Abstract
Dual-energy virtual noncalcium images are increasingly used to identify marrow edema which accompanies bony pelvic injuries and marrow pathology obscured by cancellous bone. We present a clinical perspective of our experience using virtual noncalcium images in the work up of pelvic osseous pathology.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The incidence of falls resulting in hip fractures rises with advancing age, and delayed diagnosis and treatment of hip fractures can lead to significant mortality [1,2,3]. For instance, untreated cervical hip fractures carry the risk of future displacement. In the emergency setting, radiographs are routinely obtained when a hip fracture is suspected; however, 3.1–4.4% of hip fractures are not identified on initial radiographs [4, 5].
Conventional single-energy CT has a higher sensitivity for hip fractures than radiographs, and is readily available in most emergency departments. In the elderly presenting with a history of trauma, the evaluation should always include both bone and soft-tissue windowing as the marrow edema associated with acute fractures is detectable when viewed with soft-tissue imaging kernels. Additionally, a comparison of the symptomatic and asymptomatic side can help confirm the presence of marrow edema. Several authors have reported on the bone bruise as an ancillary CT finding to aid detection of nondisplaced fractures [5,6,7]. For instance, in a retrospective review of normal or equivocal radiographs, Geijer et al. identified a bone bruise and lipohemarthrosis on conventional (single energy CT) in 113 of 115 patients with a cortical fracture [5]. Henes et al. report good validity and reliability (r = 0.989) with a quantitative Hounsfield unit (HU) cutoff value for a bone bruise (35.7 HU) and moderate agreement with qualitative assessment when evaluating occult sacral insufficiency fractures [6].
With conventional CT, however, identification of bone marrow edema associated with occult fractures is limited by cancellous bone [8]. MRI is the gold standard for diagnosing hip fractures because it is exquisitely sensitive for the associated edema [9]; however, MRI is time intensive, not available 24/7 in most facilities, and contraindicated in certain patient populations. Dual-energy CT exploits the photon energy-dependent attenuation of different material acquired with two x-ray spectra (100 and 140kVP with tin filter), to differentiate and quantify material composition [10]. Using post processing software calcium signal can be removed from the images displaying cancellous bone to enable the easy identification of edema in the bone marrow [11]. These images are called virtual noncalcium images.
In this review, we describe the spectrum of pathology identified during the evaluation of hip pain with dual-energy CT virtual noncalcium images—findings which were otherwise subtle or occult on radiographs or conventional single-energy CT. We also discuss other applications of dual-energy CT with virtual noncalcium reconstruction in the pelvis.
Dual-energy CT virtual noncalcium image acquisition and reconstruction
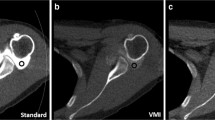
In our clinical practice, virtual noncalcium imaging is part of the routine workflow when a pelvis CT is requested to evaluate for hip fractures in the emergency department. We utilize a dual-source CT scanner (Somatom Definition Flash, Siemens Healthcare, Forchheim, Germany), with tube voltages set at 100/140 kV using a tin filter, quality reference tube-current-time-product values of 300 and 232 mAs, respectively, for the low and high x-ray tube energies, detector collimation of 32 × 0.6 mm, and a pitch of 0.6. This technique matches our single-energy pelvic CT for radiation exposure. Virtual noncalcium images are then reconstructed using commercially available dual-energy analysis software, and presented to the radiologist alongside conventional multiplanar thin section images reconstructed with a sharp kernel to display bones.
Limitations of this technique include large patient body habitus, which can cause beam hardening of images obtained using the low energy x-ray tube. This beam hardening may potentially limit the quality of the source and virtual noncalcium images [12]. Additionally, normal red marrow and red marrow reconversion have higher CT attenuation on virtual noncalcium images and can confound findings of true bone marrow edema. Automated reconstruction of virtual noncalcium post processed images is now available, eliminating the need for time-consuming post-processing by the technologist or radiologist on a thin-client workstation [13], with images automatically exported to PACS for image evaluation.
Dual-energy CT sensitivity and specificity
Dual-energy CT with virtual noncalcium reconstruction is highly sensitive and specific in identifying traumatic marrow edema using MRI as the gold standard [8, 14, 15]. In an evaluation of 14 patients with 36 sites of MRI-confirmed bone bruises in the knee, dual-energy CT with virtual noncalcium reconstruction was shown to detect bone bruises for at least 10 weeks following trauma [14]. A study prospectively evaluating the diagnostic performance of virtual noncalcium images in traumatic ankle injuries demonstrated a sensitivity of 90% and specificity of approximately 80% for identifying unique sites of bone edema [15]. For nondisplaced hip fractures, the sensitivity and specificity of dual-energy CT with virtual noncalcium images is estimated to range between 77–91% and 92–99%, respectively [16]. And finally, a meta-analysis, including 450 patients and 1,901 lesions in the ankle, hip, knee and spine, dual-energy CT was shown to have a pooled sensitivity and specificity of 85 and 97%, respectively [17].
Pathology identified by dual-energy CT virtual noncalcium imaging
Nondisplaced or minimally displaced pelvic fractures
When the clinical examination does not produce the expected symptoms, and radiographs are negative, occult fractures may be falsely excluded and treatment not implemented in a timely fashion. Bone marrow edema associated with acute fractures is readily apparent on virtual noncalcium images (Figs. 1, 2, 3, 4, and 5). The anatomic distribution of bone marrow edema identifies the site of bony injury and can have important management implications, e.g., edema associated with an occult nondisplaced intertrochanteric fracture will extend from the medial cortex to the lateral cortex and suggest an unstable fracture pattern that would benefit from surgical management (Figs. 2 and 3) [18].
91-year-old female with a nondisplaced right greater trochanteric fracture without extension to the intertrochanteric region or medial cortex, occult on radiographs. The fracture is not visible on conventional single energy CT bone windows (a); however, edema (red arrows) is noted in the right greater trochanter with normal fatty marrow seen in the left greater trochanter (white arrow) on soft tissue windows of the conventional CT (b) and on the virtual noncalcium image (c), indicating a nondisplaced fracture. Marrow edema is very nicely shown on the 3D surface rendered coronal image (d) as green color (red arrow). The fracture does not extend to the medial cortex and so surgery was not performed. Due to increase in pain, an MRI was obtained several days later which confirmed the greater trochanteric fracture. Axial T1-weighted MRI (e) and T2-weighted MRI with fat saturation (f) of the right proximal femur demonstrate the fracture with associated marrow edema (white arrows)
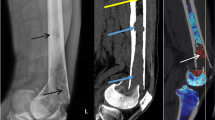
54-year-old male with a left proximal intertrochanteric fracture. This is occult on the radiograph of the left hip (not shown). The fracture is seen as a subtle cortical step at the greater trochanter (white arrow) on the coronal conventional single-energy CT image with subtle high attenuation seen in the intertrochanteric region consistent with bone marrow edema (red arrows) (a). The associated marrow edema is more apparent on the dual-energy virtual noncalcium image (b), and extends from the medial cortex to the lateral cortex, an indication for surgical management. The patient subsequently underwent pinning of the intertrochanteric fracture based on the dual-energy CT images alone without need for MRI
79-year-old female with acute, nondisplaced mid-cervical left femoral fracture. The fracture is very subtle on the coronal conventional CT (a) (white arrow); however, there is bone marrow edema (red arrows) in the subcapital region particularly on soft tissue windows (not shown) which give a higher diagnostic confidence for fracture if compared to the asyptomatic hip. Coronal virtual noncalcium image (b) well demonstrates edema within the left femoral neck (red arrows)
75-year-old female with acute nondisplaced fractures of the bilateral superior and left inferior pubic rami, and a radiographically occult incomplete left subcapital femoral fracture. The pelvic fractures are occult on the radiograph of the pelvis (not shown). No fracture is seen in the left femoral neck on bone windows (not shown), while the marrow edema in the subcapital region (red arrows) is difficult to differentiate from the normal red marrow in the intertrochanteric region (a, white arrow). The left superior pubic rami fractures are apparent on the conventional single-energy CT image (b, white arrows). Bone marrow edema associated with the pelvic fractures can be seen in the 3D surface color rendered image of the virtual noncalcium image (c, red arrows). Artifact with green coloration obscures visualization of the sacrum. Bone marrow edema is associated with an acute, nondisplaced incomplete left proximal femur subcapital fracture (yellow arrow). The patient proceeded to have the left hip pinned based on the dual-energy CT imaging without requiring MRI
Acute and chronic slipped femoral capital epiphyses. A 13-year-old boy presents to the ER with 21-week history of left hip pain and denied any right hip pain. Coronal conventional single energy CT (a) demonstrates bilateral slipped femoral capital epiphyses (white arrows). 2D color rendering of the virtual noncalcium coronal image (b) demonstrates edema in the left femoral neck (red arrows), indicating acute on chronic slipped capital femoral epiphysis. No edema in the right femoral neck indicates chronic changes only. The patient went on to have both hips pinned
When compared to MRI as the gold standard for the detection of hip fractures, virtual noncalcium imaging has a sensitivity of up to 90% and a positive predictive value of up to 86% [19]. In a retrospective study of 118 patients with symptoms suspicious for a nondisplaced hip fracture, Kellock et al. report the sensitivity for detecting hip fractures using virtual noncalcium imaging with concurrent bone reconstructions as 95–100% [16]. This represents an incremental 4–5% increase in sensitivity (for two out of three readers) over the sole use of bone reconstruction to detect these fractures. The specificity of virtual noncalcium images, with MRI as the reference standard, is however variable, ranging between 40%—in an early study of 25 patients which may be due to low numbers in the study [19]— and 99–100% when used in conjunction with CT bone reconstruction [16].
The median diagnostic confidence for detecting a nondisplaced hip fracture in the study by Kellock et al. was high (10 out of 10) using bone reconstructed images solely or in conjunction with virtual noncalcium images. However, to clinically exclude a nondisplaced hip fracture, diagnostic confidence was significantly increased when bone reconstructed images and virtual noncalcium images were used concurrently in comparison with the sole use of bone reconstructions [16]. Interpreting virtual noncalcium images alongside CT bone reconstructions can decrease the rate of interpretive error.
Intramedullary neoplastic disease and associated complications
Osseous metastatic diseases are often silent or missed at imaging interpretation until they present with pain and pathologic fractures. Purely lytic or tiny sclerotic bone lesions may pose diagnostic dilemmas on single-energy CT due to lack of perception of an abnormality. The associated bone marrow edema or marrow replacement and infiltration are often identifiable on virtual noncalcium images. Bone marrow edema associated with metastatic lesions can appear mass-like with a clear demarcation between edema and normal marrow (Figs. 6 and 7).
Metastatic lesions in a 63-year-old female presenting with left hip pain. Coronal single-energy CT (a and c) and dual-energy CT (b and d) of the pelvis demonstrating multiple osseous metastatic lesions in the right ilium and left femoral neck (red arrows) in a patient with metastatic lung adenocarcinoma. Lesions are more conspicuous on the virtual noncalcium images compared to the conventional single-energy CT
60-year-old female with a history of renal cell carcinoma with a pathologic intertrochanteric fracture of the proximal left femur. Coronal CT (a) of the pelvis demonstrates the intertrochanteric fracture (white arrow), without obvious underlying mass. Coronal dual-energy CT virtual noncalcium image (b) and 3D surface color rendered virtual noncalcium image (c) reveals marrow replacement with sharply defined margins consistent with a mass, adjacent to the greater trochanter and in the femoral neck (red arrows), representing the biopsy-proven metastatic lesion
Several recent studies have reported on the potential of dual-energy CT in the detection and work up of bone neoplasms [20,21,22,23,24,25]. For instance, dual-energy CT is helpful in guiding the interventionalist during CT-guided biopsy of suspicious lesions identified on MRI, bone scans, or Positron Emission Tomography/CT, as these are poorly displayed on single-energy CT (Fig. 8). Burke et al. present four cases in which dual-energy CT was used to biopsy malignant pelvic neoplasms which were radiographically occult on single-energy CT [25]. Kosmala et al. found that the performance of dual-energy CT was comparable to MR imaging in the diagnosis of focal infiltrative bone marrow lesions of the spine and pelvis in patients with myeloma [21]. These studies support a growing application of dual-energy CT in the work up of osseous metastatic disease.
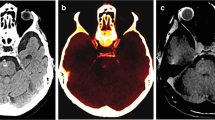
38-year-old male with treated B cell lymphoma with recurrent disease in the left iliac wing. Axial PET/CT of the pelvis demonstrates the FDG avid lesion in the left iliac wing (a, arrow) which was occult on the conventional single-energy CT (b). 2D color rendering of the dual energy CT (c) demonstrates more diffuse asymmetric marrow change within the left ilium (red arrows) with focal edema corresponding with the site of FDG avidity in the left iliac wing, which was subsequently biopsied and represented recurrent lymphoma
Ablation of pelvic osseous lesions
Pelvic metastases are often treated using cryoablation under CT guidance. During the ablation procedure, an ice ball forms within the target lesion and surrounding tissues resulting in a lowering of the tissue density and formation of low attenuation images. This phenomenon is readily identifiable in the soft tissue [26] on single-energy CT but not in bone as the CT number shift is small relative to the baseline attenuation of bone. Critical anatomic structures adjacent to the bone such as the bowel wall, nerve roots, and skin, are therefore put at risk of cryodamage. With virtual noncalcium imaging, soft-tissue attenuation from the ice ball in the bone can be identified. In a recent study at our institution [27] using human and porcine cadaveric samples, formation of ice at several treatment sites in the spine and pelvis was readily identified on dual-energy virtual noncalcium imaging, while remaining occult on mixed-kV images (a surrogate for single-energy CT; Fig. 9). The ice was identified in real-time before involving the adjacent soft tissue during the ablation procedure. If implemented clinically, virtual noncalcium imaging could potentially improve patient safety, while ensuring complete cryoablation of the target volume in the pelvis.
Human cadaveric study with multiple cryoablation probes in the right ilium demonstrating formation of ice within the marrow of the right ilium during cryoablation at 10 min, readily identified on prone axial (a, left) and coronal (b, left) dual-energy virtual noncalcium imaging (red arrows), while remaining occult on mixed-kV images (a surrogate for single-energy CT) (a and b, right)
Avascular necrosis
Avascular necrosis is another cause of bone marrow edema identifiable on dual-energy CT (Fig. 10). Patients with avascular necrosis often present with groin pain, which occurs at rest and worsens with weight-bearing. These symptoms are nonspecific and would necessitate imaging to exclude the possibility of a hip fracture. In the absence of sclerosis, subchondral fracture, or articular irregularities of the subchondral bone plate, early avascular necrosis may be missed on radiographs or single-energy CT. Bone marrow edema serves as a useful secondary sign of osseous pathology which can lead to early MRI for avascular necrosis detection. In a study evaluating patients with MRI-proven findings of avascular necrosis of the hip, the incidence of missed avascular necrosis on initial single-energy CT was 89% [28]. The diagnostic performance of dual-energy CT in identifying avascular necrosis of the hip has not been reported. This has, however, been reported for other anatomic sites. Pianta et al. report a 100% correlation with pathology-proven proximal pole scaphoid avascular necrosis (8 patients) [29]. In the acute presentation of groin pain with bone marrow edema identified on dual-energy CT, the confident diagnosis of avascular necrosis or a subtle hip fracture can be achieved with concurrent reading of the virtual noncalcium images and the conventional CT.
59-year-old female with avascular necrosis of the both femoral heads, presenting as right hip pain. Avascular necrosis was occult on the coronal single-energy CT (not shown). However, coronal dual-energy CT virtual noncalcium image (a) shows edema in both femoral heads, suspicious for avascular necrosis (red arrows). Coronal scout (b) from a right hip MRI obtained 12 days later demonstrates serpiginous low signal consistent with avascular necrosis in both femoral heads (white arrows), better seen on the dedicated right hip coronal T1-weighted image (c, white arrow)
Conclusion
In the emergency setting, dual-energy CT with virtual noncalcium reconstructed images can serve as a useful problem-solving technique when dealing with patients, particularly elderly osteopenic patients with pelvic or hip pain following trauma. The advantage of dual-energy CT with virtual noncalcium reconstruction includes its increased availability compared to MRI. Virtual noncalcium images may be helpful for assessment of areas that are indeterminate on single-energy CT or x-rays for a nondisplaced fracture. Additionally, other pathology which may present in the emergency setting as hip pain, such as avascular necrosis and metastatic disease, can be identified using this technique. The ability to exclude pathology may obviate the need for additional imaging with MRI.
References
Faulkner KA, Cauley JA, Studenski SA, Landsittel DP, Cummings SR, Ensrud KE, et al. Lifestyle predicts falls independent of physical risk factors. Osteoporos Int. 2009;20(12):2025–34.
Papadimitriou N, Tsilidis KK, Orfanos P, Benetou V, Ntzani EE, Soerjomataram I, et al. Burden of hip fracture using disability-adjusted life-years: a pooled analysis of prospective cohorts in the CHANCES consortium. Lancet Public Health. 2017;2(5):e239–e46.
Youm T, Koval KJ, Kummer FJ, Zuckerman JD. Do all hip fractures result from a fall? Am J Orthop (Belle Mead NJ). 1999;28(3):190–4.
Dominguez S, Liu P, Roberts C, Mandell M, Richman PB. Prevalence of traumatic hip and pelvic fractures in patients with suspected hip fracture and negative initial standard radiographs: a study of emergency department patients. Acad Emerg Med. 2005;12(4):366–9.
Geijer M, Dunker D, Collin D, Gothlin JH. Bone bruise, lipohemarthrosis, and joint effusion in CT of non-displaced hip fracture. Acta Radiol. 2012;53(2):197–202.
Henes FO, Groth M, Bley TA, Regier M, Nuchtern JV, Ittrich H, et al. Quantitative assessment of bone marrow attenuation values at MDCT: an objective tool for the detection of bone bruise related to occult sacral insufficiency fractures. Eur Radiol. 2012;22(10):2229–36.
Henes FO, Groth M, Kramer H, Schaefer C, Regier M, Derlin T, et al. Detection of occult vertebral fractures by quantitative assessment of bone marrow attenuation values at MDCT. Eur J Radiol. 2014;83(1):167–72.
Pache G, Krauss B, Strohm P, Saueressig U, Blanke P, Bulla S, et al. Dual-energy CT virtual noncalcium technique: detecting posttraumatic bone marrow lesions—feasibility study. Radiology. 2010;256(2):617–24.
Pandey R, McNally E, Ali A, Bulstrode C. The role of MRI in the diagnosis of occult hip fractures. Injury. 1998;29(1):61–3.
McCollough CH, Leng S, Yu L, Fletcher JG. Dual- and multi-energy CT: principles, technical approaches, and clinical applications. Radiology. 2015;276(3):637–53.
Reagan AC, Mallinson PI, O’Connell T, McLaughlin PD, Krauss B, Munk PL, et al. Dual-energy computed tomographic virtual noncalcium algorithm for detection of bone marrow edema in acute fractures: early experiences. J Comput Assist Tomogr. 2014;38(5):802–5.
Guimaraes LS, Fletcher JG, Harmsen WS, Yu L, Siddiki H, Melton Z, et al. Appropriate patient selection at abdominal dual-energy CT using 80 kV: relationship between patient size, image noise, and image quality. Radiology. 2010;257(3):732–42.
Wortman JR, Uyeda JW, Fulwadhva UP, Sodickson AD. Dual-energy CT for abdominal and pelvic trauma. Radiographics. 2018;38(2):586–602.
Ai S, Qu M, Glazebrook KN, Liu Y, Rhee PC, Leng S, et al. Use of dual-energy CT and virtual non-calcium techniques to evaluate post-traumatic bone bruises in knees in the subacute setting. Skelet Radiol. 2014;43(9):1289–95.
Guggenberger R, Gnannt R, Hodler J, Krauss B, Wanner GA, Csuka E, et al. Diagnostic performance of dual-energy CT for the detection of traumatic bone marrow lesions in the ankle: comparison with MR imaging. Radiology. 2012;264(1):164–73.
Kellock TT, Nicolaou S, Kim SSY, Al-Busaidi S, Louis LJ, O’Connell TW, et al. Detection of bone marrow edema in nondisplaced hip fractures: utility of a virtual noncalcium dual-energy CT application. Radiology. 2017;284(3):922.
Suh CH, Yun SJ, Jin W, Lee SH, Park SY, Ryu CW. Diagnostic performance of dual-energy CT for the detection of bone marrow oedema: a systematic review and meta-analysis. Eur Radiol. 2018;28(10):4182–94.
Roberts KC, Brox WT. AAOS clinical practice guideline: management of hip fractures in the elderly. J Am Acad Orthop Surg. 2015;23(2):138–40.
Reddy T, McLaughlin PD, Mallinson PI, Reagan AC, Munk PL, Nicolaou S, et al. Detection of occult, undisplaced hip fractures with a dual-energy CT algorithm targeted to detection of bone marrow edema. Emerg Radiol. 2015;22(1):25–9.
Horger M, Fritz J, Thaiss WM, Ditt H, Weisel K, Haap M, et al. Comparison of qualitative and quantitative CT and MRI parameters for monitoring of longitudinal spine involvement in patients with multiple myeloma. Skelet Radiol. 2018;47(3):351–61.
Kosmala A, Weng AM, Heidemeier A, Krauss B, Knop S, Bley TA, et al. Multiple myeloma and dual-energy CT: diagnostic accuracy of virtual noncalcium technique for detection of bone marrow infiltration of the spine and pelvis. Radiology. 2018;286(1):205–13.
Kosmala A, Weng AM, Krauss B, Knop S, Bley TA, Petritsch B. Dual-energy CT of the bone marrow in multiple myeloma: diagnostic accuracy for quantitative differentiation of infiltration patterns. Eur Radiol. 2018;28(12):5083–90.
Thomas C, Schabel C, Krauss B, Weisel K, Bongers M, Claussen CD, et al. Dual-energy CT: virtual calcium subtraction for assessment of bone marrow involvement of the spine in multiple myeloma. AJR Am J Roentgenol. 2015;204(3):W324–31.
Yuan Y, Zhang Y, Lang N, Li J, Yuan H. Differentiating malignant vertebral tumours from non-malignancies with CT spectral imaging: a preliminary study. Eur Radiol. 2015;25(10):2945–50.
Burke MC, Garg A, Youngner JM, Deshmukh SD, Omar IM. Initial experience with dual-energy computed tomography-guided bone biopsies of bone lesions that are occult on monoenergetic CT. Skelet Radiol. 2019;48(4):605–13.
Lee FT Jr, Chosy SG, Littrup PJ, Warner TF, Kuhlman JE, Mahvi DM. CT-monitored percutaneous cryoablation in a pig liver model: pilot study. Radiology. 1999;211(3):687–92.
Morris J, Michalak G, Leng S, Moynagh M, Kurup AN, McCollough CH, Fletcher JG. Dual-energy CT monitoring of cryoablation zone growth in the spinal column and bony pelvis: a laboratory study. J Vasc Interv Radiol. 2019. https://doi.org/10.1016/j.jvir.2019.01.030
Barille MF, Wu JS, McMahon CJ. Femoral head avascular necrosis: a frequently missed incidental finding on multidetector CT. Clin Radiol. 2014;69(3):280–5.
Pianta M, McCombe D, Slavin J, Hendry S, Perera W. Dual-energy contrast-enhanced CT to evaluate scaphoid osteonecrosis with surgical correlation. J Med Imaging Radiat Oncol. 2019;63(1):69–75.
Acknowledgements
Sonia Watson, PhD, assisted in editing the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Francis Baffour, M.D.: Nothing to disclose.
Katrina Glazebrook, M.B., Ch.B: Nothing to disclose.
Jonathan Morris, M.D.: Nothing to disclose.
Gregory Michalak, Ph.D.: Nothing to disclose.
Joel Fletcher, M.D.: Grant, Siemens AG and Consultant, Medtronic PLC.
Shuai Leng, Ph.D.: Nothing to disclose.
Cynthia McCollough, Ph.D.: Research Grant, Siemens AG.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Institutional IRB approval was obtained.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Baffour, F.I., Glazebrook, K.N., Morris, J.M. et al. Clinical utility of virtual noncalcium dual-energy CT in imaging of the pelvis and hip. Skeletal Radiol 48, 1833–1842 (2019). https://doi.org/10.1007/s00256-019-03243-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00256-019-03243-8