Abstract
Purpose
123I presents imaging problems owing to high-energy photon emission. We investigated the influence of collimators on 123I-MIBG heart/mediastinum ratios (H/M ratios). Secondly, we assessed the influence on H/M ratios of different activity concentrations, simulating clinical conditions. Thirdly, the value of scatter correction was assessed.
Methods
The AGATE cardiac phantom was filled with 123I in three sequential conditions: A, heart and mediastinal activity; B, adding lung activity; and C, adding liver activity (protocol I). In protocol II, myocardium and liver were filled with different activities ranging from low to high. For each condition, static anterior planar and single-photon emission computed tomography studies were acquired on a Siemens e.cam (SI) and a General Electric Millennium VG (GE) system, using low-energy high-resolution and medium-energy (ME) collimators for protocol I and only ME collimators for protocol II . For the SI camera, a triple energy window (TEW) scatter correction was applied.
Results
Planar H/M ratios were influenced by scatter and septal penetration from increasing amounts of liver activity. These effects were less pronounced for ME collimators. Although the TEW scatter correction increased ratios overall, TEW correction did not improve the relative differences between the ratios. TEW correction therefore does not add any benefit to obtain an accurate reflection of myocardial activity concentrations.
Conclusion
For straightforward implementation of semi-quantitative 123I-MIBG myocardial studies, we recommend the use of ME collimators without scatter correction.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Increased sympathetic neuronal activity, in patients with various cardiac diseases, has been related to disease severity and prognosis [1, 2]. Cardiac sympathetic neuronal function and activity can be assessed non-invasively by use of 123I-metaiodobenzylguanidine (MIBG), an analogue of noradrenaline [3]. In patients with chronic heart failure, angiotensin-converting enzyme inhibitors [4, 5], β-receptor antagonists [6–9] and spironolactone [10, 11] have been shown to ameliorate functional capacity and prognosis. Using semi-quantitative analysis, these beneficial effects were found to be associated with increased 123I-MIBG uptake and reduced washout. Since semi-quantitative analysis of cardiac 123I-MIBG uptake is characterised by a low inter-individual and within-subject variability [12], semi-quantitative cardiac 123I-MIBG scintigraphy has become a valuable tool for the non-invasive assessment of prognosis and the effect of therapeutic intervention.
In addition to the prime emission of 159-keV photons, 123I emits high-energy photons of more than 400 keV [approximately 2.87%, main contributor 529 keV (1.28%)]. These high-energy photons lead to penetration of the collimator septa and cause scatter detected in the 159-keV energy window. Regardless, low-energy (LE) collimators are frequently used for imaging 123I-MIBG [13]. Septal penetration affects estimation of the heart/mediastinum (H/M) ratio in 123I-MIBG imaging with an LE collimator [14]. Medium-energy (ME) collimators have been shown to improve quantitative accuracy in 123I studies at the expense of spatial resolution [13, 14]. In patients with overt heart failure, semi-quantitative analysis of cardiac 123I-MIBG studies is complicated by the decrease/absence of cardiac uptake. In this clinical condition the semi-quantitative analysis may be influenced by scatter from other organs (e.g. liver). However, data on the influence of collimator choice in 123I studies on semi-quantitative cardiac analysis are limited [14]. Especially data for single-photon emission computed tomography (SPECT) are lacking with regard to the influence of collimator choice on homogeneity of cardiac 123I-MIBG distribution under different clinical conditions.
An approach to reduce/eliminate scatter is post-acquisition pixel by pixel scatter correction from images acquired in energy windows above and below the photopeak window [15]. Data on the effect of this triple energy window (TEW) scatter correction method in 123I studies on semi-quantitative cardiac analysis are limited [14].
To assess the influence of LE and ME collimators in 123I-MIBG studies on semi-quantitative cardiac analysis, we first studied the influence of different collimators and gamma cameras on anterior planar H/M ratios using the AGATE cardiac phantom [16]. Secondly, we assessed the influence of different activity concentrations, simulating clinical conditions, on the homogeneity of cardiac MIBG distribution. In addition we assessed the effect of TEW scatter correction.
Materials and methods
Gamma cameras and collimators
A dual-head gamma camera system with a 3/8-in sodium iodide crystal (e.cam, Siemens) (SI) and a dual-head gamma camera system with a 5/8-in sodium iodide crystal (Millennium VG, General Electric Medical Systems) (GE) were used. Two types of collimator were tested: low energy high resolution (LEHR) and ME, as provided by the gamma camera manufacturers (Table 1). All collimators had a hexagonal parallel-hole design. The Siemens collimators were manufactured from lead foil and the General Electric collimators were cast.
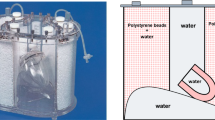
AGATE cardiac phantom
The Amsterdam 3D gated cardiac phantom (AGATE phantom) is a realistic 3D electrocardiogram (ECG) gated cardiac phantom with known left ventricular volumes and ejection fractions. This AGATE phantom was designed and constructed as an insert in the Data Spectrum anthropomorphic torso phantom, and initially developed to evaluate quantitative measurements obtained from gated myocardial SPECT [16].
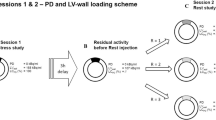
For this study, the AGATE phantom was configured with a fixed left ventricular myocardial volume of 80 ml, uniform myocardial wall activity and thickness, and a left ventricular cavity volume of 120 ml. Data acquisition was performed without applying ECG gating. The compartmental volumes of the anthropomorphic torso phantom were 10,300 ml for mediastinum (after insertion of the cardiac phantom insert), 330 and 360 ml for right and left lungs, respectively (after filling with Styrofoam beads), and 1,200 ml for liver.
Study protocol I: LEHR versus ME collimators (LEHR vs ME)
The AGATE cardiac phantom myocardial compartment (heart) and anthropomorphic phantom compartments were filled with a solution of 123I in three sequential conditions: A, heart (25 kBq/ml; 2 MBq) and mediastinum (1 kBq/ml; 10 MBq) activity; B, adding lung activity (5 kBq/ml; 4 MBq); C, adding liver activity (33.3 kBq/ml; 40 MBq). Static anterior planar and SPECT studies were acquired for each condition. Three planar and three SPECT data sets (A, B and C) were thus generated for each camera–collimator combination (Table 2).
Study protocol II: different clinical conditions
To mimic different clinical conditions, the AGATE cardiac phantom was filled to produce six conditions, each with a constant concentration of 123I in the mediastinum and lungs, but with different combinations of heart and liver concentrations (Table 2): D, low heart activity (12.5 kBq/ml; 1 MBq), mediastinum (1 kBq/ml; 10 MBq), lungs (5 kBq/ml; 4 MBq) and no liver activity; E, low heart activity and normal liver activity (33.3 kBq/ml; 40 MBq); F, normal heart activity (25 kBq/ml; 2 MBq) and normal liver activity; G, low heart activity and high liver activity (66.6 kBq/ml; 80 MBq); H, normal heart activity and high liver activity; I, high heart activity (100 kBq/ml; 4 MBq) and high liver activity.
Static anterior planar and SPECT studies were acquired for each condition using only the ME collimator. Six planar and SPECT data sets were thus generated for each camera–ME collimator combination (Table 2). Protocols I and II were performed on two separate days. At the end of each series of acquisitions for a particular filling condition, samples were taken and measured in a gamma well counter, in order to verify the activity concentration in the different compartments. The measured activity concentration values corresponded to those expected. Condition F, which equals condition C of protocol I, was incorporated in order to check for reproducibility between the two experiments.
Acquisition parameters
For both SI and GE cameras, 123I was imaged with a 15% energy window set symmetrically over the 159-keV photopeak. For SI only, images were acquired with triple energy windows (TEW), in order to study the influence of scatter correction on H/M ratios. This option was available only on the SI camera. The prime photopeak energy window of 15% window width was centred on the 159-keV photopeak and a contiguous scatter window of 7% of the 159-keV photopeak was set below and above the prime window.
In order to normalise for differences in pixel size, data acquisitions were zoomed with a factor of 1.34 and 1.45 for the GE and SI, respectively. The static anterior planar images were acquired for 5 min in a 128×128 matrix with a pixel size of 3.3 mm. SPECT acquisitions were performed with the 15% prime photopeak energy window only, over 360°, step and shoot, 30 projections per head each rotating 180°, 45 s per projection, 64×64 matrix, with a pixel size of 6.6 mm, and the auto-contour facility of the cameras. No attenuation correction was applied.
Image analysis
Analysis was performed on the Hermes workstation (Hermes Medical Solutions). SI planar images of conditions C, D, E, G, H and I were corrected on a pixel basis using the TEW method as described by Ichihara et al. [15]. Scatter counts in each pixel were calculated using the following formula:
where Cscat=scattered counts in the prime photopeak image, Clow=counts in the lower energy window and Chigh=counts in the high-energy window. The ratio 15/14 represents the ratio of the prime photopeak window width and summed width of the scatter windows. Scatter-corrected pixel counts were calculated using the following formula:
where Ccorr=scatter-corrected counts in the prime photopeak image and Cprime=original counts in the prime photopeak image.
Planar acquisitions were aligned in X and Y to one reference image. Planar regions of interest (ROIs) for the whole heart, anterior myocardial segment and mediastinum were drawn once and applied to all planar images (Fig. 1a). The whole heart ROI encompasses the whole left ventricle, i.e. both myocardium and cavity. The myocardial ROI is the region of interest representing the anterior left ventricular wall.
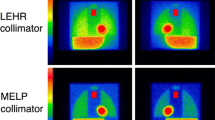
ROI definition and difference in image quality. a ROI definition on planar image. 1 mediastinum, 2 whole heart, 3 anterior myocardial wall. b ROI definition on SPECT short axis slice with whole myocardium and segmental anterior, inferior and septal ROIs. Difference in image quality between c ME and d LEHR
SPECT studies were pre-smoothed with a Wiener filter (used clinically), reconstructed with filtered back-projection and reoriented to generate short axis slices. Short axis slices were 3D reoriented to one reference condition. Three successive mid-ventricular short axis slices were added and ROIs drawn for the whole myocardium (whole heart) and anterior, inferior and septal myocardial segments. All ROIs were applied to equivalent slices in different SPECT studies (Fig. 1b).
For all imaging conditions and acquisitions, H/M ratios for whole heart and regional segments were obtained from ROI counts/pixel, which were corrected for physical decay of 123I so that count densities could be directly compared. H/M ratios were calculated for both uncorrected and scatter-corrected conditions for SI only. For comparison of LEHR and ME collimators, the H/M ratios were normalised to filling condition A, and expressed as percentages. For comparison of count densities within anterior, inferior and septal segments in the SPECT studies, the average count density in each ROI segment was compared with the average count density of the total myocardium ROI. Assuming that the count density within the total myocardium of the AGATE cardiac phantom should be uniform, the percentage difference between segmental count density and average total myocardium count density was calculated.
Results
Protocol I: LEHR vs ME
Visually there was a clear difference in image quality between LEHR and ME collimators, as illustrated in Fig. 1c and d. The planar data were first analysed without scatter correction. Planar H/M ratios were higher for ME than for LEHR collimators for both cameras (Table 3). The ratios for the lateral segment of the myocardium were higher than those for the whole heart. Each collimator–camera combination showed comparable A and B ratios, but for C these ratios decreased by approximately 10% for ME and 20% for LEHR collimators, irrespective of camera. The latter can be explained by a more pronounced increase in count density for LEHR mediastinal ROI than for whole heart and myocardial ROIs (Fig. 2). The count densities increased less for the ME ROIs.
LEHR vs ME: influence of septal penetration on planar count density distribution. Data are normalised to condition A, and expressed as percentages. Count densities were corrected for decay. See Fig. 1 for definition of ROIs. Condition A: heart and mediastinum filled with 123I; B: condition A + lung activity; C: B + liver activity. LEHR Low energy high resolution, ME medium energy, GE Millennium VG, General Electric, SI e.cam, Siemens
As seen in Fig. 3, the SPECT-derived regional heart count densities remained similar whereas the mediastinal count densities increased considerably for condition C, and more so for the LEHR collimators. The measured total myocardial count densities increased from filling condition A to C (data not shown). Figure 4 shows that the count density within the myocardium was inhomogeneous. There was an overestimation of the measured count density in both the anterior and the septal wall and an underestimation of count density in the inferior wall. The underestimation (20%) in the inferior wall decreased (10%) after adding liver activity (Fig. 4c).
LEHR vs ME: influence of septal penetration on SPECT count density distribution. Data were normalised to condition A and expressed as percentages. Count densities were corrected for decay. See Fig. 1 for definition of the myocardial ROI. Condition A: heart and mediastinum filled with 123I; B: condition A + lung activity; C: B + liver activity. LEHR Low energy high resolution, ME medium energy, GE Millennium VG, General Electric, SI e.cam, Siemens
LEHR vs ME: measured planar count densities compared with expected average count densities for different filling conditions. The total measured myocardial counts were divided by the volume of the myocardial ROIs (anterior wall, septal wall and inferior wall) to give expected average count densities. The actual measured count densities were expressed as the percentage differences from expected count densities. a, b and c represent filling conditions A, B and C respectively. Condition A: heart and mediastinum filled with 123I; B: condition A + lung activity; C: B + liver activity. LEHR Low energy high resolution, ME medium energy, GE Millennium VG, General Electric, SI e.cam, Siemens
Different phantom filling conditions
As the ME collimator-generated data were less influenced by penetration of the collimator septa, the series of experiments to investigate H/M ratios in different phantom filling conditions were performed using the ME collimators only.
Condition F showed the same order of count statistics compared with condition C, resulting in similar H/M ratios (ME–SI 2.45 vs 2.45 and ME–GE 2.44 vs 2.39 for conditions C and F, respectively).
There was an unmistakable influence on the planar H/M ratios from increasing liver activity. Increasing the liver activity with unchanged low myocardial activity led to a decrease in H/M ratios (Fig. 5a) explained by progressively increasing mediastinal count densities (data not shown). Increasing myocardial activity with unchanged high liver activity caused H/M ratios initially to increase less than one would expect on the basis of increased myocardial activity (Fig. 5b). This is related to a non-proportional increase in myocardial count density with respect to the increase in myocardial activity (Fig. 5c).
Effect of TEW scatter correction on planar H/M
In general TEW scatter correction increased planar-derived H/M ratios for the different ME-collimated clinical conditions (Table 4). Only in condition C (H2/L40) was TEW scatter correction applied to both LEHR- and ME-collimated data. For LEHR-acquired data, the TEW scatter correction showed an increased H/M ratio (for the whole myocardium from 1.66 without TEW to 2.34 with TEW), which was similar to the ME H/M ratio without TEW scatter correction (2.45). TEW further increased the ME H/M ratios for condition C (for whole myocardium from 2.45 without TEW to 3.40 with TEW). Figure 6 shows that the improvement in H/M ratios can be explained by a more pronounced reduction in mediastinal count density compared with myocardial count density.
Influence of TEW scatter correction on count densities for the different filling conditions of the AGATE cardiac phantom. a Influence of TEW scatter correction on whole heart count densities. b Influence of TEW scatter correction on regional myocardial count densities. c Influence of TEW scatter correction on mediastinal count densities. Data are expressed as percentage difference compared to count densities without TEW scatter correction. See Table 2 for the different filling conditions (D, E, G, H, I) of the cardiac phantom and Fig. 1 for the definition of ROIs
Discussion
LEHR vs ME
The present study shows a clear influence of collimator choice on 123I-MIBG H/M ratios irrespective of camera type, collimator specifications and acquisition technique. 123I-MIBG image quality and H/M ratios from ME collimators were superior to those from LEHR collimators. Planar H/M ratios were mainly influenced by variations in mediastinal count densities, which were less pronounced for the ME collimators. The variation in the SPECT regional heart count densities suggests that, for conditions A and B, the underestimation of the count density in the inferior wall is probably related to attenuation. Scatter from liver activity, as simulated in condition C, however, reduced this underestimation (Fig. 4).
This effect is related to a reduction of septal penetration of high-energy photons of 123I. These results are in line with previously published studies [13, 14]. The influence of 123I high-energy photons on septal penetration in LEHR collimation is distance dependent [13]. The high-energy photons from 123I pass through the LEHR collimator septa and reach the detector crystal as if there was no collimator present, so that the number of high-energy photons reaching the crystal is approximately inversely related to the square of the distance. Changing the source distance, however, has only a minimal effect on the collimated 159-keV photons reaching the crystal. Therefore, in order to minimise the effects of septal penetration, the ME collimator is preferred. However, the use of ME collimation provides relatively low spatial resolution which may hamper accurate estimation of activity in small regions through a partial volume effect. In brain SPECT imaging with 123I-labelled agents, collimation with LEHR is preferred, because high spatial resolution is required, the head and brain tissue lead to a more or less homogeneous scatter, and the regions are mostly equidistant from the gamma camera. In cardiac scintigraphy with 123I-labelled agents, however, H/M ratios are assessed from counts in relatively large regions, the thorax and abdomen lead to an inhomogeneous scatter, and the myocardium is not equidistant from the gamma camera, especially for SPECT imaging. In cardiac scintigraphy with 123I-labelled agents the trade-off between spatial resolution and septal penetration is therefore in favour of low septal penetration. Moreover, as demonstrated by Inoue et al. in a checker phantom, the use of ME collimation in cardiac scintigraphy with 123I showed contrast accuracy similar to 99mTc [14]. We would therefore advocate the use of ME collimation in cardiac scintigraphy with 123I.
In the present phantom study, the two different camera systems with ME collimators produced similar semi-quantitative planar H/M ratios, despite different camera specifications, collimator design and different count efficiencies (Table 1). There is variability in the reported 123I-MIBG H/M ratios among institutions and between cameras used [17]. Standardisation of acquisition and processing is a prerequisite for extrapolation and implementation of published data. Apparently, ME collimation in planar scintigraphy plays a pivotal role in reducing variability in the results. In order to make it feasible to interchange 123I-MIBG H/M ratios from different gamma cameras, the use of ME collimation in combination with planar acquisition is essential.
Different phantom filling conditions
In the present phantom study the data showed that 123I-MIBG H/M ratios were influenced by scatter and septum penetration from increasing amounts of liver activity. Increasing liver activity with unchanged low myocardial activity led to decreasing H/M ratios explained by progressively increasing mediastinal count densities. This low myocardial activity with varying amounts of liver activity especially mimics the frequently observed clinical condition in patients with overt heart failure. In general, variations in liver activity and subsequent influence on scatter in the mediastinum are not taken into account in the interpretation of 123I-MIBG H/M ratios.
TEW scatter correction
Various methods of scatter correction have been described to improve image quality and quantitative accuracy [18]. The TEW scatter correction method estimates the scatter component in the prime photopeak from counts in a window just below and above the prime photopeak window [15]. The scatter correction is made on a pixel by pixel basis; therefore a requirement for the scatter correction images is good flood field uniformity in the scatter energy windows. In this phantom study, TEW scatter correction increased planar LEHR-assessed H/M ratios to levels similar to ME-determined H/M ratios, although this was assessed in only one clinical condition (C). One objective of scatter correction is to improve the accuracy of H/M ratios for different clinical conditions. Although TEW scatter correction increased all planar ME-collimated H/M ratios, TEW scatter correction did not improve the contrast between the ME-collimated H/M ratios for the different heart activities.
In a clinical setting of heart failure, myocardial count densities are generally low. TEW scatter correction, however, reduces the already low count density, which increases the uncertainty in ratio determination. Moreover, the TEW scatter correction-induced reduction in count density hampers the identification of endo- and epicardium and will therefore influence the definition of the myocardial ROIs. This decreases reproducibility of ratios. In addition, TEW scatter correction introduces noise, again increasing the uncertainty of generated ratios.
In cardiac SPECT with 123I-labelled agents, TEW has been reported to improve semi-quantitative accuracy [19, 20]. Although TEW resulted in an overall improvement in semi-quantitative accuracy, different degrees of over- and underestimation were reported. The lack of correction for depth response, complicated geometry and differences in tissue densities of the chest makes it difficult to obtain accurate scatter correction. These difficulties can result in over- or underestimation of count densities, especially for SPECT. We therefore decided not to perform TEW scatter correction in the cardiac phantom SPECT data.
In addition to theoretical limitations, the TEW method has limited availability in various gamma camera systems because TEW requires special hardware and software. Rather than try to filter unwanted counts by a post-acquisition scatter correction method, it is preferable to acquire data directly with less scatter. ME collimation without scatter correction is straightforward to implement and is therefore preferred in cardiac 123I scintigraphy.
Conclusion
Collimation had a definite effect on H/M ratios in favour of ME collimators irrespective of camera, collimator specification and acquisition technique. Planar H/M ratios from ME-collimated acquisitions were influenced by scatter from increasing amounts of liver activity. TEW scatter correction did not improve the differentiation of myocardial activity concentrations in the phantom. Therefore, for a simple and generally applicable method, the overall advice for semi-quantitative cardiac 123I-MIBG is to use ME collimators and no scatter correction.
References
Merlet P, Valette H, Dubois-Rande JL, Moyse D, Duboc D, Dove P, et al. Prognostic value of cardiac metaiodobenzylguanidine imaging in patients with heart failure. J Nucl Med 1992;33:471–7.
Ogita H, Shimonagata T, Fukunami M, Kumagai K, Yamada T, Asano Y, et al. Prognostic significance of cardiac 123I metaiodobenzylguanidine imaging for mortality and morbidity in patients with chronic heart failure: a prospective study. Heart 2001;86:656–60.
Patel AD, Iskandrian AE. MIBG imaging. J Nucl Cardiol 2002;9:75–94.
Somsen GA, van Vlies B, de Milliano PA, Borm JJ, van Royen EA, Endert E, et al. Increased myocardial [123I]-metaiodobenzylguanidine uptake after enalapril treatment in patients with chronic heart failure. Heart 1996;76:218–22.
Takeishi Y, Atsumi H, Fujiwara S, Takahashi K, Tomoike H. ACE inhibition reduces cardiac iodine-123-MIBG release in heart failure. J Nucl Med 1997;38:1085–9.
de Milliano PA, de Groot AC, Tijssen JG, Eck-Smit BL, Van Zwieten PA, Lie KI. Beneficial effects of metoprolol on myocardial sympathetic function: evidence from a randomized, placebo-controlled study in patients with congestive heart failure. Am Heart J 2002;144:E3.
Eichhorn EJ, McGhie AL, Bedotto JB, Corbett JR, Malloy CR, Hatfield BA, et al. Effects of bucindolol on neurohormonal activation in congestive heart failure. Am J Cardiol 1991;67:67–73.
Gerson MC, Craft LL, McGuire N, Suresh DP, Abraham WT, Wagoner LE. Carvedilol improves left ventricular function in heart failure patients with idiopathic dilated cardiomyopathy and a wide range of sympathetic nervous system function as measured by iodine 123 metaiodobenzylguanidine. J Nucl Cardiol 2002;9:608–15.
Yamazaki J, Muto H, Kabano T, Yamashina S, Nanjo S, Inoue A. Evaluation of beta-blocker therapy in patients with dilated cardiomyopathy—clinical meaning of iodine 123-metaiodobenzylguanidine myocardial single-photon emission computed tomography. Am Heart J 2001;141:645–52.
Kasama S, Toyama T, Kumakura H, Takayama Y, Ichikawa S, Suzuki T, et al. Spironolactone improves cardiac sympathetic nerve activity and symptoms in patients with congestive heart failure. J Nucl Med 2002;43:1279–85.
Kasama S, Toyama T, Kumakura H, Takayama Y, Ichikawa S, Suzuki T, et al. Effect of spironolactone on cardiac sympathetic nerve activity and left ventricular remodeling in patients with dilated cardiomyopathy. J Am Coll Cardiol 2003;41:574–81.
Somsen GA, Verberne HJ, Fleury E, Righetti A. Normal values and within-subject variability of cardiac I-123 MIBG scintigraphy in healthy individuals: implications for clinical studies. J Nucl Cardiol 2004;11:126–33.
Dobbeleir AA, Hambye AS, Franken PR. Influence of high-energy photons on the spectrum of iodine-123 with low- and medium-energy collimators: consequences for imaging with 123I-labelled compounds in clinical practice. Eur J Nucl Med 1999;26:655–8.
Inoue Y, Suzuki A, Shirouzu I, Machida T, Yoshizawa Y, Akita F, et al. Effect of collimator choice on quantitative assessment of cardiac iodine 123 MIBG uptake. J Nucl Cardiol 2003;10:623–32.
Ichihara T, Ogawa K, Motomura N, Kubo A, Hashimoto S. Compton scatter compensation using the triple-energy window method for single- and dual-isotope SPECT. J Nucl Med 1993;34:2216–21.
Visser JJ, Sokole EB, Verberne HJ, Habraken JB, van de Stadt HJ, Jaspers JE, et al. A realistic 3-D gated cardiac phantom for quality control of gated myocardial perfusion SPET: the Amsterdam gated (AGATE) cardiac phantom. Eur J Nucl Med Mol Imaging 2004;31:222–8.
Yamashina S, Yamazaki J. Role of MIBG myocardial scintigraphy in the assessment of heart failure: the need to establish evidence. Eur J Nucl Med Mol Imaging 2004;31:1353–5.
Buvat I, Benali H, Todd-Pokropek A, Di Paola R. Scatter correction in scintigraphy: the state of the art. Eur J Nucl Med 1994;21:675–94.
Takeda K, Saito K, Makino K, Saito Y, Aoki S, Koji T, et al. Iodine-123-BMIPP myocardial washout and cardiac work during exercise in normal and ischemic hearts. J Nucl Med 1997;38:559–63.
Saito K, Takeda K, Okamoto S, Okamoto R, Makino K, Tameda Y, et al. Detection of doxorubicin cardiotoxicity by using iodine-123 BMIPP early dynamic SPECT: quantitative evaluation of early abnormality of fatty acid metabolism with the Rutland method. J Nucl Cardiol 2000;7:553–61.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Verberne, H.J., Feenstra, C., de Jong, W.M. et al. Influence of collimator choice and simulated clinical conditions on 123I-MIBG heart/mediastinum ratios: a phantom study. Eur J Nucl Med Mol Imaging 32, 1100–1107 (2005). https://doi.org/10.1007/s00259-005-1810-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00259-005-1810-3