Abstract
Purpose
The purpose of this study was to assess whether pre-operative 99mTc-methoxyisobutylisonitrile (MIBI) scintigraphy and neck ultrasound (US) are of value in improving the outcome of subtotal parathyroidectomy in patients with secondary hyperparathyroidism.
Methods
Forty-eight consecutive haemodialysis patients with severe secondary hyperparathyroidism prospectively underwent “blinded” subtotal parathyroid surgery, with 1-year follow-up to establish cure or relapse of their secondary hyperparathyroidism. Double-phase 99mTc-MIBI scintigraphy and neck US were performed pre-operatively in all patients. When the preserved gland showed 99mTc-MIBI uptake or an abnormal size on US, it was considered that “99mTc-MIBI advice” and “US advice”, respectively, had not been followed. Pre-operative and follow-up parathyroid hormone (PTH) levels were obtained in all patients. All data were evaluated on a patient by patient basis.
Results
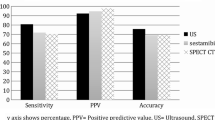
Four parathyroid glands were identified in each patient at primary surgery, resulting in an operative success rate of 100%. Their weight ranged from 15 to 7,300 mg (mean 1,120±900 mg). Nine of the 48 patients (19%) showed a recurrence of their secondary hyperparathyroidism. The recurrence rate was 2% (1/48) and 10% (5/48), respectively, when 99mTc-MIBI and US advice was followed. The sensitivity, specificity, NPV and PPV for pre-operative imaging were 72%, 95%, 97% and 80% respectively for 99mTc-MIBI, and 55%, 67%, 87% and 28% for US.
Conclusion
99mTc-MIBI scintigraphy is a reliable non-invasive exploratory tool and its preoperative use results in a significant reduction in the number of recurrences in haemodialysis patients with secondary hyperparathyroidism who are candidates for subtotal parathyroidectomy. The use of neck US did not significantly improve the results obtained with 99mTc-MIBI alone.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Secondary hyperparathyroidism (SHP) is a frequent complication in patients with chronic renal failure. Despite treatment with active vitamin D metabolites and phosphate binders, it is sometimes difficult to control SHP and, unfortunately, the more dialysis is used, the more likely it is that a patient will not respond to medical treatment and will require a parathyroidectomy [1].
High-resolution sonography (US) is a significant imaging tool in the evaluation of the parathyroid glands. US is a technique that depends on operator skill, which explains the wide variability in the reported sensitivity (ranging from 30–80%) for the detection of abnormal parathyroid glands [2–8]. The potential of 99mTc-methoxyisobutylisonitrile (MIBI) to identify the presence of hyperfunctioning autonomous parathyroid glands is well known. Comparison of morphological and functional data strongly suggests that 99mTc-MIBI not only reveals parathyroid enlargement but can also identify the presence of hyperfunctioning parathyroid tissue [9, 10]. Imaging of the parathyroid glands using 99mTc-MIBI and neck US has been widely used in the identification of solitary parathyroid adenomas, which is the most common finding in patients with primary hyperparathyroidism [8, 11].
Some groups have indicated that 99mTc-MIBI imaging should also be used initially to localise abnormal glands in haemodialysis patients with SHP, prior to US, magnetic resonance imaging and computed tomography [12, 13]. However, use of imaging procedures in SHP patients, in whom multiglandular hyperplastic disease is the most common finding, is controversial. Some authors are against pre-operative parathyroid scintigraphy on the grounds that its low sensitivity means that it is of no additional value [14]. In fact, they think that SHP patients who have not had previous neck surgery do not require pre-operative localisation because of the high success rate of cervical exploration and the limited sensitivity and specificity of all imaging modalities currently in use [15–17]. However, it should be recognised that the rate of persistent or recurrent disease in this setting is as high as 10–30%, the main cause being incomplete localisation of glands; this suggests that more caution is warranted when ruling out a role for pre-operative imaging [18, 19]. This is especially evident in re-operated patients and in those with unsuspected ectopic glands, in whom 99mTc-MIBI is of significant value.
The aim of this study was to assess whether pre-operative 99mTc-methoxyisobutylisonitrile (MIBI) scintigraphy and neck ultrasound (US) are of value in improving the outcome of subtotal parathyroidectomy in patients with secondary hyperparathyroidism.
Materials and methods
Patients
Forty-eight (n=48) consecutive haemodialysis patients (24 males, 24 females) with a mean age of 49.8±14.2 years (range 24–74 years) and severe SHP [defined as symptoms of renal osteodystrophy in addition to a parathyroid hormone (PTH) value of ≥600 pg/ml] were prospectively included for parathyroid surgery. They were selected on the basis of two separate PTH determinations above 600 pg/ml at a minimum interval of 30 days. Additional inclusion criteria were serum calcium above 10.5 mg/dl (2.625 mmol/l) and serum phosphorus above 5.5 mg/dl (1.77 mmol/l), pruritus not responding to medical therapy, calciphylaxis and/or unexplained symptomatic myopathy. Follow-up was for at least 1 year after surgery. Pre- and postoperative as well as follow-up PTH levels were obtained in all patients. All data were evaluated on a patient by patient basis. Relapse was defined as reappearance of PTH-dependent hypercalcaemia.
The study project was approved by the local hospital ethical committee and informed consent was obtained from each patient.
Double-phase MIBI scintigraphy
All patients underwent 99mTc-MIBI scintigraphy pre-operatively less than 1 month prior to surgery. Patients were injected intravenously with 740 MBq of 99mTc-MIBI. The labelling efficiency had previously been assessed by thin-layer chromatography. Radiochemical purity was always >95%. Anterior views of the neck and the upper thorax at a fixed interval of 300 s/frame and a matrix size of 256×256 were obtained with the patient in the supine position. Images were obtained at 15 min (initial or thyroid phase) and 2 h (delayed or parathyroid phase) after radiotracer administration. A digital gamma camera (GE Medical Systems, SP4-HR) with a low-energy, high-resolution, parallel-hole collimator was used. All patients with positive findings on 99mTc-MIBI scintigraphy underwent a thyroid scan to rule out the presence of thyroid nodules.
Focal areas of increased uptake showing either a relative progressive increase in uptake over time or a fixed uptake which persisted on delayed imaging were considered to be pathological (Fig. 1). To evaluate the possible effect of 99mTc-MIBI wash-out, additional focal sites of uptake visualised only in the early phase were also interpreted as pathological parathyroid glands.
a In the initial (left) and the delayed (right) phase of the study, 99mTc-MIBI shows fixed uptake in the lower pole of the right thyroid lobe and in both poles of the left thyroid lobe, attributable to pathological parathyroid glands. b US of the neck shows two nodular hypoechoic lesions, suggesting parathyroid adenoma/hyperplasia. They are situated below the lower pole (left) and in upper pole (right) of the left thyroid lobe, and measure 3.9×3.3 mm and 3.4×3.3 mm, respectively
Neck ultrasound
Parathyroid US was performed in all patients. The ultrasonographic study of the neck was performed with a Toshiba Powervision or Toshiba Applio colour Doppler (Toshiba, Nasu, Japan) using a multifrequency linear transducer (7–11 MHz). The US was carried out with the patient in the supine position and with the neck in hyperextension (when necessary a cushion was placed under the patient’s shoulders). In the US grey-scale study, longitudinal and axial US sections were obtained from the angle of the mandible to the sternal notch, and laterally to include the carotid and jugular vessels. The patient was also explored with the head turned to the contralateral side in order to better visualise the deep cervical planes. Normal parathyroid glands are not visualised with the currently available equipment. When pathological glands were observed, the echostructure (homogeneous vs heterogeneous echogenicity, calcification) and size (longitudinal, antero-posterior and transverse diameters) were evaluated. The colour Doppler vascularisation pattern (polar distribution of the colour with no perinodular colour distribution, diffuse intraparenchymal distribution, perinodular pattern) was reported when detected in the colour Doppler study.
Surgery
Results of parathyroid scintigraphy and neck US regarding pre-operative gland localisation (termed 99mTc-MIBI or US advice) were not provided to the surgeon prior to the operation. Exploration for abnormal parathyroid glands was performed with the patient under general anaesthesia, using a transverse collar incision. The operative technique included subtotal parathyroidectomy performed by an experienced surgeon for all patients. The retro-thyroid approach was used in all patients. Three and a half glands were totally removed, leaving half of the gland with the most normal appearance or in the anatomical position that would least complicate re-intervention in the event of recurrence. The remnant gland left in place was marked with a non-reabsorbable thread to facilitate any re-operative detection. When the gland preserved by the surgeon showed 99mTc-MIBI uptake, it was considered that “99mTc-MIBI advice” had not been followed. When the preserved gland showed an abnormal size on US, it was considered that “US advice” had not been followed.
Histopathological findings
Three histopathological parameters were analysed for this study: the confirmation of parathyroid tissue on frozen sections, hyperplasia on definitive histopathology, and information regarding the weight of the removed parathyroid glands. Only those parathyroid glands that were removed intact were analysed, by weight, for a comparative study with pre-operative 99mTc-MIBI results.
Statistical analysis
The Mann-Whitney U test was used to compare distributions between the two groups. Correlation between parameters was calculated using Pearson’s correlation coefficient. Sensitivity, specificity, positive predictive value (PPV) and negative predictive value (NPV) were evaluated by standard methods. A p value of <0.05 was considered statistically significant.
Results
Four parathyroid glands were identified in each patient at primary surgery, resulting in an operative success rate of 100%. The definitive histopathological findings identified hyperplasia of all the removed parathyroid glands. Their weight ranged from 15 to 7,300 mg (mean 1,120±900 mg). Parathyroid US revealed at least one enlarged gland in 45/48 patients, the maximum gland diameter being 10.2 mm. 99mTc-MIBI showed uptake in at least one gland in 43/48 patients. Nine of the 48 patients included in the study (19%) showed a biochemical relapse during the follow-up, and they were considered to have had a recurrence of their SHP.
The recurrence rate with “blinded surgery” was 19% (9/48), compared with 10% (5/48) when US advice was followed. A recurrence rate of only 2% (1/48) was observed when 99mTc-MIBI advice was considered (p<0.0005). Comparing the recurrence group with patients without evidence of recurrence in the follow-up, PTH values were similar pre-operatively (915±232 pg/ml in patients with recurrence vs 969±77 pg/ml in those without recurrence). One month later, PTH values remained indistinguishable (209±63 pg/ml in the recurrence group vs 169±23 pg/ml in the non-recurrence group). However, 1 year after surgery, PTH values proved to be significantly higher in the group with recurrence ((884±217 pg/ml, vs 119±17 pg/ml in the non-recurrence group; p<0.0005) . A similar situation was observed if pre-operative 99mTc-MIBI advice was taken into account: PTH values were similar in the two groups pre-operatively and 1 month later. However, 1 year after surgery, PTH values were significantly higher (p<0.0005) in those patients in whom 99mTc-MIBI advice was not followed (Fig. 2a). By contrast, no significant differences were found between patients in whom US advice was followed and those in whom it was not (Fig. 2b). The results in respect of biochemical recurrence according to whether 99mTc-MIBI or US advice was or was not followed are summarised in Table 1.
The overall sensitivity, specificity, NPV and PPV for pre-operative imaging advice were 72%, 95%, 97% and 80%, respectively, for 99mTc-MIBI, and 55%, 67%, 87% and 28% for US. 99mTc-MIBI showed a significantly higher specificity, PPV and NPV than US (p>0.0005), but there was no significant difference in sensitivity. Differences in the echostructure and/or in the colour Doppler vascularisation pattern did not yield significant additional value to the overall US results. In four cases, the initial phase of 99mTc-MIBI scanning was determinant in the detection of pathological parathyroid glands which washed out on the delayed images. Interestingly, in eight of the nine confirmed recurrences, 99mTc-MIBI advice was not followed. In two of these cases an ectopic hyperplastic gland only suspected by 99mTc-MIBI was found at re-operation (Fig. 3). There was only in one case in which 99mTc-MIBI advice was followed (i.e. a normally functioning parathyroid gland on 99mTc-MIBI was left at surgery) and recurrence was detected. We found two false positive cases in which 99mTc-MIBI advice was not followed but there was no relapse of the SHP during follow-up; one of these cases was a papillary thyroid cancer, and the second, an infiltrated lymph node (also from a differentiated thyroid cancer).
a99mTc-MIBI scintigraphy shows fixed uptake below the thyroid gland in the initial (left) and the delayed (right) phase of the study, suggesting an ectopic parathyroid gland in the upper mediastinum. b Neck US was unremarkable. At surgery, three parathyroid glands were identified in the cervical region and removed, and these showed hyperplastic tissue. The patient had to undergo re-operation to remove the ectopic tissue and has since remained asymptomatic
Discussion
Bilateral surgical exploration with identification of all glands is required in SHP patients, since multiglandular disease with hyperplasia of parathyroid glands occurs in most cases. For this reason, some authors consider pre-operative examinations to be superfluous, time consuming or an avoidable expense [20]. Additionally, the sensitivity of imaging procedures has been reported to be lower than in primary hyperparathyroidism, where the pre-operative use of combined neck US and parathyroid scintigraphy has recently been proposed for minimally invasive explorations [21]. On the other hand, the relatively small size of some hyperplastic or adenomatous glands and the common occurrence of unexpected ectopic and/or supernumerary glands [11, 22–24] have led to a high rate of re-operation due to missed glands located in the neck [13, 25]. This raises the question of the need to perform pre-operative imaging in order to increase the success rate of surgery in SHP, especially in patients with end-stage renal failure exhibiting hyperplastic parathyroid glands, in whom major anaesthesia risks are frequent.
It remains unproven that having the pre-operative imaging information available to the surgeon actually results in a lower postoperative relapse rate. This would probably require a further study with a larger number of patients. Despite this, our results show a significantly lower relapse rate when using 99mTc-MIBI (2%) compared with “blinded surgery” alone (19%). Its use might allow us at least to confirm or discount the presence of ectopic or supernumerary glands, which is crucial to the planning of the surgical procedure, and to facilitate the accurate localisation of the glands, particularly during re-operations. Our results support this line of thought. In fact, we found that PTH values had fallen similarly 1 month after surgery (by 20% when MIBI advice was followed vs 22% when MIBI advice was not followed). Therefore, at 1 month following surgery it is probably too early to detect SHP recurrence and PTH values do not carry any significant prognostic value at that time. Nevertheless, 1 year later PTH levels were significantly lower in the group in which 99mTc-MIBI advice was followed (reduction of 84% vs 35%; p<0.0005). At this point in time, pre-operative 99mTc-MIBI results clearly provide significant advantages regarding SHP recurrence.
Some groups have performed parathyroid scintigraphy using 99mTc-tetrofosmin [26]; however, this radiotracer is only appropriate when using the subtraction technique owing to lower wash-out at the level of the thyroid gland, and it would not be suitable for the double-phase technique. 99mTc-MIBI is now considered the radionuclide of reference for parathyroid gland scanning [27–29]. This radiotracer has shown itself to be highly accurate in reflecting PTH levels without external influences [30], and has proved to be a useful tool in clinical management, allowing the physician to discriminate between patients who will and those who will not respond to calcitriol treatment [31].
There are a number of variations in the methodology for 99mTc-MIBI scintigraphy. Some groups suggest that higher sensitivities are achieved using oblique views, pin-hole and SPECT [15, 17, 32]. However, the usefulness of these techniques in routine practice is still debatable because of the considerable extra time demands on the gamma camera. In both primary and secondary hyperparathyroidism, the sensitivity of pre-operative parathyroid scintigraphy using planar images has proven similar to that obtained using the above-mentioned methods, so their advantages have yet to be proven [19]. A recent trend in parathyroid scintigraphy is the use of subtraction 123I/99mTc-MIBI, which may also increase the sensitivity of double-phase 99mTc-MIBI; however, our results show a sensitivity practically identical to that disclosed in a previous publication using 123I/99mTc-sestamibi SPECT [32], while our NPV is much higher. 99mTc-MIBI’s higher specificity (p<0.0005) compared with surgery has not been previously reported and explains why the relapse rate is significantly higher in patients operated on without prior 99mTc-MIBI scintigraphy.
As has been described in other published series, the over-expression of the multidrug-resistant protein or P-glycoprotein may be the main cause of false negative 99mTc-MIBI scans in the delayed phase (in our series, four cases with histologically confirmed hyperplasia were not detected in the delayed phase) [33]. Taking this into account, positive findings in the early scan should be considered to represent pathological parathyroid glands in order to improve the overall sensitivity of double-phase 99mTc-MIBI [34]. False positive results have been described, the most common causes being multinodular goitres or thyroid nodules, which can usually be well defined by performing a thyroid scan. Another cause of cervical 99mTc-MIBI uptake can be the tumoural avidity of the radiotracer [35]. The two false positive results in the present study were due to thyroid cancer in one patient and an infiltrated lymph node from lymphoma in the second case. In accordance with other published series [2–8], neck US showed poor results in SHP patients; this was especially because of its low sensitivity, which has been found to be as low as 30% in some series. This low sensitivity is probably attributable to limitations related to anatomical areas inaccessible to insonation and the technique’s dependence on operator skill [2–8].
In conclusion, 99mTc-MIBI scintigraphy is a reliable non-invasive exploratory tool and its preoperative use results in a significant reduction in the number of recurrences in haemodialysis patients with secondary hyperparathyroidism who are candidates for subtotal parathyroidectomy. The use of neck US did not significantly improve the results obtained with 99mTc-MIBI alone.
References
Andress DL. Intravenous versus oral vitamin D therapy in dialysis patients: what is the question? Am J Kidney Dis 2001;38:S41–4
Ishibashi M, Nishida H, Hiromatsu Y, Kojima K, Tabuchi E, Hayabuchi N. Comparison of technetium-99m-MIBI, technetium-99m-tetrofosmin, ultrasound and MRI for localization of abnormal parathyroid glands. J Nucl Med 1998;39:320–4
Rubello D, Mazzarotto R, Casara D. The role of technetium-99m methoxyisobutylisonitrile scintigraphy in the planning of therapy and follow-up of patients with differentiated thyroid carcinoma after surgery. Eur J Nucl Med 2000;27:331–40
Rubello D, Saladini G, Casara D, Borsato N, Toniato A, Piotto A, et al. Parathyroid imaging with pertechnetate plus perchlorate/MIBI subfraction scintigraphy–a fast and effective technique. Clin Nucl Med 2000;25:527–31
Casara D, Rubello D, Piotto A, Pelizzo MR. 99mTc-MIBI radio-guided minimally invasive parathyroid surgery planned on the basis of a preoperative combined 99mTc-pertechnetate/99mTc-MIBI and ultrasound imaging protocol. Eur J Nucl Med 2000;27:1300–4
Casara D, Rubello D, Cauzzo C, Pelizzo MR. Tc-99m-MIBI radio-guided minimally invasive parathyroidectomy: Experience with patients with normal thyroids and nodular goiters. Thyroid 2002;12:53–61
Geatti O, Shapiro B, Orsolon PG, Proto G, Guerra UP, Antonucci F, et al. Localization of parathyroid enlargement—experience with Tc-99m methoxyisobutylisonitrile and Tl-201 scintigraphy, ultrasonography and computed-tomography. Eur J Nucl Med 1994;21:17–22
Gofrit ON, Lebensart PD, Pikarsky A, Lackstein D, Gross DJ, Shiloni E. High-resolution ultrasonography: highly sensitive, specific technique for preoperative localization of parathyroid adenoma in the absence of multinodular thyroid disease. World J Surg 1997;21:287–91
Torregrosa JV, Fernandez-Cruz L, Canalejo A, Vidal S, Astudillo E, Almaden Y, et al. 99mTc-sestamibi scintigraphy and cell cycle in parathyroid glands of secondary hyperparathyroidism. World J Surg 2000;24:1386–90
Piga M, Bolasco P, Satta L, Altieri P, Loi G, Nicolosi A, et al. Double-phase parathyroid technetium-99m-MIBI scintigraphy to identify functional autonomy in secondary hyperparathyroidism. J Nucl Med 1996;37:565–9
Proye CA, Carnaille B, Bizard JP, Quievreux JL, Lecomte-Houcke M. Multiglandular disease in seemingly sporadic primary hyperparathyroidism revisited—where are we in the early 1990s—a plea against unilateral parathyroid exploration. Surgery 1992;112:1118–22
Pons F, Torregrosa JV, Vidal-Sicart S, Sabater L, Fuster D, Fernandez-Cruz L, et al. Preoperative parathyroid gland localization with technetium-99m sestamibi in secondary hyperparathyroidism. Eur J Nucl Med 1997;24:1494–8
Ishibashi M, Nishida H, Okuda S, Suekane S, Hayabuchi N. Localization of parathyroid glands in hemodialysis patients using Tc-99m sestamibi imaging. Nephron 1998;78:48–53
Olaizola I, Zingraff J, Heuguerot C, Fajardo L, Leger A, Lopez J, et al. [Tc-99m]-sestamibi parathyroid scintigraphy in chronic haemodialysis patients: static and dynamic explorations. Nephrol Dial Transpl 2000;15:1201–6
Spanu A, Falchi A, Manca A, Marongiu P, Cossu A, Pisu N, et al. The usefulness of neck pinhole SPECT as a complementary tool to planar scintigraphy in primary and secondary hyperparathyroidism. J Nucl Med 2004;45:40–8
Lorberboym M, Minski I, Macadziob S, Nikolov G, Schachter P. Incremental diagnostic value of preoperative Tc-99m-MIBI SPECT in patients with a parathyroid adenoma. J Nucl Med 2003;44:904–8
Price DC. Radioisotopic evaluation of the thyroid and the parathyroids. Radiol Clin North Am 1993;31:991–1015
Hindie E, Urena P, Jeanguillaume C, Melliere D, Berthelot JM, Menoyo-Calonge V, et al. Preoperative imaging of parathyroid glands with technetium-99m-labelled sestamibi and iodine-123 subtraction scanning in secondary hyperparathyroidism. Lancet 1999;353:2200–4
Giordano A, Rubello D, Casara D. New trends in parathyroid scintigraphy. Eur J Nucl Med 2001;28:1409–20
Sofferman RA, Nathan MH. The ectopic parathyroid adenoma: a cost justification for routine pre-operative localization with technetium-99m-sestamibi scan. Arch Otolaryngol Head Neck Surg 1998;124:649–54
Lumachi F, Ermani M, Basso S, Zucchetta P, Borsato N, Favia G. Localization of parathyroid tumours in the minimally invasive era: which technique should be chosen? Population-based analysis of 253 patients undergoing parathyroidectomy and factors affecting parathyroid gland detection. Endocr Relat Cancer 2001;8:63–9
Levin KE, Clark OH. The reasons for failure in parathyroid operations. Arch Surg 1989;124:911–5
Wang CA, Gaz RD, Moncure AC. Mediastinal parathyroid exploration—a clinical and pathological study of 47 cases. World J Surg 1986;10:687–95
Bruining HA, Birkenhager JC, Ong GL, Lamberts SWJ. Causes of failure in operations for hyperparathyroidism. Surgery 1987;101:562–5
Rothmun M, Wagner P. Reoperations for persistent and recurrent secondary hyperparathyroidism. Ann Surg 1988;207:310–4
Vallejos V, Martin-Comin J, Mora J, Gonzalez MT, Rafecas A, Munoz A, et al.Use of 99mTc-tetrofosmin scintigraphy in the diagnosis of patients with hyperparathyroidism. Rev Esp Med Nucl 1998;17:94–101
Ambrosoni P, Olaizola I, Heuguerot C, Parodi MN, Caorsi H, Caputti S, et al. The role of imaging techniques in the study of renal osteodystrophy. Am J Med Sci 2000;320:90–5
Olaizola I, Aznarez A, Jorgetti V, Petraglia A, Caorsi H, Acuna G, et al. Are there any differences in the parathyroid response in the different types of renal osteodystrophy? Nephrol Dial Transpl 1998;13 (Suppl 3):15–8
Torregrosa JV, Palomar MR, Pons F, Sabater L, Gilabert R, Llovera J, et al. Has double-phase MIBI scintigraphy usefulness in the diagnosis of hyperparathyroidism? Nephrol Dial Transpl 1998;13:37–40
Fuster D, Ybarra J, Torregrosa JV, Setoain X, Martin F, Ortega ML, et al. Double-phase parathyroid Tc-99m-sestamibi scintigraphy in chronic haemodialysis patients: correlation with biochemical markers of parathyroid function. Nucl Med Commun 2003;24:85–90
Torregrosa JV, Fuster D, Ybarra J, Moreno A, Valveny N. Predicting the effect of intravenous calcitriol on parathyroid gland activity using double-phase 99mTc-sestamibi scintigraphy. Am J Kidney Dis 2004;44:476–80
Neumann DR, Esselstyn CB Jr, Madera A, Wong CO, Lieber M. Parathyroid detection in secondary hyperparathyroidism with I-123/Tc-99m-sestamibi subtraction single photon emission computed tomography. J Clin Endocr Metab 1998;83:3867–71
Kao A, Shiau YC, Tsai SC, Wang JJ, Ho ST. Technetium-99m methoxyisobutylisonitrile imaging for parathyroid adenoma: relationship to P-glycoprotein or multidrug resistance-related protein expression. Eur J Nucl Med Mol Imagin 2002;29:1012–5
Krausz Y, Shiloni E, Bocher M, Agranovicz S, Manos B, Chisin R. Diagnostic dilemmas in parathyroid scintigraphy. Clin Nucl Med 2001;26:997–1001
Iwata M, Kasagi K, Misaki T, Matsumoto K, Iida Y, Ishimori T, et al. Comparison of whole-body 18F-FDG PET, 99mTc-MIBI SPET, and post-therapeutic 131I-Na scintigraphy in the detection of metastatic thyroid cancer. Eur J Nucl Med 2004;31:491–8
Acknowledgements
This research was supported in part by the grants RTICCC C03/10 and IM3 G03/185 from the Instituto de Salud Carlos III.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Fuster, D., Ybarra, J., Ortin, J. et al. Role of pre-operative imaging using 99mTc-MIBI and neck ultrasound in patients with secondary hyperparathyroidism who are candidates for subtotal parathyroidectomy. Eur J Nucl Med Mol Imaging 33, 467–473 (2006). https://doi.org/10.1007/s00259-005-0021-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00259-005-0021-2