Abstract
In the past decade, there have been major improvements in our understanding of angiogenesis at the genetic, molecular and cellular levels. Concentrated efforts in this area have led to new therapeutic approaches to ischaemic heart disease using angiogenic factors, gene therapy and progenitor cells. Despite very promising experimental results in animal studies, large clinical trials have failed to confirm the results in patients with coronary artery disease. Important questions such as selection of growth factors and donor cells, as well as the timing, dose and route of administration, have been raised and need to be answered. Molecular imaging approaches which may provide specific markers of the angiogenic process (e.g. integrin expression in endothelial cells) have been introduced and are expected to address some of these questions. Although few clinical imaging results are currently available, animal studies suggest the potential role of molecular imaging for characterisation of the angiogenetic process in vivo and for the monitoring of therapeutic effects.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Myocardial ischaemia causes reversible or irreversible myocardial injury and may lead to heart failure due to extensive myocardial necrosis, hibernation and ventricular remodelling. At the same time, ischaemia triggers the formation of collateral vessels via angiogenesis, but this endogenous compensation may not be sufficient in advanced disease [1]. Recent advances in our understanding of angiogenesis with regard to molecular, genetic and cellular mechanisms offer the potential for therapeutic angiogenesis [2, 3]. Several angiogenic strategies, including cytokine therapies, gene therapies and cell transplantation therapies, have been examined, and animal studies have indicated enhanced angiogenesis [4–7]. Based on these animal experiments, clinical studies have been initiated and the first results of large clinical trials with recombinant proteins and gene therapies have been published [8–11]. However, the results have been variable and have raised many methodological questions, including details of the therapeutic strategy (e.g. timing, dose and route) and the use of appropriate end-points [12, 13].
Non-invasive imaging techniques are promising tools to address these unsolved questions. Assessments of myocardial perfusion and left ventricular function by means of SPECT, PET, MRI or echocardiography are important validated methods to explore the therapeutic efficacy of angiogenesis [12]. Furthermore, recent developments in molecular imaging techniques may offer more specific visualisation of therapeutic targets and provide early markers of the angiogenic process [14].
Mechanism of angiogenesis in ischaemic heart disease
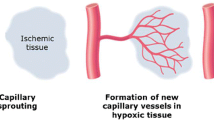
Three different subtypes of neovascularisation are described: angiogenesis, arteriogenesis and vasculogenesis [15–17]. Angiogenesis is a process fundamental to neovascularisation stimulated by inflammation and ischaemia. The general definition of angiogenesis is the growth and development of new capillary blood vessels from pre-existing vasculature involving mature endothelial cells [17]. The process consists of an early sprouting phase followed by an introspective phase. However, the new capillaries generated via angiogenesis lack a complete medial layer, which causes abnormal permeability and vasomotor functions [17].
Arteriogenesis is the maturation of capillary vessels into fully developed vessels equipped with smooth muscle cells in the tunica media [17, 18]. In contrast to angiogenesis, arteriogenesis occurs independently of hypoxia and is typically observed outside of ischaemic regions. The stimulus for arteriogenesis is thought to be increased shear stress [19]. Arteriogenesis is important for the development of large collateral vessels and represents the target of neovascularisation therapies.
Vasculogenesis represents the formation of new capillaries during embryonic development [17, 20, 21]. This process is characterised by the differentiation of endothelial cells from cellular precursors.
Recently, experimental studies have suggested the presence of circulating endothelial progenitor cells in the postnatal phase and their incorporation into newly formed vessels. This interesting concept represents the combination of angiogenesis and vasculogenesis contributing to neovascularisation of adult tissue in response to an angiogenic stimulus such as ischaemia [21, 22].
Angiogenesis involves a complex interplay of many molecules and cells, as well as the extracellular matrix. First, the basement membrane undergoes disintegration, which is facilitated by urokinase-type plasminogen activator (u-PA) and matrix metalloproteinases (MMPs) released from activated inflammatory cells; this allows endothelial cell migration and results in the liberation of growth factors [23, 24]. Second, migration and proliferation of endothelial cells are promoted by angiogenic factors such as vascular endothelial growth factor (VGEF) and basic fibroblast growth factor (bFGF), which are released from endothelial cells and inflammatory cells [25]. Tube formation of endothelial cells and the reconstruction of the basement membrane are the final steps in angiogenesis, and are mainly modulated by signalling transduction between the extracellular matrix and endothelial cells mediated by integrins, which are expressed by the endothelial cells [26].
Tissue hypoxia is a strong initiator of angiogenesis in the setting of ischaemia. As an acute local reaction, vasodilation to increase blood flow as a means to increase oxygen delivery is observed. But further compensatory processes such as angiogenesis involve changes in gene transcription [27]. The transcription factors, the heterodimeric hypoxia-inducible factors (HIFs), are known to play a key role in modulating expression of hypoxia-sensitive genes, including VGEFs, VGEF receptors, bFGFs, nitric oxide synthase (NOS) and angiopoietin genes [27–29]. In normally oxygenated tissue, HIFs are downregulated by ubiquitination and proteasomal degradation, but are rapidly activated in hypoxic conditions and bind to promoter elements, inducing transcription of hypoxia-sensitive genes. Once reoxygenation has occurred, HIFs again undergo degradation, and the transcription activation is downregulated [28] (Fig. 1).
Steps in angiogenesis, and a part of the mechanism of angiogenesis induced by hypoxia (see text). Angiogenesis consists of degradation of the basement membrane (a), activation of endothelial cells (b) and endothelial cell migration, and proliferation and synthesis of a new basement membrane (c). Hypoxia induces multiple angiogenic factors, including vascular endothelial growth factor (VEGF), via activation of hypoxia-inducible factors (HIFs). These angiogenic factors enhance the angiogenesis sequence. Inflammatory cells and endothelial progenitor cells (EPCs) derived from bone marrow are involved in angiogenesis
Another important stimulus for angiogenesis appears to be the inflammatory processes which are observed in ischaemic tissues. The presence of inflammatory cells such as monocytes, macrophages, platelets and mast cells is associated with local secretion of angiogenic factors including several cytokines, growth factors and proteinases [30]. Among these factors, PR39 and interleukin-1 are reported to enhance HIF activities [31, 32].
In general, angiogenesis is well regulated by a number of stimulatory and inhibitory factors. Activators include vascular growth factors, some cytokines, extracellular matrix macromolecules, cell adhesion molecules and others (Table 1) [33]. Endothelial cells and macrophages produce most of these factors. On the other hand, other cytokines (e.g. interferon α and interleukin-12), steroids (e.g. medroxyprogesterone acetate and cortisone), heparin binding factors (e.g. protamine, platelet factor IV and VEGF receptor antagonist), protease inhibitors and antibiotic substances are reported to inhibit angiogenesis [34, 35].
Among these numerous modulators of angiogenesis, VEGF is one of the most important and potent stimulators of endothelial cell activation and proliferation [15, 36]. VEGF is a homodimeric protein belonging to the cystine knot growth factor family. Several isoforms exist (VEGF 121, 145, 165, 189 and 206), derived from splicing of a single gene [37]. These isoforms differ in their binding affinity to heparin and to receptors. Two distinct receptor tyrosine kinases have been identified as VEGF receptor-1 (Flt-1) and VEGF receptor-2 (KDR), expressed on the surface of endothelial cells [38]. These two receptors share approximately 44% amino acid homology, but have been suggested to have distinct biological roles [36, 39]. VEGF receptor-1 is the major mediator of endothelial cell proliferation and survival in angiogenesis. In contrast, VEGF receptor-2 does not mediate mitotic activity of endothelial cells, but is necessary for organisation of the vascular system during early embryonic development [36, 37]. As described above, VEGF and VEGF receptor gene expression is induced by hypoxia, as well as by other growth factors and cytokines, and mediated through the activation of HIF expression [40–43].
The extracellular matrix is another well-known key factor that regulates angiogenesis by controlling mobilisation of cells and storage of growth factors [44]. In addition, signal transduction between the extracellular matrix and endothelial cells is an important factor regulating cell migration, proliferation and survival. The integrin superfamily, which is characterised by a heterodimeric receptor with α and β subunits, plays an important role in endothelial cell attachment and signal transduction [45]. The presence of 18 different α subunits, nine different β subunits and 24 different combinations of α and β subunits has been reported for the integrin family [46]. Endothelial cells express eight different integrins depending on the location and activations [46]. Integrin αvβ3, αvβ5 and α2β1 are barely detectable in the quiescent state, but are upregulated in angiogenic endothelial cells [47]. α5β1, α1β1 and α3β1 are expressed at low levels in the quiescent state, and α5β1 shows increased expression in the angiogenic state [48, 49]. Integrins recognise specific extracellular matrix ligands necessary for migration and other molecules such as the arginine-glycine-asparagine (RGD) sequence [50, 51] (Table 2).
During recent years, αvβ3 integrin has been well studied. The crystal structure of αvβ3 integrin demonstrates binding of the RGD sequence with the extracellular structure of both αv and β3 subunits [52, 53]. Blockage of αvβ3 integrin by antibody or peptide antagonists has prevented blood vessel formation in a variety of animal experiments [54–56]. Anti-αvβ3 integrin antibody is reported to block bFGF-induced angiogenesis and to inhibit up to 50% of VEGF-induced angiogenesis [55]. These data clearly indicate the fundamental role of the integrins in angiogenesis. Via the RGD sequence, αvβ3 integrins seem to mediate adhesion of endothelial cells to extracellular matrix molecules and enhance endothelial cell proliferation, migration and tube formation [49]. In addition to their RGD-dependent action, αvβ3 integrins are reported to bind to VEGF, bFGF, VEGF receptors and insulin receptors, to promote angiogenesis. Inhibitors have also been identified which directly bind to αvβ3 integrin, including thrombospondin, MMPs and tumstatin [49, 57, 58]. Although the exact interactions have not yet been defined, these data suggest an important and complex role for integrin αvβ3 expression in regulating angiogenesis.
Therapeutic myocardial angiogenesis in ischaemic heart disease
Advances in the understanding of angiogenesis mechanisms have led to the development of new angiogenesis therapies for ischaemic heart disease. Administration of growth factors such as FGF, VEGF, hepatocyte growth factors and platelet-derived growth factors, as recombinant proteins or as the gene encoding these proteins, has been reported to increase capillary density and collateral vessels in various animal models with ischaemia [4, 5, 7, 59, 60]. Several routes—intravenous, intracoronary, intramyocardial and intrapericardial injection—have been developed to deliver the angiogenic substances to the heart. Based on successful observations in animal studies, clinical trials have been initiated. One of the first reports of clinical therapeutic angiogenesis was a randomised study of 40 patients using intramyocardial injection of recombinant FGF during bypass surgery [61]. The study showed successful enhancement of angiogenesis, as demonstrated by angiography, in the FGF-injected patients compared with control patients. In addition, continuous improvement of the left ventricular ejection fraction was observed in the FGF group at long-term (3 years) follow-up [62]. Several other phase-1 clinical studies with recombinant proteins and gene therapies for angiogenesis, mainly with FGF and VEGF, have followed and have yielded similarly promising results regarding improvements in symptoms and perfusion.
However, the results of subsequent large randomised placebo-controlled trials are inconsistent (Table 3). The VIVA (Vascular Growth Factor in Ischemia for Vascular Angiogenesis) trial was a prospective, randomised, placebo-controlled study to evaluate a single intracoronary VEGF-1 protein administration followed by three intravenous doses in 178 patients with reversible SPECT perfusion defects [9]. There were no significant improvements in exercise time and angina scores at 60 days. Although there was a significant reduction in angina symptoms in the highest dose group, no objective improvements in perfusion were observed on SPECT and angiography at up to 1 year of follow-up. FIRST (FGF-2 Initiating Revascularization Support Trial) was another study with intracoronary infusion of FGF-2 protein at three different randomised doses, as well as a placebo, in 337 patients with chronic angina [8]. There were no significant differences in exercise time and regional perfusion as assessed by SPECT after 90 days.
In the case of the gene delivery approach, the AGENT (angiogenic GENe Therapy) trial randomised 79 patients with chronic stable ischaemic heart disease to receive intracoronary injections of adenovirus vector containing the FGF-4 gene or placebo [10]. There were no significant improvements in exercise treadmill testing with FGF-4 treatment after 4 and 12 weeks, except for a subgroup of patients with baseline treadmill testing equal to or lower than 10 min [10]. In the REVAS (Randomised Evaluation of VEGF for Angiogenesis in Severe Coronary disease) trial, cardiac gene transfer was performed by intramyocardial injection via a mini-thoracotomy using adenovirus vector containing the VEGF121 gene in 67 patients with severe angina and no options for revascularisation [11]. There were significant improvements in exercise tolerance after 12 and 26 weeks. However, nuclear perfusion imaging yielded better results in the control group, although the therapeutic group achieved higher exercise workloads.
Consequently, the results from clinical trials are inconclusive, and there remain many issues that need to be addressed, including appropriate selection of patients, choice of angiogenic factors, optimal dose of therapeutic agents and the timing and route of the application delivery method.
Cell-based therapy is another therapeutic strategy in ischaemic heart disease. In post-natal angiogenesis, endothelial progenitor cells are thought to be recruited from bone marrow via peripheral blood to ischaemic lesions and then incorporated into new vessel formation. Based on this hypothesis, endothelial progenitor cells are employed as potential donor cells in therapeutic angiogenesis. Endothelial progenitor cells, which have the potential to proliferate and differentiate into mature endothelial cells, are characterised by surface markers such as VEGFR-2, CD34 and CD133, and can be isolated from peripheral blood, bone marrow and umbilical cord blood [63]. However, recent studies have demonstrated that haematopoietic stem cells and mesenchymal stem cells without expression of CD34 are also progenitor cells for angiogenesis [64]. Thus, the exact lineage and phenotype of endothelial progenitor cells still needs to be clarified [65].
Kawamoto et al. [6] showed that human endothelial progenitor cells decrease infarct size, increase capillary density and inhibit left ventricular remodelling when intravenously injected in the ischaemic rat model [6]. Furthermore, these transplanted cells are incorporated into neovascularisation of ischaemic areas, as documented by fluorescence microscopy and immunohistochemical staining. In subsequent experiments, the same authors also demonstrated successful neovascularisation by endothelial progenitor cells in a porcine ischaemia model. Assmus et al. [66] treated 20 acute myocardial infarction patients with intracoronary infusion of progenitor cells from either the bone marrow or peripheral blood and found improved ventricular function at 4 weeks’ follow-up. The results seem very promising, but further large prospective, randomised trials are required to define the efficacy and safety of cell-based angiogenic therapies.
Imaging modalities for perfusion and function in therapeutic angiogenesis
Non-invasive imaging to assess myocardial perfusion and ventricular function in therapeutic angiogenesis can be used to investigate whether blood flow and functional recovery correlate with the observed symptomatic benefit in clinical trials. For this purpose, imaging modalities include the nuclear techniques of single-photon emission computed tomography (SPECT) and positron emission tomography (PET), magnetic resonance imaging (MRI) and echocardiography. However, none of these modalities fulfils all the requirements for monitoring angiogenesis. Each method has its strengths and weaknesses concerning sensitivity, availability, reproducibility and feasibility of quantitative measurements.
SPECT perfusion imaging
Myocardial perfusion imaging with SPECT (MPI) using 201Tl chloride or 99mTc-based perfusion agents is the most widely used and well-established method for diagnosis, risk stratification and viability assessment in ischaemic heart disease [67]. Some of the phase I trials of therapeutic angiogenesis have demonstrated improved myocardial perfusion using SPECT [68, 69]. However, subsequent large trials have failed to show significant improvement in perfusion recovery in the therapy group [8, 9, 11] (Table 3). The feasibility of using MPI to assess perfusion changes induced by therapeutic angiogenesis remains to be established. It is well known that SPECT imaging can monitor the improvement in perfusion after bypass surgery or percutaneous transluminal coronary angioplasty in ischaemic heart disease [70]. However, the changes in perfusion induced by angiogenic therapy may be relatively small and occur over a longer time frame than the changes observed with conventional interventional therapies. In addition, collateral vessels induced by therapeutic angiogenesis may be functionally abnormal and may cause myocardial perfusion steal [71, 72].
Further studies in animal models are required to define the value of MPI for quantitative assessment of the success of angiogenesis.
PET perfusion imaging
There are no clinical data yet, but PET perfusion imaging has some advantages over SPECT methods in the assessment of perfusion during angiogenesis therapy. Superior spatial and temporal resolution, better sensitivity and the feasibility of attenuation correlation are the major technical advantages of PET imaging [73]. These advantages make it possible to measure absolute regional blood flow with PET using 15O-water or 13N-ammonia perfusion tracers [74]. The concentrations of these tracers in blood and myocardial tissue and their changes over time can be quantified, and tracer kinetic models can be applied to obtain flow (per minute per tissue volume). While it seems difficult to use PET for large clinical trials because of the limited current availability, the expanding use of PET systems is making the technology available for future angiogenesis trials [75].
MRI
Because of its higher spatial resolution compared with nuclear imaging techniques and its ability to delineate soft tissue without contrast agents or ionising radiation, MRI is well suited to assess cardiac morphology and ventricular function for ischaemic heart disease. Moreover, dynamic first-pass imaging methods using the widely available contrast agent, gadolinium diethyltriamine penta-acetic acid (Gd-DTPA), are available for the assessment of myocardial perfusion [76, 77]. Studies with the pig model of ischaemia have demonstrated the feasibility of assessing improvement in global and regional function and in myocardial blood flow as a result of therapeutic angiogenesis [4, 78, 79]. In a clinical phase I study, Laham et al. [80] used MRI with gadolinium-DTPA to assess the effects of intracoronary FGF-2 administration in 51 patients with myocardial ischaemia. In this study, MRI demonstrated improvement of regional wall thickening and a reduction in the delayed enhancement area. These preliminary data demonstrate the potential feasibility of using MRI to assess the efficacy of therapeutic angiogenesis.
Echocardiography
Myocardial echocardiography is inexpensive, widely available and non-invasive. Therefore it is an attractive technique for evaluation of ventricular function and blood flow. Its temporal and spatial resolution is superior to that of nuclear imaging techniques. Measurement of myocardial perfusion with echocardiography involves intravenous injection of gas-filled microbubbles as red cell tracers, which are acoustic scatterers, to delineate regional microvascular perfusion [81]. Mills et al. [82] showed the potential of this technique in the evaluation of the natural history of collateral development following coronary occlusion in the dog heart. Recently, new approaches to quantify myocardial blood flow with constant venous infusion of microbubbles have been proposed, and Villanueva et al. demonstrated improved collateral flow and reserve with VEGF therapeutic angiogenesis, using the technique in a dog model of myocardial infarction [83, 84]. One of the major limitations of this method is the dependence on experienced operators. Nuclear imaging and MRI are superior to echocardiography in this respect. However, its low cost and non-invasiveness still make it attractive for the assessment of therapeutic angiogenesis strategies in future clinical routine use.
Imaging of molecular markers of angiogenesis
Changes in myocardial perfusion and ventricular function are important as surrogate markers of clinical outcome, allowing assessment of therapeutic angiogenesis strategies. However, molecularly targetted imaging of angiogenic signalling pathways promises to be a further step forwards in the evaluation of specific and early aspects of angiogenesis mechanisms. As discussed above, angiogenesis is a multi-step, highly regulated process involving numerous growth factors and interactions between a number of cell types. Therefore, in order to induce sufficient angiogenesis with therapeutic strategies in ischaemic heart disease, optimised interventions at several steps of the angiogenesis pathway with multiple factors or progenitor cells seems to be required. In vivo monitoring of specific key steps of angiogenesis over time, which is uniquely achieved with molecular imaging techniques, is expected to solve the demanding task of optimising the therapeutic strategies. Recently, some initial animal studies have been performed on molecular targeted imaging for angiogenesis in ischaemic disease.
αvβ3 integrin imaging
As has been previously remarked, αvβ3 integrin expression on vessels is generally rare in adults, but it is seen on endothelial cells during angiogenesis in response to angiogenic growth factors such as bFGF [85]. Furthermore, αvβ3 integrin expression is fundamental for endothelial cell proliferation, adhesion and survival. Therefore, it is a good candidate for targeted delivery of imaging agents.
Some radiolabelled tracers targeting αvβ3 integrin expression were recently introduced for PET and SPECT imaging including 18F-galacto-RGD [86, 87], 111In-RP747 [88] and 99mTc-NC100692 [89, 90]. These tracers have demonstrated favourable characteristics for imaging of integrin expression in tumour models.
Meoli et al. [91] reported, for the first time, non-invasive nuclear imaging of myocardial angiogenesis in an experimental animal model of myocardial infarction using 111In-RP747. Eleven rats were studied 2 weeks after myocardial occlusion (45 min) and reperfusion using 111In-RP747 or a non-specific control agent. Histological examination revealed neovascularisation and over-expression of αv and β3 integrin subunits in the infarcted region. 111In-RP747 retention was seen (twofold increase) in the infarcted regions, but no regional retention was observed with the non-specific control compound, indicating specific 111In-RP747 uptake for αvβ3 integrin expression on angiogenic endothelial cells. Further studies in transient coronary occlusion canine models were performed with SPECT. Serial SPECT imaging was performed 10 h, 1 week and 3 weeks after reperfusion. Images demonstrated focal tracer accumulation, with the maximum increase in uptake occurring at 1 week.
Another report on angiogenesis imaging targeting αvβ3 integrin in ischaemic tissue was published by Hua et al. [90]. They studied mice with femoral artery occlusion at days 1, 3, 7 and 14 using a 99mTc-NC100692 SPECT tracer. Tracer uptake was assessed non-invasively with a pinhole planar imaging system. Increased uptake was observed at day 3 after femoral occlusion; it peaked at day 7 and decreased by 14 days. Additional experiments with fluorescent NC100692 analogue confirmed the localisation of the tracer in endothelial cells on tissue sections.
18F-galacto-RGD is a PET tracer for αvβ3 integrin expression developed at our institution [86, 87]. Specific tracer uptake was confirmed by dose-dependent blocking effects with pre-treatment using a non-radiolabelled cyclic RGD sequence containing peptide and using tumour cells which express αvβ3 integrin on their surface [92]. The feasibility of determination of αvβ3 integrin expression on endothelial cells was studied in A431 tumour cells which induce extensive angiogenesis and do not express integrin [93]. Using the PET tracer, we studied tracer accumulation in ischaemic–reperfusion model rat hearts [94]. Rats were subjected to 20 min of coronary occlusion and subsequent reperfusion. Following 3 weeks of recovery, 37 MBq of 18F-galacto-RGD was injected via the tail vein, and evaluation of tracer uptake in the myocardium with in vivo PET imaging and ex vivo autoradiography was performed. Homogeneous tracer distribution was observed in normal control rats; however, focal increased tracer uptake was shown with autoradiographic analysis in ischaemic rat hearts. In vivo small animal PET imaging successfully visualised the focal tracer uptake in areas with a corresponding reduction in 13N-ammonia perfusion (Fig. 2). In this study, the potential feasibility of non-invasive visualisation of integrin expression in ischaemic myocardium with PET was demonstrated. Already, 18F-galacto-RGD has been applied in clinical settings to evaluate tumour expression of αvβ3 [95]. A sufficient tumour to background ratio was obtained with PET imaging in this clinical study. Furthermore, there is a favourable tracer biodistribution because of predominantly renal tracer elimination, and the effective dose is similar to that of 18F-FDG [96]. Future clinical application in the assessment of therapeutic myocardial angiogenesis is expected using 18F-galacto-RGD.
Imaging of αvβ3 integrin expression in a rat model of coronary occlusion (20 min)/reperfusion using 18F-galacto-RGD. a Autoradiographic images of a non-operated normal heart and an ischaemic heart with occlusion/reperfusion at 1 week. Focal tracer accumulation is seen in the ischaemic heart. b In vivo short axis PET images demonstrating focal uptake of 18F-galacto-RGD in the corresponding area, with a decrease in perfusion on 13N-ammonia PET, 1 week after the ischaemic event
Targeted contrast ultrasound molecular imaging of integrin expression has been reported recently. Lipid microbubbles were targeted for integrin expression by surface conjugation with either monoclonal antibody against the αv integrin subunit or RGD-containing peptide [97, 98]. Leong-Poi et al. [98] assessed the antigenic response to ischaemia and FGF-2 using a hindlimb ischaemia rat model. Targeted bubble signals from the ischaemic limb were increased at 4 and 7 days after ligation of the iliac artery, and FGF-2 enhanced the signal increase. Unlike nuclear tracers, microbubbles circulate exclusively within the intravascular space, and therefore the retention reflects only the signal from endothelial cells that are located in accessible neovasculature [99]. An interesting feature of microbubbles is the potential for targeted local delivery of drugs, genes or cells by acoustic destruction of the microbubbles [100–103]. This is still in the early stages of animal studies, but echocardiography with molecular targeted microbubbles is a very promising technique for optimising angiogenesis therapies, as well as molecular angiogenesis imaging.
VEGF receptor expression imaging
VEGF is a most important and potent angiogenic factor in the regulation of endothelial cell proliferation and survival, as we have described above. Expression of the VEGF gene and VEGF receptors is strongly enhanced by hypoxia in the angiogenic process. Therefore, VEGF receptors are good candidates for imaging angiogenesis in ischaemic tissues.
Using 111In-labelled recombinant human VEGF121 in a rabbit model of unilateral hindlimb ischaemia, Lu et al. [104] tested the imaging of VEGF receptor expression in ischaemic tissues. Ten days after femoral artery occlusion, tracer uptake was assessed by postmortem gamma counting studies and planar scintigraphic imaging. Tracer uptake in ischaemic muscle was significant increased over contralateral and sham-operated normal perfused muscle. The increased uptake was also detected by scintigraphic imaging, but this finding was subtle on the planar scintigraphic image. Further SPECT studies may be required over time and from an early assessment time point.
Matrix metalloproteinase (MMP) activity imaging
MMPs are proteolytic enzymes that cause extracellular protein degradation. In the early stage of angiogenesis, they are responsible for degradation of vascular basement membranes, resulting in endothelial cell migration and growth factor liberation [23, 24]. These proteinases are also responsible for left ventricular remodelling by degrading extracellular matrix in the heart after myocardial infarction [105]. The recent finding that pharmacological inhibition of MMPs attenuates left ventricular dilatation in the infarcted mouse heart has led to the proposal that MMP inhibitors have the potential to be used therapeutically after myocardial infarction [105]. However, there remain several questions, including the optimal timing for, the spectrum and the specificity of the blocking therapy, and its effects on angiogenesis [105, 106].
Recently, Su et al. [107] demonstrated the feasibility of MMP activation imaging in a murine model of myocardial infarction. Regional uptake of 111In-labelled MMP- targeted radiolabelled tracer (111In-RP782) in the infarcted area was confirmed by autoradiography 1 week after myocardial infarction. Using a similar 99mTc-labelled tracer, non-invasive visualisation of tracer uptake was shown 1 and 3 weeks after myocardial infarction in regions of decreased 201Tl perfusion. While further confirmatory animal studies are required, this non-invasive technique holds promise for the provision of insights into the role of MMPs not only in ventricular remodelling but also in angiogenesis in ischaemic heart disease.
Summary
Changes in myocardial perfusion and ventricular function imaged non-invasively by means of SPECT, PET, MRI or echocardiography are important as surrogate markers of clinical outcome in therapeutic angiogenesis. New molecular imaging strategies which target specific aspects of the angiogenic process, such as integrin overexpression, VEGF receptor expression and MMP activation, have been proposed recently. These new approaches are expected to answer numerous questions that have arisen in recent large clinical trials of therapeutic angiogenesis (e.g. regarding the selection of growth factors and progenitor cells, timing, dose and route of administration). The results of early animal studies of these new molecular imaging strategies are very promising, but further efforts need to be made to establish their sensitivity, specificity and quantitative capability in monitoring the specific molecular events of angiogenesis for clinical use.
References
Sasayama S, Fujita M. Recent insights into coronary collateral circulation. Circulation 1992;85:1197–204.
Toyota E, Matsunaga T, Chilian WM. Myocardial angiogenesis. Mol Cell Biochem 2004;264:35–44.
Tomanek RJ, Schatteman GC. Angiogenesis: new insights and therapeutic potential. Anat Rec 2000;261:126–35.
Pearlman JD, Hibberd MG, Chuang ML, Harada K, Lopez JJ, Gladstone SR, et al. Magnetic resonance mapping demonstrates benefits of VEGF-induced myocardial angiogenesis. Nat Med 1995;1:1085–9.
Harada K, Friedman M, Lopez JJ, Wang SY, Li J, Prasad PV, et al. Vascular endothelial growth factor administration in chronic myocardial ischemia. Am J Physiol 1996;270:H1791–802.
Kawamoto A, Gwon HC, Iwaguro H, Yamaguchi JI, Uchida S, Masuda H, et al. Therapeutic potential of ex vivo expanded endothelial progenitor cells for myocardial ischemia. Circulation 2001;103:634–7.
Ueno H, Li JJ, Masuda S, Qi Z, Yamamoto H, Takeshita A. Adenovirus-mediated expression of the secreted form of basic fibroblast growth factor (FGF-2) induces cellular proliferation and angiogenesis in vivo. Arterioscler Thromb Vasc Biol 1997;17:2453–60.
Simons M, Annex BH, Laham RJ, Kleiman N, Henry T, Dauerman H, et al. Pharmacological treatment of coronary artery disease with recombinant fibroblast growth factor-2: double-blind, randomized, controlled clinical trial. Circulation 2002;105:788–93.
Henry TD, Annex BH, McKendall GR, Azrin MA, Lopez JJ, Giordano FJ, et al. The VIVA trial: Vascular endothelial growth factor in Ischemia for Vascular Angiogenesis. Circulation 2003;107:1359–65.
Grines CL, Watkins MW, Helmer G, Penny W, Brinker J, Marmur JD, et al. Angiogenic Gene Therapy (AGENT) trial in patients with stable angina pectoris. Circulation 2002;105:1291–7.
Stewart DJ, Hilton JD, Arnold JM, Gregoire J, Rivard A, Archer SL, et al. Angiogenic gene therapy in patients with nonrevascularizable ischemic heart disease: a phase 2 randomized, controlled trial of AdVEGF(121) (AdVEGF121) versus maximum medical treatment. Gene Ther 2006;13:1503–11.
Simons M, Bonow RO, Chronos NA, Cohen DJ, Giordano FJ, Hammond HK, et al. Clinical trials in coronary angiogenesis: issues, problems, consensus: an expert panel summary. Circulation 2000;102:E73–86.
Fam NP, Verma S, Kutryk M, Stewart DJ. Clinician guide to angiogenesis. Circulation 2003;108:2613–8.
Weissleder R, Mahmood U. Molecular imaging. Radiology 2001;219:316–33.
Risau W. Mechanisms of angiogenesis. Nature 1997;386:671–4.
Ware JA, Simons M. Angiogenesis in ischemic heart disease. Nat Med 1997;3:158–64.
Carmeliet P. Mechanisms of angiogenesis and arteriogenesis. Nat Med 2000;6:389–95.
Buschmann I, Schaper W. The pathophysiology of the collateral circulation (arteriogenesis). J Pathol 2000;190:338–42.
Schaper W, Scholz D. Factors regulating arteriogenesis. Arterioscler Thromb Vasc Biol 2003;23:1143–51.
Drake CJ. Embryonic and adult vasculogenesis. Birth Defects Res C Embryo Today 2003;69:73–82.
Walter DH, Dimmeler S. Endothelial progenitor cells: regulation and contribution to adult neovascularization. Herz 2002;27:579–88.
Asahara T, Masuda H, Takahashi T, Kalka C, Pastore C, Silver M, etal. Bone marrow origin of endothelial progenitor cells responsible for postnatal vasculogenesis in physiological and pathological neovascularization. Circ Res 1999;85:221–8.
Shapiro SD. Matrix metalloproteinase degradation of extracellular matrix: biological consequences. Curr Opin Cell Biol 1998;10:602–8.
Pepper MS. Role of the matrix metalloproteinase and plasminogen activator-plasmin systems in angiogenesis. Arterioscler Thromb Vasc Biol 2001;21:1104–17.
Streuli C. Extracellular matrix remodelling and cellular differentiation. Curr Opin Cell Biol 1999;11:634–40.
Serini G, Valdembri D, Bussolino F. Integrins and angiogenesis: a sticky business. Exp Cell Res 2006;312:651–8.
Semenza GL. HIF-1, O(2), and the 3 PHDs: how animal cells signal hypoxia to the nucleus. Cell 2001;107:1–3.
Jewell UR, Kvietikova I, Scheid A, Bauer C, Wenger RH, Gassmann M. Induction of HIF-1alpha in response to hypoxia is instantaneous. Faseb J 2001;15:1312–4.
Semenza GL. Hypoxia-inducible factor 1: master regulator of O2 homeostasis. Curr Opin Genet Dev 1998;8:588–94.
Sunderkotter C, Steinbrink K, Goebeler M, Bhardwaj R, Sorg C. Macrophages and angiogenesis. J Leukoc Biol 1994;55:410–22.
Li J, Post M, Volk R, Gao Y, Li M, Metais C, et al. PR39, a peptide regulator of angiogenesis. Nat Med 2000;6:49–55.
Hellwig-Burgel T, Rutkowski K, Metzen E, Fandrey J, Jelkmann W. Interleukin-1beta and tumor necrosis factor-alpha stimulate DNA binding of hypoxia-inducible factor-1. Blood 1999;94:1561–7.
Folkman J, Klagsbrun M. Angiogenic factors. Science 1987;235:442–7.
Folkman J, Ingber D. Inhibition of angiogenesis. Semin Cancer Biol 1992;3:89–96.
Auerbach W, Auerbach R. Angiogenesis inhibition: a review. Pharmacol Ther 1994;63:265–311.
Ferrara N, Gerber HP, LeCouter J. The biology of VEGF and its receptors. Nat Med 2003;9:669–76.
Robinson CJ, Stringer SE. The splice variants of vascular endothelial growth factor (VEGF) and their receptors. J Cell Sci 2001;114:853–65.
Marti HH, Risau W. Systemic hypoxia changes the organ-specific distribution of vascular endothelial growth factor and its receptors. Proc Natl Acad Sci USA 1998;95:15809–14.
Zachary I, Gliki G. Signaling transduction mechanisms mediating biological actions of the vascular endothelial growth factor family. Cardiovasc Res 2001;49:568–81.
Jingjing L, Srinivasan B, Bian X, Downey HF, Roque RS. Vascular endothelial growth factor is increased following coronary artery occlusion in the dog heart. Mol Cell Biochem 2000;214:23–30.
Ema M, Taya S, Yokotani N, Sogawa K, Matsuda Y, Fujii-Kuriyama Y. A novel bHLH-PAS factor with close sequence similarity to hypoxia-inducible factor 1alpha regulates the VEGF expression and is potentially involved in lung and vascular development. Proc Natl Acad Sci USA 1997;94:4273–8.
Forsythe JA, Jiang BH, Iyer NV, Agani F, Leung SW, Koos RD, et al. Activation of vascular endothelial growth factor gene transcription by hypoxia-inducible factor 1. Mol Cell Biol 1996;16:4604–13.
Shweiki D, Itin A, Soffer D, Keshet E. Vascular endothelial growth factor induced by hypoxia may mediate hypoxia-initiated angiogenesis. Nature 1992;359:843–5.
Stupack DG, Cheresh DA. ECM remodeling regulates angiogenesis: endothelial integrins look for new ligands. Sci STKE 2002;2002:PE7.
Wu WB, Peng HC, Huang TF. Disintegrin causes proteolysis of beta-catenin and apoptosis of endothelial cells. Involvement of cell-cell and cell-ECM interactions in regulating cell viability. Exp Cell Res 2003;286:115–27.
van der Flier A, Sonnenberg A. Function and interactions of integrins. Cell Tissue Res 2001;305:285–98.
Max R, Gerritsen RR, Nooijen PT, Goodman SL, Sutter A, Keilholz U, et al. Immunohistochemical analysis of integrin alpha vbeta3 expression on tumor-associated vessels of human carcinomas. Int J Cancer 1997;71:320–4.
Enenstein J, Kramer RH. Confocal microscopic analysis of integrin expression on the microvasculature and its sprouts in the neonatal foreskin. J Invest Dermatol 1994;103:381–6.
Hodivala-Dilke KM, Reynolds AR, Reynolds LE. Integrins in angiogenesis: multitalented molecules in a balancing act. Cell Tissue Res 2003;314:131–44.
Albelda SM, Daise M, Levine EM, Buck CA. Identification and characterization of cell-substratum adhesion receptors on cultured human endothelial cells. J Clin Invest 1989;83:1992–2002.
Plow EF, Haas TA, Zhang L, Loftus J, Smith JW. Ligand binding to integrins. J Biol Chem 2000;275:21785–8.
Xiong JP, Stehle T, Diefenbach B, Zhang R, Dunker R, Scott DL, et al. Crystal structure of the extracellular segment of integrin alpha Vbeta3. Science 2001;294:339–45.
Xiong JP, Stehle T, Zhang R, Joachimiak A, Frech M, Goodman SL, et al. Crystal structure of the extracellular segment of integrin alpha Vbeta3 in complex with an Arg-Gly-Asp ligand. Science 2002;296:151–5.
Brooks PC, Montgomery AM, Rosenfeld M, Reisfeld RA, Hu T, Klier G, et al. Integrin alpha v beta 3 antagonists promote tumor regression by inducing apoptosis of angiogenic blood vessels. Cell 1994;79:1157–64.
Friedlander M, Brooks PC, Shaffer RW, Kincaid CM, Varner JA, Cheresh DA. Definition of two angiogenic pathways by distinct alpha v integrins. Science 1995;270:1500–2.
MacDonald TJ, Taga T, Shimada H, Tabrizi P, Zlokovic BV, Cheresh DA, et al. Preferential susceptibility of brain tumors to the antiangiogenic effects of an alpha(v) integrin antagonist. Neurosurgery 2001;48:151–7.
Silletti S, Kessler T, Goldberg J, Boger DL, Cheresh DA. Disruption of matrix metalloproteinase 2 binding to integrin alpha vbeta 3 by an organic molecule inhibits angiogenesis and tumor growth in vivo. Proc Natl Acad Sci USA 2001;98:119–24.
Maeshima Y, Yerramalla UL, Dhanabal M, Holthaus KA, Barbashov S, Kharbanda S, et al. Extracellular matrix-derived peptide binds to α(v)β(3) integrin and inhibits angiogenesis. J Biol Chem 2001;276:31959–68.
Affleck DG, Bull DA, Bailey SH, Albanil A, Connors R, Stringham JC, et al. PDGF(BB) increases myocardial production of VEGF: shift in VEGF mRNA splice variants after direct injection of bFGF, PDGF(BB), and PDGF(AB). J Surg Res 2002;107:203–9.
Ahmet I, Sawa Y, Iwata K, Matsuda H. Gene transfection of hepatocyte growth factor attenuates cardiac remodeling in the canine heart: a novel gene therapy for cardiomyopathy. J Thorac Cardiovasc Surg 2002;124:957–63.
Schumacher B, Pecher P, von Specht BU, Stegmann T. Induction of neoangiogenesis in ischemic myocardium by human growth factors: first clinical results of a new treatment of coronary heart disease. Circulation 1998;97:645–50.
Stegmann TJ, Hoppert T, Schlurmann W, Gemeinhardt S. First angiogenic treatment of coronary heart disease by FGF-1: long-term results after 3 years. CVR 2000;1:5–10.
Kermani P, Leclerc G, Martel R, Fareh J. Effect of ionizing radiation on thymidine uptake, differentiation, and VEGFR2 receptor expression in endothelial cells: the role of VEGF(165). Int J Radiat Oncol Biol Phys 2001;50:213–20.
Reyes M, Dudek A, Jahagirdar B, Koodie L, Marker PH, Verfaillie CM. Origin of endothelial progenitors in human postnatal bone marrow. J Clin Invest 2002;109:337–46.
Hirschi KK, Goodell MA. Hematopoietic, vascular and cardiac fates of bone marrow-derived stem cells. Gene Ther 2002;9:648–52.
Assmus B, Schachinger V, Teupe C, Britten M, Lehmann R, Dobert N, et al. Transplantation of Progenitor Cells and Regeneration Enhancement in Acute Myocardial Infarction (TOPCARE-AMI). Circulation 2002;106:3009–17.
Underwood SR, Anagnostopoulos C, Cerqueira M, Ell PJ, Flint EJ, Harbinson M, et al. Myocardial perfusion scintigraphy: the evidence. Eur J Nucl Med Mol Imaging 2004;31:261–91.
Hendel RC, Henry TD, Rocha-Singh K, Isner JM, Kereiakes DJ, Giordano FJ, et al. Effect of intracoronary recombinant human vascular endothelial growth factor on myocardial perfusion: evidence for a dose-dependent effect. Circulation 2000;101:118–21.
Laham RJ, Sellke FW, Edelman ER, Pearlman JD, Ware JA, Brown DL, et al. Local perivascular delivery of basic fibroblast growth factor in patients undergoing coronary bypass surgery: results of a phase I randomized, double-blind, placebo-controlled trial. Circulation 1999;100:1865–71.
Giedd KN, Bergmann SR. Myocardial perfusion imaging following percutaneous coronary intervention: the importance of restenosis, disease progression, and directed reintervention. J Am Coll Cardiol 2004;43:328–36.
Bonow RO. Contractile reserve and coronary blood flow reserve in collateral-dependent myocardium. J Am Coll Cardiol 1999;33:705–7.
Sambuceti G, Parodi O, Giorgetti A, Salvadori P, Marzilli M, Dabizzi P, et al. Microvascular dysfunction in collateral-dependent myocardium. J Am Coll Cardiol 1995;26:615–23.
Schwaiger M. Myocardial perfusion imaging with PET. J Nucl Med 1994;35:693–8.
Beller GA, Bergmann SR. Myocardial perfusion imaging agents: SPECT and PET. J Nucl Cardiol 2004;11:71–86.
Gropler RJ, Soto P. Recent advances in cardiac positron emission tomography in the clinical management of the cardiac patient. Curr Cardiol Rep 2004;6:20–6.
Muhling O, Jerosch-Herold M, Nabauer M, Wilke N. Assessment of ischemic heart disease using magnetic resonance first-pass perfusion imaging. Herz 2003;28:82–9.
Klassen C, Nguyen M, Siuciak A, Wilke NM. Magnetic resonance first pass perfusion imaging for detecting coronary artery disease. Eur J Radiol 2006;57:412–6.
Lopez JJ, Laham RJ, Stamler A, Pearlman JD, Bunting S, Kaplan A, et al. VEGF administration in chronic myocardial ischemia in pigs. Cardiovasc Res 1998;40:272–81.
Tse HF, Kwong YL, Chan JK, Lo G, Ho CL, Lau CP. Angiogenesis in ischaemic myocardium by intramyocardial autologous bone marrow mononuclear cell implantation. Lancet 2003;361:47–9.
Laham RJ, Chronos NA, Pike M, Leimbach ME, Udelson JE, Pearlman JD, et al. Intracoronary basic fibroblast growth factor (FGF-2) in patients with severe ischemic heart disease: results of a phase I open-label dose escalation study. J Am Coll Cardiol 2000;36:2132–9.
Kaul S. Myocardial contrast echocardiography: 15 years of research and development. Circulation 1997;96:3745–60.
Mills JD, Fischer D, Villanueva FS. Coronary collateral development during chronic ischemia: serial assessment using harmonic myocardial contrast echocardiography. J Am Coll Cardiol 2000;36:618–24.
Wei K, Jayaweera AR, Firoozan S, Linka A, Skyba DM, Kaul S. Quantification of myocardial blood flow with ultrasound-induced destruction of microbubbles administered as a constant venous infusion. Circulation 1998;97:473–83.
Villanueva FS, Abraham JA, Schreiner GF, Csikari M, Fischer D, Mills JD, et al. Myocardial contrast echocardiography can be used to assess the microvascular response to vascular endothelial growth factor-121. Circulation 2002;105:759–65.
Drake CJ, Cheresh DA, Little CD. An antagonist of integrin alpha v beta 3 prevents maturation of blood vessels during embryonic neovascularization. J Cell Sci 1995;108(Pt 7):2655–61.
Haubner R, Kuhnast B, Mang C, Weber WA, Kessler H, Wester HJ, et al. [18F]Galacto-RGD: synthesis, radiolabeling, metabolic stability, and radiation dose estimates. Bioconjug Chem 2004;15:61–9.
Haubner R, Wester HJ, Burkhart F, Senekowitsch-Schmidtke R, Weber W, Goodman SL, et al. Glycosylated RGD-containing peptides: tracer for tumor targeting and angiogenesis imaging with improved biokinetics. J Nucl Med 2001;42:326–36.
Harris TD, Kalogeropoulos S, Nguyen T, Liu S, Bartis J, Ellars C, et al. Design, synthesis, and evaluation of radiolabeled integrin alpha v beta 3 receptor antagonists for tumor imaging and radiotherapy. Cancer Biother Radiopharm 2003;18:627–41.
Bach-Gansmo T, Danielsson R, Saracco A, Wilczek B, Bogsrud TV, Fangberget A, et al. Integrin receptor imaging of breast cancer: a proof-of-concept study to evaluate 99mTc-NC100692. J Nucl Med 2006;47:1434–9.
Hua J, Dobrucki LW, Sadeghi MM, Zhang J, Bourke BN, Cavaliere P, et al. Noninvasive imaging of angiogenesis with a 99mTc-labeled peptide targeted at alphavbeta3 integrin after murine hindlimb ischemia. Circulation 2005;111:3255–60.
Meoli DF, Sadeghi MM, Krassilnikova S, Bourke BN, Giordano FJ, Dione DP, et al. Noninvasive imaging of myocardial angiogenesis following experimental myocardial infarction. J Clin Invest 2004;113:1684–91.
Haubner R, Wester HJ, Weber WA, Mang C, Ziegler SI, Goodman SL, et al. Noninvasive imaging of alpha(v)beta3 integrin expression using 18F-labeled RGD-containing glycopeptide and positron emission tomography. Cancer Res 2001;61:1781–5.
Haubner R, Weber WA, Beer AJ, Vabuliene E, Reim D, Sarbia M, et al. Noninvasive visualization of the activated alphavbeta3 integrin in cancer patients by positron emission tomography and [18F]galacto-RGD. PLoS Med 2005;2:e70.
Higuchi T, Watzlowik P, Reder S, Huisman M, Nekolla S, Wester HJ, et al. F-18 galacto-RGD PET to determine myocardial integrin expression following ischemia-reperfusion in a rat model. J Nucl Med 2006;47 Suppl 1:128, abstract.
Beer AJ, Haubner R, Sarbia M, Goebel M, Luderschmidt S, Grosu AL, et al. Positron emission tomography using [18F]galacto-RGD identifies the level of integrin alpha(v)beta3 expression in man. Clin Cancer Res 2006;12:3942–9.
Beer AJ, Haubner R, Goebel M, Luderschmidt S, Spilker ME, Wester HJ, et al. Biodistribution and pharmacokinetics of the alphavbeta3-selective tracer 18F-galacto-RGD in cancer patients. J Nucl Med 2005;46:1333–41.
Ellegala DB, Leong-Poi H, Carpenter JE, Klibanov AL, Kaul S, Shaffrey ME, et al. Imaging tumor angiogenesis with contrast ultrasound and microbubbles targeted to alpha(v)beta3. Circulation 2003;108:336–41.
Leong-Poi H, Christiansen J, Klibanov AL, Kaul S, Lindner JR. Noninvasive assessment of angiogenesis by ultrasound and microbubbles targeted to alpha(v)-integrins. Circulation 2003;107:455–60.
Villanueva FS. Molecular images of neovascularization: art for art’s sake or form with a function? Circulation 2005;111:3188–91.
Korpanty G, Chen S, Shohet RV, Ding J, Yang B, Frenkel PA, et al. Targeting of VEGF-mediated angiogenesis to rat myocardium using ultrasonic destruction of microbubbles. Gene Ther 2005;12:1305–12.
Vancraeynest D, Havaux X, Pouleur AC, Pasquet A, Gerber B, Beauloye C, et al. Myocardial delivery of colloid nanoparticles using ultrasound-targeted microbubble destruction. Eur Heart J 2006;27:237–45.
Zen K, Okigaki M, Hosokawa Y, Adachi Y, Nozawa Y, Takamiya M, et al. Myocardium-targeted delivery of endothelial progenitor cells by ultrasound-mediated microbubble destruction improves cardiac function via an angiogenic response. J Mol Cell Cardiol 2006;40:799–809.
Zhigang W, Zhiyu L, Haitao R, Hong R, Qunxia Z, Ailong H, et al. Ultrasound-mediated microbubble destruction enhances VEGF gene delivery to the infarcted myocardium in rats. Clin Imaging 2004;28:395–8.
Lu E, Wagner WR, Schellenberger U, Abraham JA, Klibanov AL, Woulfe SR, et al. Targeted in vivo labeling of receptors for vascular endothelial growth factor: approach to identification of ischemic tissue. Circulation 2003;108:97–103.
Creemers EE, Cleutjens JP, Smits JF, Daemen MJ. Matrix metalloproteinase inhibition after myocardial infarction: a new approach to prevent heart failure? Circ Res 2001;89:201–10.
Heymans S, Luttun A, Nuyens D, Theilmeier G, Creemers E, Moons L, et al. Inhibition of plasminogen activators or matrix metalloproteinases prevents cardiac rupture but impairs therapeutic angiogenesis and causes cardiac failure. Nat Med 1999;5:1135–42.
Su H, Spinale FG, Dobrucki LW, Song J, Hua J, Sweterlitsch S, et al. Noninvasive targeted imaging of matrix metalloproteinase activation in a murine model of postinfarction remodeling. Circulation 2005;112:3157–67.
Acknowledgements
The authors thank Ura Frenklah, M.D. for his excellent editorial help. The work relating to 18F-gRGD was in part supported by the Deutsche Forschungsgemeinschaft and a Bristol-Myers Squibb unrestricted research grant.
Author information
Authors and Affiliations
Corresponding authors
Rights and permissions
About this article
Cite this article
Higuchi, T., Wester, H.J. & Schwaiger, M. Imaging of angiogenesis in cardiology. Eur J Nucl Med Mol Imaging 34 (Suppl 1), 9–19 (2007). https://doi.org/10.1007/s00259-007-0436-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00259-007-0436-z