Abstract
The purpose of this set of guidelines is to help the nuclear medicine practitioner perform a good quality lung isotope scan. The indications for the test are summarised. The different radiopharmaceuticals used for the ventilation and the perfusion studies, the technique for their administration, the dosimetry, the acquisition of the images, the processing and the display of the images are discussed in detail. The issue of whether a perfusion-only lung scan is sufficient or whether a full ventilation–perfusion study is necessary is also addressed. The document contains a comprehensive list of references and some web site addresses which may be of further assistance.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Purpose
The purpose of this guideline is to offer the nuclear medicine team a helpful framework in daily practice. This guideline deals with the indications, acquisition, processing and interpretation of lung scintigraphy in children. It should be taken in the context of “good practice” of nuclear medicine and local regulations.
The present document is inspired by the desire of the European Association of Nuclear Medicine and the Society of Nuclear Medicine to have guidelines for most nuclear medicine procedures. This guideline is more specifically tailored to European nuclear medicine practice.
This guideline summarises the views of the Paediatric Committee of the European Association of Nuclear Medicine.
Background and definitions
Lung scintigraphy can be easily performed in children since it requires little or no co-operation, unlike most traditional lung function tests. The respiratory function of the lung can be studied by ventilation (V) and perfusion (Q) scintigraphy [1]. There are also scintigraphic techniques for the study of lung functions not directly related to gas exchange, like mucociliary clearance and epithelial permeability; however, very little work has so far been devoted to the latter studies in children [2].
Indications
It should be underlined that lung scintigraphy provides functional information often undetected on the basis of traditional X-ray techniques. Whilst in case of an obvious abnormality on the chest X-ray, such as lung consolidation, lung scintigraphy simply duplicates the information, lung isotope scan is particularly helpful when chest X-ray findings are normal.
Lung scintigraphy in children has been used in several lung diseases [3–8]. Mismatch in ventilation/perfusion images is found in congenital heart and great vessel diseases [9–11], with a mismatched segmental perfusion defect most likely being due to lung sequestration with arterial supply from the thoracic or abdominal aorta. A lung perfusion study may also be used to quantify the right-to-left shunt fraction [12]. Lung scintigraphy allows correct interpretation of radiological hyperlucent areas, as in partial obstruction due to missed foreign body inhalation; it is also highly sensitive in detecting the late sequelae of it [13]. The lung isotope scan is also helpful in evaluating the extent of functional impairment in cystic fibrosis and bronchiectasis, both at diagnosis and during follow-up [14–20]. It can also have a place in the study of lung involvement in suspected recurrent respiratory conditions of unknown origin [21–23] or in assessing the efficacy and side-effects of some treatments [24–28].
Common indications
-
Primary abnormalities of the lung and pulmonary vessels
-
Congenital anomalies of the heart and great vessels pre- and post-surgery
-
Infective and post-infective lung damage
-
Evaluation of regional lung function with bronchiectasis
-
Evaluation of postoperative regional lung function
-
Cystic fibrosis
-
Foreign body inhalation
-
Detection and measurement of right-to-left shunts
Uncommon or still experimental indications
-
Suspected pulmonary embolism
-
Suspected anomalies of mucociliary function
-
Evaluation of pulmonary toxicity
-
Evaluation of aerosol deposition before administration of nebulised drugs
Perfusion-only scan or ventilation/perfusion scan?
In the case of primary respiratory disease such as foreign body or cystic fibrosis, almost perfect matching exists between ventilation and perfusion because of the very efficient regional hypoxic vasoconstriction mechanism. However, in primary vascular disease (such as pulmonary embolism or abnormalities of the pulmonary artery) perfusion is more affected than ventilation. Therefore, perfusion scintigraphy should be the initial step in all the common indications listed above.
When perfusion is normal, a ventilation scan is not necessary, especially in departments where the ventilation scan would be performed with 99mTc-labelled aerosols or Technegas, which is a relatively time-consuming examination. When perfusion is abnormal, it is up to the clinician to decide whether a primary vascular abnormality is likely or not, thus necessitating a ventilation scan. If the patient complains of an acute problem (for example, an acute chest infection or a recent episode of pulmonary embolism) and the ventilation scan is performed one or more days after the perfusion scan, the perfusion scan should be repeated because the pulmonary pathology may change in the meantime. In contrast, if the indication for lung scintigraphy is a more chronic pathology (for example, tuberculosis, sequestration of a lung segment, chronic pulmonary embolism or thrombosis with very few clinical signs) it would be unnecessary to repeat the perfusion scan when the ventilation scan is performed. The majority of indications for lung isotope scans in paediatrics are primary ventilation abnormalities, for which the ventilation scan would simply duplicate the information provided by the perfusion scan. Reversible ventilation disturbances that cause secondary perfusion defects should be minimised by proper patient preparation (see “Preparation prior to the arrival in the department” section).
In nuclear medicine departments where 81mKr is available, this strategy can be reconsidered because of the very simple and straightforward use of this isotope and its negligible radiation burden.
Procedure
Patient’s clinical history
The referring paediatrician, together with the nuclear medicine physician/radiologist, should decide which kind of scintigraphy or which particular procedure best answers the clinical question for each patient.
The nuclear medicine physician/radiologist has to know not only the clinical question but also the clinical history (focussed on the respiratory problems), the condition of the airways, the possible presence of congenital heart diseases and any possible previous surgery.
The results of a recent chest X-ray and of lung function tests are important in most cases for appropriate isotope scan interpretation.
A history of possible allergies should be obtained with particular reference to previous allergic reactions to human serum albumin.
Patient presentation and preparation
Preparation prior to arrival in the department
No preparation is normally required for the studies listed below. If a child is affected by an acute or chronic airway disease, the referring clinician has to make sure that the nuclear medicine team is aware of this before a ventilation and/or a perfusion study is performed. Information on whether and when the medical or physical therapy should be continued or withdrawn should also be included. This is especially important in children with congenital heart diseases or asthma with recurrent pneumonia or bronchitis. Administration of bronchodilators and steroid aerosol therapy for at least 3 weeks and removal of mucous secretions with mucolytics and chest physiotherapy improve the scintigraphic diagnosis of regional lung disorders [5, 22]. A follow-up study should be performed with the patient in the same condition.
Preparation prior to radiopharmaceutical administration
Sedation is not necessary in the vast majority of cases.
-
a)
Perfusion scan
Whenever possible, the injection and the imaging should be performed in different rooms. A small venous cannula should be inserted first and the tracer administered later via the cannula, just before acquiring images. A good explanation of each step of the test and reassurance are essential to gain the child’s and parents’ cooperation: this is important for a successful intravenous injection of the radiopharmaceutical and makes the child relaxed before the procedure [29].
-
b)
Ventilation scan, mucociliary clearance and epithelial permeability studies
The procedure is explained to the parents and to those children who can understand [29]. There is no particular preparation; children with respiratory problems are used to aerosol therapy and respiratory function tests and can easily accept functional tests via a mouthpiece. Neonates and infants usually fall asleep after a good meal and are not aware of a gently applied face mask.
Radiopharmaceuticals
Perfusion study
Radiopharmaceutical
-
–99mTc-MAA (macroaggregated albumin).
99mTc-MAA
99mTc-MAA (particle size 20–100 μm) is injected intravenously for perfusion studies. In children, MAA should be preferred to microspheres, because of its shorter biological half-life, which reduces the radiation burden. Labelled particles are trapped during their first transit through the pulmonary circulation, in proportion to local blood flow.
Ventilation study
Radiopharmaceuticals: 99m-Tc labelled:
-
a) diethylenetriamine penta-acetic acid (DTPA) aerosol;
-
b) Technegas (dispersion of labelled carbon particles)
-
81m Kr: gas, added to breathed air
99mTc-aerosols
Ventilation studies can be safely performed using inhaled radioactive droplets (aerosols) labelled with 99mTc. Many different aerosols have been used, but DTPA [1, 30, 31] should be preferentially used in children because of the fast renal clearance, which lowers the radiation burden. Even small droplets (0.8–15 μm) have a sufficiently big mass to be affected by turbulent ventilatory flow and can easily distribute within the oral and bronchial mucosa. Ingestion of saliva may cause high gastric signal with possible difficult visualisation of the left lung base. Tracer administration should be quick enough to avoid frequent swallows; co-operative children can be asked to rinse their mouth with water before the beginning of the acquisition. Aerosols containing particles that are not re-absorbed must be used for evaluation of mucociliary clearance. Albumin nanocolloid aerosols have been widely used for this purpose but only with suboptimal results in terms of duration of the examination and reproducibility. DTPA broncho-alveolar epithelial permeability is in fact excessively fast, especially in diseased lungs, and is thus not suitable for measuring the efficacy of mucociliary clearance.
99mTc-Technegas
The name Technegas was invented in November 1984 to describe this relatively new agent for ventilation studies [32], produced by a dedicated apparatus (Technegas generator).
Technegas consists of hexagonal flat crystals of technetium metal cocooned in multiple layers of graphite sheets, completely isolating the metal from the external environment. Each particle is 5–30 nm wide in cross-section and 3 nm thick, and is suspended in an argon carrier gas as a consequence of its production.
The particles are clearly hydrophobic, which is of considerable importance for a lung agent as they will be repelled from aqueous surfaces and water vapour, only being trapped by the surfactant material present in abundance in the alveolar (respiratory airways) region. It has been demonstrated unequivocally that virtually all the activity reaches beyond the 16th division of the bronchial tree. In young infants and babies, owing to lack of cooperation, and in any patient with severe bronchial obstruction, Technegas may also accumulate in proximal bronchi and the trachea. When a significant amount of tracer is trapped in the oropharynx and swallowed with saliva, this may cause artefacts such as those observed with radiolabelled aerosols.
Krypton-81m
81mKr gas allows easy performance of regional ventilation studies during constant continuous inhalation. Because of its very short half-life of 13 s, a significant fraction of the gas is no longer radioactive during the time necessary for 81mKr gas to mix with the air in the alveoli. The slower the regional ventilation (i.e. local air exchange in and out of the alveoli), the smaller the fraction of the still radioactive krypton which reaches the alveoli [33]. Therefore, the signal intensity on the scintigraphic image is related to the exchange of air in and out of the alveoli, also called specific ventilation. The regional distribution of krypton does not represent pure ventilation, but rather a mixture of ventilation and volume. Such proportionality, however, is not linear, and ventilatory mixing may be very fast, sufficient to minimise the radioactive decay effect. This condition is frequently present in neonates and small infants, and may cause difficulty in detecting reduction of regional ventilation [34, 35]. However, these disadvantages are balanced by the unique capability of 81mKr to study tidal breathing with a negligible radiation burden; also, the acquisition of a ventilation study using 81mKr is straightforward, without requiring special patient co-operation. A 81mKr ventilation study can be performed even with the child under sedation. The 81mKr generator (81Rb/81mKr ) produces krypton diluted in atmospheric air; the parent isotope rubidium (81Rb) is obtained as a cyclotron product. The generator remains sufficiently active for clinical purposes for about 12 h after the calibration time. Adjusting the air flow input at 2 l/min, the output of a 100-MBq generator is about 150 MBq/l. The cost of these generators can be lowered by sharing them among different departments during the working day. Unfortunately, nowadays it may be rather difficult to purchase 81m Kr generators, as most companies no longer produce them.
Tracer administration
99mTc-MAA
99mTc-MAA is administered intravenously. This tracer must be kept in its glass vial and gently shaken before withdrawing it into a syringe; once in the syringe, it must be injected with no delay, to avoid adherence of the 99mTc-albumin particles to the inner wall of the syringe. Gravity influences the distribution of ventilation and perfusion tracers. In the upright posture, ventilation and perfusion physiologically increase from the apex to the base [36], whilst in the supine position all zones are equally well visualised, if normally functioning. When a ventilation and a perfusion scan have to be performed within the same session, the two tracers must be administered with the patient in the same position. If 99mTc-labelled radioaerosols or Technegas are used for ventilation scan, the ventilation scan should be performed first. As the radioactive output from the aerosol device or the Technegas generator is normally very low (see “Administered activity for a lung perfusion study”section) and 99mTc-MAA carries an activity 3–times as high, the perfusion images are not significantly affected by the previous ventilation count rate. If 81mKr gas is used for the ventilation scan, this can be acquired before the perfusion scan or both examinations may be performed simultaneously as a dual-isotope scan.
Care must be taken in calculating the amount of particles administered, considering that neonates have about ten times fewer pre-capillary vessels than adults [37]. The number of particles should be kept as low as possible in order to embolise no more than 0.1% of the total lung capillary vessels. A practical table is the following:
Weight | No. of particles |
<10 kg | 10,000–50,000 |
10–20 kg | 50,000–150,000 |
20–35 kg | 150,000–300,000 |
35–50 kg | 300,000–500,000 |
If a severe reduction (more than 50%) of the pulmonary vascular bed is known or suspected, a proportional reduction in the number of particles to be injected is mandatory. A good rule of thumb is to prepare the tracer in order to obtain a known amount of activity (e.g. 1–1.5 MBq) every 5,000 particles present in the vial and to inject 1 MBq/kg body weight. For the measurement of right-to-left shunts (see “Processing” section) the number of macroaggregates to be injected must be reduced to 10,000–20,000 [38] and the concentration of the activity is therefore increased.
When administering 99mTc-MAA, one should refrain from withdrawing blood into the syringe as labelling of small clots may occur with hot spots appearing on the scan as a result.
It is very important that the nuclear medicine physician/radiologist is aware of congenital cardiac and great vessel anomalies as well as of a possible different post-surgical anatomy. For example, in cavopulmonary anastomosis, the blood goes from the superior vena cava to one lung and from the inferior vena cava to the opposite lung. Therefore, differential blood supply to the lungs has to be assessed by two-step 99mTc-MAA perfusion scintigraphy; this means the acquisition of a first set of images after tracer injection in one of the upper limbs followed by a repeat acquisition after tracer injection in one of the lower limbs [39–41].
99mTc-aerosols
Using 99mTc aerosols, it is important to avoid contamination, either from breathed air or from excessive air flow of the aerosol. Radiolabelled aerosols can be administered in front of the camera via a surgical-type face mask fitted over the nose and mouth of infants younger than 2 years or via a nebuliser hood [42]; a mouthpiece and nose clips must be used in older children and in adults. Breathed particles can be efficiently trapped in cheap plastic filters. Aerosol administration is stopped after 2 min. Pulmonary retention is less than one-tenth of the nebulised tracer, so the aerosol machine should be loaded with as much as 15 times the activity of the DTPA needed, diluted in 2 ml of saline. The calculated administered dose is scaled on a body surface basis [43, 44]. Minimum activity within the lungs should be not less than 10 MBq, to allow for sufficient count statistics. When perfusion and ventilation scans have to be performed within the same session, the administered activity for the ventilation scan should be about one-third of the dose of 99mTc-MAA for the perfusion study. It is necessary to test the procedure in each nuclear medicine department and to modify the dose placed into the nebuliser in order to correct for differences in the efficiency of different aerosol devices.
99mTc-Technegas
The patient should be familiarised with the single-use plastic breathing set with a special filter to capture breathed Technegas. The machine generates very reproducible amounts of Technegas. A 5-s breath-hold at the end of the inspiration is strongly recommended because it increases tracer retention for each breath from 20% to 80%.
If at all possible, patients should be supine during the inhalation. It is better to administer the tracer in a separate and well-ventilated room different to the scanning room, in order to prevent environmental contamination and an increase in background activity. The inhaled Technegas should be monitored by a simple dosimeter. Administration should last for a maximum of 10 min. Technegas administration in the scanning room is not ideal, and may be performed only if there is no alternative. Tracer administration should last until a sufficient count rate has been achieved (2 kcounts/min is suggested).
Once the isotope administration has been completed, the patient may return to the waiting area until the beginning of the acquisition. Technegas imaging of lungs of volunteers up to 22 h after tracer administration has shown a less than 3% loss of activity from the lung field in that time, correcting for radioactive decay.
Krypton-81m
81mKr gas is eluted with humidified air through the rubidium generator and administered by continuous inhalation during the acquisition of the images, mixed with atmospheric air. A standard oxygen mask can be used in children, connected with a 200–300 ml volume reservoir, where 81mKr accumulates to maintain a constant concentration in the airways. In neonates and small infants, tidal breathing is low compared with 81mKr flow (2 l/min), so that a constant concentration is obtained by simply placing the tip of the tube close to the nostrils; the excess of gas that is not inhaled can be removed by simply blowing it away from the field of view with a fan. Since the ventilation rate in normal infants at term is about 200 ml/kg per minute [45], this approach is theoretically valid for infants weighing less than 10 kg. A plastic tube to quickly transfer the 81mKr gas from the generator to the air breathed by the patient is necessary to avoid excessive radioactive decay; the tube should therefore be no longer than 2–3 m and rather thin. Because of the rapid 81mKr decay, environmental contamination is not a problem and the radiation burden is very low as compared with other radioisotopes for ventilation studies and with a chest X-ray.
Contraindications and precautions
No adverse effects have been reported from inhalation of 81mKr gas, 99mTc-Technegas, 99mTc-DTPA or other aerosols. The administration of 99mTc-human albumin particles is contra-indicated in patients with a history of hypersensitivity to products containing human serum albumin. The presence of a massive right-to-left shunt causes some concern because of systemic micro-embolisation. However, only a very small fraction of the systemic capillaries are temporarily embolised and symptoms due to embolisation have never been reported in the literature.
Dosimetry
Administered activity for a lung perfusion study
-
Minimum activity: 15 MBq 99mTc-MAA.
-
The maximum activity ranges between 100 and 160 MBq, according to the different national societies and local rules.
-
The administered dose should be scaled based on the body surface area [43, 44].
Administered dose for a lung ventilation study
See 99mTc aerosols in “Tracer administration” section
Radiation burden
These data are calculated for a 5-year-old child [46–49]:
Radiopharmaceutical | EDE, mSv/MBq | Target organ, mGy/MBq |
99mTc-MAA | 0.034 | Lung, 0.2 |
99mTc-DTPA aerosol | 0.02 | Bladder, 0.08 |
99mTc- Technegas | 0.047 | Lung, 0.33 |
81mKr | Precise calculation not possible |
The above table is only an example. It must be underlined that, for ventilation tracers, these are estimations based on MIRD methodology for internal contamination. Precise calculation of EDE with 81mKr is not possible. The usual administered activity in adults is within the range 40–400 MBq 81mKr. A very rough estimate of the average effective dose for a ventilation study in children is within the range 0.004–0.01 mSv. Data are not available for other radiopharmaceuticals. Care must be taken in checking the efficiency of the delivery apparatus and in reducing the radiation burden due to emission from its reservoir.
Image acquisition
Perfusion studies
The child is placed supine on the gamma camera couch or better, if possible, directly on the collimator surface. Acquisition must begin within a few minutes from the administration. A high-resolution, low-energy collimator should be used. Static perfusion images are obtained in a 128×128 or 256×256 matrix format, the latter to be preferred. From 200 k up to 500 k counts per view are sufficient, depending on the size of the child, with a zoom large enough to include both lungs in the field of view with good margins. Anterior, posterior, left and right anterior and posterior oblique views are the standard set of images to be acquired; care must be taken in acquiring the oblique views so that the two lungs are clearly separated in the image. In children there is little point in adding lateral views because of the significant number of photons shining through from the contralateral lung [4, 5]. If only calculation of the split lung perfusion is required, anterior and posterior projections are sufficient. For the quantification of right-to-left shunt, a posterior image of the whole body for the same time as the posterior projection of the lungs is necessary [50, 51].
Ventilation studies
99mTc-labelled aerosols and Technegas
The child is placed supine on the gamma camera couch or better, if possible, directly on the collimator surface. Grown-up children who do not require sedation may be scanned in the upright position, for example sitting on a stool. However, and especially if 81mKr is used as the ventilation agent, the upright position may be more difficult for the patient to keep absolutely still in the same position for both the ventilation and perfusion images (children find it easier to keep still in the supine position, when they lie flat on the couch—or collimator—surface). When aerosols are administered, acquisition must begin within a few minutes from the administration, whilst no such time constraints apply in acquiring images after Technegas inhalation. A high-resolution, low-energy collimator is recommended. Owing to the smaller amount of activity administered, static ventilation images are obtained in a 128×128 matrix format, and 200 k counts per view are sufficient with a zoom large enough to encompass both lungs in the field of view, with good margins. Anterior, posterior, left and right anterior and posterior oblique views are the standard set of images to be acquired; care must be taken in acquiring the oblique views so that the two lungs are clearly separated in the image.
Mucociliary clearance and epithelial permeability
The study of mucociliary clearance and epithelial permeability requires the acquisition of a dynamic study in the posterior projection with a 128×128 matrix. A general-purpose, low-energy collimator is preferable to obtain adequate counting statistics. For epithelial permeability studies the duration of the scan should be at least 30 min, with a frame acquired every 30 s; in pathological cases the clearance is faster. Study of the mucociliary clearance, a slower phenomenon with a longer clearance time in abnormal cases, requires a duration of at least 60 min, with a frame duration of 1 min.
Krypton-81m
The child is positioned supine on the gamma camera couch or better, if possible, directly on the collimator surface. Acquisition must begin within a few minutes from tracer administration. A medium-energy, general-purpose collimator can be used with 81mKr (190 keV peak energy) because its spatial resolution is sufficient, even in small babies and newborns, to detect subsegmental defects. A high-resolution low-energy collimator may be preferable, provided that septa penetration is sufficiently low. A low-energy collimator is, however, acceptable. As there are different collimator models on the market from different manufacturers, it is suggested that each department tests each model and selects the one felt to be preferable. Owing to the smaller amount of administered activity, static ventilation images are acquired with a 128×128 matrix format. Two hundred k counts per view are sufficient with an electronic zoom large enough to encompass both lungs in the field of view, with good margins. Anterior, posterior, left and right anterior and posterior oblique views constitute the standard set of images to be recorded. Care must be taken in acquiring the oblique views so that the two lungs are clearly separated in the image.
Processing
Semi-quantitative numerical data can be obtained from ventilation and perfusion studies. These are useful in the follow-up of severe lung diseases and in the pre- and post-surgical evaluation. The left/right count ratio (or counts in one lung as a percentage of the total) is obtained from the geometric mean of the counts from both lungs in the anterior and posterior views; it is a useful index in unilateral lung disease (for instance in pulmonary artery malformations, hyperlucent lung, surgical shunts, congenital heart diseases and hypoplastic lung). Normally, the ratio is very close to one; counts from the left lung are slightly less, from 42% to 45% of the total [5, 11].
In the evaluation of right-to-left cardiac shunts (R-L shunt), methods for the quantitative assessment are described, based on the use of 99mTc-albumin MAA perfusion scintigraphy [12, 38, 50, 51]. In fact, in the case of a R-L shunt the MAA bypasses the pulmonary capillary bed and is trapped in the organs with the highest blood flow, i.e. the brain and the kidneys. For this purpose, it is necessary to acquire a whole-body scan in both the anterior and the posterior view, starting 2 min after the injection of 99mTc-MAA, at a speed of 30 cm/min. On these images, regions of interest (ROIs) encompassing the body and lung contours must be drawn and the geometric mean of the counts included in corresponding anterior and posterior ROIs obtained. The amount of shunted blood can be obtained by the following formula:
R-L shunt (%) = [(total body counts−lung counts) / total body counts] ×100 [12, 50].
When measuring a R-L shunt, the presence of free technetium must be taken into account and the labelling efficiency for 99mTc-MAA should be more than 98%. The images must be visually analysed to look for uptake in the thyroid gland and the gastric mucosa due to physiological fragmentation of particles and not to a R-L shunt.
Hard copy
It is preferable to view the study on the screen of the workstation rather than on a hard copy. If hard copies are required by the referring clinician, images should be presented on X-ray film or on photographic quality paper. A linear grey scale (neither logarithmic, nor exponential) should be used. The final display should always include all the views correctly acquired. Colour prints (with arbitrary colour scales) are not useful and may lead to misinterpretation. The ROIs used for computerised analysis should be included in the hard copy as well as all the numerical data required for the report. Curves relative to mucociliary clearance or epithelial permeability should also be included.
Interpretation/reporting/pitfalls
Interpretation
A recent chest X-ray should be available to assist in the interpretation of the images. The ventilation and perfusion scans should be reported describing the site, number and extent of the abnormalities. The use of simplified charts of lung segments [52, 53] greatly helps in the description of the anatomical site of the defects. However, the anatomical shape of the lungs may be modified by disease or may be unpredictable because of individual congenital variations. The knowledge of normal variants in children is essential (e.g. more prominent and central cardiac silhouette, anterior elevation of the right diaphragm in the supine position due to the liver, round-shaped latero-basal margins of the lungs often seen in newborns and infants). In congenital heart disease, the right heart can sometimes be very enlarged, causing the appearance of a very narrow lung base on scintigraphic images: this should not be mistaken for lung disease.
Reporting
The report should specify the tracer used, the amount of activity administered, the route of administration and the patient’s posture during tracer administration. The description of the findings should begin with a general description of both lungs, followed by a comment on the possible presence of a difference in tracer distribution between the two lungs and possible defects in each lung and their site. If numerical data have been obtained, normal values should also be quoted.
The conclusion of the report should:
-
confirm or exclude the presence of regional lung disease;
-
describe the changes caused by medical or surgical treatment—if any—in relation to previous scans;
-
suggest further investigations, if needed.
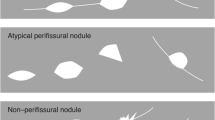
Pitfalls
-
Technetium-labelled inhaled particles/aerosols may be swallowed by the child, so activity in the stomach may be seen, and this must be correctly interpreted.
-
Obstructive airway disease or incorrect breathing during administration of aerosols may cause inhomogeneous clot-like distribution of the tracer in the main bronchi, which makes evaluation of more peripheral ventilation very difficult.
-
The very fast exchange of air in and out of the alveoli in the lungs of small babies and newborns may limit the functional value of 81mKr ventilation images (see Krypton-81m in “Ventilation study”section): if local reduction of ventilation is suspected and the 81mKr scan is normal, then a Tc99m-labelled aerosol scan may help.
-
Chest wall compression during i.v. tracer administration (in the attempt to keep the child still) may reduce local perfusion: under these circumstances the tracer for a lung perfusion study should not be administered.
-
Local hypoxic vasoconstriction (regional hypoperfusion secondary to hypoventilation) due to transitory causes (like mucous plugging or bronchial constriction) should be treated pharmacologically before performing a lung perfusion scan. A typical example is in asthmatic children, in whom hypoxic vasoconstriction can cause an abnormal distribution pattern that is not necessarily indicative of permanent lung damage.
-
Age-related differences of regional perfusion have to be taken into account: perfusion abnormalities in the upper zones are more typical in diseases of early infancy, while the lower zones are more frequently involved in pathology of later childhood [27].
References
O’Brodovich HM, Coates G. Quantitative ventilation-perfusion lung scans in infants and children: utility of submicronic radiolabelled aerosol to assess ventilation. J Paediatr 1984;105:377–83.
Agnew JE, Sutton PP, Pavia D. Radioaerosol assessment of mucociliary clearance: towards definition of a normal range. Br J Radiol 1986;59:147–51.
Johnson K. Ventilation and perfusion scanning in children. Paediatr Respir Rev 2000;1(4):347–53.
Piepsz A, Gordon I, Hahn K. Paediatric nuclear medicine. Eur J Nucl Med 1991;18:41–66.
Ciofetta G, Ronchetti R, Silverman M. Regional lung function testing in children. Eur Respir J Suppl 1989 Mar;4:171S-180S.
Gilday DL, Poulouse KP, Dore EK, et al. Accuracy of detection of pulmonary embolism by lung scanning correlated with pulmonary angiography. Am J Roentgenol 1972;115:732–8.
Falconer AR, Brown RA, Helms P, et al. Pulmonary sequelae in survivors of congenital diaphragmatic hernia. Thorax 1990;2:126–9.
Stefanutti G, Filippone M, Tommasoni N, et al. Cardiopulmonary anatomy and function in long-term survivors of mild to moderate congenital diaphragmatic hernia. J Pediatr Surg 2004;39:526–31.
Gelfand MJ, Hannon DW. Nuclear studies of the heart and great vessels. In: Miller J, Gelfand MJ, editors. Pediatric nuclear imaging. Philadelphia: WB Saunders; 1994. p 83–101.
Pruckmayer M, Zacheri S, Salzer-Muhar U, et al. Scintigraphic assessment of pulmonary and whole-body blood flow patterns after surgical intervention in congenital heart disease. J Nucl Med 1999;40:1477–83.
Kim JH, Lee DS, Chung JK, et al. Quantitative lung perfusion scintigraphy in postoperative evaluation of congenital right ventricular outflow tract obstructive lesions. Clin Nucl Med 1966;21:471–6.
Lu G, Shih WJ, Chou C. 99mTc-MAA total-body imaging to detect intrapulmonary right to left shunts and to evaluate the therapeutic effect in pulmonary arteriovenous shunts. Clin Nucl Med 1996;21:197–202.
Piepsz A. Late sequelae of foreign body inhalation; a multicentric scintigraphic study. Eur J Nucl Med 1988;13:578–81.
Stanchino ML, Tantisira KG, Aquino SL, et al. Association of lung perfusion disparity and mortality in patients with cystic fibrosis awaiting lung transplantation. J Heart Lung Transplant 2002;21(2):217–25.
Itti E, Fauroux B, Pigeot J, et al. Quantitative lung perfusion scan as a predictor of aerosol distribution heterogeneity and disease severity in children with cystic fibrosis. Nucl Med Commun 2004;25(6):563–9.
Piepsz A, Decostre P, Baran D. Scintigraphic study of pulmonary blood flow distribution in cystic fibrosis. J Nucl Med 1973;14:326–30.
Samanek M, Houstek J, Vavrova V. Distribution of pulmonary blood flow in children with cystic fibrosis. Acta Paediatr Scand 1971;60:149–57.
Piepsz A, Wetzburger C, Spehl M, et al. Critical evaluation of lung scintigraphy in cystic fibrosis: study of 113 patients. J Nucl Med 1980;21:909–13.
Vandervivere J, Sphel M, Dab I et al: Brochiectasis in childhood. Comparison of chest roentgenograms, bronchography and lung scintigraphy. Pediatr Radiol 1980;9(4):193–8.
Eastman KM, Fall AJ, Mitchell L, Spencer DA. The need to redefine non cystic fibrosis bronchiectasis in childhood. Thorax 2004;59(4):324–7.
Ciofetta G, Fatone R, Caresta D, et al. Recurrent bronchitis in childhood: the case for scintigraphic investigation. Eur J Nucl Med 1985;11:172.
Ciofetta G. Lung scintigraphy in the assessment of recurrent bronchitis and pneumonia in children. Q J Nucl Med 1997;41:292–301.
Hardoff R, Rivlin J, Front A. The contribution of perfusion scintigraphy in the evaluation of children suffering from recurrent localized pneumonia. Eur J Nucl Med 1990;17:152–5.
Alderson PO, Chen DC, Fleishman MJ, et al. Radioaerosol scintigraphy in infants and children born to mothers with HIV disease. Pediatric pulmonary and cardiovascular complications (of vertically transmitted human immunodeficiency virus) study group. Radiology 1999;210(3):815–822.
Lerondel S, Vecellio None L, Faure L, et al. Gene therapy for cystic fibrosis with aerosolized adenovirus-CFTR: characterization of the aerosol and scintigraphic determination of lung deposition in baboons. J Aerosol Med 2001;14(1):95–105.
Dubus JC, Vecellio L, De Monte M, et al. Aerosol deposition in neonatal ventilation. Pediatr Res 2005;58(1):10–4.
Regnis JAM, Robinson DL, Bailey P, et al. Mucociliary clearance in patients with cystic fibrosis and in normal subjects. Am J Respir Crit Care Med 1994;150:66–71.
de Azambuja E, Fleck JF, Barreto SS, et al. Pulmonary epithelial permeability in patients treated with bleomycin containing chemotherapy detected by technetium-99m diethylene triamine penta-acetic acid aerosol (99mTc-DTPA) scintigraphy. Ann Nucl Med 2005;19(2):131–5.
Ljung B. The child in diagnostic nuclear medicine. Eur J Nucl Med 1997;24:683–90.
Pielter P, Bardies M, Chetanneau A, et al. Comparison of technetium-99m and phytate aerosol in ventilation studies. Eur J Nucl Med 1992;19:349–54.
Cabahug CJ, McPeck M, Palmer LB, et al. Utility of technetium-99m-DTPA in determining regional ventilation. J Nucl Med 1996;37:239–44.
Jackson P, Mackey D, van der Wall H. Physical and chemical nature of Technegas. J Nucl Med. 1998;39(9):1646–9.
Fazio F, Jones T. Assessment of regional ventilation by continuous inhalation of radioactive krypton-81m. Br Med J 1975;3:673–6.
Ciofetta G, Silverman M, Hughes JMB. Quantitative approach to the study of regional lung function in children using krypton-81m. Br J Radiol 1980;53:950–9.
Ham HR, Vandevivere J, Dab I, et al. Limitations of steady state krypton-81m ventilation study in children. Nucl Med Commun 1981;2:43–8.
Kaneko K, Milic-Emili J, Dolovich MB, et al. Regional distribution of ventilation and perfusion as a function of body position. J Appl Physiol 1966;21:767–77.
Inselman LS, Mellins RB. Growth and development of the lung. J Pediatr 1981;98:1–15.
Grimon G, Andre L, Bernard O, et al. Detection of intrapulmonary shunts in children with liver disease. J Nucl Med 1994;35:1328–32.
Del Torso S, Kelly MJ, Kalff V, et al. Non-invasive assessment of pulmonary blood supply after staged repair of pulmonary atresia. Br Heart J 1985;54:209–14.
Boothroyd AE, McDonald EA, Carthy H. Lung perfusion scintigraphy in patients with congenital heart disease: sensitivity and important pitfalls. Nucl Med Commun 1996;17:33–9.
Kreutzer C, Mayorquim RC, Kreutzer GO, et al. Experience with one and half ventricle repair. J Thorac Cardiovasc Surg 1999;117:662–8.
Amirav I, Balanov I, Goremberg M et al. Nebuliser hood compared to mask in wheezy infants: aerosol therapy without tears! Arch Dis Childhood 2003;88:719–23.
Haycock GB, Schwartz GJ, Wisotsky DH. Geometric method for measuring body surface area: a height-weight formula validated in infants, children, and adults. J Pediatr 1978;93:62–6.
Piepsz A, Hahn K, Roca I, et al. A radiopharmaceutical schedule for imaging in paediatrics. Paediatric Task Group of the European Association of Nuclear Medicine. Eur J Nucl Med 1990;17:127–9.
Nelson NM, Prod’hom LS, Cherry RB, et al. Pulmonary function in the newborn infant II. Perfusion estimation by analysis of the arterial-alveolar CO2 differences. Pediatrics 1962;30:975.
Stabin MG, Gelfand MJ. Dosimetry of pediatric nuclear medicine procedures. Q J Nucl Med 1998;42:93–112.
Thomas SR. MIRD pamphlet no 18; administered cumulated activity for ventilation studies. J Nucl Med 2001;42(3):520–6.
Stabin MG. Pediatric nuclear medicine. In: Treves ST, editor. New York: Springer, chapter 26; 1994.
Annals of the ICRP, 1998; 80(28/3):31–3.
Semih Dogan A, Rezai K, Kirchner PT, et al. A scintigraphic sign for detection of right-to-left shunts. J Nucl Med 1993;34(9):1607–11.
Sugyiama M, Sakahara H, Igarashi T, et al. Scintigraphic evaluation of small pulmonary right-to-left shunt and therapeutic effect in pulmonary arteriovenous malformation. Clin Nucl Med 2001;26:757–60.
Morrell NW, Roberts CM, Jones BE, et al. The anatomy of radioisotope lung scanning. J Nucl Med 1992;33(5):676–83.
Magnussen JS, Chicco P, Palmer AW, et al. Optimisation of the scintigraphic segmental anatomy of the lungs. J Nucl Med 1997;38:1987–91.
Author information
Authors and Affiliations
Corresponding author
Additional information
More information about Technegas may be found on the website http://www.dupharma.dk/prod08.htm
More information about 99mTc-labelled aerosols may be found on the website http://www.healthlinemed.com
Under the Auspices of the Paediatric Committee of the European Association of Nuclear Medicine.
Rights and permissions
About this article
Cite this article
Ciofetta, G., Piepsz, A., Roca, I. et al. Guidelines for lung scintigraphy in children. Eur J Nucl Med Mol Imaging 34, 1518–1526 (2007). https://doi.org/10.1007/s00259-007-0485-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00259-007-0485-3