Abstract
Introduction
There is growing evidence that myocardial metabolism plays a key role not only in ischaemic heart disease but also in a variety of diseases which involve myocardium globally, such as heart failure and diabetes mellitus. Understanding myocardial metabolism in such diseases helps to elucidate the pathophysiology and assists in making therapeutic decisions.
Measurement
As well as providing information on regional changes, PET can deliver quantitative information about both regional and global changes in metabolism. This capability of quantitative measurement is one of the major advantages of PET along with physiological positron tracers, especially relevant in evaluating diseases which involve the whole myocardium.
Discussion
This review discusses major PET tracers for metabolic imaging and their clinical applications and contributions to research regarding ischaemic heart disease and other diseases such as heart failure and diabetic heart disease. Future applications of positron metabolic tracers for the detection of vulnerable plaque are also highlighted briefly.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction: Why PET?
The myocardium uses a variety of substrates, predominantly free fatty acids (FFAs), glucose and lactate, as sources of energy. Myocardial metabolism is much more complex than brain and/or tumour metabolism, which are also major targets for PET metabolic imaging.
Understanding the myocardial metabolism of substrates is very important for understanding the pathophysiology of various cardiac diseases and for designing therapeutic interventions. Early studies of myocardial metabolic imaging were mainly focussed on the ischaemic heart disease. The findings of those studies demonstrated the usefulness of 18F-fluorodeoxyglucose positron emission tomography (PET) imaging to detect viable myocardium. Over the past decade, a growing body of evidence has been accumulated showing that changes in myocardial metabolism play a key role in various other cardiac conditions, such as heart failure, diabetes and the myocardium under biventricular pacing. However, due to difficulties in evaluating metabolism in human subjects, the alterations in myocardial metabolism under such conditions are poorly understood.
There are several biophysical tools to visualise myocardial metabolism non-invasively. PET, single-photon emission computed tomography (SPECT) and nuclear magnetic resonance spectroscopy (MRS) are included in this category. Among them, PET offers several unique advantages, including intrinsic capability of quantitative measurement and the use of physiological substrates such as acetate and FFAs labelled with positron-emitting radionuclides. On the other hand, PET has some shortcomings. One major and critical disadvantage of PET is its poor availability. However, the availability of PET equipment is increasing as oncological applications of PET increase.
SPECT is one of the other choices for evaluating myocardial metabolism. A radioiodine-labelled long chain fatty acid, 123I-(p-iodophenyl)-3-(R,S) methylpentadecanoic acid (BMIPP), which is one of the fatty acid metabolism tracers, is commercially available and widely used for clinical diagnosis, especially in Japan. However, SPECT currently lacks the capability of quantitative measurement. The measurement of myocardial metabolism in absolute units is important for the study of diseases such as heart failure and dilated cardiomyopathy, which may not display regional disparities. Practically, this capability of quantitative measurement is only provided by PET.
Metabolic substrates and their PET tracers
Metabolism of myocardium in brief
Normal myocardium utilises both glucose and FFAs. Under fasting conditions, the myocardium mainly uses fatty acids as the major source of fuel for oxidation. In response to insulin stimulation or increased work load, the rate of glucose uptake is increased. When ischaemic insults complicate the myocardium, the utilisation of exogenous glucose also increases. A huge amount of evidence supports the notion that this phenomenon plays a key role in diagnosing myocardial ischaemia and viability. The early development and application of PET tracers for heart disease was focussed on ischaemic heart disease, especially on viability assessment.
Figure 1 provides a summary of myocardial substrate metabolism and PET tracers.
Glucose metabolism and FDG
Fluorine-18 fluorodeoxyglucose (FDG) is a glucose analogue which traces the transmembranous uptake and phosphorylation of exogenous glucose in living tissue. FDG that enters the myocardium is phosphorylated to FDG-6-phosphate, and then does not enter further metabolic pathways and accumulates in the myocardium. Thus, the uptake of FDG reflects the uptake and metabolism of glucose [1, 2]. FDG has played a fundamental role in cardiac PET imaging, especially as the “gold standard” for viability assessment. In contrast to other metabolic tracers such as 11C-palmitate and 11C-acetate which require dynamic imaging, a significant body of evidence supports the conclusion that even a simple static image of FDG uptake contains significant metabolic information about viability. The ease of use of FDG has contributed to its becoming the most familiar PET tracer used for clinical applications.
Not only the relative distribution of FDG uptake, but also the metabolic rate of glucose (MRG) in absolute units can be measured with PET. To measure absolute MRG, mathematical modelling such as compartment model analysis [3, 4] or graphical plot analysis [5, 6] and dynamic data acquisition over about 1 h are required.
The rate of FDG uptake is not equal to the rate of glucose uptake. Several experimental studies have provided critical information about the ratio of FDG uptake to glucose uptake. This ratio is called the lumped constant (LC). Usually, the LC is around 0.6–0.7 and a fixed (that is why it is called the lumped “constant”) value is used for the PET analysis [2, 4]. Using this constant, the metabolism of glucose can be evaluated with FDG PET. However, some early studies indicated that LC could vary. LC can differ between organs [7], so we cannot simply apply LC measured in some other tissue such as the cerebral cortex to the myocardium. Even under physiological conditions, LC can vary over a wide range depending on the concentration of blood insulin [8]. In this context, when the metabolic rate of glucose or even the relative distribution of FDG is analysed, one must note that the values calculated from FDG PET are merely rough estimates of glucose metabolism/uptake, although they are still very useful.
Fatty acid metabolism and PET tracers
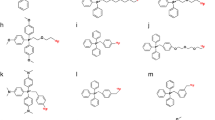
PET has unique advantages for tracing physiological substrates labelled with positron emitters. However, usually, a physiological tracer requires dynamic data acquisition and mathematically complex analysis such as compartment model analysis or graphical plot analysis. Metabolically trapped tracers such as FDG are easy to use because a static image by itself provides valuable information. On the other hand, trapped tracers usually have problems regarding discrepancies between physiological substrates, which results in difficulty in image interpretation. For fatty acid metabolism, physiological tracers such as 11C-palmitate were introduced first, and, more recently, trapped tracers such as 18F-FTHA were developed.
11C-palmitate is long-chain saturated fatty acid labelled with carbon-11, which has a physical half-life of only 20 min. It is biologically identical to non-radioactive circulating palmitate. Once 11C-palmitate is taken up into the myocardium, β-oxidation breaks it down to generate acetyl-CoA. This 11C-labelled acetyl-CoA is oxidised via the citric acid cycle and finally released from the myocardium in the form of 11C-CO2. The analysis of FFA metabolism using 11C-palmitate is complex because this tracer is metabolised through a complex pathway of β-oxidation and the citric acid cycle. Some studies use simple clearance time as the index of FFA metabolism [9], while others use complex compartment model analysis [10]. The most frequently used method is dividing the 11C washout curve into two phases—early rapid clearance and late slow washout [11]—and then calculating each washout rate. According to early studies, early rapid clearance reflects fatty acid oxidation and late slow washout reflects turnover of the lipid pool.
14(R,S)-[18F]Fluoro-6-thia-heptadecanoic acid (FTHA) is a relatively new long-chain fatty acid analogue [12–14]. It is designed to undergo metabolic trapping after formation of two acetyl-CoA molecules. In the myocardium, subsequent to the partial β-oxidation, the majority of the radioactive metabolites are trapped in the mitochondria [15]. Thus, in the heart, uptake of FTHA traces mainly β-oxidation of FFA. There are some other PET FFA tracers such as 16-[18F]-fluoro-4-thia-palmitate (FTP) [16], 15-[18F]fluoro-3-oxa-pentadecanoate (FOP) [17] and trans-9(RS)-18F-fluoro-3,4(RS,RS)-methyleneheptadecanoic acid (FCPHA) [18]. These tracers are all designed to trace β-oxidation and to be trapped in the myocardium. These trapped tracers are conceptually not ideal to trace the metabolism of FFA. Each has some advantages and disadvantages. For example, FTHA does not trace FFA uptake accurately under hypoxic conditions [19]. It is still not clear which tracer is most reliable or most clinically useful.
Oxidative metabolism and 11C-acetate
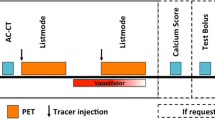
11C-acetate is a well-known tracer for analysing myocardial oxidative metabolism. Because of the high extraction fraction in the coronary circulation, 11C-acetate is rapidly distributed to the myocardium, and then enters the citric acid cycle. Finally, 11C activity is cleared from the myocardium in the form of 11C-CO2. By calculating the washout rate, the oxidative metabolism in the myocardium is measured [20]. Usually, to calculate the washout rate constant of 11C-acetate, mono-exponential fitting is used, and thus this constant is usually called “kmono” (Fig. 2). The citric acid cycle lies metabolically downstream of any aerobic metabolism, so the metabolic milieu such as the blood glucose or FFA concentration in the blood has only minor effects on 11C-acetate kinetics [21]. This independence from the metabolic milieu is one major benefit of using 11C-acetate.
The other major benefit of 11C-acetate is its capability of measuring myocardial perfusion. The high first-pass extraction fraction of 11C-acetate in the myocardium implies that the early tracer uptake is flow dependent [22] (Fig. 3). Gropler et al. demonstrated that the early distribution measured 1–3 min after injection was closely correlated with myocardial blood flow distribution measured with 15O-water [23]. Additionally, some recent studies showed that not only the relative distribution but also absolute measurement can be performed with 11C-acetate using mathematical compartment model analysis [24–26].
Typical myocardial and blood pool time-activity curves obtained during the first 300 s after the intravenous administration of 11C-acetate (left panel) and 13N-ammonia (right panel). Both 11C-acetate and 13N-ammonia are rapidly taken up into the myocardium. No significant washout occurs during the early phase. Note the similarity of the time-activity curves. This high first-pass extraction fraction of 11C-acetate in the myocardium allows perfusion measurement with 11C-acetate
This multipotent character of 11C-acetate is very unique among PET tracers. Using 11C-acetate, simultaneous determination of myocardial blood flow and oxygen consumption can be performed with a single data acquisition. If ECG gating is possible with dynamic acquisition (five-dimensional imaging [27]), even cardiac function can be evaluated simultaneously. It is very challenging to acquire dynamic serial images with ECG gating using regularly available PET scanners. Porenta et al. attempted this by performing dynamic acquisition and ECG-gated acquisition sequentially, not simultaneously, and successfully obtained perfusion, oxygen consumption and cardiac function using a single imaging protocol [28].
Clinical application for ischaemic heart disease
Concept of detection of viability
It is unquestionable that viability is one of the most important aspects of the diagnostic and prognostic work-up of CAD patients. Precise assessment of viability is among the most important missions of nuclear cardiology. Many end-points have been proposed for understanding and diagnosing myocardial viability, including preserved cellular metabolism, membrane integrity, perfusion status, presence or absence of apoptosis, preserved contractile reserve and metabolic reserve. There are many methods for evaluating these end-points, including SPECT, PET, dobutamine stress echo and magnetic resonance imaging. What should be considered the gold standard technique for viability assessment has long been the subject of debate. From the physiological point of view, these methods are divided into two major categories. One of the categories observes a static cellular condition such as metabolism or membrane integrity, like a snapshot. This category includes most of the nuclear imaging techniques. The techniques included in the other category look at the dynamic response to stress (usually inotropic stress), like a motion picture. This category includes dobutamine echo and some of the nuclear techniques.
FDG: a gold standard for viability
The major contribution of FDG PET imaging to cardiology is viability assessment in ischaemic heart disease. The level of myocardial flow at rest alone does not define the myocardial viability after ischaemic insults. The “stunned myocardium” after acute ischaemia usually shows near-normal perfusion. In some cases of hibernating myocardium, the resting flow cannot differentiate hibernating myocardium from irreversible myocardial scar formation. The residual metabolism in viable myocardium helps to identify viable myocardium. Relatively higher uptake of FDG compared with a perfusion tracer such as 13N-ammonia in dysfunctional myocardium indicates viable myocardium. This finding was first reported by Tillish et al. [29]. Since then, FDG imaging has been thought of as one of the gold standards for viability, mainly due to the huge volume of cumulative evidence obtained using this technique since Tillisch’s study.
Unlike the brain, which mainly depends on glucose metabolism, the myocardium is an omnivore. There are three major circulating substances which affect the myocardial metabolism: blood glucose, FFAs and insulin. Many other factors, such as the fasting period and age, also affect the FDG uptake [30]. Even hospitalisation status (in-patients or out-patients) has an influence on the myocardial FDG uptake [31]. This complexity interferes with the interpretation of data obtained from FDG PET imaging. To accommodate this complexity of metabolism, there are several different protocols for myocardial FDG PET imaging. These protocols can be divided into two major categories. One is imaging under low myocardial glucose metabolism, which includes imaging under fasting conditions. The other protocol images the myocardium under high to maximum myocardial glucose metabolism, which includes oral glucose loading and the euglycaemic insulin clamp technique.
Under fasting conditions, the normal myocardium primarily utilises fatty acids, while glucose utilisation, and thus FDG uptake, becomes minimal. Under this condition, ischaemic myocardium with enhanced glucose metabolism markedly takes up FDG, which is displayed on PET images as hot spots. The problem of imaging under fasting conditions is the heterogeneous distribution of FDG in the normal myocardium. Usually, the lateral wall of the left ventricle tends to show higher FDG uptake than the septum [32, 33]. High background activity with low tissue FDG uptake also leads to poor image quality. For these reasons, FDG PET under fasting conditions has recently not been recommended for clinical viability assessment.
The most commonly used protocol is oral glucose loading. Ingestion of about 50–70 g of glucose p.o. stimulates insulin secretion, and increases the FDG uptake into normal myocardium to near maximum. This enhances the image quality, with homogeneous myocardial FDG uptake. Euglycaemic insulin clamping is an alternative technique to oral glucose loading, and is slightly more complex but guarantees more stable and controlled metabolic conditions. Under these conditions, FDG uptake into normal and ischaemic but viable myocardium is enhanced, and negative FDG uptake is considered to indicate scar tissue.
With dynamic acquisition, not only the relative tracer distribution but also the absolute metabolic rate of glucose (MRG) can be measured with PET. A threshold of 0.25 mol/min/g under euglycaemic insulin clamp has been proposed for viability assessment [34, 35]. However, this value should be applicable only under insulin clamp. Bax et al. also found that use of relative MRG, which is normalised to MRG of a remote area, gave better accuracy than use of absolute MRG [35]. This is probably because regional glucose uptake on an absolute scale varies widely in both remote normally contracting and dysfunctional regions on an inter-individual basis, even under euglycaemic insulin clamp [36]. Morita et al. reported that increased MRG and glucose transport are found in patients with LV dysfunction, especially in dysfunctional segments [37]. This may also influence the inter-individual variability of MRG. According to these results and the time-consuming nature of absolute measurement (usually more than 1 h is required for dynamic acquisition), absolute measurement is infrequently used.
How to interpret the FDG PET image is also important. The most popular criterion is flow–metabolism mismatch, which indicates reduced perfusion with preserved FDG uptake. A large body of evidence indicates that segments with mismatch frequently show improved function following revascularisation (Fig. 4). However, using this criterion requires a perfusion image, preferably acquired with PET. Relative FDG uptake (usually expressed as % uptake), which is normalised to the uptake of normal myocardium, is also useful for viability assessment. Usually, segments with greater than 50% of normal myocardium uptake are considered viable [36, 38]. This method is easier than the flow–metabolism mismatch criterion because it does not require a perfusion image. The limitation of % uptake criterion is that mild concordant reduction of perfusion and FDG uptake is diagnosed as viable with this criterion (Fig. 5). This mild concordant reduction may represent a mixture of subendocardial scar (=totally dead) and normal epicardial myocardium (=totally normal). This condition usually does not show recovery after revascularisation [39]. Because of this limitation, the mismatch criterion is usually preferred for viability assessment. However, experienced physicians usually take both criteria (and all available information) into account for the diagnosis.
A typical image of flow–metabolism mismatch in viable myocardium (short axis images). Severely reduced perfusion is found on the anteroseptal wall (left panel: yellow asterisks). Note the relatively maintained FDG uptake on the anteroseptal wall (right panel: yellow asterisks). Significant wall motion recovery was found after coronary artery bypass grafting of the left descending artery
The theoretical limitation of the % FDG uptake criterion. Owing to the limited spatial resolution of PET, normal myocardium containing subendocardial scar shows a modest relative reduction in FDG uptake. This condition is diagnosed as viable with the % uptake criterion, although it usually does not show improved function after revascularisation
There are several other methods to assess viability. Viability assessment using nuclear techniques usually tends to show a high negative predictive value (NPV) and a low positive predictive value (PPV). On the other hand, dobutamine stress echocardiography usually tends to show lower NPV and higher PPV. FDG PET seems to show “well-balanced” NPV and PPV values [40, 41]. The choice of imaging modalities does not depend solely on sensitivity/specificity but also on the clinical settings. For example, the high specificity and low cost of dobutamine stress echo favour it as the first choice for viability prediction. On the other hand, FDG PET should be helpful as a last resort to assess viability when clinical suspicion of viability remains after other techniques have proved negative. Barrington et al. compared the diagnostic accuracy of Tl SPECT, MIBI SPECT, dobutamine echo and PET (FDG/NH3) with respect to hibernation in the same study population [42]. They found that when all four imaging modalities were analysed with multivariate analysis, FDG PET was the only independent predictor of hibernation. They concluded that, considering the relatively low PPV of nuclear techniques, including PET, echocardiography could be used as a first-line test, with FDG PET as a second-line test.
However, the most important issue in clinical practice is whether the difference in accuracy between methods is unacceptably large or fairly small. If the difference in accuracy is significant but fairly small, other problems such as low availability may outweigh the significance of this difference. A recent study by Siebelink et al. partially addressed this question [43]. That study compared the survival of patients randomised to PET-based or SPECT-based management. The authors found only a very small and non-significant difference between these two management strategies.
FDG: problems and their solutions
The above result was somewhat shocking, because it means it is not necessary to perform PET to make a Go/No Go decision about coronary intervention in clinical practice. The PET cardiology community must make FDG PET imaging more accurate and sophisticated. There are several problems that need to be solved to make FDG PET more reliable and useful.
The one major problem in viability assessment using FDG PET is the absence of a standardised method. Both the imaging protocol (dynamic/static, loading/insulin clamp/fasting) and data interpretation (mismatch/%uptake/metabolic rate) lacks standards. Knuuti et al. stressed this issue in their review in 2002 [44]. In 2003, ASNC issued a practice guideline for FDG/perfusion PET imaging [45, 46]. The requirement for standardisation was partially solved by this guideline. However, we still need more studies, especially large-scale multi-centre trials, to establish the usefulness of FDG PET imaging in viability assessment.
One of the solutions for improving the accuracy of viability assessment with PET comes from the technology commonly used in SPECT. Appling the gated SPECT analysis technique to FDG PET [47, 48], evaluation becomes more precise [49, 50]. The big problem with this technique is the reliability of the analysis program, such as QGS, 4D-MSPECT or the Emory cardiac tool box. These programs are all designed for clinical SPECT use. Thus, parameters such as gamma fitting for wall detection are not optimised for PET. For several reasons (patents, FDA regulations, etc.) it is very hard for PET users to change and optimise such parameters. It is reported that ventricular volumes (EDV and ESV) measured by gated FDG PET are higher than those measured with MIBI SPECT, although there is a very good correlation between the former and the latter [51]. Even with this limited methodology, gated FDG PET shows significant incremental value over viability diagnosis, as assessed by the perfusion–metabolism mismatch criterion [49].
One of the best-known disadvantages of PET is its low availability. PET scanners and on-site cyclotrons are too expensive for local hospitals. PET has only been available for a limited number of patients and researchers, at least in the last century. Because of this problem, the capabilities of FDG SPECT were instead studied for decades [52, 53]. Using an ultra-high-energy collimator, an FDG image could be obtained with routinely used relatively inexpensive gamma cameras. Some studies showed comparable results to conventional PET scanners [54, 55]. However, there are also results raising questions about the reliability of FDG SPECT [56, 57]. Owing to the absence of photon attenuation correction in the majority of SPECT scanners, it is reported that different diagnostic criteria are required in the inferior wall for viability assessment [57]. However, FDG SPECT has one benefit over PET, namely, that it allows dual-isotope simultaneous acquisition (DISA). PET imaging uses only one photopeak (511 keV) high-energy photon, and thus simultaneous dual-tracer acquisition is impossible. DISA using FDG and 99mTc perfusion tracer allows simultaneous flow metabolism analysis with acceptable feasibility [58, 59].
11C-acetate: oxidative metabolism and metabolic reserve
The conceptual basis for viability assessment using 11C-acetate is fundamentally similar to that when using FDG, i.e. detecting the residual metabolism in viable tissue. Resting oxidative metabolism is known to be preserved in the viable myocardium [60]. By measuring this maintained oxidative metabolism, viable myocardium can be detected. One major advantage of 11C-acetate over FDG is its independence from the metabolic milieu. The disadvantage of 11C-acetate PET is its complexity of analysis. These issues have been briefly mentioned previously.
However, evaluation of oxidative metabolism only at rest may not clearly measure viability. Hata et al. studied 28 patients with CAD [61] and found significant overlap of the k mono value between viable and non-viable myocardium under resting conditions. In their study, viability was defined using wall motion recovery after revascularisation measured with echocardiography. In this case, an inotropic stress test, usually performed with low-dose dobutamine continuous infusion, is helpful. The overlap of k mono disappears when measured under low-dose dobutamine stress test conditions [61].
It is important to note that the parameters measured under the inotropic stress test and those measured under resting conditions are fundamentally different. Yoshinaga et al. compared dobutamine stress echocardiography, FDG uptake at rest, and oxidative metabolism measured with 11C acetate at rest and under dobutamine stress test [62]. In this complex study, they found that contractile reserve measured with dobutamine stress echocardiography is closely related to the oxidative metabolic response to inotropic stress measured with 11C-acetate PET. There was also a discrepancy between contractile reserve and FDG uptake. This result is important because it indicates that the difference in sensitivity/specificity for viability assessment between dobutamine echo and nuclear methods, especially FDG PET, may not depend on the methodology. These results indicate that there may be a fundamental difference because we are simply looking at different things. Dobutamine echo and dobutamine acetate PET evaluate dynamic response to inotropic stress. Inotropic stress simulates the condition after revascularisation, and thus a good response to inotropic stress assures functional recovery. On the other hand, FDG PET (and perhaps also rest/re-injection Tl uptake) looks at the static condition of myocardium to predict functional recovery. These are fundamentally different. It may be appropriate to call the inotropic stress test a “viability confirming test” and resting cell condition analysis such as FDG PET, a “viability prediction test”.
11C-palmitate
In ischaemic myocardium, use of fatty acids is diminished. Thus, early PET studies of ischaemic myocardium were focussed on FFA metabolism measurement using 11C-palmitate. However, mainly due to the relatively complex synthesis and data interpretation compared with those for other metabolic compounds such as FDG or 11C-acetate, 11C-palmitate is becoming a “lost tracer” for clinical investigation of ischaemia in practice. However, there have been some interesting studies using this tracer. Miyabe et al. reported combining 11C-acetate and 11C-palmitate for evaluation of chronic hypokinetic myocardium [63]. They showed that, in general, washout of 11C-acetate, which is an index of oxidative metabolism, is correlated with washout of 11C-palmitate, which is an index of FFA metabolism. However, when the analysis was limited to areas of low FFA metabolism, palmitate washout was similar between chronically hypokinetic areas and normokinetic areas even though the former showed higher oxidative metabolism. This may show uncoupling of FFA washout and oxidative metabolism in chronically damaged myocardium. However, owing to the small number of patients examined, their results must be interpreted with caution.
Clinical application for non-ischaemic heart diseases
For ischaemic heart disease, the major player in the disease pathophysiology is perfusion. Changes in metabolism are a consequence of the disease process and somewhat less important than changes in perfusion. The disease process is mainly regional, and regional differences are important for diagnosis.
In diseases which involve the myocardium more globally, such as heart failure, cardiomyopathy and diabetes, myocardial metabolism should play a more important role. These disease processes involve the myocardium as a whole, and thus the ability to perform quantitative measurement, which is a major advantage of PET over SPECT, is much more important than in regional analysis.
Heart failure and metabolism
It has been reported that myocardial fatty acid utilisation (MFAU), measured using 18F-FTHA, is significantly increased in congestive heart failure [64] and that this increased MFAU can be normalised with β-adrenoreceptor blockade [65]. A recent complex study using 11C-palmitate, 15O-water, 11C-acetate and 11C-glucose showed decreased MFAU and increased myocardial glucose metabolism in dilated cardiomyopathy (DCM) patients [66]. Morita et al. studied ten NYHA II–III patients and found that MRG and K 1 of glucose, which indicates the glucose transport ratio, were increased compared with the values in normal subjects [37]. These conflicting results have been due to the heterogeneity of patient populations. For example, the majority of patients in the studies that indicated increased MFAU [64, 65] had ischaemic cardiomyopathy. On the other hand, the two studies mentioned above that demonstrated increased glucose metabolism [37] and impairment of FFA metabolism [66] did not include ischaemic patients. The difficulty of measurement and differences in the tracer may also have contributed to the discrepancies in the results.
In any case, in non-ischaemic heart disease, especially in severe heart failure, some metabolic changes play key roles in determining patient prognosis and disease progression. There are several lines of evidence that indicate that metabolic intervention can help to improve LV function, mechanical efficiency in diabetes [67, 68] or DCM [69–71]. The improvement in LV function with long-term treatment with a β-adrenergic receptor antagonist was reported to be associated with a switch in myocardial metabolism away from FFA oxidation towards glucose metabolism [65].
Given these advances in metabolic intervention for clinical treatment of severe heart failure [72–74], the importance of evaluating myocardial metabolism will increase. The requirement for PET, which can measure not only regional but also global changes in metabolism in absolute units, in this field will increase.
Heart failure and cardiac efficiency
kmono, which is an index of myocardial oxidative metabolism, is closely related to the cardiac workload. Thus, usually, kmono is well correlated with rate–pressure product. However, in some cases this relationship between kmono and rate–pressure product is lost [75, 76]. Measurement of myocardial energy efficiency may help in understanding such abnormal metabolic conditions.
The concept of myocardial efficiency, in other words, coupling/uncoupling of myocardial workload and oxidative metabolism (Fig. 6), is usually analysed as the work metabolic index (WMI) calculated using the following equation [77, 78].
The concept of myocardial efficiency and the work metabolic index (WMI). The WMI was determined as the ratio of cardiac work (= product of stroke volume index, systolic blood pressure and heart rate) and metabolism. Increased metabolism without sufficient cardiac work makes the WMI smaller, indicating poor myocardial efficiency. The normal value for WMI has not yet been established, although many studies have reported the normal range to be around 5.0×106 (ml/m2×mmHg)
For oxidative metabolism, k mono (washout rate of acetate) is usually applied. A study using WMI as a marker of myocardial efficiency revealed that in DCM patients, not only oxidative metabolism but also WMI was significantly reduced compared with that in normal subjects [79]. An early study [77] showed that in DCM patients, oxidative metabolism was increased by dobutamine infusion; however, in contrast, metabolic efficiency was reduced with a decrease in systemic vascular resistance. This concept of myocardial efficiency is mainly applied for the evaluation of DCM or cardiac resynchronisation therapy, but it is also useful in ischaemic heart disease. The effect of β-blocker therapy has been measured with this approach not only in DCM patients but also in ischaemic cardiomyopathy patients [78]. Improvement of WMI was observed after metoprolol medication in both groups of patients, which means that the myocardium works equally well with less oxidative costs. These results indicate that WMI should be a very useful index for evaluating cardiac diseases and monitoring the effectiveness of therapeutic interventions.
Cardiac resynchronisation therapy and PET
Cardiac resynchronisation therapy (CRT) was proposed about 10 years ago as an adjunctive treatment for severe heart failure. Since then, a huge number of studies have demonstrated its efficacy and mechanism of action. Several recent PET studies have evaluated the effect of CRT on myocardial metabolism. A change in glucose metabolism has been observed after CRT: a study using FDG revealed that heterogeneous glucose metabolism in the left ventricular myocardium is rendered homogeneous by CRT [80]. The majority of PET metabolism studies on CRT have focussed on oxidative metabolism measured with 11C-acetate. It has been reported that CRT leads to responses in oxidative metabolism and metabolic reserve of the right ventricle [81], cardiac efficiency [82] and distribution of oxidative metabolism in the left ventricular wall [83].
It is well known that not all patients respond to CRT. Usually, to identify those patients likely to respond to CRT, electrocardiography (QRS length, etc.) or echocardiography (contraction, strain analysis, etc.) is performed. One recent report has shown that FDG PET is also useful to identify responders and predict outcomes in ischaemic cardiomyopathy patients [84]. Using FDG PET to quantify the extent of viable tissue, a close correlation between the number of viable segments and improvement in cardiac index was found. Similar results which suggested the usefulness of viability assessment for predicting response to CRT were also obtained in an FDG SPECT study [85]. Although these results were only demonstrated in patients with ischaemic cardiomyopathy, it is clear that PET metabolic imaging is useful for prediction and evaluation of the response to CRT.
Diabetes and other conditions
Early studies with FDG indicated that FDG PET imaging sometimes fails in severe diabetic patients. In some cases of diabetes with severe hyperglycaemia, FDG uptake in the myocardium was negative or minimal. This phenomenon is recognised as a limitation of FDG PET. According to recent advances in understanding myocardial metabolism, this abnormal metabolism in diabetic patients is an issue of concern.
Studies of animal models of diabetes mellitus have demonstrated up-regulation of fatty acid utilisation pathways in the myocardium [86]. Insulin-mediated glucose transport is also decreased in diabetic animal models [87]. These findings suggest that the heart becomes nearly solely dependent upon FFA metabolism in diabetes. However, little is known about the effect of diabetes mellitus on the human heart.
There are several types of conflicting evidence. One study found increased myocardial fatty acid utilisation (MFAU) and myocardial fatty acid oxidation (MFAO) in type 1 diabetes [88]. The negative relationship between plasma fatty acid level and MFAO which exists in normal myocardium was also found to be lost in type 1 diabetic hearts. On the other hand, studies from Finland suggested that, in patients with impaired glucose tolerance (IGT), clearance of 11C-palmitate, which is a index of β-oxidation of FFA, does not differ from that in normal subjects [89]. Uptake of 18F-FTHA in IGT patients was also found to be similar to that in normal subjects [90].
These discrepancies may be explained by differences in the method of analysis, the tracer used and the patient population. The inclusion criteria of the study by Herrero et al. [88], which showed increased MFAO and MFAU, were strictly set so that only patients with type 1 diabetes were included, and the age of the subjects was younger than that in other studies. Thus, these results may not be applicable to the type 2 diabetes or IGT patients. A study that measured myocardial fatty acid metabolism with 124I-heptadecanoic acid suggested that β-oxidation in the myocardium could differ between type 1 and type 2 diabetes mellitus, although no significant difference was detected [91].
Although there are many conflicting and inconclusive data about metabolism in the conditions mentioned above, non-invasive measurement should still be considered important because the ideal therapeutic intervention for these conditions will be non-invasive. There is also a growing body of evidence which suggests that marked changes in myocardial metabolism occur with other conditions such as obesity [92], insulin resistance and even simple aging [93]. However, this evidence has mainly been obtained in the rodent model or in isolated hearts, and little is known about human hearts. PET will provide a reliable way to study and diagnose these conditions.
Future prospects: positron metabolic tracers and their contribution to preventive medicine
In the near future, the major focus of cardiovascular medicine will move from intervention for acute/chronic coronary disease to primary/secondary prevention. Identifying the mild, perhaps global as well as regional, changes in coronary circulation and endothelial function which are already known to precede significant coronary disease will be required for such preventive cardiovascular medicine.
There is much evidence indicating that there is a relationship between plaque vulnerability and coronary events that is key to understanding and preventing acute coronary syndrome. Many tracers have been proposed for the diagnosis of plaque vulnerability. One promising way to diagnose vulnerability is detection of inflammation with FDG. Since Rudd et al. reported detection of carotid plaque vulnerability using FDG with strikingly beautiful PET/CT images [94], many studies have reported the usefulness of FDG PET for plaque diagnosis. A recent report showed that uptake of FDG in carotid plaque is closely related to plaque inflammation [95]. Even plaque reduction and stabilisation with lipid-lowering therapy could be detected in the carotid artery [96]. However, it is very hard to image these changes in the coronary artery with PET or even with PET/CT, primarily owing to the limited spatial resolution and high background activity in the myocardium adjacent to the coronary artery. Cardiac motion also causes deterioration in the image quality even with the ECG-gating technique.
One solution to these problems is the invasive catheter approach. A Japanese group developed a catheter-based intravascular radiation detector (IVRD) to measure FDG uptake in small coronary plaques [97, 98]. The IVRD is designed to detect mainly β, and not γ, rays in order to ignore high systemic and myocardial background activity (Fig. 7). The authors reported that low activity of 18F point sources could be correctly measured in a canine in vivo model. Although measurement of actual plaque activity in living organs has not yet been validated, a catheter-based technique is one possible solution for the detection of small vulnerable plaques. The future of this technique is not clear because of its invasiveness. The importance of and requirement for regional evaluation provided by invasive techniques like this should be discussed further, because atherosclerosis is not a regional process but involves the whole body.
a The IVRD system, consisting of a probe, an automatic pullback unit and a controller. b Using the IVRD system, small 18F activities placed on the surface of the canine femoral artery were detected. Measurement was repeated twice (blue and red lines), showing good reproducibility. (Reproduced from Hosokawa et al. [98], with permission from the Society of Nuclear Medicine)
Conclusions
PET provides reliable information on myocardial metabolism in a non-invasive and subject-friendly way. Early studies using PET mainly focussed on ischaemic heart disease. Although myocardial perfusion is the key issue of ischaemia, assessment of metabolism in the ischaemic myocardium has had a huge impact on our understanding of the pathophysiology and on therapeutic decision-making. Recent advances in cardiology have revealed that in diseases which involve the myocardium globally, such as heart failure and diabetes mellitus, myocardial metabolism plays an even more central role in disease development and treatment. By virtue of its ability to measure myocardial metabolism quantitatively, PET may become an increasingly valuable tool which serves to elucidate these conditions.
References
Sokoloff L, Reivich M, Kennedy C, Des Rosiers MH, Patlak CS, Pettigrew KD, et al. The [14C]deoxyglucose method for the measurement of local cerebral glucose utilization: theory, procedure, and normal values in the conscious and anesthetized albino rat. J Neurochem 1977;28:897–916.
Phelps ME, Huang SC, Hoffman EJ, Selin C, Sokoloff L, Kuhl DE. Tomographic measurement of local cerebral glucose metabolic rate in humans with (F-18)2-fluoro-2-deoxy-D-glucose: validation of method. Ann Neurol 1979;6:371–88.
Krivokapich J, Huang SC, Phelps ME, Barrio JR, Watanabe CR, Selin CE, et al. Estimation of rabbit myocardial metabolic rate for glucose using fluorodeoxyglucose. Am J Physiol 1982;243:H884–95.
Krivokapich J, Huang SC, Selin CE, Phelps ME. Fluorodeoxyglucose rate constants, lumped constant, and glucose metabolic rate in rabbit heart. Am J Physiol 1987;252:H777–87.
Gambhir SS, Schwaiger M, Huang SC, Krivokapich J, Schelbert HR, Nienaber CA, et al. Simple noninvasive quantification method for measuring myocardial glucose utilization in humans employing positron emission tomography and fluorine-18 deoxyglucose. J Nucl Med 1989;30:359–66.
Choi Y, Hawkins RA, Huang SC, Gambhir SS, Brunken RC, Phelps ME, et al. Parametric images of myocardial metabolic rate of glucose generated from dynamic cardiac PET and 2-[18F]fluoro-2-deoxy-d-glucose studies. J Nucl Med 1991;32:733–8.
Virtanen KA, Peltoniemi P, Marjamaki P, Asola M, Strindberg L, Parkkola R, et al. Human adipose tissue glucose uptake determined using [18F]-fluoro-deoxy-glucose ([18F]FDG) and PET in combination with microdialysis. Diabetologia 2001;44:2171–9.
Botker HE, Bottcher M, Schmitz O, Gee A, Hansen SB, Cold GE, et al. Glucose uptake and lumped constant variability in normal human hearts determined with [18F]fluorodeoxyglucose. J Nucl Cardiol 1997;4:125–32.
Tamaki N, Kawamoto M, Takahashi N, Yonekura Y, Magata Y, Torizuka T, et al. Assessment of myocardial fatty acid metabolism with positron emission tomography at rest and during dobutamine infusion in patients with coronary artery disease. Am Heart J 1993;125:702–10.
Bergmann SR, Weinheimer CJ, Markham J, Herrero P. Quantitation of myocardial fatty acid metabolism using PET. J Nucl Med 1996;37:1723–30.
Schon HR, Schelbert HR, Robinson G, Najafi A, Huang SC, Hansen H, et al. C-11 labeled palmitic acid for the noninvasive evaluation of regional myocardial fatty acid metabolism with positron-computed tomography. I. Kinetics of C-11 palmitic acid in normal myocardium. Am Heart J 1982;103:532–47.
DeGrado TR, Coenen HH, Stocklin G. 14(R,S)-[18F]fluoro-6-thia-heptadecanoic acid (FTHA): evaluation in mouse of a new probe of myocardial utilization of long chain fatty acids. J Nucl Med 1991;32:1888–96.
Ebert A, Herzog H, Stocklin GL, Henrich MM, DeGrado TR, Coenen HH, et al. Kinetics of 14(R,S)-fluorine-18-fluoro-6-thia-heptadecanoic acid in normal human hearts at rest, during exercise and after dipyridamole injection. J Nucl Med 1994;35:51–6.
Altehoefer C, vom Dahl J, Bares R, Stocklin GL, Bull U. Metabolic mismatch of septal beta-oxidation and glucose utilization in left bundle branch block assessed with PET. J Nucl Med 1995;36:2056–9.
Takala TO, Nuutila P, Pulkki K, Oikonen V, Gronroos T, Savunen T, et al. 14(R,S)-[18F]Fluoro-6-thia-heptadecanoic acid as a tracer of free fatty acid uptake and oxidation in myocardium and skeletal muscle. Eur J Nucl Med Mol Imaging 2002;29:1617–22.
Degrado TR, Kitapci MT, Wang S, Ying J, Lopaschuk GD. Validation of 18F-fluoro-4-thia-palmitate as a PET probe for myocardial fatty acid oxidation: effects of hypoxia and composition of exogenous fatty acids. J Nucl Med 2006;47:173–81.
DeGrado TR, Wang S, Rockey DC. Preliminary evaluation of 15-[18F]fluoro-3-oxa-pentadecanoate as a PET tracer of hepatic fatty acid oxidation. J Nucl Med 2000;41:1727–36.
Shoup TM, Elmaleh DR, Bonab AA, Fischman AJ. Evaluation of trans-9-18F-fluoro-3,4-methyleneheptadecanoic acid as a PET tracer for myocardial fatty acid imaging. J Nucl Med 2005;46:297–304.
Renstrom B, Rommelfanger S, Stone CK, DeGrado TR, Carlson KJ, Scarbrough E, et al. Comparison of fatty acid tracers FTHA and BMIPP during myocardial ischemia and hypoxia. J Nucl Med 1998;39:1684–9.
Brown M, Marshall DR, Sobel BE, Bergmann SR. Delineation of myocardial oxygen utilization with carbon-11-labeled acetate. Circulation 1987;76:687–96.
Tamaki N, Magata Y, Takahashi N, Kawamoto M, Torizuka T, Yonekura Y, et al. Myocardial oxidative metabolism in normal subjects in fasting, glucose loading and dobutamine infusion states. Ann Nucl Med 1992;6:221–8.
Armbrecht JJ, Buxton DB, Schelbert HR. Validation of [1-11C]acetate as a tracer for noninvasive assessment of oxidative metabolism with positron emission tomography in normal, ischemic, postischemic, and hyperemic canine myocardium. Circulation. 1990;81:1594–605.
Gropler RJ, Siegel BA, Geltman EM. Myocardial uptake of carbon-11-acetate as an indirect estimate of regional myocardial blood flow. J Nucl Med 1991;32:245–51.
Sciacca RR, Akinboboye O, Chou RL, Epstein S, Bergmann SR. Measurement of myocardial blood flow with PET using 1-11C-acetate. J Nucl Med 2001;42:63–70.
Sun KT, Yeatman LA, Buxton DB, Chen K, Johnson JA, Huang SC, et al. Simultaneous measurement of myocardial oxygen consumption and blood flow using [1-carbon-11]acetate. J Nucl Med 1998;39:272–80.
van den Hoff J, Burchert W, Borner AR, Fricke H, Kuhnel G, Meyer GJ, et al. [1-11C]Acetate as a quantitative perfusion tracer in myocardial PET. J Nucl Med 2001;42:1174–82.
Feng B, Pretorius PH, Farncombe TH, Dahlberg ST, Narayanan MV, Wernick MN, et al. Simultaneous assessment of cardiac perfusion and function using 5-dimensional imaging with Tc-99m teboroxime. J Nucl Cardiol 2006;13:354–61.
Porenta G, Cherry S, Czernin J, Brunken R, Kuhle W, Hashimoto T, et al. Noninvasive determination of myocardial blood flow, oxygen consumption and efficiency in normal humans by carbon-11 acetate positron emission tomography imaging. Eur J Nucl Med 1999;26:1465–74.
Tillisch J, Brunken R, Marshall R, Schwaiger M, Mandelkern M, Phelps M, et al. Reversibility of cardiac wall-motion abnormalities predicted by positron tomography. N Engl J Med 1986;314:884–8.
de Groot M, Meeuwis AP, Kok PJ, Corstens FH, Oyen WJ. Influence of blood glucose level, age and fasting period on non-pathological FDG uptake in heart and gut. Eur J Nucl Med Mol Imaging 2005;32:98–101.
Kaneta T, Hakamatsuka T, Takanami K, Yamada T, Takase K, Sato A, et al. Evaluation of the relationship between physiological FDG uptake in the heart and age, blood glucose level, fasting period, and hospitalization. Ann Nucl Med 2006;20:203–8.
Gropler RJ, Siegel BA, Lee KJ, Moerlein SM, Perry DJ, Bergmann SR, et al. Nonuniformity in myocardial accumulation of fluorine-18-fluorodeoxyglucose in normal fasted humans. J Nucl Med 1990;31:1749–56.
Hicks RJ, Herman WH, Kalff V, Molina E, Wolfe ER, Hutchins G, et al. Quantitative evaluation of regional substrate metabolism in the human heart by positron emission tomography. J Am Coll Cardiol 1991;18:101–11.
Pagano D, Lewis ME, Townend JN, Davies P, Camici PG, Bonser RS. Coronary revascularisation for postischaemic heart failure: how myocardial viability affects survival. Heart 1999;82:684–8.
Bax JJ, Fath-Ordoubadi F, Boersma E, Wijns W, Camici PG. Accuracy of PET in predicting functional recovery after revascularisation in patients with chronic ischaemic dysfunction: head-to-head comparison between blood flow, glucose utilisation and water-perfusable tissue fraction. Eur J Nucl Med Mol Imaging 2002;29:721–7.
Knuuti MJ, Nuutila P, Ruotsalainen U, Teras M, Saraste M, Harkonen R, et al. The value of quantitative analysis of glucose utilization in detection of myocardial viability by PET. J Nucl Med 1993;34:2068–75.
Morita K, Katoh C, Yoshinaga K, Noriyasu K, Mabuchi M, Tsukamoto T, et al. Quantitative analysis of myocardial glucose utilization in patients with left ventricular dysfunction by means of 18F-FDG dynamic positron tomography and three-compartment analysis. Eur J Nucl Med Mol Imaging. 2005;32:806–12.
Baer FM, Voth E, Deutsch HJ, Schneider CA, Horst M, de Vivie ER, et al. Predictive value of low dose dobutamine transesophageal echocardiography and fluorine-18 fluorodeoxyglucose positron emission tomography for recovery of regional left ventricular function after successful revascularization. J Am Coll Cardiol 1996;28:60–9.
Bax JJ, Visser FC, Elhendy A, Poldermans D, Cornel JH, van Lingen A, et al. Prediction of improvement of regional left ventricular function after revascularization using different perfusion-metabolism criteria. J Nucl Med 1999;40:1866–73.
Underwood SR, Bax JJ, vom Dahl J, Henein MY, Knuuti J, van Rossum AC, et al. Imaging techniques for the assessment of myocardial hibernation. Report of a Study Group of the European Society of Cardiology. Eur Heart J 2004;25:815–36.
Bax JJ, Wijns W, Cornel JH, Visser FC, Boersma E, Fioretti PM. Accuracy of currently available techniques for prediction of functional recovery after revascularization in patients with left ventricular dysfunction due to chronic coronary artery disease: comparison of pooled data. J Am Coll Cardiol 1997;30:1451–60.
Barrington SF, Chambers J, Hallett WA, O’Doherty MJ, Roxburgh JC, Nunan TO. Comparison of sestamibi, thallium, echocardiography and PET for the detection of hibernating myocardium. Eur J Nucl Med Mol Imaging 2004;31:355–61.
Siebelink HM, Blanksma PK, Crijns HJ, Bax JJ, van Boven AJ, Kingma T, et al. No difference in cardiac event-free survival between positron emission tomography-guided and single-photon emission computed tomography-guided patient management: a prospective, randomized comparison of patients with suspicion of jeopardized myocardium. J Am Coll Cardiol 2001;37:81–8.
Knuuti J, Schelbert HR, Bax JJ. The need for standardisation of cardiac FDG PET imaging in the evaluation of myocardial viability in patients with chronic ischaemic left ventricular dysfunction. Eur J Nucl Med Mol Imaging 2002;29:1257–66.
Bacharach SL, Bax JJ, Case J, Delbeke D, Kurdziel KA, Martin WH, et al. American Society of Nuclear Cardiology practice guidelines. J Nucl Cardiol 2003;10:543–56.
Schelbert HR, Beanlands R, Bengel F, Knuuti J, DiCarli M, Machac J, et al. PET myocardial perfusion and glucose metabolism imaging: part 2—guidelines for interpretation and reporting. J Nucl Cardiol 2003;10:557–71.
Schaefer WM, Lipke CS, Nowak B, Kaiser HJ, Buecker A, Krombach GA, et al. Validation of an evaluation routine for left ventricular volumes, ejection fraction and wall motion from gated cardiac FDG PET: a comparison with cardiac magnetic resonance imaging. Eur J Nucl Med Mol Imaging 2003;30:545–53.
Saab G, Dekemp RA, Ukkonen H, Ruddy TD, Germano G, Beanlands RS. Gated fluorine 18 fluorodeoxyglucose positron emission tomography: determination of global and regional left ventricular function and myocardial tissue characterization. J Nucl Cardiol 2003;10:297–303.
Santana CA, Shaw LJ, Garcia EV, Soler-Peter M, Candell-Riera J, Grossman GB, et al. Incremental prognostic value of left ventricular function by myocardial ECG-gated FDG PET imaging in patients with ischemic cardiomyopathy. J Nucl Cardiol 2004;11:542–50.
Slart RH, Bax JJ, van Veldhuisen DJ, van der Wall EE, Dierckx RA, de Boer J, et al. Prediction of functional recovery after revascularization in patients with coronary artery disease and left ventricular dysfunction by gated FDG-PET. J Nucl Cardiol 2006;13:210–9.
Yamakawa Y, Takahashi N, Ishikawa T, Uchino K, Mochida Y, Ebina T, et al. Clinical usefulness of ECG-gated 18F-FDG PET combined with 99mTc-MIBI gated SPECT for evaluating myocardial viability and function. Ann Nucl Med 2004;18:375–83.
Bax JJ, Visser FC, van Lingen A, Huitink JM, Kamp O, van Leeuwen GR, et al. Feasibility of assessing regional myocardial uptake of 18F-fluorodeoxyglucose using single photon emission computed tomography. Eur Heart J 1993;14:1675–82.
Drane WE, Abbott FD, Nicole MW, Mastin ST, Kuperus JH. Technology for FDG SPECT with a relatively inexpensive gamma camera. Work in progress. Radiology 1994;191:461–5.
Burt RW, Perkins OW, Oppenheim BE, Schauwecker DS, Stein L, Wellman HN, et al. Direct comparison of fluorine-18-FDG SPECT, fluorine-18-FDG PET and rest thallium-201 SPECT for detection of myocardial viability. J Nucl Med 1995;36:176–9.
Bax JJ, Cornel JH, Visser FC, Fioretti PM, van Lingen A, Huitink JM, et al. Prediction of improvement of contractile function in patients with ischemic ventricular dysfunction after revascularization by fluorine-18 fluorodeoxyglucose single-photon emission computed tomography. J Am Coll Cardiol 1997;30:377–83.
Chen EQ, MacIntyre WJ, Go RT, Brunken RC, Saha GB, Wong CY, et al. Myocardial viability studies using fluorine-18-FDG SPECT: a comparison with fluorine-18-FDG PET. J Nucl Med 1997;38:582–6.
Mabuchi M, Kubo N, Morita K, Noriyasu K, Itoh Y, Katoh C, et al. Value and limitation of myocardial fluorodeoxyglucose single photon emission computed tomography using ultra-high energy collimators for assessing myocardial viability. Nucl Med Commun 2002;23:879–85.
Fukuchi K, Katafuchi T, Fukushima K, Shimotsu Y, Toba M, Hayashida K, et al. Estimation of myocardial perfusion and viability using simultaneous 99mTc-tetrofosmin-FDG collimated SPECT. J Nucl Med 2000;41:1318–23.
Matsunari I, Kanayama S, Yoneyama T, Matsudaira M, Nakajima K, Taki J, et al. Electrocardiographic-gated dual-isotope simultaneous acquisition SPECT using 18F-FDG and 99mTc-sestamibi to assess myocardial viability and function in a single study. Eur J Nucl Med Mol Imaging 2005;32:195–202.
Gropler RJ, Geltman EM, Sampathkumaran K, Perez JE, Moerlein SM, Sobel BE, et al. Functional recovery after coronary revascularization for chronic coronary artery disease is dependent on maintenance of oxidative metabolism. J Am Coll Cardiol 1992;20:569–77.
Hata T, Nohara R, Fujita M, Hosokawa R, Lee L, Kudo T, et al. Noninvasive assessment of myocardial viability by positron emission tomography with 11C acetate in patients with old myocardial infarction. Usefulness of low-dose dobutamine infusion. Circulation 1996;94:1834–41.
Yoshinaga K, Katoh C, Beanlands RS, Noriyasu K, Komuro K, Yamada S, et al. Reduced oxidative metabolic response in dysfunctional myocardium with preserved glucose metabolism but with impaired contractile reserve. J Nucl Med 2004;45:1885–91.
Miyabe H, Ohte N, Iida A, Narita H, Yoshida T, Kimura G. Evaluation of fatty acid beta-oxidation in patients with prior myocardial infarction in relation to myocardial blood flow, total oxidative metabolism, and left ventricular wall motion. Circ J 2005;69:1459–65.
Taylor M, Wallhaus TR, Degrado TR, Russell DC, Stanko P, Nickles RJ, et al. An evaluation of myocardial fatty acid and glucose uptake using PET with [18F]fluoro-6-thia-heptadecanoic acid and [18F]FDG in patients with congestive heart failure. J Nucl Med 2001;42:55–62.
Wallhaus TR, Taylor M, DeGrado TR, Russell DC, Stanko P, Nickles RJ, et al. Myocardial free fatty acid and glucose use after carvedilol treatment in patients with congestive heart failure. Circulation 2001;103:2441–6.
Davila-Roman VG, Vedala G, Herrero P, de las Fuentes L, Rogers JG, Kelly DP, et al. Altered myocardial fatty acid and glucose metabolism in idiopathic dilated cardiomyopathy. J Am Coll Cardiol 2002;40:271–7.
Rosano GM, Vitale C, Sposato B, Mercuro G, Fini M. Trimetazidine improves left ventricular function in diabetic patients with coronary artery disease: a double-blind placebo-controlled study. Cardiovasc Diabetol 2003;2:16.
Rosano GM, Vitale C, Fragasso G. Metabolic therapy for patients with diabetes mellitus and coronary artery disease. Am J Cardiol 2006;98:14J–18J.
Di Napoli P, Taccardi AA, Barsotti A. Long term cardioprotective action of trimetazidine and potential effect on the inflammatory process in patients with ischaemic dilated cardiomyopathy. Heart 2005;91:161–5.
Schmidt-Schweda S, Holubarsch C. First clinical trial with etomoxir in patients with chronic congestive heart failure. Clin Sci (Lond) 2000;99:27–35.
Lee L, Campbell R, Scheuermann-Freestone M, Taylor R, Gunaruwan P, Williams L, et al. Metabolic modulation with perhexiline in chronic heart failure: a randomized, controlled trial of short-term use of a novel treatment. Circulation 2005;112:3280–8.
Morrow DA, Givertz MM. Modulation of myocardial energetics: emerging evidence for a therapeutic target in cardiovascular disease. Circulation 2005;112:3218–21.
Lopaschuk GD. Optimizing cardiac fatty acid and glucose metabolism as an approach to treating heart failure. Semin Cardiothorac Vasc Anesth 2006;10:228–30.
Tuunanen H, Engblom E, Naum A, Nagren K, Hesse B, Airaksinen KE, et al. Free fatty acid depletion acutely decreases cardiac work and efficiency in cardiomyopathic heart failure. Circulation 2006;114:2130–7.
Torizuka T, Tamaki N, Kasagi K, Misaki T, Kawamoto M, Tadamura E, et al. Myocardial oxidative metabolism in hyperthyroid patients assessed by PET with carbon-11-acetate. J Nucl Med 1995;36:1981–6.
Hattori N, Tamaki N, Kudoh T, Masuda I, Magata Y, Kitano H, et al. Abnormality of myocardial oxidative metabolism in noninsulin-dependent diabetes mellitus. J Nucl Med 1998;39:1835–40.
Beanlands RS, Bach DS, Raylman R, Armstrong WF, Wilson V, Montieth M, et al. Acute effects of dobutamine on myocardial oxygen consumption and cardiac efficiency measured using carbon-11 acetate kinetics in patients with dilated cardiomyopathy. J Am Coll Cardiol 1993;22:1389–98.
Beanlands RS, Nahmias C, Gordon E, Coates G, deKemp R, Firnau G, et al. The effects of beta(1)-blockade on oxidative metabolism and the metabolic cost of ventricular work in patients with left ventricular dysfunction: a double-blind, placebo-controlled, positron-emission tomography study. Circulation 2000;102:2070–5.
Bengel FM, Permanetter B, Ungerer M, Nekolla S, Schwaiger M. Non-invasive estimation of myocardial efficiency using positron emission tomography and carbon-11 acetate-comparison between the normal and failing human heart. Eur J Nucl Med 2000;27:319–26.
Nowak B, Sinha AM, Schaefer WM, Koch KC, Kaiser HJ, Hanrath P, et al. Cardiac resynchronization therapy homogenizes myocardial glucose metabolism and perfusion in dilated cardiomyopathy and left bundle branch block. J Am Coll Cardiol 2003;41:1523–8.
Knuuti J, Sundell J, Naum A, Engblom E, Koistinen J, Ylitalo A, et al. Assessment of right ventricular oxidative metabolism by PET in patients with idiopathic dilated cardiomyopathy undergoing cardiac resynchronization therapy. Eur J Nucl Med Mol Imaging 2004;31:1592–8.
Lindner O, Sorensen J, Vogt J, Fricke E, Baller D, Horstkotte D, et al. Cardiac efficiency and oxygen consumption measured with 11C-acetate PET after long-term cardiac resynchronization therapy. J Nucl Med 2006;47:378–83.
Lindner O, Vogt J, Kammeier A, Fricke E, Holzinger J, Lamp B, et al. Cardiac re-synchronization therapy: effects on myocardial perfusion at rest, after vasodilation and oxygen consumption. Nuklearmedizin 2006;45:10–14.
van Campen CM, Visser FC, van der Weerdt AP, Knaapen P, Comans EF, Lammertsma AA, et al. FDG PET as a predictor of response to resynchronisation therapy in patients with ischaemic cardiomyopathy. Eur J Nucl Med Mol Imaging 2007;34:309–15.
Ypenburg C, Schalij MJ, Bleeker GB, Steendijk P, Boersma E, Dibbets-Schneider P, et al. Extent of viability to predict response to cardiac resynchronization therapy in ischemic heart failure patients. J Nucl Med 2006;47:1565–70.
Belke DD, Larsen TS, Gibbs EM, Severson DL. Altered metabolism causes cardiac dysfunction in perfused hearts from diabetic (db/db) mice. Am J Physiol Endocrinol Metab 2000;279:E1104–13.
Li SH, McNeill JH. In vivo effects of vanadium on GLUT4 translocation in cardiac tissue of STZ-diabetic rats. Mol Cell Biochem 2001;217:121–9.
Herrero P, Peterson LR, McGill JB, Matthew S, Lesniak D, Dence C, et al. Increased myocardial fatty acid metabolism in patients with type 1 diabetes mellitus. J Am Coll Cardiol 2006;47:598–604.
Knuuti J, Takala TO, Nagren K, Sipila H, Turpeinen AK, Uusitupa MI, et al. Myocardial fatty acid oxidation in patients with impaired glucose tolerance. Diabetologia 2001;44:184–7.
Turpeinen AK, Takala TO, Nuutila P, Axelin T, Luotolahti M, Haaparanta M, et al. Impaired free fatty acid uptake in skeletal muscle but not in myocardium in patients with impaired glucose tolerance: studies with PET and 14(R,S)-[18F]fluoro-6-thia-heptadecanoic acid. Diabetes 1999;48:1245–50.
Turpeinen AK, Kuikka JT, Vanninen E, Uusitupa MI. Abnormal myocardial kinetics of 123I-heptadecanoic acid in subjects with impaired glucose tolerance. Diabetologia 1997;40:541–9.
Coort SL, Bonen A, van der Vusse GJ, Glatz JF, Luiken JJ. Cardiac substrate uptake and metabolism in obesity and type-2 diabetes: role of sarcolemmal substrate transporters. Mol Cell Biochem 2006 Sep 19; [Epub ahead of print].
McMillin JB, Taffet GE, Taegtmeyer H, Hudson EK, Tate CA. Mitochondrial metabolism and substrate competition in the aging Fischer rat heart. Cardiovasc Res 1993;27:2222–8.
Rudd JH, Warburton EA, Fryer TD, Jones HA, Clark JC, Antoun N, et al. Imaging atherosclerotic plaque inflammation with [18F]-fluorodeoxyglucose positron emission tomography. Circulation. 2002;105:2708–11.
Tawakol A, Migrino RQ, Bashian GG, Bedri S, Vermylen D, Cury RC, et al. In vivo 18F-fluorodeoxyglucose positron emission tomography imaging provides a noninvasive measure of carotid plaque inflammation in patients. J Am Coll Cardiol 2006;48:1818–24.
Tahara N, Kai H, Ishibashi M, Nakaura H, Kaida H, Baba K, et al. Simvastatin attenuates plaque inflammation: evaluation by fluorodeoxyglucose positron emission tomography. J Am Coll Cardiol 2006;48:1825–31.
Mukai T, Nohara R, Ogawa M, Ishino S, Kambara N, Kataoka K, et al. A catheter-based radiation detector for endovascular detection of atheromatous plaques. Eur J Nucl Med Mol Imaging 2004;31:1299–303.
Hosokawa R, Kambara N, Ohba M, Mukai T, Ogawa M, Motomura H, et al. A catheter-based intravascular radiation detector of vulnerable plaques. J Nucl Med 2006;47:863–7.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kudo, T. Metabolic imaging using PET. Eur J Nucl Med Mol Imaging 34 (Suppl 1), 49–61 (2007). https://doi.org/10.1007/s00259-007-0440-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00259-007-0440-3