Abstract
This study demonstrates high-efficiency sterilisation of single cancer cells in a SCID mouse model of leukaemia using rituximab, a monoclonal antibody that targets CD20, labelled with terbium-149, an alpha-emitting radionuclide. Radio-immunotherapy with 5.5 MBq labelled antibody conjugate (1.11 GBq/mg) 2 days after an intravenous graft of 5·106 Daudi cells resulted in tumour-free survival for >120 days in 89% of treated animals. In contrast, all control mice (no treatment or treated with 5 or 300 µg unlabelled rituximab) developed lymphoma disease. At the end of the study period, 28.4%±4% of the long-lived daughter activity remained in the body, of which 91.1% was located in bone tissue and 6.3% in the liver. A relatively high daughter radioactivity concentration was found in the spleen (12%±2%/g), suggesting that the killed cancer cells are mainly eliminated through the spleen. This promising preliminary in vivo study suggests that targeted alpha therapy with 149Tb is worthy of consideration as a new-generation radio-immunotherapeutic approach.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Single cancer cells in circulation and small cancer cell clusters can be effectively targeted with radio-immunoconjugates that specifically bind to the cells and deliver the required dose. Alpha-emitting radioisotopes may be of great advantage in this kind of therapy because of their higher linear energy transfer (LET) value and, consequently, the shorter penetration track compared to β−- and γ-radiation [1]. It has been shown that only a very few alpha-hits are sufficient to kill a cell [2], and the short range of the alpha particles increases the safety profile of alpha-emitters because non-specific irradiation of normal tissue (or plasma) around the target cells is greatly reduced or absent [3]. Additionally, since single cancer cells in circulation are immediately accessible to the injected (i.v.) radio-immunoconjugate, the shorter half-lives of a few alpha-emitting radioisotopes may be advantageous [4]. Only a small number of alpha-emitting radionuclides fulfill the requirements for this specific nuclear medical application: 225Fm, 225Ac, 224Ra, 223Ra, 213Bi, 212Bi, 211At and 149Tb. Especially 213Bi and 211At have proven to be very promising candidates, because of the availability (225Ac/213Bi generator) and the convenient half-life of 7.2 h (211At) (for example see refs. [5, 6]).
Today, new approaches in conjugation with chelating ligands allow the stable labelling of macromolecules (such as monoclonal antibodies) or peptides with metallic radionuclides. The first clinical proof-of-principle of targeted alpha therapy was observed using the HuM195 antibody labelled with the short-lived (46 min) 213Bi radionuclide [7], which is a daughter product in the decay chain of 225Ac (10 days). The mother nuclide, 225Ac, is itself considered a candidate for targeted alpha therapy (TAT), and corresponding studies are ongoing [3, 8]. A potential drawback with use of 225Ac is the possibility that the short-lived alpha-emitting daughter nuclides in the decay chain will escape from the place of origin, leading to uncontrolled deposition of the radiation dose throughout the body.
The partial alpha-emitting nuclide 149Tb (T 1/2=4.118 h, E α=3.967 MeV; range in tissue =28 μm), which belongs to the group of rare earth elements, has been proposed as a promising alpha-emitter for TAT [4, 9, 10, 11]. Its chemical behaviour is very close to that of yttrium or lutetium, whose isotopes 90Y and 177Lu are currently the most predominant metallic radionuclides used in clinical radio-immunotherapy (RIT) [12]. Thus, existing approaches for labelling of chelated bioconjugates with these metallic radionuclides, as well as 166Ho, 153Sm, 213Bi or 225Ac, can be directly applied to 149Tb. Previous in vitro studies have revealed certain advantages of 149Tb over 213Bi for treating single cells [13]. These advantages, which relate to the lower energy and higher LET of alpha particles emitted by 149Tb, partially compensate for its lower alpha branching (17%, Fig. 1) [13, 14]. The longer half-life of 149Tb (4.12 h) compared with 213Bi (46 min) represents a clear advantage, both at the level of bioconjugate preparation and for administration to patients for tumour cell targeting. On the other hand, the fate of long-lived daughter products that appear during the decay of 149Tb would need to be considered carefully in the dosimetry (Fig. 1).
Simplified decay scheme of 149Tb and the list of the most relevant gamma transitions (adopted from [17]). Note that the decay of the 149Tb itself as well as the first daughter products is accompanied by relatively intense gamma emission, while the longer-lived daughter products of the second and third generations show very little gamma contribution
In this paper we describe the first in vivo survival study using a 149Tb-based TAT approach in SCID (severe combined immuno-deficient) mice. SCID mice, being deficient in T and B cell immune defence, easily develop tumour masses after injection of cancer cells. Daudi cells, which are derived from a human Burkitt lymphoma, are one of several cell lines that can rapidly colonise these mice. Depending on the injection route, different tumour types can develop. As few as 100 injected (i.v.) Daudi cells are sufficient to kill SCID mice due to tumour development [15]. Since Daudi cells express a high number of CD20 antigens, rituximab can target Daudi cells with high specificity. Thus, an early stage of this model, within 3 days of i.v. xenograft, before the formation of manifested tumour nodes, provides an ideal system to study the proposed advantages of 149Tb-based TAT.
The primary aim of this work was to examine the efficacy of 149Tb-labelled rituximab to specifically kill circulating single cancer cells or small cell clusters in vivo. SCID mice following i.v. xenograft with Daudi cells represent a perfect model for leukaemia [16]. Our experimental model involves TAT intervention within 3 days of i.v. xenograft, and hence before the formation of manifested tumour nodes, which we did not intend to target in this study. According to our experimental hypothesis, mice xenotransplanted with a lethal number of Daudi cells will survive provided that a sufficient dose of 149Tb has been delivered via rituximab to all tumour cells. Secondly, we aimed to obtain information about the behaviour of the daughter products generally formed in the radioactive decay chain. The 17% alpha decay mode of the 149Tb generates an isobar chain with the mass number A=145 with 145Eu (T 1/2=5.93 days), 145Sm (T 1/2=340 days) and 145Pm (T 1/2=17.7 years). The EC-process decay chain of 149Tb forms the stable 149Sm passing the 149Gd (T 1/2=9.28 days) and the 149Eu (T 1/2=93.1 days) ([17], Fig. 1). Most of these isotopes are easily detectable using high-resolution gamma spectroscopic techniques (Fig. 1). In particular, we expected that differences in daughter isotope behaviour induced by the different decay modes (alpha versus EC) would be apparent.
Materials and methods
Cell line
Daudi cells (ATCC Nr. CCL-213) were used to simulate a leukaemia model in mice. The cells were cultured in RPMI 1640 medium supplemented with 10% heat-inactivated fetal calf serum and 0.5% penicillin (10,000 U/ml)/streptomycin (10 mg/ml) (Sigma-Aldrich). The cell suspension to be injected into mice was prepared by centrifuging the culture for 3 min at 1,200 rpm, washing with PBS and re-suspending in PBS at 2.5·107 cells per ml.
Antibody conjugate
Rituximab antibody (Rituxan; IDEC Pharmaceuticals, San Diego, and Genentech Inc, San Francisco) is a chimeric version of anti CD-20 monoclonal antibody consisting of human IgG1 constant domains and murine variable domains. The rituximab antibody conjugated with SCN-CHX-A-DTPA (2-(4-isothiocyanatobenzyl)-cyclohexyl-diethylenetriamine penta-acetic acid), used in this study, was kindly provided by Dr. D.A. Scheinberg (Memorial Sloan Kettering Cancer Center, New York).
Radionuclide
The 149Tb was produced using the on-line isotope separator facility ISOLDE at CERN (Geneva, Switzerland) [18, 19]. A tantalum-foil target (120 g/cm2) was irradiated with 1.0- or 1.4-GeV protons delivered from the CERN PS-Booster accelerator. The radio-lanthanides generated in the spallation process are released from the target material, which is kept at about 2,200°C, ionised by surface ionisation and accelerated to 60 keV. From the obtained radioactive ion beams, the A=149 isobars (149Dy, 149Tb and molecular ions 133CeO+ and 133LaO+) were implanted (60 keV) and thus collected in thin layers of KNO3 (10 mg/cm2) on aluminium backings. The 149Tb was separated from its daughters (149Gd and 145Eu) and the pseudo-isobars 133Ce and 133La by cation exchange chromatography using Aminex A5 resin and α-hydroxyisobutyric acid as eluent. A typical elution chromatogram is presented in Fig. 2. The 149Tb fraction (150–200 µl) was evaporated to dryness and re-dissolved in 50 µl of 100 mM HCl. The final 149Tb concentration was 2 GBq/ml (54 mCi/ml) at the end of chromatographic separation (EOS).
Separation of the A=149 isobars obtained in the on-line isotope separation process at ISOLDE by using cation exchange chromatography. Column: Aminex A 5 in NH4 + form, 3×60 mm2, eluent: α-HIBA, elution speed: 100 µl/min (one drop =35 µl= one fraction). The isotopic content of each fraction has been determined by high-resolution gamma ray spectrometry
Labelling procedure
From 25 to 40 µl of the 149Tb solution characterised above was used immediately for the labelling procedure. The pH was adjusted to 5.5 by adding 60 µl of 3 M CH3COONH4 solution, followed by the addition of 10 µl (40 mg/ml) ascorbic acid. After adding 5 µl of a stock solution of the chelated antibody in PBS (10 mg/ml), the mixture was incubated for 10 min at room temperature, before dilution to a final volume of 1.0 ml in PBS-1% human serum. The radiochemical purity of the labelled rituximab was determined by instant thin-layer chromatography (1.5×15 cm ITLC-SG strips, Gelman Instrument Company) using 0.1 M acetate buffer of pH 6 as a mobile phase and the linear analyser (Berthold). The injection of the radio-immunoconjugate into the mice was performed 1 h after EOS. The in vitro behaviour of the labelled bioconjugate (immunoreactivity, cell binding, cell killing efficiency) has been described in a previous paper [14]. With the same antibody we observed up to 55% cell binding without extrapolation to infinite antigen excess.
Mice survival studies
The in vivo studies were performed using 26 female SCID mice (C.B.-17/ICR, Iffa Credo) under the authorisation Nr: GE 31.1.1049/1879/II. The mice, which were 8 weeks old at the start of the experiment and weighed 20 g on average, were kept in sterile, ventilated boxes. Before injecting cells and antibodies, mice were anaesthetised by i.p. (intraperitoneal) injection of 10 ml per kg (typically 0.2 ml) of an anaesthetic (2.4 ml Ketasol 50, 0.8 ml Rompun, 6.8 ml 0.9% NaCl). Each mouse received 5·106 Daudi cells by injection of 0.2 ml cell suspension in PBS into the tail vein. Two days after xenotransplantation the mice were divided into four groups: the first group received 5 μg rituximab in 0.1 ml PBS i.v.; the second group, 300 μg rituximab in 0.1 ml PBS i.v.; and the third group, 5.5 MBq 149Tb-CHX-A-DTPA-rituximab radio-immunoconjugate (5 μg labelled rituximab in 0.2 ml, i.v.); the fourth group was left without any treatment. A summary of the in vivo study is presented in Table 1. According to the authorised protocol, the mice were surveyed for 120 days: their behaviour was logged each day, their condition was supervised once a week by a veterinarian, and they were weighed three times a week. At the appearance of obvious signs of paralysis, visible tumour masses or a weight loss of >15%, the mice were sacrificed. One mouse was sacrificed shortly after injection (2 h p.i.) and kept deep-frozen for later analysis, in order to act as a reference for later quantification of the daughter radioactivity distribution.
Retention and daughter radioactivity distribution
Organ samples were taken from the sacrificed mice and the radioactivity concentration of the long-lived daughter products was determined by using high-resolution gamma spectroscopy (18% HP-Ge detector in combination with the Gamma spectrometer Genie 2000, Canberra). Whole, intact mice, as well as isolated organ samples, were measured. Since the radioactivity content of the samples was essentially very low, long measuring times (between 1 and 24 h) were applied.
Statistical analysis
The survival of animals until sacrifice because of disease development or the end of the experiment (no disease development) was compared between the different groups according a Kaplan Meier analysis using the Lee-Desu evaluation of the Unistat 3.0 statistical package (Megalon, Novato CA, USA).
Results
Preparation of labelled rituximab
Mass-separated and radiochemically pure 149Tb was obtained after chromatographic separation of the collected isobars with mass number A=149 at the on-line mass separator facility at CERN (Fig. 2). The overall time needed for the radiochemical separation and the labelling procedure was 1 h. Radiolabelling of the rituximab with this 149Tb-preparation was almost quantitative (>99%) within 10 min incubation time. The obtained preparation was thus ready for injection without further purification. The radioactivity concentration of the labelled antibody solution was 27.8 MBq/ml (0.75 mCi/ml), while the specific activity was 1.11 GBq/mg (30 mCi/mg) at the moment of injection.
Survival in a SCID mouse model of leukaemia
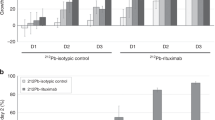
We set out to evaluate the efficacy of 149Tb-based TAT using a SCID mouse model of leukaemia [16]. Our experimental model involved the i.v. xenografting of a lethal number of Daudi cells followed by TAT intervention at a time point when most of the Daudi cells would be expected to remain in circulation, and before the appearance of manifested tumours, which we did not intend to target in this study. Survival data over a period of 4 months for treated mice and controls are shown in Fig. 3. All mice in the untreated control group developed clear signs of Burkitt lymphoma and were consequently sacrificed within 37 days. Fifty percent of them developed visible macroscopic tumours while the others were sacrificed when they showed clear signs of paralysis or a weight loss >15% of the initial body weight (Table 1).
The injection of a single, low dose of rituximab (5 µg/animal) did not show any therapeutic effect, and all mice in this group had to be sacrificed within 43 days. As can be seen from Fig. 3, the survival curves of this group and the control group (untreated mice) are almost identical. Of the mice in this group, 83% expressed obvious signs of paralysis or weight loss of >3 g, while 17% developed visible macroscopic tumour masses.
A different survival pattern was observed after treatment with a high dose of rituximab (300 µg per animal, corresponding to 15 mg/kg). Although a single dose of 15 mg/kg rituximab significantly increased the life expectancy—50% of mice in this group survived 100 days—ultimately, tumours developed in all animals (an example is shown in Fig. 4a) before the end of the observation period.
In contrast, the mice treated with the radioactive 149Tb-CHX-DTPA-rituximab (5 µg rituximab per animal) were almost completely protected over the entire observation period, with only one mouse in this group being lost after 48 days due to abdominal tumour growth. The remaining eight mice (89%) showed normal behaviour without any signs of disease for 4 months after grafting (Fig. 4b). All of these mice were sacrificed after 120 days and were found to be tumour free at dissection. Thus, a single injection of 5.5 MBq 149Tb-labelled rituximab (5 µg MoAb), which corresponds to an injected dose of 280 MBq/kg body weight (7.5 mCi/kg), produced long-term survival without evidence of any disease at 120 days. The survival increase after the RIT compared with all the control groups (no treatment, 5 µg and 300 µg unlabelled rituximab) was highly significant in the statistical Lee-Desu comparisons (P<0.005).
Biodistribution of labelled rituximab and the daughter radionuclides
In Fig. 5 we present typical gamma spectra of retained activity in organs recorded 120 days after injecting the short-lived radio-immunoconjugate. The biodistribution of 149Tb-CHX-A-DTPA-rituximab radio-immunoconjugate shortly after injection was assessed using a single mouse sacrificed at 2 h. The retention of the long-lived daughter nuclides at 120 days after injection is presented in Table 2. After 2 h, the organs with high blood pool, like the spleen, heart and kidney (42%, 41% and 24% ID/g), showed relatively high radioactivity concentration. High amounts of the radio-immunoconjugate were found in the liver at this time point (18%±3% injected dose), confirming the results of earlier systematic studies [20]. The values in the other organs were relatively low. After 120 days, 71.6% of the primary injected radioactive atoms had been excreted from the mice. The retention of the daughter products was 28.4%±4%, of which 91.1% remained in the bone tissue and 6.3% in the liver.
Discussion
Protection of mice treated with labelled rituximab
Here we show that TAT with rituximab labelled with the high-purity alpha-emitting radio-lanthanide 149Tb led to almost complete protection of xenografted mice over 4 months without detectable signs of toxicity, under conditions where all animals in the control groups had to be sacrificed during the observation period due to the development of tumour diseases. The efficacy of the radionuclide bioconjugate as opposed to the unconjugated tumour targeting antibody alone is underlined by the complete lack of protection in the control group that received 5 µg unlabelled rituximab per animal, and the relatively poor protection afforded by the higher dose unlabelled rituximab group (300 µg per animal). The degree of protection afforded by the 149Tb-labelled rituximab indicates that TAT with 149Tb is, on the basis of its efficacy, worthy of further consideration as a novel radio-immunotherapeutic strategy.
Biodistribution of label and decay products
From earlier studies we have learnt that once the lanthanides are trapped in a tissue, like liver or bone, they are fixed quite stably [20, 21]. The blood clearance for free radio-lanthanides or radio-lanthanides injected in solutions containing chelate ligands (citrate, EDTMP, NTA, EDTA, DTPA and others) is fast (half-time <1 h) [21, 22]. The radio-lanthanides are then present mainly in the bone matrix and the liver, with the liver uptake determined by the ionic radius of the lanthanide [21, 22, 23]. In the case of macromolecules (like monoclonal antibodies) the blood clearance is slow (half-time ~1 day) [20]. Thus, most of the 149Tb will decay while the labelled bioconjugate is in circulation and the free daughter nuclides formed in the radioactive decay would follow the biodistribution known for free radio-lanthanides. The biodistribution found 120 days after treatment corresponds to the distribution patterns known for the free radio-lanthanide: highest daughter nuclide accumulation in bone and liver (91.1% and 6.3% of the retained activity, respectively) [21, 22]. The spleen shows a radioactivity concentration almost as high as bone and significantly higher compared with liver. We interpret this result as evidence that the targeted and killed cancer cells are eliminated mainly through the spleen, where the remaining radioactive daughter atoms are then trapped.
The long-lived daughter products are formed along two main decay processes: the isobar chain with A=145 is generated via the alpha decay mode of the initial 149Tb, while the isobar chain with A=149 is formed after the EC- or β+-process. In the case of an alpha decay, the recoil energy of the 145Eu daughter nuclei (110 keV) exceeds significantly the chemical binding energy. Consequently, the original molecule, the antibody construct, is destroyed and the daughter atom is initially stabilised as free Eu3+ ion. In the case of the EC-decay mode, the bound rupture is induced due to the Auger electron emission forming free daughter species [24, 25] with 100% efficiency. However, it cannot be assumed that the daughter species escapes from its place of origin; it could eventually be bound to other proteins in the immediate environment. Consequently, one may not necessarily expect identical behaviour from daughter products generated in the two different pathways: alpha or EC process. Analysis of the gamma spectroscopic data revealed that there was no statistically significant difference in the ratio of retained 145Sm to 149Eu in the organs from that predicted by the branching ratio of 149Tb. Thus, the radioactive decay pathway does not influence the biodistribution or redistribution of the long-lived daughter lanthanides.
Extrapolation to clinical application
A preliminary dose estimation for patients injected with 5 GBq 149Tb-rituximab was performed based on MIRDOSE 3.1 [26]. Assuming total decay of 149Tb-rituximab in circulation and 100% retention of daughter nuclides in the body with a bone uptake of 91%, the total equivalent dose to the bone marrow as the critical organ would be 540 mSv/5 GBq (108 mSv/GBq) (see also Table 3). 149Tb itself would contribute 66.7% of the bone marrow radiation dose (45.2% due to the α-radiation using an α-radiation weight factor of WR=10) and 21.5% due to its γ- and β+-radiation) while the daughter nuclides would contribute 33.3% only. The dose contribution from daughter nuclides estimated in this way represents a worst-case estimation (assuming 100% retention), since only 28.4% of the long-lived daughter products were retained in mice 120 days p.i. Thus, injection of a potentially therapeutic activity, 5 GBq 149Tb-rituximab, in a 70-kg patient, would deliver a bone marrow radiation dose far below the critical level. This preliminary dose estimation is well compatible with considerations presented in the review by McDevitt et al. [8].
For further reduction of the retention of the daughter nuclides one could apply single or multiple injections of chelating ligands like EDTA or DTPA during or shortly after the treatment. This approach is already practiced as a preventive action in treatments with 90Y- or 177Lu-DOTATOC [27].
Time constraints and availability
Spallation reaction in combination with on-line mass separator technology was used for the production of 149Tb for this study. The radiochemical separation and purification of the 149Tb were relatively easy to perform in about 30 min in this specific case, since we started from non-carrier-added preparations. The final 149Tb preparation was obtained in very high purity and in a small volume, and the labelling of the bioconjugate was fast (10 min) and almost quantitative. The administration of the preparation should be carried out as rapidly as possible after purification of the 149Tb, since levels of contamination with daughter nuclides will increase with time. For example, application of a fixed dose of the 149Tb-labelled bioconjugate 4 h after the final purification of the isotope itself (EOS) leads to an increase in the long-lived daughter content by a factor of 2. According to the preliminary dose estimation one could define a shelf-life for the 149Tb-labelled bioconjugate of about 4–6 h. For a longer delay it would be advisable to repurify the 149Tb from the accumulated daughter products, a process that could require 30 min.
Several nuclear processes could be used to make this interesting alpha-emitting isotope available on large scale: light particle (p, d, He)-induced reactions on 152Gd as target material, heavy ion-induced reactions on light lanthanide targets or spallation reaction on Ta as target [19]. Off-line and on-line mass separation process may support a very high isotopic purity [19, 28].
For the time being, only a few centres may be able to make this isotope. On the other hand, all the above-mentioned technologies are well developed and available today. In summary, should 149Tb continue to show promise in further studies of TAT, then it would be technically feasible to make the isotope available on a large scale and on a routine basis.
References
Hall EJ. Radiobiology for the radiologist. 4th edn. Philadelphia: Lippincott, 1994.
Maecklis RM, Lin JY, Beresford B, Achter RW, Hines JJ, Humm JL. Cellular kinetics, dosimetry, and radiobiology of alpha-particle radioimmunotherapy: inducing of apoptosis. Radiat Res 1992; 130:220–226.
McDevitt MR, Ma D, Simon J, Frank RK, Scheinberg D. Design of225Ac-radiopharmaceuticals. Appl Rad Isot 2002; 57:841–847.
Allen BJ, Blagojevic N. Alpha and beta emitting radiolanthanides in targeted cancer therapy: the potential role for terbium-149. Nucl Med Commun 1996; 17:40–47.
Zalutsky MR, Vaidyanathan G. Astatine-211 labeled radiotherapeuticals: an emerging approach to targeted alpha particle therapy. Current Pharm Design 2000; 6:1433–1455.
Huber R, Seidl C, Schmid E, Seidenschwang S, Becker K-F, Schuhmacher C, Apostolidis C, Nikula T, Kremmer E, Schwaiger M, Senekowitsch-Schmidtke. Locoregional alpha-radioimmunotherapy of intraperitoneal tumor cell dissemination using a tumor-specific monoclonal antibody. Clin Cancer Res 2003; 9:3922–3928.
Jurcic JG, Larson SM, Sgouros G, McDevitt MR, Finn RD, Divgi CR, Ballangrud ÅM, Hamacher KA, Ma D, Humm JL, Brechbiel MW, Molinet R, Scheinberg DA. Targeted α-particle immunotherapy for myeloid leukemia. Blood 2002; 100:1233–1239.
McDevitt MR, Sgouros G, Finn RD, Humm JL, Jurcic JG, Larson SM, Scheinberg DA. Radioimmunotherapy with alpha-emitting radionuclides. Eur J Nucl Med 1998; 25:1341–1351.
Allen BJ, Goozee G, Imam S, Sarkar S, Leigh J, Beyer G-J. Targeted cancer therapy: The potential role of terbium-149. 6th International Conference on Radiopharmaceutical Dosimetry, Gatlington, Tenn. (USA), May 7–10, 1996, CERN-PPE/96–127, 1996
Charlton DE, Utteridge TD, Allen BJ. Theoretical treatment of human hemopoietic stem cell survival following irradiation by alpha particles. Int J Radiat Biol 1998; 74:111–118.
Allen BJ. Can alpha immunotherapy succeed where other modalities have failed? Nucl Med Commun 1999; 20:205–207.
Wagner HN Jr, Wiseman GA, Marcus CS, et al. Administration guidelines for radioimmunotherapy of Non-Hodgkin’s lymphoma with90Y-labeled anti-CD20 monoclonal antibody. J Nucl Med 2002; 43:267–272.
Miederer M, Seidl C, Beyer G-J, Charlton DE, Vranješ-Đurić SD, Čomor JJ, Huber R, Nikula T, Apostolidis C, Schuhmacher C, Becker K-F, Senekowitsch-Schmidtke R. Comparison of the radiotoxicity of two alpha emitting immunoconjugates, terbium-149 and bismuth-213, directed against a tumor-specific, exon 9 deleted (d9) E-cadherin adhesion protein. Radiat Res 2002; 159:612–620.
Vranješ SD, Miederer M, Čomor JJ, Soloviev D, Beyer G-J and the ISOLDE collaboration. Labeling of monoclonal antibodies with 149-Tb for targeted alpha therapy. J Lab Comp Radiopharm 2001; 44:718–720.
Ghetie MA, Richardson J, Tucker T, Jones D, Uhr JW, Vitetta ES. Disseminated or localized growth of a human B-cell tumor (Daudi) in SCID mice. Int J Cancer 1990; 45:481–485.
McDevitt MR, Ma D, Lai LT, Simon J, Borchardt P, Frank RK, Wu K, Pellegrini V, Curcio MJ, Miederer M, Bander NH, Scheinberg DA. Tumor therapy with targeted atomic nanogenerators. Science 2001; 294:1537–1540.
Firestone RB. Table of isotopes, 8th edn. New York: Wiley-Interscience, 1996.
Kugler E. The ISOLDE facility. Hyperfine Interactions 2000; 129:23–42.
Beyer G-J, Čomor JJ, Daković M, Soloviev D, Tamburella C, Hagebø E, Allan B, Dmitriev SN, Zaitseva NG, Starodub GY, Molokanova LG, Vranješ SD, Miederer M, and the ISOLDE Collaboration. Production routes of the alpha emitting 149-Tb for medical application. Radiochim Acta 2002; 90:247–252.
Beyer G-J, Offord RE, Künzi G, Jones RML, Ravn U, Aleksandrova Y, Werlen RC, Mäcke H, Lindroos M, Jahn S, Tengblad O, and the ISOLDE Collaboration. Biokinetics of monoclonal antibodies labeled with radio-lanthanides and 225-Ac in xenografted nude mice. J Label Compd Radiopharm 1995; 37:229–530.
Beyer G-J, Münze R, Fromm WD, Franke WG, Henke E, Khalkin VA, Lebedev NA. Spallation produced 167-Tm for medical application. In: Medical radionuclide imaging 1980, vol 1. Vienna: IAEA; 1981:587 (IAEA-SM-247/60).
Beyer G-J, Offord R, Künzi G, Aleksandrova Y, Ravn U, Jahn S, Backe J, Tengblad O, Lindroos M, and the ISOLDE Collaboration. The influence of EDTMP-concentration on the biodistribution of radio-lanthanides and225Ac in tumor bearing mice. Nucl Med Biol 1997; 24:367–372.
Beyer G-J, Bergmann R, Schomäcker K, Rösch F, Schäfer G, Kulikov EV, Novgorodov AF. Comparison of the biodistribution of225Ac and radiolanthanides as citrate complexes. Isotopenpraxis 1990; 26:111–114.
Beyer G-J, Herrmann E, Khalkin VA. Chemical effects related to different radioactive decay processes of cerium isotopes chelated with different polyaminocarbonic acids. Dubna: JINR P 12–7758, 1974.
Beyer G-J, Herrmann E. Chemical effects of nuclear transformations in lanthanide chelate complexes. In: Proceedings of the COST Chemistry Action D18, Mid Term Evaluation Workshop on Lanthanide Chemistry for Diagnosis and Therapy, Heidelberg (Germany), July 22–25, 2002, p 26.
Stabin MG. MIRDOSE: personal computer software for internal dose assessment in nuclear medicine. J Nucl Med 1996; 37:538–546.
Breeman WAP, DeJong M, Krenning EP. Labeling of DOTA-peptides at high specific activities. ICFE’5, Geneva, Switzerland, August 24–29, 2003, CO4-SL8, abstract book p 197.
Beyer G-J, Ruth TJ. The role of electromagnetic separators in the production of radiotracers for bio-medical research and nuclear medical applications. NIM B 2003; 204:694–700.
Acknowledgement
The authors wish to thank Prof. S. Larson (MSKCC New York) for his very valuable discussion during the preparation of this manuscript and Prof. D. Scheinberg (MSKCC New York) for providing the rituximab-DTPA bioconjugate used in this study. The support by the Swiss National Science Foundation Project Nr. 31–53672.98 and by the European Commission within the HPRI-Program Nr. HPRI-CT-1999–00018 is acknowledged.
Author information
Authors and Affiliations
Consortia
Corresponding author
Rights and permissions
About this article
Cite this article
Beyer, GJ., Miederer, M., Vranješ-Đurić, S. et al. Targeted alpha therapy in vivo: direct evidence for single cancer cell kill using 149Tb-rituximab. Eur J Nucl Med Mol Imaging 31, 547–554 (2004). https://doi.org/10.1007/s00259-003-1413-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00259-003-1413-9