Abstract
Purpose
We investigated whether a myocardial perfusion gradient during pharmacologically induced hyperemia also occurred during sympathetic stimulation with cold pressor testing (CPT), which commonly induces a paradoxical coronary vasoconstriction in individuals with coronary risk factors.
Methods
Myocardial blood flow (MBF) was measured in absolute units (ml/g/min) with 13N-ammonia and PET at rest, during CPT, and during pharmacologic vasodilation in 59 participants with coronary risk factors (“at risk”) and in 43 healthy individuals (controls). MBF was assessed globally as mean MBF, and in the mid and mid-distal myocardium of the left ventricle (LV). A decrease in MBF from mid to mid-distal LV myocardium was defined as MBF difference indicative of a perfusion gradient.
Results
The change in mean MBF to CPT (ΔMBF) in the at-risk group was significantly reduced compared with controls (0.05±0.19 vs 0.31±0.20 ml/g/min, p<0.0001), whereas mean MBF during pharmacologic vasodilation in the at-risk group tended to be lower than in controls (1.72±0.71 vs 2.00±0.64 ml/g/min, p=NS). Absolute MBFs during CPT and pharmacologic vasodilation were significantly lower in the mid-distal than in the mid LV myocardium, resulting in a significant MBF difference in the at-risk group (0.15±0.06 and 0.27±0.12 ml/g/min, p<0.0001) that was not observed in controls (0.007±0.05 and 0.014±0.10 ml/g/min, p=NS). In the at-risk group there was a significant correlation between the difference of mid to mid-distal MBF during CPT and that during pharmacologic vasodilation (r=0.43, p<0.004), suggesting functional alterations of epicardial vessels as the predominant cause for the observed MBF difference.
Conclusion
The relative decrease in MBF from the mid to the mid-distal left-ventricular myocardium suggests an intracoronary pressure decline during CPT and pharmacologic vasodilation, which is likely to reflect an impairment of flow-mediated epicardial vasomotor function.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
A longitudinal, base-to-apex myocardial perfusion gradient has previously been observed during pharmacologically stimulated hyperemia in patients with coronary artery disease (CAD) or with coronary risk factors [1–3]. This perfusion gradient has been attributed to fluid dynamic consequences of CAD-induced diffuse luminal narrowing or to functional alterations of the epicardial coronary conduit vessels [1, 2, 4]. Resistance to flow, as defined by the Hagen-Poiseuille equation for a simple rigid tube, is predominantly related to the velocity of flow and, importantly, inversely to the fourth power of the vessel diameter. In the normal coronary circulation, increases in flow velocity are associated with a flow-related and, thus, endothelium- and nitric oxide-mediated dilation of the epicardial conduit vessel which compensates for the velocity-induced increase in resistance, so that the resistance remains low [5, 6]. If, however, due to diffuse luminal narrowing or to an impairment of the flow-related dilation, the conduit vessel fails to dilate [6, 7], then as intracoronary pressure measurements have demonstrated, resistance to higher flows increases and a progressive proximal-to-distal decline in the intracoronary pressure occurs [4] that is associated with a gradual, base-to-apex decrease in myocardial perfusion [1, 2, 4].
Alternatively, such a perfusion gradient might also occur even if the flow velocity remains constant but the diameter of the conduit vessel decreases. In the presence of dysfunctional endothelium, a sympathetically induced functional decrease in epicardial conduit artery diameter may not be overcome by an adequate flow-mediated and, thus, endothelium-dependent vasodilation. Such a “paradoxical” coronary vasoconstriction may occur during mental stress or, as demonstrated by quantitative coronary angiography, during sympathetic stimulation with cold pressor testing (CPT) [7–12]. In this regard, PET-measured myocardial blood flow (MBF) combined with CPT may provide more selective information on coronary endothelium-dependent vasomotor function [7, 13–15]. The paradoxical vasoconstriction during CPT as observed in patients with diffuse CAD may also occur, as earlier investigations suggest, in individuals without clinically manifest CAD but with coronary risk factors [12–14, 16, 17].
Thus, by means of 13N-ammonia PET measurement of MBF, we aimed to explore whether a previously described myocardial perfusion gradient during hyperemic flow increases ascribed to epicardial wall stiffness also occurs during sympathetic stimulation with CPT, which commonly induces a paradoxical, functional decrease in coronary artery diameter in individuals with risk factors for CAD.
Materials and methods
Patient population
The study population consisted of 102 asymptomatic participants (44 men, 58 women; age 44±10 years) (Table 1). They were grouped according to the presence or absence of coronary risk factors. Fifty-nine participants (27 men, 32 women; age 45±11 years) with coronary risk factors were assigned to the “at-risk” group, while 43 age-matched healthy individuals without coronary risk factors (17 men, 26 women; age 43±13 years) were assigned to a normal control group. A prerequisite for study inclusion was the absence of perfusion defects on semiquantitative evaluation of PET images during pharmacologically induced hyperemia that argued against the presence of hemodynamically significant obstructive CAD. Further exclusion criteria were evidence of left ventricular hypertrophy on the electrocardiogram and use of cholesterol-lowering statin medication. Vasoactive medications, including calcium channel blockers, β-blockers, and diuretics, were discontinued at least 24 h before MBF assessment by means of PET. Angiotensin-converting enzyme (ACE) inhibitors were discontinued 3 days before the study session. In the at-risk group, 12 individuals had hypercholesterolemia [total cholesterol ≥240 mg/dl; low-density lipoprotein (LDL) cholesterol ≥160 mg/dl], 19 were long-term smokers (>10 pack-years), 14 had newly diagnosed type 2 diabetes (fasting plasma glucose ≥126 mg/dl), seven had insulin resistance by the homeostasis model approximation (homeostasis model insulin resistance) [15] and seven had hypertension (blood pressure of ≥140/90 mmHg; average of three measurements over 1 month). Thirty-six individuals had one coronary risk factor, 21 patients had two, and two patients had three coronary risk factors.
The normal controls had a <5% probability of CAD, because cardiovascular symptoms like angina pectoris or dyspnea were absent, and the physical examination and the rest ECG were normal [18]. All women in the normal control group had regular menses and were not on birth control. They were studied at mid-cycle of the menstrual period. In the at-risk group, seven women were premenopausal; three were long-term smokers, one had hypercholesterolemia, one had diabetes and one had insulin resistance. The remaining 25 women were postmenopausal (cessation of menses ≥1 year) and were not on hormone replacement therapy. All study participants refrained from caffeine-containing beverages for ≥24 h and from smoking for ≥4 h prior to study, and all were in a fasting state. Each study participant signed the informed consent form as approved by the UCLA Medical Institutional Review Board. MBF analysis of 44 of these study participants was reported in previous studies employing pharmacologic vasodilation with dipyridamole [19, 20]. Thus, the latter dipyridamole MBF studies were re-analysed retrospectively, while in the remaining participants adenosine-induced MBF increases were evaluated prospectively.
Measurement of MBF with PET
A whole-body PET scanner (ECAT EXACT HR +, Siemens/CTI model 931/08-12) with an effective isotropic resolution of 10mm full-width at half-maximum and a 15.5-cm axial field of view was used [21]. First, transmission images were recorded for 20 minutes. Beginning with each intravenous 13N-ammonia injection [555–740 MBq (15–20 mCi)], transaxial image sets were acquired serially (12 frames of 10 s each, two frames of 30 s each, one frame of 60 s and one frame of 900 s). Measurements were performed first at baseline, then during CPT and finally, during pharmacologically induced hyperemia. Forty-five minutes were allowed between MBF measurements for physical decay of 13N-ammonia [21]. For the CPT, study participants immersed the left hand in ice water for 60 s when 13N-ammonia was injected, while CPT continued for another 60 s [13].
Vasodilation was induced pharmacologically with standard infusion of adenosine or dipyridamole (140 μg/kg/min) as described previously [22]. Both vasodilator agents have been shown to induce comparable levels of hyperemia [22]. The serially acquired transaxial image sets were reoriented into short-axis images and assembled into polar maps. The reoriented 13N-ammonia images and the corresponding polar maps were generated from the last, 900-s image set and they were subjected to visual and semi-quantitative visual analysis. Heart rate (HR), blood pressure (BP), and a 12-lead ECG were recorded continuously during each MBF measurement. From the average of HR and BP during the first 2 min of each image acquisition, the rate–pressure product (RPP) was determined as an index of cardiac work.
Quantitative evaluation of MBF
On the polar map of the last 900-s image set, regions of interest (ROIs) were assigned to the territories of the three coronary arteries (Fig. 1). In addition, two circumferential ROIs were assigned to the mid and the mid-distal portion of the left ventricular (LV) myocardium, as also illustrated in Fig. 1. The ROIs were then copied to the serial polar maps acquired during the first 2 min after tracer injection and regional time-activity curves were generated. In addition, a small, 25-mm2 ROI was assigned to the LV blood pool on the most basal short-axis slice for derivation of the arterial tracer input function. Corrections of the myocardial time-activity curves used a recovery coefficient that assumed a uniform, 1-cm-thick LV myocardium [23]. The time-activity curves were corrected for physical decay and were fitted with a previously validated two-compartment tracer kinetic model [21, 24]. Since MBFs in absolute estimates (ml/g/min) in the myocardial territory of the left anterior descending artery, left circumflex artery, and right coronary artery were similar, they were averaged and the resulting global MBF of the LV was subsequently indicated as mean MBF. Further, a decrease in MBF from mid to mid-distal LV myocardium was defined as MBF difference (in ml/g/min) indicative of a perfusion gradient. Changes in the MBF difference from baseline to hyperemia or to CPT were defined as ΔMBF difference (MBF difference during hyperemia or CPT minus MBF difference at baseline).
Data analysis
Mean values are given with standard deviations. Hemodynamic parameters, mean MBF, and MBF in the mid and the mid-distal circumferential ROIs at rest, during CPT, and during hyperemia were analysed by repeated-measures ANOVA. Post hoc comparisons were made by means of Scheffé analysis, which examines the differences between any two means while controlling the significance level. Correlations between selected variables were estimated by Spearman correlation coefficients. All test procedures were two-sided with a p value ≤0.05, indicating statistical significance.
Results
Clinical characteristics
Table 1 summarizes the clinical characteristics of the study population. Serum levels of total cholesterol, triglyceride, and glucose were higher in the at-risk group than in the control group, while LDL and HDL levels were similar. Moreover, the body mass index (BMI) was significantly higher in the at-risk than in the control group. Of the study participants with hypertension, two were receiving combined medical treatment with β-blockers and ACE inhibitors, one person, treatment with β- and calcium channel blockers, and four participants, treatment with diuretics alone (Table 1).
Hemodynamic parameters
At baseline, heart rate and blood pressures were similar in the two study groups (Table 2). CPT induced significant increases in heart rate and systolic and diastolic blood pressure (p<0.05) that were similar in the two study groups. Accordingly, RPPs did not differ between the two groups either at baseline or during CPT (Table 2). Also, as listed in Table 2, pharmacologic vasodilation produced significant increases in heart rate in both study groups (p<0.05), while systolic and diastolic blood pressures remained essentially unchanged from baseline. No significant differences in heart rate or RPP existed between the two study groups during pharmacologic vasodilation. Finally, adenosine and dipyridamole produced comparable hemodynamic responses in both study groups so that, as listed in Table 2, heart rates and RPPs were similar during adenosine and dipyridamole stimulation in the normal controls and in the at-risk group.
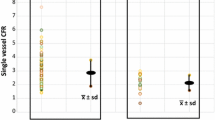
Global MBF during cold pressor testing and pharmacological vasodilation
Quantitative evaluation of global LV MBF at rest revealed comparable mean MBFs for both study groups (Table 2, Fig. 2). There was a significant increase in mean MBF from rest to CPT in the control (p<0.0001), but not in the at-risk group (p=NS) (Table 2, Fig. 2). During CPT, flows had not significantly increased from baseline in the at-risk group (p=NS), so that the mean MBF was significantly lower than in the control group (p<0.0001) (Fig. 2). Accordingly, the change in mean MBF from rest to CPT (ΔMBF) in the at-risk group was also significantly reduced as compared with the control group (0.05±0.19 vs 0.31±0.20 ml/g/min, p<0.0001). The attenuation of the flow response to CPT was independent of the specific risk factor (Table 3). Further, when the at-risk study participants were divided into subgroups by risk factor or the number of risk factors, mean MBFs were found on ANOVA to be similar among the subgroups and to be equally diminished when compared with those of the normal controls (Tables 2, 3).
Pharmacologically induced vasodilation caused a significant increase in mean MBF from baseline in both study groups (p<0.0001) (Table 2). The mean MBF during pharmacologic vasodilation tended to be lower in the at-risk than in the normal control group although this difference did not achieve statistical significance (Table 2, Fig. 2). No inter-group differences between adenosine and dipyridamole hyperemic mean MBFs were noted (control group: 0.66±0.14 to 1.85±0.50 vs 0.65±0.13 to 2.1± 0.73 ml/g/min; at-risk group: 0.68±0.16 to 1.71±0.75 vs 0.70±0.15 to 1.72±0.67 ml/g/min; p=NS), nor were there any significant differences in mean hyperemic MBFs when study participants were divided into subgroups by risk factors or by the number of risk factors (p=NS by ANOVA) (Table 3).
MBF differences during hyperemia and cold pressor testing
In the normal controls, pharmacologic vasodilation raised MBFs homogeneously, resulting in near-identical mid and mid-distal LV MBF during hyperemia (Fig. 3). In the at-risk individuals, however, pharmacologic vasodilation induced a heterogeneous flow response. While MBF during hyperemia in the mid LV reached similar levels to those in the normal controls (p=NS) (Fig. 3), the flow increase was significantly less in the mid-distal LV myocardium (Fig. 3). On average, MBFs during pharmacologic vasodilation differed by 0.27±0.12 ml/g/min (MBF difference) in the mid and mid-distal LV myocardium in the at-risk participants as compared to only 0.014±0.10 ml/g/min in the normal controls (Table 2, Fig. 4). CPT similarly induced heterogeneities in MBF in the at-risk individuals. MBF rose to 0.82±0.20 ml/g/min in the mid LV myocardium, but only to 0.67±0.20 ml/g/min in the mid-distal LV myocardium (Fig. 3). This resulted in an MBF difference of 0.15±0.06 ml/min/g between the mid and mid-distal LV myocardium (Table 2, Fig. 4). There was no MBF difference in normal controls (0.007±0.05 ml/g/min) (Table 2 and Fig. 4). Mid and mid-distal LV MBF in the normal volunteers averaged 0.96±0.26 and 0.96±0.25 ml/g/min, respectively, during CPT (Fig. 3). When the at-risk individuals were divided into subgroups by coronary risk factors or the number of coronary risk factors, again no significant inter-group differences in MBF differences were noted on ANOVA (Table 3). The observed MBF differences therefore did not appear to be related to the type of coronary risk factor. Also, no relationship was observed between the MBF differences during CPT or pharmacologic vasodilation and age (r=0.12 and r=0.06, p=NS). Grouping the at-risk individuals by the median age of 47 years into younger and older study participants, similar MBF differences during CPT and pharmacologic vasodilation were observed (0.15±0.05 vs 0.14±0.07 and 0.28±0.12 vs 0.26±0.12 ml/g/min; p=NS) in the 29 and 30 individuals with an average age of 36±7 and 54±5 years, respectively.
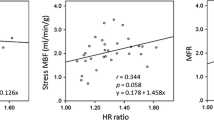
Cold pressor and vasodilator stress and MBF difference
Possible dependence of the stress-induced heterogeneities in MBF on the magnitude of the cold pressor or the vasodilator stress was examined. The magnitude of the pharmacologic vasodilation was estimated from the mid-LV MBF. This appeared to be justified because flows in the mid LV were assumed to be affected less by possible coronary vasomotor abnormalities as compared to flows in the mid-distal LV. This assumption is also in line with the findings of the current study that the mid LV MBFs were similar to the hyperemic MBFs in the normal volunteers (Fig. 3). As seen in Fig. 5, MBF differences in the at-risk individuals correlated significantly with the mid LV MBF during both pharmacologically induced hyperemia and CPT (Fig. 5a,b), implicating the velocity of coronary blood flow as a determinant of the MBF differences or the mid to mid-distal myocardial flow gradient. Further, as Fig. 5c illustrates, MBF differences during hyperemia were correlated with those during CPT, which may suggest an impairment of coronary vasomotor function at the site of the epicardial conduit vessels as the cause for the perfusion gradient.
In contrast to these flow increase studies, CPT-induced MBF differences were unrelated to the blood flow changes. As depicted in Fig. 6, CPT raised global mean MBF in proportion to the increase in RPP and, thus, in cardiac work in the normal controls (Fig. 6a) but not in the at-risk individuals (Fig. 6b). The latter finding in the at-risk group implies an uncoupling of impaired endothelium-dependent vasomotion from the CPT-induced metabolic demand. On average, mean MBF in these at-risk individuals remained unchanged from baseline despite significant increases in cardiac work (Fig. 2). Nevertheless, the ΔMBF difference during CPT increased in magnitude with the increase in RPP in the at-risk individuals (Fig. 6d) while it remained essentially unchanged in the normal volunteers (Fig. 6c). Thus, in the at-risk individuals higher increases in the RPP during sympathetic stimulation with CPT were associated with a greater ΔMBF difference. Since in the at-risk group no marked increase in MBF during CPT was observed (Fig. 2), the significant correlation between the increase in RPP and the ΔMBF difference in the at-risk individuals (Fig. 6d) suggests a sympathetically induced decrease in coronary artery diameter that accounted for the MBF difference or mid to mid-distal flow gradient during CPT.
Discussion
The major finding of the current study is the heterogeneous response of regional MBF to sympathetic stimulation with cold pressor testing (CPT) in individuals without clinically manifest CAD but with coronary risk factors not observed in healthy controls. The heterogeneous blood flow response resulted in a mid to mid-distal myocardial perfusion gradient in individuals with coronary risk factors. In contrast to the previously observed perfusion gradient during pharmacologic vasodilation [1, 2], the perfusion gradient occurred in the absence of an increase in global left ventricular MBF. This could be consistent with our hypothesis that the perfusion gradient likely resulted from a decrease in luminal diameter, predominantly of the epicardial coronary vessel, that raised the resistance to coronary flow [9], which remained constant and caused a proximal-to-distal decline in intracoronary perfusion pressure [4]. Notably, the present study is the first to confirm that both sympathetic and pharmacologic stimuli, commonly used in the assessment of coronary vasomotion, are indeed associated with an abnormal perfusion gradient in individuals with coronary risk factors. Such a perfusion gradient as measured with PET has been suggested to reflect early functional and/or structural alterations of the epicardial artery [1, 2].
The myocardial perfusion gradient during pharmacologic vasodilation as described previously [1, 2] and as observed in the current study has been ascribed to complex interplay between intracoronary flow velocity increases and luminal changes of the epicardial conduit vessel. According to the Hagen-Poiseuille equation, major determinants of the resistance to coronary flow include the velocity of blood flow and the fourth power of the vessel diameter. Higher flow velocities, as encountered during pharmacologic vasodilation, are associated in the normal coronary circulation with the flow-related increase in diameter of the conduit vessel so that the resistance to coronary flow remains essentially constant. If the flow-related and, thus, endothelium-mediated vasodilation is attenuated or even absent, as reported in patients with diffuse CAD or with coronary risk factors [7, 9, 11, 13, 14, 16], then the resistance to flow increases and, as demonstrated through invasive measurements [4], intracoronary pressure progressively declines from proximal to distal along the coronary conduit vessels. CAD-induced diffuse luminal narrowing, increased stiffness of the arterial wall and impairment of the flow-related conduit vessel dilation [1, 2, 11, 13] due to a decrease in the bioavailability of the endothelium-derived nitric oxide have been proposed as possible explanations [25–27].
As the current findings indicate, a perfusion gradient may also occur during sympathetic stimulation with CPT despite only modest or even absent increases in global MBF. Consequently, just the absence of the normally flow-related conduit vessel dilation is unlikely to account for the observed perfusion gradient. More likely is an actual decrease in the vessel diameter that for the same coronary flow would lead to an increase in resistance and thus to a progressive proximal-to-distal decline in intracoronary pressure. Several investigations have indeed reported such a decrease in luminal diameter or paradoxical vasoconstriction of the epicardial conductance vessels in patients with diffuse CAD or with coronary risk factors but without angiographic evidence for atherosclerotic disease [7, 10–13, 16, 17]. If, as previous investigations have suggested [28], increases in heart rate and blood pressure in response to CPT are related to an increase in serum norepinephrine concentrations as a measure of the degree of sympathetic stimulation, then the observed association between increases in rate–pressure product and the perfusion gradient suggests that the severity of the perfusion gradient is related to the degree of sympathetic stimulation. And indeed, in the current study we found that in the at-risk individuals higher increases in the rate–pressure product during sympathetic stimulation with CPT were associated with a greater magnitude of the perfusion gradient.
It was observed in the current study that the normal metabolically mediated increase in global myocardial (or coronary) blood flow in response to increases in cardiac work was diminished or even absent following sympathetic stimulation; this supports the findings of previous investigations [11, 13, 14, 29] and indicates that the vasoconstrictor effect of sympathetic stimulation may affect not only the coronary conductance but also the coronary arteriolar vessels [11, 13]. Such vasoconstriction in the coronary arteriolar vessels, associated with an increase in vascular resistance, may in fact have offset the magnitude of the perfusion gradient during CPT, resulting in a less pronounced gradient than one might have expected. Conversely, because no marked increase in global MBF was observed in the at-risk group during CPT, the significant correlation between the increase in rate–pressure product and the magnitude of the perfusion gradient may suggest that a sympathetically induced vasoconstriction, predominantly at the site of the conduit vessels, accounts for the perfusion gradient. Notably, the development of a perfusion gradient during CPT, as observed in the current study, is consistent with previous invasive findings [9]. In the latter study, quantitative coronary angiography, combined with intracoronary flow velocity measurements, demonstrated an increase in intravascular shear stress (or resistance to flow) during CPT in patients with diffuse CAD, while coronary flow remained constant but, importantly, the luminal diameter of the conduit vessel decreased [9]. Possible explanations for the perfusion gradient in the current study include CAD-induced diffuse luminal narrowing [1], structural alterations of the coronary arterial wall with an increase in vessel stiffness [30] and functional alterations of the vasomotor control [7, 10–13, 16, 17]. While CAD and structural alterations of the arterial wall could have been excluded by coronary angiography and intracoronary ultrasound, for ethical reasons their use could not be justified in the current study, given that the patients were asymptomatic. In this regard, normal stress and rest myocardial perfusion images with 13N-ammonia and PET, as inclusion criteria in the study population, argued at least against the presence of hemodynamically significant obstructive coronary artery lesions, but, of course, CAD-induced early and subclinical structural alterations of the artery wall may have been present. Consequently, in the current study an increase in vessel wall stiffness due to structural alterations of the arterial wall, including intimal thickening (as associated with coronary risk factors [30]), may, in conjunction with functional alterations of the coronary circulation, indeed have accounted for the perfusion gradient during sympathetic stimulation [13, 14, 17]. Coronary risk factors such as arterial hypertension, insulin resistance or diabetes may induce myocardial remodeling involving structural components of the myocytes in addition to the occurrence of fibrosis [31]. In such patients, even in the absence of clinically evident left ventricular hypertrophy, higher extravascular resistive forces may also contribute to the manifestation of the perfusion gradient [32]. Conceptually, an increase in age-related stiffness of the coronary artery wall might also mechanistically diminish the ability of the vessel to dilate and give rise to the observed abnormal perfusion gradient. In the current study population, however, there was no association between the perfusion gradient in response to CPT or pharmacologic vasodilation and the age of the individual study participants, nor was the perfusion gradient dependent on the type of coronary risk factors. Thus, the observed perfusion gradient did not appear to be related to age-induced structural alterations of the vessel wall or the type of coronary risk factors. This suggests a common functional abnormality of the coronary vasomotor response as the predominant cause for the perfusion gradient. The impairment of the flow-related predominantly epicardial vasodilator response and its severity, however, may account for the observed statistically significant correlation between the perfusion gradients during CPT and those during pharmacological vasodilation.
It is important to bear in mind, however, that in the present study the perfusion gradient was noted only when MBF during pharmacologic vasodilation was measured in absolute units (ml/g/min), and not when the relative 13N-ammonia tracer uptake was evaluated on polar maps. Several factors may explain these discordant observations. First, it is possible that in our study, participants had less severe CAD-induced structural alterations of the arterial wall, as described in previous investigations [1, 3], which may have resulted in a less pronounced perfusion gradient. Second, myocardial 13N-ammonia concentrations as net radionuclide uptake correlate with MBF in a non-linear fashion [21]. This is because metabolic trapping of 13N-ammonia in the myocardium competes with flow-dependent back diffusion, so that at higher flows a greater fraction of 13N-ammonia returns from the extravascular space into the blood pool. This competition causes a progressive decline in the 13N-ammonia retention fraction with increase in blood flow. Thus, the portion of the curve that describes net radionuclide uptake of 13N-ammonia and MBF is relatively flat in the hyperemic flow range [21]. To balance this limitation, MBF-calculating radiotracer kinetic models are applied that correct for the declining radionuclide retention at higher coronary flow rates [21, 33]. Relative regional differences in radionuclide uptake are then magnified into greater differences in absolute MBF with any flow-calculating tracer kinetic model, depending on the flow rate and the radionuclide [3]. This may explain why the assessment of absolute MBF (ml/g/min) identifies perfusion gradient abnormalities even in the absence of objectively quantified relative regional perfusion defects [2, 3, 33]. Third, the MBF gradient was determined in our study only over a relatively short longitudinal distance between mid and mid-distal LV myocardium in order to avoid confounding partial volume effects on MBF measurements in the apical portion of the heart. Thus, the perfusion gradient in our study was of less magnitude than that described previously by Gould et al. [1] with a different analysis approach.
Clinical implications
The observation of a longitudinal, mid to mid-distal LV MBF gradient during sympathetic stimulation has potential clinical implications. One is that it may contribute to the non-invasive identification of developing, early coronary atherosclerosis in the absence of regional stress-induced perfusion defects. The presence of such a perfusion gradient would also suggest that the disease process affects not only the coronary microcirculation but also the function of the coronary epicardial conductance vessels [13]. Secondly, although constriction of the conductance vessels in the absence of coronary stenosis is less likely to occur during physical exercise, as demonstrated by invasive investigations of the coronary vasomotor response during exercise [34], the perfusion gradient may be associated with activities occurring during daily life in patients with CAD. For example, even in individuals without CAD but with coronary risk factors, the sympathetically mediated responses to mental stress may lead to MBF heterogeneities [8]. As increases in cardiac work in such individuals are then not accompanied by appropriate increases in MBF, such sympathetically induced episodes during daily life may be associated with transient ischemic episodes [35].
Conclusion
The relative decrease in MBF from the mid to mid-distal LV myocardium suggests a decline in intracoronary pressure during CPT and pharmacologic vasodilation, which is likely to reflect an impairment of flow-mediated epicardial vasomotor function. Thus, PET measurements of stress-induced regional MBF heterogeneity could be a promising tool to probe non-invasively flow-dependent epicardial vasomotion. While such inferences may be intuitively correct, they still await direct confirmation through prospective invasive angiographic investigations.
References
Gould KL, Nakagawa Y, Nakagawa K, Sdringola S, Hess MJ, Haynie M, et al. Frequency and clinical implications of fluid dynamically significant diffuse coronary artery disease manifest as graded, longitudinal, base-to-apex myocardial perfusion abnormalities by noninvasive positron emission tomography. Circulation 2000;101:1931–1939.
Hernandez-Pampaloni M, Keng FY, Kudo T, Sayre JS, Schelbert HR. Abnormal longitudinal, base-to-apex myocardial perfusion gradient by quantitative blood flow measurements in patients with coronary risk factors. Circulation 2001;104:527–532.
Sdringola S, Patel D, Gould KL. High prevalence of myocardial perfusion abnormalities on positron emission tomography in asymptomatic persons with a parent or sibling with coronary artery disease. Circulation 2001;103:496–501.
De Bruyne B, Hersbach F, Pijls NH, Bartunek J, Bech JW, Heyndrickx GR, et al. Abnormal epicardial coronary resistance in patients with diffuse atherosclerosis but “normal” coronary angiography. Circulation 2001;104:2401–2406.
Drexler H, Zeiher AM, Wollschlager H, Meinertz T, Just H, Bonzel T. Flow-dependent coronary artery dilatation in humans. Circulation 1989;80:466–474.
Cox DA, Vita JA, Treasure CB, Fish RD, Alexander RW, Ganz P, et al. Atherosclerosis impairs flow-mediated dilation of coronary arteries in humans. Circulation 1989;80:458–465.
Zeiher AM, Drexler H, Wollschlager H, Just H. Modulation of coronary vasomotor tone in humans. Progressive endothelial dysfunction with different early stages of coronary atherosclerosis. Circulation 1991;83:391–401.
Schoder H, Silverman DH, Campisi R, Karpman H, Phelps ME, Schelbert HR, et al. Effect of mental stress on myocardial blood flow and vasomotion in patients with coronary artery disease. J Nucl Med 2000;41:11–16.
Zeiher AM, Drexler H. Coronary hemodynamic determinants of epicardial artery vasomotor responses during sympathetic stimulation in humans. Basic Res Cardiol 1991;86 (Suppl 2):203–213.
Nabel EG, Ganz P, Gordon JB, Alexander RW, Selwyn AP. Dilation of normal and constriction of atherosclerotic coronary arteries caused by the cold pressor test. Circulation 1988;77:43–52.
Schindler TH, Nitzsche EU, Munzel T, Olschewski M, Brink I, Jeserich M, et al. Coronary vasoregulation in patients with various risk factors in response to cold pressor testing: contrasting myocardial blood flow responses to short- and long-term vitamin C administration. J Am Coll Cardiol 2003;42:814–822.
Schindler TH, Hornig B, Buser PT, Olschewski M, Magosaki N, Pfisterer M, et al. Prognostic value of abnormal vasoreactivity of epicardial coronary arteries to sympathetic stimulation in patients with normal coronary angiograms. Arterioscler Thromb Vasc Biol 2003;23:495–501.
Schindler TH, Nitzsche EU, Olschewski M, Brink I, Mix M, Prior J, et al. PET-measured responses of MBF to cold pressor testing correlate with indices of coronary vasomotion on quantitative coronary angiography. J Nucl Med 2004;45:419–428.
Zeiher AM, Drexler H, Wollschlager H, Just H. Endothelial dysfunction of the coronary microvasculature is associated with coronary blood flow regulation in patients with early atherosclerosis. Circulation 1991;84:1984–1992.
Prior JO, Quinones MJ, Hernandez-Pampaloni M, Facta AD, Schindler TH, Sayre JW, et al. Coronary circulatory dysfunction in insulin resistance, impaired glucose tolerance, and type 2 diabetes mellitus. Circulation 2005;111:2291–2298.
Schindler TH, Nitzsche EU, Olschewski M, Magosaki N, Mix M, Prior JO, et al. Chronic inflammation and impaired coronary vasoreactivity in patients with coronary risk factors. Circulation 2004;110:1069–1075.
Zeiher AM, Drexler H, Wollschlaeger H, Saurbier B, Just H. Coronary vasomotion in response to sympathetic stimulation in humans: importance of the functional integrity of the endothelium. J Am Coll Cardiol 1989;14:1181–1190
Diamond GA, Forrester JS. Analysis of probability as an aid in the clinical diagnosis of coronary-artery disease. N Engl J Med 1979;300:1350–1358.
Campisi R, Nathan L, Pampaloni MH, Schoder H, Sayre JW, Chaudhuri G, et al. Noninvasive assessment of coronary microcirculatory function in postmenopausal women and effects of short-term and long-term estrogen administration. Circulation 2002;105:425–430.
Campisi R, Czernin J, Schoder H, Sayre JW, Marengo FD, Phelps ME, et al. Effects of long-term smoking on myocardial blood flow, coronary vasomotion, and vasodilator capacity. Circulation 1998;98:119–125.
Schelbert HR, Phelps ME, Huang SC, MacDonald NS, Hansen H, Selin C, et al. N-13 ammonia as an indicator of myocardial blood flow. Circulation 1981;63:1259–1272.
Chan SY, Brunken RC, Czernin J, Porenta G, Kuhle W, Krivokapich J, et al. Comparison of maximal myocardial blood flow during adenosine infusion with that of intravenous dipyridamole in normal men. J Am Coll Cardiol 1992;20:979–985.
Hutchins GD, Caraher JM, Raylman RR. A region of interest strategy for minimizing resolution distortions in quantitative myocardial PET studies. J Nucl Med 1992;33:1243–1250.
Kuhle WG, Porenta G, Huang SC, Buxton D, Gambhir SS, Hansen H, et al. Quantification of regional myocardial blood flow using 13N-ammonia and reoriented dynamic positron emission tomographic imaging. Circulation 1992;86:1004–1017.
Buus NH, Bottcher M, Hermansen F, Sander M, Nielsen TT, Mulvany MJ. Influence of nitric oxide synthase and adrenergic inhibition on adenosine-induced myocardial hyperemia. Circulation 2001;104:2305–2310.
Tawakol A, Forgione MA, Stuehlinger M, Alpert NM, Cooke JP, Loscalzo J, et al. Homocysteine impairs coronary microvascular dilator function in humans. J Am Coll Cardiol 2002;40:1051–1058.
Wyss CA, Koepfli P, Namdar M, Siegrist PT, Luscher TF, Camici PG, et al. Tetrahydrobiopterin restores impaired coronary microvascular dysfunction in hypercholesterolaemia. Eur J Nucl Med Mol Imaging 2005;32:84–91.
Victor RG, Leimbach WN, Jr., Seals DR, Wallin BG, Mark AL. Effects of the cold pressor test on muscle sympathetic nerve activity in humans. Hypertension 1987;9:429–436.
Nitenberg A, Ledoux S, Valensi P, Sachs R, Attali JR, Antony I. Impairment of coronary microvascular dilation in response to cold pressor-induced sympathetic stimulation in type 2 diabetic patients with abnormal stress thallium imaging. Diabetes 2001;50:1180–1185.
Kern MJ. Coronary physiology revisited: practical insights from the cardiac catheterization laboratory. Circulation 2000;101:1344–1351.
Fang ZY, Schull-Meade R, Downey M, Prins J, Marwick TH. Determinants of subclinical diabetic heart disease. Diabetologia 2005;48:394–402.
Hesse B, Meyer C, Nielsen FS, Sato A, Hove JD, Holm S, et al. Myocardial perfusion in type 2 diabetes with left ventricular hypertrophy: normalisation by acute angiotensin-converting enzyme inhibition. Eur J Nucl Med Mol Imaging 2004;31:362–368.
Kaufmann PA, Camici PG. Myocardial blood flow measurement by PET: technical aspects and clinical applications. J Nucl Med 2005;46:75–88.
Kaufmann PA, Frielingsdorf J, Mandinov L, Seiler C, Hug R, Hess OM. Reversal of abnormal coronary vasomotion by calcium antagonists in patients with hypercholesterolemia. Circulation 1998;97:1348–1354.
Panza JA, Quyyumi AA, Diodati JG, Callahan TS, Bonow RO, Epstein SE. Long-term variation in myocardial ischemia during daily life in patients with stable coronary artery disease: its relation to changes in the ischemic threshold. J Am Coll Cardiol 1992;19:500–506.
Acknowledgements
The authors wish to thank the PET Imaging and Cyclotron staff for their support in the imaging studies, Akiyaa Nickelson for preparing the illustrations, and Victoria Bender for her secretarial assistance. This work was supported by a Research Grant HL 33177, National Heart, Lung and Blood Institute, Bethesda, MD.
Author information
Authors and Affiliations
Corresponding author
Additional information
The authors have full control of all primary data and agree to allow EJNMMI to review the data if requested.
Rights and permissions
About this article
Cite this article
Schindler, T.H., Facta, A.D., Prior, J.O. et al. PET-measured heterogeneity in longitudinal myocardial blood flow in response to sympathetic and pharmacologic stress as a non-invasive probe of epicardial vasomotor dysfunction. Eur J Nucl Med Mol Imaging 33, 1140–1149 (2006). https://doi.org/10.1007/s00259-006-0069-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00259-006-0069-7