Abstract
Purpose
Myocardial flow reserve (MFR) measurement has an important role in assessing the functional severity of coronary artery stenosis. However, a discrepancy between the anatomical severity of coronary artery stenosis and MFR is often observed. Such a discrepancy may be explained by coronary risk factors. In this study, we aimed to investigate the influence of coronary artery stenosis severity and risk factors on MFR.
Methods
Seventy-four patients suspected to have coronary artery disease and seven age-matched healthy volunteers were enrolled. Myocardial blood flow (MBF) and MFR were measured using 15O-labelled water PET. Regional MFR was calculated in regions with significant coronary artery stenosis (stenotic regions) and in regions without significant stenosis (remote regions). The contributions of coronary artery stenosis severity and coronary risk factors were assessed using univariate and multivariate analyses.
Results
In stenotic regions, MFR correlated inversely with coronary artery stenosis severity (r=−0.50, p<0.01). Univariate analysis did not show any significant difference in MFR between the patients with and the patients without each risk factor. In remote regions, however, MFR was significantly decreased in the diabetes and smoking groups (each p<0.05). By multivariate analysis, diabetes and smoking were independent predictors of MFR (each p<0.05). In the group with more than one risk factor, MFR was significantly lower (2.78±0.79) than in the other group (3.40±1.22, p<0.05).
Conclusion
MFR is influenced not only by coronary stenosis severity but also by coronary risk factors. In particular, the influence of risk factors should be considered in regions without severe coronary stenosis.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Coronary artery disease (CAD) continues to be a major cause of death in modern industrialised societies. Techniques for measuring myocardial blood flow (MBF) have an important role in identifying patients with CAD and determining their prognosis. Positron emission tomography (PET) is the most accurate non-invasive imaging technique for measuring regional MBF. The measurement of regional myocardial perfusion permits measurement of myocardial flow reserve (MFR) and evaluation of the physiological significance of coronary lesions. However, a discrepancy is often observed between the anatomical severity of coronary stenosis and MFR. Such a discrepancy may be explained by coronary risk factors, such as diabetes, hypertension, hyperlipidaemia, smoking, left ventricular hypertrophy, gender and age [1–17]. Many risk factors associated with atherosclerosis may cause a decrease in MFR despite angiographically normal coronary arteries. The aim of this study was to assess the influence of coronary stenosis severity and risk factors on MFR in patients suspected to have CAD.
Materials and methods
Study population
This study included patients suspected to have CAD who underwent both coronary angiography and PET with 15O-labelled water within an interval of 2 months. No clinical events or changes in medication occurred between the two studies. Patients with a history of myocardial infarction (MI) or coronary artery bypass grafting were excluded. This study enrolled 74 patients (53 men and 21 women, mean age 63.0±9.8 years) who matched all the criteria.Seven age-matched normal volunteers served as controls for the MBF and vasodilator measurements. They were selected because their history and physical examinations placed them at low risk for CAD; all had a normal resting electrocardiogram (ECG) and no coronary risk factors.Cardiac medications were not withdrawn before the study because of the severity of anginal symptoms. All patients were carefully instructed to refrain from caffeine intake and smoking during the 24 h before the PET study. All of them gave written informed consent. This study was approved by the Ethics Committee of Hokkaido University Hospital.
Coronary angiography
All patients underwent coronary angiography. Selective angiography of the right and left coronary arteries in multiple views was performed using the Judkins technique. Multiple manual injections of contrast medium were performed. Using the computerised quantitative coronary angiography analysis system (CAASII System; Pie Medical Imaging, The Netherlands), coronary stenosis severity was assessed. Coronary artery stenosis was considered significant when there was a reduction of more than 50% in the diameter of the main branch.
PET protocol
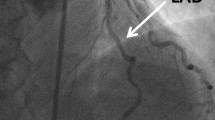
The PET scan protocol has been described previously [18, 19]. Pharmacological stress was induced by adenosine triphosphate (ATP) infusion at a rate of 0.16 mg kg−1 min−1 for 8 min through the left antecubital vein [20, 21]. MBF at rest and during ATP infusion was calculated by 15O-labelled water PET (Fig. 1). All the PET scans were obtained with an ECAT EXACT HR+ (Siemens/CTI).
In brief, a transmission scan was performed to correct photon attenuation for 6 min with a 68Ge source. Next, all the subjects inhaled 15O-labelled CO for 1 min to obtain the blood volume image. The total inhaled dose was 2,000 MBq. Then 15O-labelled water was infused into an antecubital vein to obtain the blood flow image. The administered dose was 1,000 MBq. Twelve minutes after the first infusion of 15O-labelled water, intravenous ATP infusion (0.16 mg kg−1 min−1) was started and PET acquisition was commenced 3 min after the beginning of ATP infusion. ATP infusion was continued until the end of the second 15O-labelled water PET scan. Heart rate, blood pressure and 12-lead ECG were recorded at rest and at 1-min intervals during and after the ATP administration.All the emission sinograms were reconstructed with filtered back-projection using a Hann filter (cut-off frequency, 0.3 cycles/pixel). The in-plane resolution was 4.5 mm in full-width at half-maximum in the images reconstructed into a 128×128 matrix. All the data were corrected for dead time, decay and measured photon attenuation.MBF was quantified using the single tissue compartment model developed by Katoh et al. [22]. The left ventricle was divided into three regions according to coronary artery regions (Fig. 2) and regional MBF was calculated in each region. Regional MFR was calculated as the ratio of regional hyperaemic MBF to regional MBF at rest. Two experienced doctors blind to the patients’ clinical data analysed all the PET data.
Data analysis
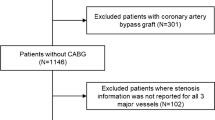
To compare the influence of risk factors on MFR in regions with and without significant coronary artery stenosis, the myocardial regions of the patients were divided into two groups: regions with significant coronary artery stenosis (stenotic region, n=47) and regions without significant stenosis (remote regions, n=67). Because we had to select one region from stenotic regions per person for univariate and multivariate analyses, we chose the region with the most severe coronary stenosis in the patients with multivessel disease. We analysed regional MBF and MFR in stenotic regions and also in the remote regions. In addition, the influence of coronary artery stenosis severity and coronary risk factors [e.g. diabetes, hypertension, hyperlipidaemia, smoking, left ventricular hypertrophy (LVH), gender, age and body mass index (BMI)] was assessed by univariate and multivariate analysis. In remote regions, the influence of coronary artery stenosis severity was excluded from the analyses.
Statistical analysis
All the data were expressed as mean±SD. Regression analysis was performed using a linear regression method. Differences in values were evaluated using a two-tailed unpaired t test. Multivariate analysis was performed using multiple regression analysis to assess the influence of coronary artery stenosis and of risk factors on MFR. A p value of <0.05 was used to determine statistical significance.
Results
Patient characteristics
Clinical variables are described in Table 1. Twenty-five patients had one-vessel disease, 15 had two-vessel disease and seven had three-vessel disease. Twenty-seven patients had no significant coronary stenosis. Thirty-five patients had previously been diagnosed as having hypertension and 32 of them (92%) had been treated with anti-hypertensive drugs. Forty-eight patients had previously been diagnosed with hyperlipidaemia and 36 of them (75%) had been treated with lipid-lowering drugs. Twenty-five patients had previously been diagnosed as having type 2 diabetes and 19 of them (76%) had been treated with anti-diabetic drugs or insulin. Twenty-five patients had a history of smoking. Ten patients had LVH assessed by echocardiography (wall thickness >12 mm). Eighteen patients were more than 70 years old. We included the patients who had already received specific medication for each risk factor.
MBF and MFR in control group
In the control group, the mean global MBF at rest was 0.91±0.16 ml min−1 g−1. The mean hyperaemic global MBF was 3.66±0.81 ml min−1 g−1 and the mean global MFR was 4.06±0.81 (Table 2).
MBF and MFR in stenotic regions
In stenotic regions, the mean MBF at rest was 0.96±0.22 ml min−1 g−1 (p=NS vs control). The mean hyperaemic MBF was 2.19±0.96 ml min−1 g−1 (p<0.001 vs control) and the mean MFR was 2.35±0.89 (p<0.001 vs control) (Table 2).
Correlation between stenosis severity and MFR in stenotic regions
In stenotic regions, the correlation between coronary artery stenosis severity and MFR was relatively weak, but statistically significant. MFR progressively decreased as the degree of stenosis increased (y=4.12−0.26x, r=−0.50, p<0.01, Fig. 3).
Univariate and multivariate analyses in stenotic regions
In stenotic regions, there was no significant difference in MFR between the patients with and those without any risk factor in univariate analysis (Table 3). MFR did not correlate with age (r=0.20, p=NS) or BMI (r=0.14, p=NS). In the multivariate analysis, coronary artery stenosis severity was the only significant predictor for MFR (R=−0.55, t=−3.78, p<0.001). None of the risk factors were significant predictors (Table 4).
MBF and MFR in remote regions
In remote regions, the mean MBF at rest was 0.94±0.22 ml min−1 g−1 (p=NS vs control). The mean hyperaemic MBF was 2.66±0.93 ml min−1 g−1 (p<0.01 vs control) and the mean MFR was 2.99±0.99 (p<0.01 vs control) (Table 2). Hyperaemic MBF and MFR in the remote regions were significantly higher than those in the stenotic regions (each p<0.01).
Univariate and multivariate analyses in remote regions
In remote regions, MFR was significantly decreased in the diabetes group (2.60±0.83 vs 3.19±1.02, p<0.05) and the smoking group (2.65±0.70 vs 3.17±1.08, p<0.05) in univariate analysis. MFR also tended to be decreased in the hypertension group (2.88±1.02 vs 3.09±0.98, p=0.38) and the hyperlipidaemia group (2.90±0.89 vs 3.16±1.18, p=0.31) (Table 5). MFR in remote regions did not correlate with age (r=0.14, p=NS) or BMI (r=0.16, p=NS). By multivariate analysis, diabetes (R=−0.27, t=−2.29, p<0.05) and smoking (R=−0.30, t=−2.32, p<0.05) were independent predictors of MFR (Table 6).
MFR and number of risk factors in remote regions
To assess the effects of coronary risk factors, including diabetes, hypertension, hyperlipidaemia and smoking, on MFR, the total number of coronary risk factors causing the decrease in MFR were compared. MFR in remote regions with two or more risk factors (n=41) was significantly lower than that in remote regions with one or no risk factors (n=26) (2.72±0.78 vs 3.43±1.15, p<0.01, Fig. 4). Although the MFR in remote regions with one or no risk factors was preserved (p=NS, vs control), that in remote regions with two or more risk factors was significantly lower than that in the control group (p<0.001, vs control). In stenotic regions, there was no significant difference in MFR between those with and those without multiple risk factors (2.31±0.96 vs 2.43±0.73, p=0.67).
Discussion
These results indicate that while reduction in MFR in stenotic regions correlated significantly with coronary artery stenosis severity rather than with the risk factors, in remote regions the reduction in MFR was influenced by the risk factors, such as diabetes or smoking. Furthermore, the MFR in remote regions was significantly decreased in patients with multiple risk factors as compared with those who had one or no risk factors.
Abnormal MFR can be due to narrowing of the epicardial coronary arteries or, in the absence of angiographically demonstrable atherosclerotic disease, may reflect dysfunction of the coronary microcirculation. Uren et al. first reported PET data describing the relationship between MFR and the severity of epicardial coronary stenosis [23]. It has been reported that MFR decreases according to coronary artery stenosis severity. Hyperaemic response decreases at >40% diameter coronary artery stenosis and is abolished at >80% stenosis [23, 24]. In our study, MFR correlated inversely with stenosis severity in regions with significant coronary artery stenosis, but the risk factors did not influence MFR. Risk factors injure the endothelium-dependent relaxation of the coronary arteries. These changes play an important role in the development of early atherosclerotic lesions, characterised by functional alterations before morphological changes can be detected. As atherosclerotic changes progress, the structural changes are established and may overrun the functional changes induced by risk factors. Therefore, in regions with significant coronary artery stenosis, the influence of severity of coronary artery stenosis is likely to be greater than that of the risk factors. Accordingly, risk factors were not determinants of MFR in the stenotic regions. Kaufmann et al. reported that coronary vasomotion in response to physical exercise was correlated with risk factors in normal coronary arteries but not in stenotic arteries [25]. Our results are concordant with their report.
Recently, Vicario et al. demonstrated the influence of risk factors on MFR in patients with one-vessel disease [26]. In their study, MFR was inversely related to the number of risk factors in regions with intermediate coronary stenosis (50%–70%). As already mentioned, in our study there was no significant correlation between MFR and the number of risk factors in stenotic regions. When we divided stenotic regions according to coronary artery stenosis (50–70%, >70%), the results did not change. The major cause of the discrepancy may be the fact that we included patients with multivessel disease and then analysed only one stenotic region per person, i.e. the most severely stenotic. It may in fact be the case that coronary risk factors do have a greater influence on patients with multivessel disease than on those with one-vessel disease, but that this was obscured in the present study by the disregarding of second and third stenotic regions in many patients.
By contrast, in remote regions the risk factors did significantly affect MFR. It has been reported that patients with MI have attenuated MBF in the regions without coronary artery stenosis, so we excluded patients with a history of MI [27]. The finding of decreased MFR in the remote regions in patients without MI may be due to an abnormality in the microcirculation attributable to the coronary risk factors. In other studies, MFR has been found to be decreased in patients with coronary risk factors, such as diabetes mellitus, hypertension, hypercholesterolaemia and smoking [1–12]. These data suggest that decreased MFR may be due to an abnormality in the regulation of coronary flow and preclinical atherosclerosis. Therefore, MFR measurements are useful in assessing the functional significance of coronary artery stenosis and in predicting coronary artery atherosclerosis and microcirculation abnormality.
Fujiwara et al. found that MFR is preserved in regions supplied by angiographically normal coronary arteries without conventional risk factors. On the other hand, MFR was significantly decreased in patients with multiple risk factors [28]. This report is consistent with our finding that MFR in the remote regions was significantly attenuated in patients with multiple risk factors as compared with those who had one or no risk factors. Furthermore, we analysed the influence of each risk factor on MFR and found diabetes and smoking to be independent significant predictors of MFR. Because we included patients who received specific medication for each risk factor, the treatment may have influenced the results. Previous reports have shown that cholesterol-lowering therapy can improve myocardial perfusion and MFR [29–34]. Similarly, anti-hypertensive treatments (e.g. angiotensin-converting enzyme inhibitors, beta-blockers and calcium antagonists) have been found to improve MFR in hypertensive patients [35–39]. Therefore the small influence of hyperlipidaemia or hypertension on MFR in our patient population may have been due to the fact that these conditions had been well controlled by medications.
The importance of using 15O-labelled water is that the calculation of MBF is independent of the partial volume effect [40]. The elimination of the partial volume effect minimises the global underestimation of myocardial radioactivity [41]. 15O-labelled water is a metabolically inert, freely diffusible tracer whose incorporation into myocytes is independent of the myocardial metabolic state [42]. Therefore 15O-labelled water PET can measure MBF even in the high flow range, and MBF can accordingly be measured accurately during hyperaemia.
Clinical implications
Flow reserve provides a way of documenting how the risk factors cause measurable damage to the coronary circulation. PET is a non-invasive and accurate tool for estimating and monitoring regional absolute MBF and MFR. By this method, we were able not only to determine physiological estimates of the severity of coronary artery stenosis but also to assess preclinical atherosclerotic changes.
Impaired coronary vasodilator capacity has been shown to be an independent predictor of long-term prognosis in patients with hypertrophic and dilated cardiomyopathies [43, 44]. MFR may be important for long-term prognosis in patients with CAD or multiple risk factors.
Limitations
Several limitations of the present study need to be mentioned. First, the number of subjects in this study was small (n=74). It is necessary to increase the number of subjects, particularly for multivariate analysis.
Second, in this study, as mentioned above, patients continued taking their usual medications. We cannot rule out the possibility that the medications selectively affected coronary vasodilator reserve. The decision to continue administering patients’ usual medications was taken because most of the patients had severe CAD and received several different medications, and continued medication ensured stable conditions during the study.
Third, we did not consider the coronary artery stenoses in the distal part or minor branches or collateral flow in the occluded vessels. Because there is much individual variation in the anatomy of coronary arteries, it is difficult to consider these effects. Furthermore, stenosis in the distal part or minor branches usually has little influence on MBF.
Conclusion
MFR is determined not only by coronary artery stenosis severity but also by coronary risk factors. In particular, the influence of risk factors should be considered in regions without significant coronary artery stenosis.
References
Yokoyama I, Momomura S, Ohtake T, Yonekura K, Nishikawa J, Sasaki Y, et al. Reduced myocardial flow reserve in non-insulin-dependent diabetes mellitus. J Am Coll Cardiol 1997;30(6):1472–1477
Yokoyama I, Ohtake T, Momomura S, Yonekura K, Woo-Soo S, Nishikawa J, et al. Hyperglycemia rather than insulin resistance is related to reduced coronary flow reserve in NIDDM. Diabetes 1998;47(1):119–124
Opherk D, Mall G, Zebe H, Schwarz F, Weihe E, Manthey J, et al. Reduction of coronary reserve: a mechanism for angina pectoris in patients with arterial hypertension and normal coronary arteries. Circulation 1984;69(1):1–7
Treasure CB, Klein JL, Vita JA, Manoukian SV, Renwick GH, Selwyn AP, et al. Hypertension and left ventricular hypertrophy are associated with impaired endothelium-mediated relaxation in human coronary resistance vessels. Circulation 1993;87(1):86–93
Kozakova M, Palombo C, Pratali L, Pittella G, Galetta F, L’Abbate A. Mechanisms of coronary flow reserve impairment in human hypertension. An integrated approach by transthoracic and transesophageal echocardiography. Hypertension 1997;29(2):551–559
Laine H, Raitakari OT, Niinikoski H, Pitkanen OP, Iida H, Viikari J, et al. Early impairment of coronary flow reserve in young men with borderline hypertension. J Am Coll Cardiol 1998;32(1):147–153
Dayanikli F, Grambow D, Muzik O, Mosca L, Rubenfire M, Schwaiger M. Early detection of abnormal coronary flow reserve in asymptomatic men at high risk for coronary artery disease using positron emission tomography. Circulation 1994;90(2):808–817
Yokoyama I, Ohtake T, Momomura S, Nishikawa J, Sasaki Y, Omata M. Reduced coronary flow reserve in hypercholesterolemic patients without overt coronary stenosis. Circulation 1996;94(12):3232–3238
Yokoyama I, Ohtake T, Momomura S, Yonekura K, Nishikawa J, Sasaki Y, et al. Impaired myocardial vasodilation during hyperemic stress with dipyridamole in hypertriglyceridemia. J Am Coll Cardiol 1998;31(7):1568–1574
Kaufmann PA, Gnecchi-Ruscone T, Schafers KP, Luscher TF, Camici PG. Low density lipoprotein cholesterol and coronary microvascular dysfunction in hypercholesterolemia. J Am Coll Cardiol 2000;36(1):103–109
Czernin J, Sun K, Brunken R, Bottcher M, Phelps M, Schelbert H. Effect of acute and long-term smoking on myocardial blood flow and flow reserve. Circulation 1995;91(12):2891–2897
Kaufmann PA, Gnecchi-Ruscone T, di Terlizzi M, Schafers KP, Luscher TF, Camici PG. Coronary heart disease in smokers: vitamin C restores coronary microcirculatory function. Circulation 2000;102(11):1233–1238
Wangler RD, Peters KG, Marcus ML, Tomanek RJ. Effects of duration and severity of arterial hypertension and cardiac hypertrophy on coronary vasodilator reserve. Circ Res 1982;51(1):10–18
Vogt M, Motz W, Strauer BE. Coronary haemodynamics in hypertensive heart disease. Eur Heart J 1992;13(Suppl D):44–49
Gimelli A, Schneider-Eicke J, Neglia D, Sambuceti G, Giorgetti A, Bigalli G, et al. Homogeneously reduced versus regionally impaired myocardial blood flow in hypertensive patients: two different patterns of myocardial perfusion associated with degree of hypertrophy. J Am Coll Cardiol 1998;31(2):366–373
Czernin J, Muller P, Chan S, Brunken RC, Porenta G, Krivokapich J, et al. Influence of age and hemodynamics on myocardial blood flow and flow reserve. Circulation 1993;88(1):62–69
Uren NG, Camici PG, Melin JA, Bol A, de Bruyne B, Radvan J, et al. Effect of aging on myocardial perfusion reserve. J Nucl Med 1995;36(11):2032–2036
Furuyama H, Odagawa Y, Katoh C, Iwado Y, Yoshinaga K, Ito Y, et al. Assessment of coronary function in children with a history of Kawasaki disease using 15O-water positron emission tomography. Circulation 2002;105(24):2878–2884
Iwado Y, Yoshinaga K, Furuyama H, Ito Y, Noriyasu K, Katoh C, et al. Decreased endothelium-dependent coronary vasomotion in healthy young smokers. Eur J Nucl Med Mol Imaging 2002;29(8):984–990
Miyagawa M, Kumano S, Sekiya M, Watanabe K, Akutzu H, Imachi T, et al. Thallium-201 myocardial tomography with intravenous infusion of adenosine triphosphate in diagnosis of coronary artery disease. J Am Coll Cardiol 1995;26(5):1196–1201
Watanabe K, Sekiya M, Ikeda S, Miyagawa M, Kinoshita M, Kumano S. Comparison of adenosine triphosphate and dipyridamole in diagnosis by thallium-201 myocardial scintigraphy. J Nucl Med 1997;38(4):577–581
Katoh C, Ruotsalainen U, Laine H, Alenius S, Iida H, Nuutila P, et al. Iterative reconstruction based on median root prior in quantification of myocardial blood flow and oxygen metabolism. J Nucl Med 1999;40(5):862–867
Uren NG, Melin JA, De Bruyne B, Wijns W, Baudhuin T, Camici PG. Relation between myocardial blood flow and the severity of coronary-artery stenosis. N Engl J Med 1994;330(25):1782–1788
Di Carli M, Czernin J, Hoh CK, Gerbaudo VH, Brunken RC, Huang SC, et al. Relation among stenosis severity, myocardial blood flow, and flow reserve in patients with coronary artery disease. Circulation 1995;91(7):1944–1951
Kaufmann PA, Frielingsdorf J, Mandinov L, Seiler C, Hug R; Hess OM. Reversal of abnormal coronary vasomotion by calcium antagonists in patients with hypercholesterolemia. Circulation 1998;97(14):1348–1354
Vicario ML, Cirillo L, Storto G, Pellegrino T, Ragone N, Fontanella L, et al. Influence of risk factors on coronary flow reserve in patients with 1-vessel coronary artery disease. J Nucl Med 2005;46(9):1438–1443
Uren NG, Crake T, Lefroy DC, de Silva R, Davies GJ, Maseri A. Reduced coronary vasodilator function in infarcted and normal myocardium after myocardial infarction. N Engl J Med 1994;331(4):222–227
Fujiwara M, Tamura T, Yoshida K, Nakagawa K, Nakao M, Yamanouchi M, et al. Coronary flow reserve in angiographically normal coronary arteries with one-vessel coronary artery disease without traditional risk factors. Eur Heart J 2001;22(6):479–487
Gould KL, Martucci JP, Goldberg DI, Hess MJ, Edens RP, Latifi R, et al. Short-term cholesterol lowering decreases size and severity of perfusion abnormalities by positron emission tomography after dipyridamole in patients with coronary artery disease. A potential noninvasive marker of healing coronary endothelium. Circulation 1994;89(4):1530–1538
Treasure CB, Klein JL, Weintraub WS, Talley JD, Stillabower ME, Kosinski AS, et al. Beneficial effects of cholesterol-lowering therapy on the coronary endothelium in patients with coronary artery disease. N Engl J Med 1995;332(8):481–487
Huggins GS, Pastemak RC, Alpert NM, Fischman AJ, Gewirtz H. Effects of short-term treatment of hyperlipidemia on coronary vasodilator function and myocardial perfusion in regions having substantial impairment of baseline dilator reverse. Circulation 1998;98(13):1291–1296
Guethlin M, Kasel AM, Coppenrath K, Ziegler S, Delius W, Schwaiger M. Delayed response of myocardial flow reserve to lipid-lowering therapy with fluvastatin. Circulation 1999;99(4):475–481
Yokoyama I, Momomura S, Ohtake T, Yonekura K, Yang W, Kobayakawa N, et al. Improvement of impaired myocardial vasodilatation due to diffuse coronary atherosclerosis in hypercholesterolemics after lipid-lowering therapy. Circulation 1999;100(2):117–122
Vita JA, Yeung AC, Winniford M, Hodgson JM, Treasure CB, Klein JL, et al. Effect of cholesterol-lowering therapy on coronary endothelial vasomotor function in patients with coronary artery disease. Circulation 2000;102(8):846–851
Gistri R, Ebert AG, Palombo C, Marabotti C, Choudhury L, Camici PG. Effect of blood pressure lowering on coronary vasodilator reserve in arterial hypertension. Cardiovasc Drugs Ther 1994;8(1):169–171
Frielingsdorf J, Seiler C, Kaufmann P, Vassalli G, Suter T, Hess OM. Normalization of abnormal coronary vasomotion by calcium antagonists in patients with hypertension. Circulation 1996;93(7):1380–1387
Motz W, Strauer BE. Improvement of coronary flow reserve after long-term therapy with enalapril. Hypertension 1996;27(5):1031–1038
Billinger M, Seiler C, Fleisch M, Eberli FR, Meier B, Hess OM. Do beta-adrenergic blocking agents increase coronary flow reserve? J Am Coll Cardiol 2001;38(7):1866–1871
Galderisi M, Cicala S, D’Errico A, de Divitiis O, de Simone G. Nebivolol improves coronary flow reserve in hypertensive patients without coronary heart disease. J Hypertens 2004;22(11):2201–2208
Iida H, Rhodes CG, Araujo LI, Yamamoto Y, de Silva R, Maseri A, et al. Noninvasive quantification of regional myocardial metabolic rate for oxygen by use of 15O2 inhalation and positron emission tomography. Theory, error analysis, and application in humans. Circulation 1996;94(4):792–807
Wisenberg G, Schelbert HR, Hoffman EJ, Phelps ME, Robinson GD Jr, Selin CE, et al. In vivo quantitation of regional myocardial blood flow by positron-emission computed tomography. Circulation 1981;63(6):1248–1258
de Silva R, Camici PG. Role of positron emission tomography in the investigation of human coronary circulatory function. Cardiovasc Res 1994;28(11):1595–1612
Cecchi F, Olivotto I, Gistri R, Lorenzoni R, Chiriatti G, Camici PG. Coronary microvascular dysfunction and prognosis in hypertrophic cardiomyopathy. N Engl J Med 2003;349(11):1027–1035
Neglia D, Michelassi C, Trivieri MG, Sambuceti G, Giorgetti A, Pratali L, et al. Prognostic role of myocardial blood flow impairment in idiopathic left ventricular dysfunction. Circulation 2002;105(2):186–193
Author information
Authors and Affiliations
Corresponding author
Additional information
This study received no financial sponsorship.
Rights and permissions
About this article
Cite this article
Tsukamoto, T., Morita, K., Naya, M. et al. Myocardial flow reserve is influenced by both coronary artery stenosis severity and coronary risk factors in patients with suspected coronary artery disease. Eur J Nucl Med Mol Imaging 33, 1150–1156 (2006). https://doi.org/10.1007/s00259-006-0082-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00259-006-0082-x