Abstract
Purpose
The aim of this study was to evaluate the significance of increased uptake of 18F-fluorodeoxyglucose (FDG) in patients with malignant lymphoma (ML) studied by positron emission tomography (PET).
Methods
A total of 1,120 consecutive scans carried out in 848 patients were reviewed; all patients had a diagnosis of ML [574 non-Hodgkin’s lymphoma (NHL) and 274 Hodgkin’s disease (HD)] and were studied at completion of therapy, for suspected recurrence or during follow-up. PET was carried out after intravenous injection of 370 MBq of 18F-FDG; images were recorded after 60–90 min. Patients were selected whose reports indicated areas of increased FDG uptake. PET findings were considered positive for lymphomatous localisation when uptake occurred at sites of previous disease, in asymmetrical lymph nodes or in nodes unlikely to be affected by inflammation (mediastinal, except for hilar, and abdominal). PET findings were adjudged negative for neoplastic localisations in the following instances: physiological uptake (urinary, muscular, thymic or gastrointestinal in patients without MALT), symmetrical nodal uptake, uptake in lesions unrelated to lymphoma that had already been identified by other imaging methods at the time of PET scan, uptake at sites atypical for lymphoma, very low uptake and non-focal uptake. PET findings were compared with the results of other diagnostic procedures (including CT and ultrasound), biopsy findings and follow-up data.
Results
Overall, 354 scans (in 256 patients) showed increased FDG uptake (244 scans in NHL and 110 in HD): in 286 cases, FDG uptake was considered pathological and indicative of ML, in 41 cases the findings were described as uncertain or equivocal and in 37 cases, FDG uptake was considered unrelated to ML (in ten scans, concurrent findings of abnormal FDG uptake attributed to ML and uptake assigned to other causes were obtained) . Of the 286 patients with positive PET findings, 274 (95.8%) were found to have residual or recurrent ML (i.e. true positives). Four of the 41 patients with inconclusive findings turned out to have ML, while in 13 patients, pathological processes other than ML could be identified as the cause of FDG uptake. ML was excluded in all patients with findings reported as non-pathological (100% true-negative rate). Therefore, the false-positive rate in our series was about 5%. The main cause of increased FDG uptake mimicking ML was inflammation.
Conclusion
Our data confirm that 18F-FDG-PET has very high but not absolute specificity for ML. As already suggested, increased FDG uptake may also be observed in patients without active disease; in most cases, however, non-pathological FDG accumulation is properly identified. Less frequently, inconclusive scans are encountered; these cases are usually caused by inflammation, which subsequently resolves.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
18F-fluorodeoxyglucose positron emission tomography (FDG-PET) has yielded very successful results in the imaging of adult and paediatric lymphomas [1]. In recent years, FDG-PET has proved to be a valuable tool for clinicians owing to its ability to provide important information that has a direct impact on patient management [2]. Several indications for FDG-PET have been suggested in patients with malignant lymphoma (ML). Useful roles for FDG-PET have been established in staging, in the evaluation of early response to chemotherapy, in the assessment of end response to therapy, in radiation therapy planning and during follow-up [2].
The effectiveness of FDG-PET is due to its ability to identify active disease [3]. After completion of therapy, FDG-PET influences patient management by differentiating patients with residual lymphoma (non-responders or partial responders) from those without viable tumours (complete responders) [4, 5]. Similarly, in cases of relapse, early identification of disease recurrence may influence the success rate of therapy by allowing for earlier treatment.
It is well known that tumours demonstrate increased uptake of the glucose analogue 18F-FDG. The detection of active lymphoma by PET is based on the degree of FDG uptake. Usually areas of increased accumulation at sites other than those of known physiological uptake are regarded as disease. FDG-PET studies may therefore be easily interpreted in the presence of intense FDG uptake at sites frequently involved by ML, as well as in the absence of any abnormal uptake. In clinical practice, however, it is not uncommon for challenging situations to arise in the presence of faintly increased uptake at sites unlikely to be involved by ML. A well-recognised example is inflammation, which can also cause markedly increased FDG uptake. The fact that PET can demonstrate high radiotracer concentration unrelated to ML means that misinterpretation of images is possible [6]. Several papers have indicated the potential limitations of PET for the study of lymphoma, and particular attention has been drawn to the lack of specificity of FDG as a lymphoma tracer [6, 7]. Since FDG-PET is rapidly gaining widespread use for ML evaluation, it is important to clarify the incidence and causes of false-positive findings.
The aim of this study was to assess the significance of increased FDG uptake in patients affected by ML and to evaluate the false-positive rate of FDG-PET for this disease.
Materials and methods
Inclusion criteria
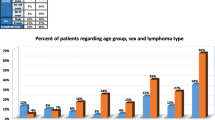
We retrospectively evaluated all FDG-PET scans carried out at our institution in patients with ML during the last 14 months. Overall, 1,312 scans were carried out; for the purpose of this study we excluded scans carried out at presentation of disease (staging). Therefore 1,120 scans obtained in 848 patients were reviewed; all patients had histologically proven ML (382 scans in 274 patients with Hodgkin’s disease and 738 scans in 574 patients with non-Hodgkin’s lymphoma).
In order to identify patients with increased uptake of 18F-FDG, we used selection criteria based on reported findings. We selected patients whose reports indicated any area of increased FDG uptake attributed to either ML or to causes independent from ML; we also included patients whose reports indicated findings that could not be attributed to a precise cause (equivocal studies).
FDG-PET imaging
Each patient was intravenously injected with 5.3 MBq/kg of 18F-FDG; images were obtained 60–90 min after tracer administration. 18F-FDG was produced in our radiopharmacy using standard synthesis techniques.
PET scans were carried out using a PET tomograph (Advance scanner, GE Medical System, Waukesha, WI). PET scan emission images were collected for 4 min for each bed position; for non-uniform attenuation correction, 2-min transmission images were used. To optimise FDG uptake in normal and neoplastic tissue, patients were asked to fast for at least 6 h before undergoing the PET examination; no patient had a history of diabetes. Before PET scanning, patients were encouraged to void in order to minimise activity in the bladder.
Image interpretation and reporting
PET images were evaluated on the basis of visual inspection by three experienced readers: in all cases agreement among readers was obtained for the final report. The scan was interpreted as negative when no pathological tracer uptake was shown by FDG-PET. Areas of focal uptake were interpreted as unequivocally positive for lymphoma when they were localised at sites of previous disease (residual disease or relapse), within asymmetrical lymph nodes or within lymph nodes unlikely to affected by inflammation (mediastinal, except for hilar, and abdominal). Sites of known physiological uptake, including the kidney, ureter, bladder and musculoskeletal areas, that showed symmetrical uptake were not described in the report and the scan was considered negative. Homogeneously increased uptake within the gastrointestinal tract in patients without MALT lymphoma was also considered non-pathological and therefore not reported. Other sites of increased uptake were described and attributed to a definite or possible cause. When FDG uptake was attributed to a non-pathological cause, the report was regarded as negative for ML and other diseases. When the uptake was considered likely to be unrelated to ML, the report was adjudged suspicious for other diseases. If increased FDG uptake could not be attributed to a precise cause, the scan was considered inconclusive.
Standardised uptake values (SUVs) were not routinely indicated on reports, but values were always available to readers through standard software that easily provided mean and maximum values for the region of interest. Thus, it was not uncommon for the SUV to be taken into account when interpreting a lesion, even though visual analysis remains the most important diagnostic criterion at our institution. For the purpose of the present study, all scans included for final evaluation were re-analysed to determine SUVs. Lesions with a SUVmax ≤2 were considered inconsistent with lymphomatous disease while areas with a SUVmax >2 were considered positive or negative for lymphomatous localisation according to the site, clinical data and other test results.
Final assessment of findings
To assess the significance of the reported findings, we collected all other available clinical data for each patient, including the results of other diagnostic imaging procedures and follow-up. The final diagnosis in all cases was established by clinicians aware of the clinical, laboratory and diagnostic imaging data. The results of other imaging procedures that were available at the time of the PET scan were used to correctly read PET images, in particular when PET results were questionable. For example, gastric FDG uptake was considered unrelated to lymphoma when endoscopy revealed gastritis.
Follow-up data were obtained for all included patients (minimum follow-up 8 months, median 10 months, range 8–14 months). Patients lacking these data were excluded from further evaluation.
Results
Overall, 1,120 scans obtained in 848 patients were reviewed; scans reported as completely negative were excluded from further evaluation, while scans reported to contain any area of increased FDG uptake were included. Four hundred and two reports met the inclusion criteria (35.9% of scans); 48 of these examinations were excluded from further consideration because of lack of follow-up data. Therefore, 354 scans (in 256 patients) were finally evaluated (Table 1).
As previously stated, assessment of final outcome was based on clinical data and on any subsequent examinations carried out following the PET scans. Further diagnostic procedures were required in 178/354 cases and included CT in 130 cases, biopsy in 15 cases, ultrasound in eight cases, bone scintigraphy in five cases, MRI in four cases, and conventional X-rays in four cases. In 16 cases, multiple procedures were carried out.
In examining the PET reports of the 354 scans, FDG uptake was considered as pathological and indicative of ML in 286 cases, as being of uncertain origin in 41 cases, and as unrelated to ML in 37 cases (these cases were therefore reported as negative); it is to be noted that in ten scans, concurrent findings of abnormal FDG uptake attributed to ML and uptake assigned to other causes were obtained. Overall results are shown in Fig. 1.
Among the 286 patients with FDG-PET findings reported as positive for lymphoma, disease was present in 274 ((i.e. there was a true-positive rate of 95.8%), while in the remaining 12 cases (4.2%), FDG-PET results proved to be falsely positive. Causes of false-positive reports are described in Table 2.
In four patients we were not able to find any possible explanation for the positive findings of FDG-PET, nor could a final diagnosis be obtained (patient 4 was affected by herpes zoster but this was unlikely to have been the cause of the observed increased uptake). Nevertheless, all four patients were in clinical and laboratory complete remission at follow-up; in all cases a subsequent FDG-PET study was completely negative (Fig. 2), and therefore these are regarded as unexplained false positives.
18F-FDG PET in a 32-year-old woman with non-Hodgkin’s lymphoma (high grade) involving the mediastinum at presentation (patient 5 of Table 2). After completion of therapy, the patient was in complete remission. PET scan was carried out 6 months later and revealed focal areas of increased 18F-FDG uptake (arrows) in the left lung, in a left rib, and in mediastinal lymph nodes (coronal sections, a). PET findings were reported as consistent with ML relapse. A CT scan carried out 2 weeks later proved completely negative. At follow-up (10 months) the patient was confirmed to be in complete remission and a further FDG PET scan yielded normal results (maximum intensity projection image, b).
In two patients (2 and 8 in Table 1), both the initial and the repeat FDG-PET studies were reported as positive. In both cases the first scan demonstrated increased uptake at superficial nodes that were reported as suspicious for ML relapse. Further examinations were consistent with local inflammation, and therefore it was suggested that FDG-PET should be repeated (at 11 weeks for patient 2 and 20 weeks for patient 8). In both patients, the second PET study demonstrated increased uptake (Fig. 3) that was even more intense, and therefore once again was reported as probably being due to ML. A biopsy was finally performed, demonstrating no involvement by ML in either patient. Thus, considering patients and not individual scans, there were ten false positives and 207 true positives, with a positive predictive value of 95.2%.
18F-FDG PET (maximum intensity projection images) in a 28-year-old man with non-Hodgkin’s lymphoma (high grade) involving the mediastinum at presentation (patient 8 of Table 2). After completion of therapy, the patient was in complete remission. PET scan was carried out 1 year later and revealed several areas of increased 18F-FDG uptake in axillary and inguinal lymph nodes (a). PET findings were reported as consistent with ML relapse. An US+CT evaluation was indicative of adenitis. A further FDG PET study carried out 20 weeks later confirmed the previous PET findings, with even more evident 18F-FDG uptake (b). A biopsy demonstrated the presence of lymphocytic hyperplasia. At follow-up (16 months) the patient was confirmed to be in complete remission.
As already mentioned, in ten scans out of 286, concurrent findings of abnormal FDG uptake attributed to ML and uptake assigned to other causes were obtained. In eight cases the other findings were described as non-pathological, while in two they were related to already known disease (benign thyroid nodules demonstrated by cytology). All ten patients were confirmed to have ML (true positives): data for this subgroup are detailed in Table 3.
There were 41 patients with uncertain findings and they could be divided into two groups: patients with findings reported as pathological but probably unrelated to ML (13 cases) and patients with inconclusive findings (28 cases). In both groups further diagnostic procedures and strict follow-up were strongly suggested.
In all 13 patients with findings reported as suspicious for other disease, pathological causes other than ML were identified as responsible for FDG accumulation; data are detailed in Table 4.
As the results indicate, a second solid tumour was identified in eight of the patients (five malignant and three benign lesions); in no case was the tumour already known at the time of the PET study. Taking into account the overall number of scans reviewed, FDG-PET allowed the detection of a second unsuspected tumour in 8/1,120 cases (0.71%) (Fig. 4).
Images showing lung FDG uptake pattern in patients with different kinds of lesion. a A young patient with Hodgkin’s disease: multiple large areas of intense parenchymal FDG uptake are observed in the lungs. b A patient with lung inflammation but negative for high-grade lymphoma localisations: there is mild and diffuse parenchymal uptake without focal areas of high uptake. c A patient with a secondary lung tumour: a single focal area of high FDG uptake is demonstrated in the left lung, without evidence of nodal involvement
Of the patients with inconclusive findings, four were found to have active ML. In the remaining 24 patients, ML was ruled out, but the cause of increased FDG uptake could be determined in only ten cases: inflammation was responsible in eight (axillary in two, inguinal in one, lung in three and mediastinal in two) and previous surgery in two.
In all 37 patients with findings reported as non-pathological, ML was ruled out. Causes of increased FDG uptake correctly identified in this group were brown adipose tissue (11 cases with bilateral cervical uptake), thymic hyperplasia (eight cases with homogeneous anterior mediastinal uptake), lymph node inflammation (five cases with bilateral mild uptake), muscle contraction (four cases), mediastinal and pulmonary inflammation (four cases with mild diffuse lobar uptake), gastritis (two cases with homogeneous gastric uptake), colitis (two cases with nodal lymphoma and diffuse and homogeneous colic uptake) and soft tissue inflammation (one case with dermal uptake and clinical aspect of inflammation).
There was no significant difference in the results obtained in patients affected by different histological forms of ML. Out of 244 scans of patients with non-Hodgkin’s lymphoma, FDG uptake was considered positive for ML in 193 cases, of uncertain origin in 31 cases (21 inconclusive and 10 probably unrelated to ML) and negative for ML in 20 cases. Among the 193 patients with non-Hodgkin’s lymphoma and positive PET findings, PET results were true positive in 186 cases (96.4%). Similarly, considering the 110 scans carried out in patients with Hodgkin’s disease, PET was positive for ML in 83 cases [results were true positive in 78/83 (94.0%)], uncertain in ten cases (seven inconclusive and three probably unrelated to ML) and negative in 17 cases. The only statistically significant difference between patients with non-Hodgkin’s lymphoma and those with Hodgkin’s disease was the incidence of active ML following an inconclusive PET scan, as all four patients with confirmed disease had non-Hodgkin’s lymphoma.
Discussion
During recent years, a number of studies [8] have demonstrated the effectiveness of FDG-PET in the evaluation of ML. 18F-FDG, however, is not an absolutely tumour-specific tracer since other pathological and non-pathological processes may cause areas of increased FDG uptake [6]. These conditions are generally the source of false-positive reports, thus complicating the use of FDG-PET in clinical practice [9].
Our study clearly indicates that the positive predictive value of FDG-PET for recurrent or residual ML is very high, i.e. about 95%, whether calculated by considering every scan or each patient. This value is significantly better than that reported in a tabulated summary of data from the literature [10] and in a recent review of published studies [11]. The difference may be accounted for by differences in the criteria used to define a positive PET scan. Indeed, in most studies any area of abnormal FDG uptake has been regarded as pathological [5], though it is well known that many potential causes of misinterpretation can be properly recognised [6]. A typical example is thymic hyperplasia, which often shows non-pathological FDG uptake and, as a result, potentially hampers the study interpretation [9, 12]. Thymic hyperplasia is related to the presence of residual thymic tissue capable of responding to therapy. “Thymic rebound” was probably the first cause of false-positive reports identified by papers describing the role of FDG-PET in ML; increased tracer uptake had already been documented in gallium scans. In fact, we have found that proper interpretation of thymic uptake on FDG-PET is possible, even in the presence of active disease at other sites.
In addition, our study included a group of patients with inconclusive PET reports, an occurrence that has generally not been taken into account in previous studies. In daily practice, however, it is recognised that not all scans can be classified as definitely positive or negative for disease, and therefore uncertain reports should also be considered in analysis. Apart from findings probably related to pathological causes other than ML, inconclusive reports in our study occurred in 28/354 scans with follow-up data (7.9%) and in 28/1,120 scans overall (2.5%). If we had incorporated these reports into the group adjudged to be positive for ML, our false-positive rate would have increased from 4.2% to 12.2%.
When examining the inconclusive reports, we found a low incidence of active ML disease, which was demonstrated in only 4/28 cases. We therefore suggest that, in the presence of evident FDG uptake not clearly attributable to disease, diagnosis of active ML should be avoided; rather, further diagnostic tests should be carried out to better define the nature of PET findings (e.g. high-resolution CT of the thorax in the presence of non-focal mildly increased FDG uptake within lung parenchyma) and there should be close follow-up, including another PET study after 3–4 months.
The rate of detection of unknown second tumours, though not high, was significant in our study (eight cases, representing 0.71% of scans). In patients treated for HD, recent data indicate a 5-year risk of 1.9% for development of second primary solid tumours [13]. Extrapolating from the short period covered by our study (about 18 months), it may be speculated that FDG-PET can provide early identification of second malignancies. In our study, a second tumour was detected only in patients without active ML (i.e. in complete remission). Certainly second tumours also occur in patients with ML relapse, and in this situation PET may lack sensitivity, as areas of increased FDG uptake due to ML may mask the existence of another tumour, especially in the presence of diffuse disease. To our knowledge, however, this event has never been reported in the literature.
In our study, the most frequent reason for a false-positive report was inflammation. It has often been claimed that FDG avidity of anti-inflammatory cells such as macrophages and leucocytes represents a limitation of FDG-PET, since active inflammation, such as granulomas and abscesses, can consequently be falsely interpreted as disease [7]. In our study, however, the presence of inflammation did not necessarily cause false-positive reports; in fact, faintly increased FDG uptake in the presence of clinical signs of inflammation was correctly interpreted in most cases. Particular attention should be paid to the location of inflammation when assessing the probability of disease. In lymphoma patients, increased uptake in bowel is most likely attributable to inflammation while uptake at any nodal site is suspicious for relapse.
The locations of increased FDG uptake which most frequently led to false-positive results were the axillary, mediastinal and inguinal nodes and the lungs. The reason is probably the higher incidence of inflammation at these sites. As expected, these were the most frequently described locations in cases with inconclusive findings. This finding is consistent with those described in the literature [11]. Nevertheless, in some cases, faint symmetrical FDG uptake was observed at nodal sites, which were properly reported as simple adenitis. Similarly, some cases of bronchitis and bronchopneumonia were properly identified on the basis of uptake characteristics. It has previously been suggested that interpretation of PET scans is improved when relevant studies and clinical data are considered [6]. We believe that in many cases a simple clinical examination may also be extremely useful.
Recently, the presence of brown adipose tissue (also called USA fat) has been heralded as a relatively frequent cause of FDG accumulation [14]. Greater availability and use of PET/CT technology will surely contribute to correct identification of brown fat uptake, and our results confirm that brown fat uptake is not an uncommon observation. In our study, however, the presence of FDG accumulation in fat did not limit the number of true-negative reports. A critical feature of any test, including FDG-PET, in the setting of oncological patients has always been the specificity of the approach. In lymphoma patients, several causes of false-positive FDG-PET studies have been claimed to exist [7]. Our study indicates that most of the potential causes of false positives can be clearly identified. Precise indication of these potential confounders in the report is mandatory to avoid unnecessary biopsy. On the other hand, one of the most important skills in PET interpretation remains the recognition of its limitations. We therefore support careful PET reporting: in the presence of clear findings, a definitive diagnosis can be given, while in many other cases PET may be used to direct the clinician to further investigations that will permit a correct diagnosis.
Several approaches have been suggested to increase PET specificity in ML. Two important methods in particular are performing a baseline scan at presentation and increasing the experience of PET readers. In patients with ML, it is common knowledge that abnormal uptake at an initially involved site is likely to be persistent disease. On the other hand, if it is seen at a site initially not involved on the baseline scan, other causes of FDG uptake must be ruled out. In our series, baseline scans were obtained at the time of initial presentation of disease in only a few patients , and we thus have few data to support the usefulness of baseline PET studies inr avoiding false positives. Nevertheless, we feel that baseline PET studies reduce false negatives, especially since the level of uptake of FDG in a particular lymphoma cannot be reliably predicted [15].
The learning curve involved in the interpretation of PET may reduce the number of false positives as well [16, 17]. Certainly, experienced readers are less likely to report muscular or normal intestinal uptake as positive findings [16, 18]. PET/CT scanners may be extremely useful for the same purpose, and the amount of data regarding the ability of PET/CT to identify non-pathological FDG uptake is rapidly growing [14]. In our series, increased uptake could easily be correctly identified in most cases on the basis of normal FDG uptake characteristics: in these cases the experience of the PET reader is clearly crucial. This simple observation reaffirms the importance of careful review of positive PET findings and comparison with known FDG uptake characteristics as well as other available patient information, including results of diagnostic tests and treatment course.
Conclusion
Our data confirm the very high but not absolute specificity of FDG-PET for ML. As has previously been suggested, increased FDG uptake may also be observed in patients without active disease; in most cases, however, non-pathological FDG accumulation can be properly identified. A careful evaluation of PET findings, along with consideration of all clinical and other investigational data, limits the false-positive rate to less than 5%. Nevertheless, inconclusive scans are possible, although not frequent. Most often they are a result of inflammation, which subsequently resolves. Overall, our data confirm the reliability and thus the usefulness of FDG-PET in patients with ML for evaluation of definitive response to therapy and during follow-up.
References
O’Doherty MJ, Hoskin PJ. Positron emission tomography in the management of lymphomas: a summary. Eur J Nucl Med Mol Imaging 2003;30(Suppl 1):s128–30.
Hoskin PJ. PET in lymphoma: what are the oncologist’s needs? Eur J Nucl Med Mol Imaging 2003;30(Suppl 1):s37–41.
Romer W, Schwaiger M. Positron emission tomography in diagnosis and therapy monitoring of patients with lymphoma. Clin Positron Imaging 1998;1(2):101–10.
Guay C, Lepine M, Verrault J, Bernard F. Prognostic value of PET using 18F-FDG in Hodgkin’s disease for posttreatment evaluation. J Nucl Med 2003;44:1225–31.
Weihrauch MR, Re D, Scheidhauer K, Ansen S, Dietlein M, Bischoff S, et al. Thoracic positron emission tomography using 18F-fluorodeoxyglucose for the evaluation of residual mediastinal Hodgkin disease. Blood 2001;98(10):2930–4.
Barrington SF, O’Doherty MJ. Limitations of PET for imaging lymphoma. Eur J Nucl Med Mol Imaging 2003;30(Suppl 1):s117–27.
Boomanji JB, Syed R, Brock C, Jankowska P, Dogan A, Costa DC, et al. Pitfalls of positron emission tomography for assessing residual mediastinal mass after chemotherapy for Hodgkin’s disease. J Clin Oncol 2002;20(15): 3347–9.
Kostakoglu L, Goldsmith SJ. Fluorine-18 fluorodeoxyglucose positron emission tomography in the staging and follow-up of lymphoma: is it time to shift gears? Eur J Nucl Med 2000;27(10):1564–78.
Spaepen K, Stroobants S, Dupont P, Bormans G, Balzarini J, Verhoef G, et al. 18F-FDG PET monitoring of tumour response to chemotherapy: 18F-FDG uptake correlate with the viable tumour cell fraction? Eur J Nucl Med Mol Imaging 2003;30(5):682–8.
Gambhir SS, Czernin J, Schwimmer J, Silverman DHS, Coleman RE, Phelps ME. A tabulated summary of the FDG PET literature. J Nucl Med 2001;42:1S–93S.
Reske SN. PET and restaging of malignant lymphoma including residual masses and relapse. Eur J Nucl Med Mol Imaging 2003;s1:S89–96.
Weinblatt ME, Zanzi I, Belakhlef A, Babchyck B, Kochen J. False positive FDG-PET imaging of the thymus of a child with Hodgkin’s disease. J Nucl Med 1997;38(6):888–90.
Chronowski GM, Wilder RB, Levy LB, Atkinson EN, Ha CS, Hagemeister FB, et al. Second malignancies after chemotherapy and radiotherapy for Hodgkin disease. Am J Clin Oncol 2004;27(1):73–80.
Yeung HWD, Grewal RK, Gonen M, Schoder H, Larson SM. Patterns of 18F-FDG uptake in adipose tissue and muscle: a potential source of false-positives for PET. J Nucl Med 2003;44:1789–96.
O’Doherty MJ, MasDonald E, Barrington SF, Mikhaeel NG, Schey S. Positron emission tomography in the management of lymphomas. Clin Oncol 2002;14:415–26.
Strauss LG. Fluorine-18 deoxyglucose and false positive results: a major problem in the diagnostics of oncological patients. Eur J Nucl Med 1996;23:1409–15.
Sandherr M, von Schilling C, Link T, Stock K, von Bubnoff N, Peschel C, et al. Pitfalls in imaging Hodgkin’s disease with computed tomography and positron emission tomography using fluorine-18-fluorodeoxyglucose. Ann Oncol 2001;12:719–22.
Shreve PD, Anzai Y, Wahl RL. Pitfalls in oncologic diagnosis with FDG PET imaging: physiologic and benign variants. Radiographics 1999;19:61–77.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Castellucci, P., Zinzani, P., Pourdehnad, M. et al. 18F-FDG PET in malignant lymphoma: significance of positive findings. Eur J Nucl Med Mol Imaging 32, 749–756 (2005). https://doi.org/10.1007/s00259-004-1748-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00259-004-1748-x