucl Med Mol Imaging 2003;30:1371–7.
Hänscheid H, Lassmann M, Luster M, Thomas SR, Pacini F, Ceccarelli C, et al. Iodine biokinetics and dosimetry in radioiodine therapy of thyroid cancer: procedures and results of a prospective international controlled study of ablation after rhTSH or hormone withdrawal. J Nucl Med 2006;47:648–54.
Schlumberger M, Pacini F. Thyroid tumors. 5th ed. Paris: Editions Nucléon; 2003.
Schober O, Gunter HH, Schwarzrock R, Hundeshagen H. Long-term hematologic changes caused by radioiodine treatment of thyroid cancer I. Peripheral blood changes. Strahlenther Onkol 1987;163:464–74.
Gunter HH, Schober O, Schwarzrock R, Hundeshagen H. Long-term hematologic changes caused by radioiodine treatment of thyroid cancer. II. Bone marrow changes including leukemia. Strahlenther Onkol 1987;163:475–85.
Van Nostrand D, Atkins F, Yeganeh F, Acio E, Bursaw R, Wartofsky L. Dosimetrically determined doses of radioiodine for the treatment of metastatic thyroid carcinoma. Thyroid. 2002;12:121–14.
Kolbert KS, Pentlow KS, Pearson JR, Sheikh A, Finn RD, Humm JL, et al. Prediction of absorbed dose to normal organs in thyroid cancer patients treated with 131I by use of 124I PET and 3-dimensional internal dosimetry software. J Nucl Med 2007;48:143–9.
Sgouros G. Blood and bone marrow dosimetry in radioiodine therapy of thyroid cancer. J Nucl Med 2005;46:899–900.
Tuttle RM, Leboeuf R, Robbins RJ, Qualey R, Pentlow K, Larson SM, et al. Empiric radioactive iodine dosing regimens frequently exceed maximum tolerated activity levels in elderly patients with thyroid cancer. J Nucl Med 2006;47:1587–91.
Samuel AM, Rajashekharrao B, Shah DH. Pulmonary metastases in children and adolescents with well-differentiated thyroid cancer. J Nucl Med 1998;39:1531–6.
Medvedec M. Thyroid stunning in vivo and in vitro. Nucl Med Commun 2005;26:731–5.
Lassmann M, Luster M, Hänscheid H, Reiners C. Impact of 131I diagnostic activities on the biokinetics of thyroid remnants. J Nucl Med 2004;4:619–25.
Sgouros G, Song H, Ladenson PW, Wahl RL. Lung toxicity in radioiodine therapy of thyroid carcinoma: development of a dose-rate method and dosimetric implications of the 80-mCi rule. J Nucl Med 2006;47:1977–84.
Song H, Prideaux A, Du Y, Frey E, Kasecamp W, Ladenson PW, et al. Lung dosimetry for radioiodine treatment planning in the case of diffuse lung metastases. J Nucl Med 2006;47:1985–94.
International Commission on Radiological Protection. ICRP publication 53: Radiation dose to patients from radiopharmaceuticals. Annals of the ICRP, vol 18. Oxford: Pergamon; 1994.
Chittenden SJ, Pratt BE, Pomeroy K, Black P, Long C, Smith N, et al. Optimization of equipment and methodology for whole body activity retention measurements in children undergoing targeted radionuclide therapy. Cancer Biother Radiopharm 2007;22:243–9.
Akabani G, Poston JW Sr. Absorbed dose calculations to blood and blood vessels for internally deposited radionuclides. J Nucl Med 1991;32:830–4.
Loevinger R, Holt JG, Hine JG. Internally administered radioisotopes. In: Hine JG, Brownell GL, editors. Radiation dosimetry. New York: Academic; 1956. p. 803–75.
Stabin MG, Sparks RB, Crowe E. OLINDA/EXM: the second-generation personal computer software for internal dose assessment in nuclear medicine. J Nucl Med 2005;46:1023–7.
Leeper RD. The effect of 131I therapy on survival of patients with metastatic papillary or follicular thyroid carcinoma. J Clin Endocrinol Metab 1973;36:1143–52.
Sgouros G. Bone marrow dosimetry for radioimmunotherapy: theoretical considerations. J Nucl Med 1993;34:689–94.
Chiesa C, De Agostini A, Ferrari M, Pedroli G, Savi A, Traino AC, et al. Dosimetria nella terapia medico nucleare del carcinoma tiroideo metastatico differenziato: calcolo della dose al midollo emopoietico. Notiziario Associazione Italiana Fisica in Medicina 2006;4:299–307.
Traino AC, Ferrari M, Cremonesi M, Stabin MG. Influence of total-body mass on the scaling of S-factors for patient-specific, blood-based red-marrow dosimetry. Phys Med Biol 2007;52:5231–48.
Acknowledgment
This work was developed under the close supervision of the Dosimetry Committee of the EANM (M Bardiès, C Chiesa, G Flux, S-E Strand, S Savolainen, M Monsieurs and M Lassmann).
Author information
Authors and Affiliations
Corresponding author
Additional information
Michael Lassmann, Carlo Chiesa and Glenn Flux are members of the EANM Dosimetry Committee.
Markus Luster is a member of the EANM Therapy Committee.
Rights and permissions
About this article
Cite this article
Lassmann, M., Hänscheid, H., Chiesa, C. et al. EANM Dosimetry Committee series on standard operational procedures for pre-therapeutic dosimetry I: blood and bone marrow dosimetry in differentiated thyroid cancer therapy. Eur J Nucl Med Mol Imaging 35, 1405–1412 (2008). https://doi.org/10.1007/s00259-008-0761-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00259-008-0761-x