Abstract
Objective
We aim to present a novel imaging technique utilizing weight-bearing CT with syndesmotic stress to identify subtle, unstable syndesmotic injuries. We illustrate this with a case presentation of such an injury in an elite athlete that ultimately required operative fixation.
Materials and methods
In order to perform an augmented stress weightbearing CT, the patient is in the standing position, feet facing forward, and with weight distributed equally. The patient is then coached to internally rotate the shin and knee. This places an external rotational moment on the TFS due to the planted foot and ankle. The augmented stress images undergo 3D reconstruction and post-processing to render coronal and sagittal images. These are subsequently compared to standard, conventional weightbearing CT images performed without the external rotation stress.
Results
We illustrate this technique by presenting a case in which a 21-year-old collegiate athlete sustained a Grade II syndesmotic injury, diagnosed by MRI and clinical exam without evidence of instability by standard weightbearing CT or weightbearing radiographs. After undergoing the augmented stress weightbearing CT, the instability was noted. This prompted subsequent operative fixation and ultimately return to sport.
Conclusion
We propose this technique for diagnosing unrecognized, subtle dynamically unstable syndesmosis injuries where clinical suspicion persists despite negative imaging, particularly in the elite athlete.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Tibiofibular syndesmotic injuries occur in association with fractures or in isolation. In athletes, these injuries are often referred to as “high ankle sprains” and make up nearly 18% of all ankle injuries [1, 2]. Syndesmotic injuries have notoriously been difficult to diagnose and treat appropriately and are associated with a prolonged return to sport, particularly when diagnosis is missed entirely or not managed effectively [1]. The Westpoint Grading System classifies syndesmotic injuries into Grades I, II, and III with further subdivision of Grade II into IIa and IIb (Table 1) [1, 3]. Isolated syndesmotic injuries are classically treated surgically when they are deemed “unstable” (West Point Grade IIb and III) as it has been shown to shorten return to play times in high level athletes [2,3,4].
Dynamic instability of the syndesmosis in the high-level athlete is difficult to diagnose, requiring a high index of suspicion and surgical stabilization to prevent late adverse sequelae, such as recurrent ankle pain, anterolateral soft tissue impingement, local synovitis, and chronic instability of distal syndesmosis [1, 5]. The literature is clear that Grade III injuries are best treated surgically, and Grade I injuries can be treated effectively with nonoperative treatment [6]. The gray area exists in differentiating type IIa and IIb injuries (stable and unstable syndesmotic injuries, respectively) [6]. In a Level 2 prospective study, Lui et al. demonstrated intraoperative stress radiographs missed half of all unstable syndesmotic injuries identified on arthroscopy that required surgery [7]. Diagnostic arthroscopy has become the gold standard in diagnosing unstable syndesmosis injuries as one is able to capture the dynamic nature of instability that occurs in the coronal, sagittal, and rotational planes [8,9,10,11]. CT images have been shown to identify syndesmosis diastasis of 2 mm or greater and has proven superior to standard stress radiographs [8, 12]. MRI, however, is the benchmark imaging modality, with the ability to detect syndesmotic injuries with 90% sensitivity and 94.8% specificity [8, 13].
Both CT and MRI have been helpful in identifying syndesmotic injuries but are static, non-weight bearing imaging modalities that cannot demonstrate dynamic instability, which may miss the unstable nature of some injuries. In addition, there is an increasing interest across the literature in utilizing weight-bearing CT to aid in diagnosing foot and ankle pathology due to its ability to identify instability and malalignment not otherwise seen in the offloaded foot [14, 15].
We aim to present a novel imaging technique utilizing weight-bearing CT with syndesmotic stress to identify subtle, unstable syndesmotic injuries. We illustrate this with a case presentation of such an injury in an elite athlete that ultimately required operative fixation.
Materials and methods
Cone beam weight bearing computed tomography (WBCT) is a well-described imaging modality for evaluation of foot and ankle injuries. This modality not only allows for anatomic characterization of an injury or pathology; physiologic anatomy can be depicted in 3 dimensions, which is a significant advantage in many applications. Furthermore, the isotropic sampling permits anatomic multiplanar reformatted images in the plane that best depicts the syndesmosis joint. We have found it highly beneficial to teach our CT technologists about syndesmosis injuries and the importance of augmented physiologic stress applied across the ankle joint (in addition to the standard WBCT) to better demonstrate instability or motion, particularly at the tibiofibular syndesmosis.
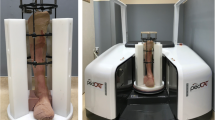
To perform an augmented stress weight bearing CT, the patient is positioned in the WBCT scanner and initial images are acquired in the standing weight bearing position with feet directed forward and weight distributed equally (Fig. 1). The handrails should only be used to steady the patient, preventing motion degraded images. A second image acquisition is then performed (augmented stress), where the patient is coached to firmly plant both feet on the ground and internally rotate the shin and knee. This places an external rotational moment on the TFS due to the planted foot and ankle (Fig. 2). It is important that the patient distributes weight as evenly as possible between the feet, so the affected side is stressed sufficiently. At the same time, the patient is instructed to limit the weight to the affected foot by their own perceived pain, offloading excess stress to the contralateral foot at the point it becomes uncomfortable. Again, the handrails are used to steady the patient to prevent image motion. The WBCT images and augmented stress images are acquired at 0.6 mm slice thickness in the axial plane and undergo 3D reconstruction and post-processing to render coronal and sagittal images, which are crucial for analysis.
Augmented stress weight bearing CT positioning. The patient is coached to internally rotate shins and knees while keeping both feet firmly planted on the ground, causing an external rotation moment at the syndesmosis. Ensure the patient is distributing weight as evenly as possible between the feet so that the affected side is stressed sufficiently. The handrails are used to steady the patient only
Results
Our case is of a 21-year-old male collegiate football player, wide receiver, that sustained an eversion injury to his left ankle during game play. He subsequently was unable to bear weight, with pain anteriorly over the distal tibiofibular joint. Pain was reproduced with dorsiflexion and eversion stress; however, he had a negative “squeeze test” on examination. Initial weight-bearing radiographs were negative (Fig. 3). Because of his equivocal examination, the patient was referred for advanced imaging. An MRI was obtained which demonstrated a syndesmotic injury; however, due to the static non weightbearing nature of this imaging modality, instability of this injury could not be determined (Fig. 4). Due to this finding, weight-bearing CT stress examination of the syndesmosis was obtained and found to have 8 mm widening of the tibiofibular syndesmosis, 4 mm increased when compared to his contralateral, uninjured ankle (Fig. 5a). This was also compared with a neutral WBCT without stress that did not illustrate the unstable nature of the injury (Fig. 5b). The coronal images also demonstrate increased uncovering of the talus underneath the tibial plafond on the weightbearing CT augmented stress (Fig. 6a) vs. the relative symmetric mortise seen on the coronal images of the non-stressed weightbearing CT scan (Fig. 6b). The significant asymmetry seen on weight bearing CT stress compared to neutral weight bearing CT emphasizes the importance of stress view imaging of the syndesmosis to diagnose subtle instability. Furthermore, three-dimensional stress images such as a CT scan evaluate rotational instability versus two-dimension stress x-rays, which is important especially with injury isolated to the AITFL in high-level athletes.
Augmented stress weightbearing (a) and neutral weightbearing (b) 0.6 mm axial cut CT images of bilateral ankles. Augmented stress weightbearing CT scan measurements taken 1 cm proximal to the ankle joint demonstrates asymmetric anterior syndesmotic widening of 4 mm greater than the contralateral uninjured ankle. This contrasts with the neutral weightbearing CT scan (b) that does not demonstrate significant widening of the syndesmosis, suggesting the importance of weightbearing stress view CT to determine subtle instability of the syndesmosis
Augmented stress weightbearing (a) and neutral weightbearing (b) coronal CT images of bilateral ankles. Augmented stress weight bearing coronal view CT scan (a) demonstrates uncoverage of the talar dome, indicative of significant instability of the syndesmosis compared to the neutral weight bearing coronal view CT scan (b)
Due to the severity of his injury as well as the inability to return to sports, the patient elected to undergo surgical fixation. Surgery included ankle arthroscopy with extensive debridement and open reduction internal fixation of syndesmosis. Diagnostic arthroscopy confirmed widening of the syndesmosis with easy access of a 3.5-mm arthroscopic syndesmosis probe in the syndesmosis (Fig. 7). An extensive arthroscopic debridement was initially performed. A tightrope button construct was used to fixate the syndesmosis. Intra-operative fluoroscopy and arthroscopy confirmed appropriate reduction of the syndesmosis (Figs. 8 and 9).
Arthroscopic view of syndesmotic injury. At the time of surgery, a diagnostic arthroscopy was performed demonstrating syndesmotic injury (a). Viewing from the medial portal, with the camera looking towards the syndesmosis, a 3.5 mm syndesmotic probe is easily placed into the syndesmosis, confirming syndesmotic injury (b)
Intraoperative arthroscopic evaluation of syndesmosis after reduction. Depicted is arthroscopic viewing from the medial portal with the camera pointing towards the syndesmosis. Probing of the syndesmosis after reduction and fixation of the syndesmosis demonstrates closure of the syndesmosis without the ability for the 3.5-mm syndesmotic probe to enter the syndesmosis
Postoperatively, the patient recovered well and underwent an expedient postoperative syndesmotic protocol. In summary, the patient was placed in a postoperative well-padded posterior splint and made non-weight-bearing to protect the healing tissue. He then was progressed from toe-touch to full weight bearing in a tall walking boot between weeks 2 and 6. Between weeks 6 and 8, he was transitioned into a regular shoe and lace-up ankle brace to work on ankle strength, range of motion, and proprioceptive exercises. Plyometric and return to sport exercises were then progressed between 3 and 4 months postoperatively. We had the patient complete a functional test before their 4-month follow-up visit, and he was cleared to return to play at that time.
Discussion
Tibiofibular syndesmotic injuries have historically been detected with standard radiographs, stress radiographs, standard CT, and MRI [5, 8, 16]. In cases where injury and stability are not obvious by these diagnostic studies, more subtle injuries may be frequently missed leading to increased morbidity, chronic instability, and increased return to play times [1,2,3,4, 17]. Chronic instability is associated with increased rates of inferior clinical results, altered joint mechanics, heterotopic ossification of the syndesmosis, and, ultimately, post-traumatic arthritis [5].
An interest in the use of weight-bearing CT in the recognition of subtle injuries of the lower extremity has been increasing. Cone-beam technology with improved designs utilizing flexible gantry movements has allowed weight-bearing CT to gain traction within the last decade [14]. The foot and ankle community has long understood the value of weight bearing imaging as the offloaded lower extremity does not appreciate dynamic instability or malalignment nearly as well as the foot and ankle that is bearing weight [15]. The addition of an augmented stress on weight-bearing CT can allow further identification of instability of the syndesmosis. Our novel imaging technique utilizing weight-bearing CT with syndesmotic stress aims at capturing the dynamic instability of Grade II syndesmotic injuries that ultimately will require surgical stabilization of the syndesmosis. This case demonstrates an instance in which a clearly disrupted AITFL, seen on MRI, was found stable to stress radiographs and standard, neutral WBCT. When given an augmented stress, the WBCT was able to clearly capture the unstable nature of the syndesmosis that was not yet realized by conventional imaging techniques.
This case study of a novel technique does have apparent limitations that warrant future investigation. Most notably, this study has a narrow indication with emphasis on diagnosing subtle injuries in elite athletes, in whom the syndesmosis will experience significant stress. The technique demonstrated in this paper does add variability in how much stress a patient may tolerate and thus, compliance with the maneuver. This will limit standardization of this technique for future study. In addition, this is an imaging technique that we illustrated with a single patient, at a single institution, with a single surgeon. Its generalizability and the clinical efficacy in capturing these injuries have yet to be determined.
We propose this technique for diagnosing otherwise unrecognized, subtle dynamically unstable syndesmosis injuries where clinical suspicion persists despite negative imaging, particularly in the elite athlete.
References
Calder JD, Bamford R, Petrie A, McCollum GA. Stable versus unstable grade II high ankle sprains: a prospective study predicting the need for surgical stabilization and time to return to sports. Arthroscopy. 2016;32(4):634–42.
Wake J, Martin KD. Syndesmosis injury from diagnosis to repair: physical examination, diagnosis, and arthroscopic-assisted reduction. J Am Acad Orthop Surg. 2020;28(13):517–27.
Gerber JP, Williams GN, Scoville CR, Arciero RA, Taylor DC. Persistent disability associated with ankle sprains: a prospective examination of an athletic population. Foot Ankle Int. 1998;19(10):653–60.
D’Hooghe P, Grassi A, Alkhelaifi K, Calder J, Baltes TPA, Zaffagnini S, et al. Return to play after surgery for isolated unstable syndesmotic ankle injuries (West Point grade IIB and III) in 110 male professional football players: a retrospective cohort study. Br J Sports Med. 2020;54(19):1168–73.
Rammelt S, Zwipp H, Grass R. Injuries to the distal tibiofibular syndesmosis: an evidence-based approach to acute and chronic lesions. Foot Ankle Clin. 2008; 13(4):611–633, vii-viii
McCollum GA, van den Bekerom MP, Kerkhoffs GM, Calder JD, van Dijk CN. Syndesmosis and deltoid ligament injuries in the athlete. Knee Surg Sports Traumatol Arthrosc. 2013;21(6):1328–37.
Lui TH, Ip K, Chow HT. Comparison of radiologic and arthroscopic diagnoses of distal tibiofibular syndesmosis disruption in acute ankle fracture. Arthroscopy. 2005;21(11):1370.
Kellett JJ, Lovell GA, Eriksen DA, Sampson MJ. Diagnostic imaging of ankle syndesmosis injuries: a general review. J Med Imaging Radiat Oncol. 2018;62(2):159–68.
Oae K, Takao M, Naito K, Uchio Y, Kono T, Ishida J, et al. Injury of the tibiofibular syndesmosis: value of MR imaging for diagnosis. Radiology. 2003;227(1):155–61.
Takao M, Ochi M, Naito K, Iwata A, Kawasaki K, Tobita M, et al. Arthroscopic diagnosis of tibiofibular syndesmosis disruption. Arthroscopy. 2001;17(8):836–43.
Takao M, Ochi M, Oae K, Naito K, Uchio Y. Diagnosis of a tear of the tibiofibular syndesmosis. The role of arthroscopy of the ankle. J Bone Joint Surg Br. 2003;85(3):324–9.
Ahn TK, Choi SM, Kim JY, Lee WC. Isolated syndesmosis diastasis: computed tomography scan assessment with arthroscopic correlation. Arthroscopy. 2017;33(4):828–34.
Chang AL, Mandell JC. Syndesmotic ligaments of the ankle: anatomy, multimodality imaging, and patterns of injury. Curr Probl Diagn Radiol. 2020;49(6):452–9.
Barg A, Bailey T, Richter M, de Cesar NC, Lintz F, Burssens A, et al. Weightbearing computed tomography of the foot and ankle: emerging technology topical review. Foot Ankle Int. 2018;39(3):376–86.
Richter M, Seidl B, Zech S, Hahn S. PedCAT for 3D-imaging in standing position allows for more accurate bone position (angle) measurement than radiographs or CT. Foot Ankle Surg. 2014;20(3):201–7.
LaMothe JM, Baxter JR, Karnovsky SC, Murphy CI, Gilbert S, Drakos MC. Syndesmotic injury assessment with lateral imaging during stress testing in a cadaveric model. Foot Ankle Int. 2018;39(4):479–84.
Haller JM, Githens M, Rothberg D, Higgins T, Barei D, Nork S. Syndesmosis and syndesmotic equivalent injuries in tibial plafond fractures. J Orthop Trauma. 2019;33(3):e74–8.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Megan R. Wolf
Arthrex: Direct payment for travel and/or courses
Stryker: Direct payment for travel and/or courses
Zimmer Biomet: Direct payment for travel and/or courses
Paragon28: Direct payment for travel and/or courses
Artelon: Direct payment for travel and/or courses
Bryan G. Vopat MD
Altior: Stock or stock Options
American Orthopaedic Foot and Ankle Society: Board or committee member
Artelon: Paid consultant
Carbon 22: Stock or stock Options
Spinal Simplicity: Stock or stock Options
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Campbell, T., Mok, A., Wolf, M.R. et al. Augmented stress weightbearing CT for evaluation of subtle tibiofibular syndesmotic injuries in the elite athlete. Skeletal Radiol 52, 1221–1227 (2023). https://doi.org/10.1007/s00256-022-04229-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00256-022-04229-9