Abstract
Objective
The tibia externally rotates to the femur during the last 20° of the knee extension motion. This kinematic phenomenon is well known as screw home movement (SHM). The purpose was to clarify the SHM in anterior cruciate ligament deficient (ACLD) knee using four-dimensional computed tomography (4DCT).
Materials and methods
Six patients with a unilateral isolated ACLD knee participated. In the static position, CT scan of the both limbs of the femur and tibia were performed. Then, 4DCT was performed around knee. In the CT gantry, subjects were positioned in supine position with 45° of knee flexion on a triangle pillow and were asked to extend the knee to full extension within 10 s on each limb. The CT data were accumulated in digital imaging and communication in medicine (DICOM) data format. From the static CT and 4DCT DICOM data, three-dimensional surfaces of the knee joint were reconstructed. The whole tibia surface was matched into the partial tibia surface of that frame using 3D-3D registration technique. After the assessment of coordination system of the whole leg, knee flexion, abduction, and external rotation angle were calculated.
Results
Knee external rotation angle was significantly smaller on the ACLD side than on the contralateral unaffected side in 0–15° of knee flexion (P < 0.05 in 0, 5, 10, and 15 degrees), while the angle was similar during 15–60° of knee flexion.
Conclusion
The absence of SHM in ACLD knee was detected using 3D-3D registration technique based on 4DCT.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The tibia externally rotates with respect to the femur about 15° during the last 20° of the knee extension [1,2,3,4,5]. This kinematic phenomenon is well known as screw home movement (SHM). SHM plays an important role to lock the knee in extension and limit anterolateral rotational movement. SHM occurs based on the unique anatomical shape at the knee joint. For instance, medial articular surface is longer than lateral articular surface, and thus, prolonged anterior glide on the medial side produces external rotation of the tibia. In addition, it has been suggested that anterior cruciate ligament (ACL) possibly contributes to SHM and ACL deficiency can result in anterolateral instability. Several studies had been done to assess SHM with or without ACL. Barrance et al. assessed knee rotation directly on 16 ACL-deficiency knees and normal patients based on cine magnetic resonance imaging (MRI) [6]. They indicated the presence of a screw home movement in normal subjects, whereas their study failed to detect impairment of SHM in patients with ACL deficiency as this movement might be too small to be detected. On the other hand, Ng AW et al. suggested that 15 of 19 patients (80%) with an intact ACL had a demonstrable normal screw home movement, while 24 of 47 patients (51%) with an ACL tear had absence of the screw home movement based on differences of medial and lateral femoral condyle positions on tibial surface using MRI [7]. They concluded that there was demonstrable absence of the normal SHM with anterior tibial translation related to presence of clinical instability. Although computed tomography (CT) has greater advantage concerning evaluation of bone morphology, little attention has been paid to the difference between ACL deficient (ACLD) and intact (ACLI) knees in SHM using CT.
The purpose of the present study was to investigate and clarify SHM in ACLD during dynamic knee motion using four-dimensional computed tomography (4DCT). It was hypothesized that ACLD knee had a different kinematic pattern in SHM, compared to ACLI knee.
Materials and methods
Subjects
Six patients with a primary unilateral isolated ACLD knee (1 male and 5 females; mean age, 28.3 ± 12 years; age range, 17–49 years; mean body mass index, 20.4 ± 0.8 kg/m2) participated in the present study. ACL tear was diagnosed by senior orthopedic surgeons (K.H., S.K., and Y.N.) using physical examination and MRI findings in each patient. All the patients were scheduled for arthroscopic ACL reconstruction. They had no history of other serious lower limb injuries, including posterior cruciate injury, medial or lateral collateral ligament injury, and symptomatic radiographic evidence of osteoarthritis in the affected limb. In addition, there was no history of injury or surgery in the contralateral knees. All subjects provided a written informed consent, which was approved by our institutional review board.
Data acquisition
All subjects were scanned by static CT and 4DCT on both limbs. In the static position, CT scan was performed for whole femur and tibia. Thereafter, 4DCT was performed using a 320-detector CT scanner (Aquilion ONE, Canon Medical Systems, Otawara, Japan). The CT scan speed was 0.275 s and all images are reconstructed using half reconstruction, so that the temporal resolution is approximately 0.16 s. Scanning parameters were as follows: peak tube voltage = 100 kVp; tube current = 40 mA; scan coverage = 160 mm; matrix size = 512 × 512 pixels; and reconstruction section thickness and section interval = 0.5 mm. In the CT gantry, subjects were positioned in supine position with 45° of knee flexion on a triangle pillow and were asked to extend the knee to full extension within 10 s on each limb (Fig. 1). Fifty-one frames of CT volumetric data were obtained for 10 s. The CT data were accumulated in digital imaging and communication in medicine (DICOM) data format.
The effective radiation dose of our 4DCT protocol was 0.075 mSv, which was determined by the dose length product measurement (187.5 mGy.cm) and calculated using the normalized coefficients (0.0004) reported in the literature [8]. A total of 0.075 mSv was lower than 0.16 mSv which was the effective radiation dose of a standard knee CT scan [9].
Evaluation based on 3D-3D registration technique
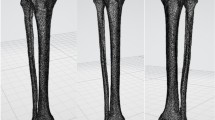
From the static CT DICOM data, three-dimensional surface data of the whole femur and tibia were reconstructed using three-dimensional visualization software (Aviso 6.4; Thermo Fisher Scientific, Tokyo, Japan). From 4DCT DICOM data, surface of the partial femur and tibia of all frames were also reconstructed. The partial femur surface of the knee joint surface in 4DCT was matched into the whole femur data in static CT by surface matching technique using iterative closet point (ICP) algorithm, from the Visualization Toolkit 8.1.0 (Kitware Inc., Clifton Park, NY, USA). Then, the whole tibia surface was matched into the matched partial tibia surface of that frame using 3D-3D registration technique reported by Oki et al. [8] (Fig. 2).
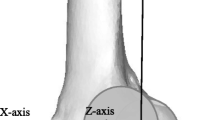
We used the coordinate systems of the femur using the method defined by Sato et al. [9] and the tibia using the method defined by Kaneda et al. [10] (Fig. 3). The angle rotated around the X-axis was defined as adduction-abduction, around Y-axis as internal–external rotation, and around the Z-axis as flexion–extension, respectively. In each frame, flexion, abduction, and external rotation angles were calculated using Euler/Cardan angles (in z-x–y order) according to the previous study [11].
Statistical analysis
As a statistical analysis, Wilcoxon signed rank-test was used to compare the differences between ACLD and ACLI. Values of p < 0.05 were considered significant. All the statistical analyses were done with the use of SPSS® Version 24 for Microsoft Windows (Chicago, IL). The sample size for the current investigation was determined to be 6 subjects in each group with 80% power (GraphPad Statmate 2, San Diego, CA). This calculation was performed using the tibial rotation angle, with defined significant differences of 3.0° between ACLD and ACLI knees.
Results
In terms of the knee abduction angle, no significant difference was found between ACLD and ACLI during 45° of knee flexion to full extension (Fig. 4). Gradually, knee abduction seemed to become large as active knee extension was done. This tendency was similar between ACLD and ACLI.
On the other hand, tibial external rotation angle was significantly different between ACLD and ACLI sides during 15° of knee flexion to full extension, while the angle was similar during 45–15° of knee flexion (Fig. 5). Specifically, tibial external rotation angle was significantly smaller on ACLD side than on ACLI side at 15° of knee flexion (− 2.03° ± 3.77 vs − 0.65° ± 2.52), at 10° of knee flexion (− 1.62° ± 2.29 vs 0.67° ± 1.47), at 5° of knee flexion (− 1.39° ± 1.97 vs 1.58° ± 0.36), and full extension (0.19° ± 0.70 vs 5.10° ± 0.8) (Table 1). In the representative case, SHM was smaller on ACLD side than on ACLI side during 15° of knee flexion to full extension (Fig. 6a, b). SHM in ACLD knee was not observed based on 4DCT data, compared to ACLI knee, as sagittal and frontal movements were similar between ACLD and ACLI knees.
(a) In this representative case, the right limb was the ACLD knee and the left limb was the ACLI knee. The tibia was shown in the view from the z-x plane. ACLI was inverted around the Z-axis and matched with ACLD. The angle was rotated around the Y-axis which was defined as internal–external rotation. b External rotation was smaller on ACLD than on ACLI during 15–0° of knee flexion in a real picture of this representative case
Discussion
The results of the present study supported the hypothesis that ACLD knee had a different kinematic pattern in SHM, compared to ACLI knee. The most important finding was that SHM in ACLD knee was not seen using 4DCT, compared to ACLI knee.
The classic SHM described by some researchers was observed based on model predictions [12, 13]. So far, various amount of SHM angles had been reported with a range of 10–36°. For example, Shoemaker et al. reported that the tibia rotated externally 10° using a simulation device [12] and Ishii et al. demonstrated that the tibia rotated externally 10.6° using intracortical pin fixation [3]. On the other hand, Wilson et al. reported that maximum SHM was 36° [13]. The initial knee flexion angle ranged from 90 to 55° of flexion, and thus reported SHM seemed to be wide range. Based on a previous study, 81% of rotational movement occurred during knee flexion from 0 to 30° [14]. Karrholm et al. report that the rotational movement of the tibia ranges from 1.6° (external rotation) to 9.0° (internal rotation) during the last 30° of knee extension in the healthy knee joint [15]. In addition, Zhang et al. demonstrated that tibial internal rotation occurred with knee flexion, and the average angle was 9.9 ± 1.9° [16]. Average of SHM in the present study was 6.1° for ACLI and 2.2° for ACLD as initial flexion angle started from 30° of knee flexion. As previous studies indicated that screw-home motion could be a characteristic of healthy knee motion, and its absence would reflect knee instability or joint disease [17,18,19]. Thus, smaller SHM for ACLD in the current investigation should be pathological phenomenon.
According to previous studies, abnormal kinematics was observed in ACLD under static condition as well as dynamic knee motion. Ng AW et al. demonstrated that absence of the normal SHM was detected in ACLD knees using MRI [7]. In addition, Murayama et al. assessed in vivo three-dimensional dynamic motion of ACLD knees during squatting from full knee extension to full flexion using 2D-3D registration technique, and concluded that SHM was impaired in ACLD knees [20]. However, these studies evaluated tibiofemoral motion in the medial and lateral compartments separately, and did not assess SHM directly. Although several researches were done to assess SHM, there has been no reports concerning 3D-3D registration technique using 4DCT. Therefore, the present study is the first to evaluate kinematics of SHM using the whole leg during active extension. Oki S et al. reported that 3D-3D registration technique depended on the accuracy of image registration from the partial segments onto the whole bones that was performed for the entire set of lengths of the femur and tibia; the errors were tolerable for femur lengths longer than 9% of the whole length and tibia lengths longer than 7% of the whole length. At the 10% of the length of the femur and 8% of the length of the tibia, errors were 0.02° for varus/valgus rotation, 0.02° for internal/external rotation, and 0.01° for extension/flexion rotation [8, 10].
Limitations
Several limitations should be noted in the present study. First, the current investigation limited to patients with ACL injury and contralateral knees in those patients were used as controls. Therefore, kinematics in healthy people was unknown. Second, the present study did not describe the bone morphology of the femur and tibia, which might affect the kinematics. Third, there was a small number of patients, even if enough power was obtained using statistical software. Lastly, muscle strength was not assessed for each patient, and thus, it was possible that quadriceps muscle strength during knee extension would affect knee kinematics. Nonetheless, 4DCT with 3D-3D registration technique is useful to evaluate SHM in patients with ACLD knee when considering the kinematic difference between ACLD and ACLI knees.
Conclusion
From the present study, SHM was different between ACLD and ACLI during 15° of knee flexion to full extension. The absence of SHM in ACLD knee was detected using 3D-3D registration technique based on 4DCT.
References
Goodfellow J, O’Connor J. The mechanics of the knee and prosthesis design. The Journal of bone and joint surgery British volume. 1978; 60-b(3):358–69.
Bytyqi D, Shabani B, Lustig S, Cheze L, Karahoda Gjurgjeala N, Neyret P. Gait knee kinematic alterations in medial osteoarthritis: three dimensional assessment. Int Orthop. 2014;38(6):1191–8.
Ishii Y, Terajima K, Terashima S, Koga Y. Three-dimensional kinematics of the human knee with intracortical pin fixation. Clin Orthop Relat Res. 1997;343:144–50.
Wretenberg P, Ramsey DK, Németh G. Tibiofemoral contact points relative to flexion angle measured with MRI. Clin Biomech (Bristol, Avon). 2002;17(6):477–85.
Asano T, Akagi M, Tanaka K, Tamura J, Nakamura T. In vivo three-dimensional knee kinematics using a biplanar image-matching technique. Clin Orthop Relat Res. 2001;388:157–66.
Barrance PJ, Williams GN, Snyder-Mackler L, Buchanan TS. Altered knee kinematics in ACL-deficient non-copers: a comparison using dynamic MRI. Journal of orthopaedic research: official publication of the Orthopaedic Research Society. 2006;24(2):132–40.
Ng AW, Griffith JF, Hung EH, Law KY, Ho EP, Yung PS. Can MRI predict the clinical instability and loss of the screw home phenomenon following ACL tear? Clin Imaging. 2013;37(1):116–23.
Oki S, Kaneda K, Yamada Y, Yamada M, et al. Four-dimensional CT analysis using sequential 3D-3D registration. Journal of visualized experiments. J Vis Exp. 2019(153).
Sato T, Koga Y, Sobue T, Omori G, Tanabe Y, Sakamoto M. Quantitative 3-dimensional analysis of preoperative and postoperative joint lines in total knee arthroplasty: a new concept for evaluation of component alignment. J Arthroplasty. 2007;22(4):560–8.
Kaneda K, Harato K, Oki S, Ota T, Yamada Y, Yamada M, et al. Three-dimensional kinematic change of hindfoot during full weightbearing in standing: an analysis using upright computed tomography and 3D–3D surface registration. J Orthop Surg Res. 2019;14(1):355.
Ishii K, Oki S, Iwamoto T, Jinzaki M, Nagura T, Matsumoto M, et al. Quantitative analysis of metacarpophalangeal joints during active flexion using four-dimensional computed tomography. Clinical biomechanics Bristol Avon. 2020;80:105188.
Shoemaker SC, Adams D, Daniel DM, Woo SL. Quadriceps/anterior cruciate graft interaction. An in vitro study of joint kinematics and anterior cruciate ligament graft tension. Clinical orthopaedics and related research. 1993(294):379–90.
Wilson DR, Feikes JD, Zavatsky AB, O’Connor JJ. The components of passive knee movement are coupled to flexion angle. J Biomech. 2000;33(4):465–73.
Coughlin KM, Incavo SJ, Churchill DL, Beynnon BD. Tibial axis and patellar position relative to the femoral epicondylar axis during squatting. J Arthroplasty. 2003;18(8):1048–55.
Karrholm J, Brandsson S, Freeman MA. Tibiofemoral movement changes of axial tibial rotation caused by forced rotation at the weight-bearing knee studied by RSA. J Bone Joint Surg Br. 2000;82(8):1201–3.
Zhang LK, Wang XM, Niu YZ, Liu HX, Wang F. Relationship between patellar tracking and the “screw-home” mechanism of tibiofemoral joint. Orthop Surg. 2016;8(4):490–5.
Kim HY, Kim KJ, Yang DS, Jeung SW, Choi HG, Choy WS. Screw-home movement of the tibiofemoral joint during normal gait: three-dimensional analysis. Clin Orthop Surg. 2015;7(3):303–9.
Hallén LG, Lindahl O. The, “screw-home” movement in the knee-joint. Acta Orthop Scand. 1966;37(1):97–106.
Sanfridsson J, Arnbjörnsson A, Fridén T, Ryd L, Svahn G, Jonsson K. Femorotibial rotation and the Q-angle related to the dislocating patella. Acta Radiol. 2001;42(2):218–24.
Murayama T, Sato T, Watanabe S, Kobayashi K, Tanifuji O, Mochizuki T, et al. Three-dimensional in vivo dynamic motion analysis of anterior cruciate ligament-deficient knees during squatting using geometric center axis of the femur. Journal of orthopaedic science : official journal of the Japanese Orthopaedic Association. 2016;21(2):159–65.
Acknowledgements
The authors would like to thank Prof. Morio Matsumoto, MD, PhD and Shu Kobayashi, MD, PhD from Department of Orthopedic Surgery, Keio University School of Medicine for clinical advice. Further support was provided by Sumi Yamashita and Hiroko Arai of Department of Clinical Biomechanics, Keio University School of Medicine.
Author information
Authors and Affiliations
Contributions
Yutaro Morishige contributed to the acquisition and analysis of data and to the writing of the manuscript. Kengo Harato contributed to the conception and design of the work, to the analysis of the results, and to the writing of the manuscript revision. Satoshi Oki contributed to the programing of 3D-3D surface registration. Kazuya Kaneda contributed to the analysis of data. Yasuo Niki contributed to the interpretation of the results. Masaya Nakamura contributed to the organization of the work and research member. Takeo Nagura contributed to the interpretation of data and to the final version of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Morishige, Y., Harato, K., Oki, S. et al. Four-dimensional computed tomographic analysis of screw home movement in patients with anterior cruciate ligament deficient knee — a 3D-3D registration technique. Skeletal Radiol 51, 1679–1685 (2022). https://doi.org/10.1007/s00256-021-03986-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00256-021-03986-3