Abstract
Objective
To assess the involvement of the atlantoaxial joint in patients with early rheumatoid arthritis (ERA) and to elucidate the risk profile for the individual patient.
Materials and methods
Consecutive ERA patients (disease duration < 12 months) were included in our study. A cervical spine magnetic resonance imaging (MRI) and X-rays (cervical spine, hands, wrists, and feet) were performed in all patients. The MRI features were correlated with clinical, radiological, and biochemical variables.
Results
Fifty patients (13 men and 37 women) with a mean age of 58.2 years (range, 36–79 years) were included in the study. In 12 (24%) patients were detectable MRI findings suggestive of the craniovertebral junction involvement. Compared with patients without cervical involvement, the patients with atlantoaxial synovitis showed a significantly higher anti-citrullinated protein antibodies (ACPA) titer [mean 200.25 UI (SD 262.44) vs. mean 22.05 (SD 40.21) (p < 0.001)]; a worse Disease Activity Score 44 joints (DAS44) [mean 5.72 (SD 0.44) vs. mean 4.52 (SD 0.53) (p < 0.001)]; a worse Health Assessment Questionnaire Disability Index (HAQ-DI) [mean 1.55 (SD 0.37) vs. mean 1.09 (SD 0.33) (p < 0.001)], and a higher Simple Erosion Narrowing Score (SENS) [mean 15.83 (SD 4.52) vs. mean 7.71 (SD 3.43) (p < 0.001)]. The multivariate analysis revealed a meaningful relationship between atlantoaxial synovitis and ACPA, DAS44, and the presence of an erosive disease.
Conclusions
The craniovertebral junction is frequently involved in ERA patients. ACPA, high disease activity, and erosive disease at baseline are predictors of atlantoaxial involvement.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Rheumatoid arthritis (RA) is the most frequent chronic inflammatory joint disease affecting 0.4–1% of the population [1]. The main RA feature is the chronic synovial inflammation leading to permanent articular damage, with a consequent disability. If not adequately treated, RA can be a poor prognosis disease with a great need of health care resources [2].
Cervical spine inflammatory changes are commonly detectable in longstanding RA: this kind of involvement ranges between 25 and 88% of patients with longstanding RA [3, 4], and it is a consequence of the intense chronic synovitis that occurs in the joints, progressing to bone erosion and consequent ligamentous laxity and finally clinical and radiological instability [5]. The commonest abnormalities are disc space narrowing at C2-C3, C3-C4, C4-C5 levels in 66.1%, followed by erosions of the odontoid process (43–47%), atlantoaxial dislocation, and apophyseal joint involvement (20–24%) [3, 6].
Involvement of the atloaxial junction, which can result in atlantoaxial instability and bone erosions at the odontoid process, begins in 25% of early RA (ERA) patients, in particular in those subjects with active and erosive arthritis [4]. Clinically, cervical pain can be secondary to instability or C2 nerve root compression, but one-half of the RA patients who had cervical instability cannot have symptoms. The traditional radiology is often inadequate to reveal the morphological damage underlying these symptoms [7, 8].
Nowadays, magnetic resonance imaging (MRI) has been progressively used in the assessment of RA thanks to its ability to identify the pathologic changes of the disease. MRI has demonstrated greater sensitivity for the detection of synovitis and erosions at the craniovertebral junction than either clinical examination or conventional radiography and can provide important information on the cervical spine involvement in ERA [4, 8, 9]. A cervical MRI study should also be performed in all patients with myelopathy or radiculopathy [10].
The aims of this study were to assess the involvement of the atlantoaxial joint in patients with ERA and to elucidate the risk profile for the individual patient.
Materials and methods
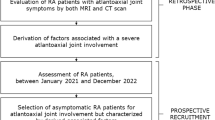
Design and study population
From April 2016 to December 2017, consecutive ERA patients were recruited from the outpatient clinic of an Italian tertiary rheumatology center.
All ERA patients were included according to the following criteria: diagnosis according the 2010 American College of Rheumatology (ACR)/ European League Against Rheumatism (EULAR) criteria for RA [11], age ≥ 18 years, disease duration less than 12 months (the disease duration was considered from the onset of the symptoms to baseline that corresponded with the point of diagnosis and with the start of treatment), and moderate/high disease activity as defined by Disease Activity Score (DAS) [12]. Patients were excluded if visual or hearing limitations were present, they did not have command of the Italian language, and/or suffered from coexisting diseases such as severe chronic obstructive pulmonary disease, heart disease, multiple sclerosis, extracorporeal dialysis, or chronic infectious disease. Patients needing biologic therapy were screened for tuberculosis prior to treatment and those at high risk for tuberculosis were allowed to enter in the study after chemoprophylaxis, as local recommendations [13].
Laboratory investigations
Baseline blood samples were obtained to evaluate the erythrocyte sedimentation rate (ESR) (normal values ≤ 15 mm/1st hour in men and ≤ 20 mm/1st hour in female) and the C-reactive protein (CRP) using standard laboratory methods. The presence of IgM-RF determined by nephelometric method (Image Beckman) and of anti–citrullinated protein antibodies (ACPA) determined by immunofluorometric assay (IFMA) (EliA CCP, ImmunoCAP 250, Phadia S.r.l., Italy). The cut-off point for the ACPA positivity was > 10 IU/ml, according to the manufacturer’s instructions, whereas a titer of IgM-RF > 40 UI/ml was considered as positive.
Clinical evaluation and data
Clinical evaluation included an assessment of disease activity by using DAS-44 joints (DAS44) [12], and a measure of physical functioning, by using the Health Assessment Questionnaire Disability Index (HAQ-DI) [14].
The DAS44 is a composite disease activity index including Ritchie Articular Index (RAI), (ranging from 0 to 78), 44 swollen joints count (SJC44), ESR and general health status (GH) (0–100 visual analogue scale [VAS]). The DAS44 is computed by the following formula: DAS = 0.53938 × √RAI + 0.0675 × (SJC44) + 0.330 ln (ESR) + 0.00722 × GH. The DAS44 can range from 0.23 to 9.87, and the values are normally distributed. High disease activity is defined by a DAS greater than 3.7, moderate disease activity between 2.4 and 3.7, low disease activity between less or equal 2.4 and greater or equal 1.6, and remission as less than 1.6. The RAI may be subjective and complicated and include a 0–3 graded evaluation of the severity of tenderness of 26 joint groups, where the highest value that counts is the highest value within each group.
The HAQ-DI assesses the degree of difficulty a person has in accomplishing tasks in eight functional areas: dressing and grooming, arising, eating, walking, hygiene, reach, grip, activities. For each item, patients are asked to rate the level of difficulty over the past week on a four-point scale, which ranges from 0 (no difficulty) to 3 (unable to perform). To calculate the disability dimension score, disability score ranges from 0 to 3, with a higher score indicating greater disability. The HAQ-DI, calculated for each of the subscales are summed, and then divided by 8. A version adapted for use among Italian patients was utilized in the present study [15].
Radiographic assessment
All the patients underwent conventional radiography of hands, wrists, and feet. The images were assessed by two experienced readers (FaS and MC), according to the Simple Erosion Narrowing Score (SENS) [16]. SENS method was derived from the Sharp’s method as modified by Sharp-van der Heijde Score (SHS) [17] and captures radiographic progression reliably compared with the more detailed SHS method [18]. As opposed to applying a semiquantitative scale of 0–4 for joint space narrowing and 0–5 for erosions, SENS simply dichotomizes whether an erosion is absent (score of 0) or present (score of 1), and whether joint space narrowing is absent (score of 0) or present (score of 1) [16]. Erosions are assessed in 32 joints of the hands and in 12 joints of the feet, joint space narrowing in 30 joints of the hands and in 12 joints of the feet, respectively. The total SENS score ranges from 0 to 86.
To estimate inter-observer and intra-observer reliability in scoring SENS, a subset of 20 randomly selected were interpreted twice by each reader at an interval of at least 2 weeks. Reliability of the readings was assessed by calculating the intraclass correlation coefficient (ICC). The inter- and intra-rater reliability estimates for SENS were excellent: inter-rater reliability 0.890 and intra-rater reliability for both readers 0.847 and 0.876. The average score for the two readers was used for the final analysis.
Cervical spine radiographs were obtained at the day of the MRI examination, in anteroposterior, transoral, and lateral and views in full flexion and extension. Images were scored by an experienced radiologist (AG) blinded to clinical data, to cervical MRI findings, as well as to foot and hand radiographs. Lateral view radiographs were used for evaluation of atlantoaxial subluxation (AAS), and transoral views were scored for the presence of odontoid process damage (erosions), and for the signs of AAS. Anterior AAS was measured by recording the shortest distance between the posterior surface of the anterior arch of the atlas and the anterior surface of the odontoid process. Vertical subluxation of the axis was diagnosed according to the Ranawat value [19].
Cervical spine MRI assessment
All the MRI examinations were performed by a radiologist (FrS), blinded to the clinical and radiographic data. MRI was carried out with a 1.5-T magnet system using a 16-channel sense neurovascular coil (Philips Medical Systems), with the patient supine and head and neck in a neutral position. The protocol included: (1) turbo spin-echo T1-weighted images on the sagittal plane, with slice thickness: 3 mm, TR: 457 ms/echo time, TE: 10 ms/echo time, echo train 5, matrix: 300 × 236, FOV: 26, Nex: 6, flip angle: 90°; (2) turbo spin T1-weighted images on coronal plane, with slice thickness: 3 mm, TR: 450 ms/echo time, TE: 9 ms/echo time; echo train 3, matrix: 192 × 153, FOV: 13, Nex: 10, flip angle 90°; (3) turbo spin-echo T1-weighted CLEAR (constant level appearance) images on axial plane, with slice thickness: 3 mm, TR: 525 ms/echo time, TE: 8 ms/echo time, echo train 3, matrix: 168 × 131, FOV: 15, Nex: 4, flip angle 90°; 4) turbo spin-echo T2-weighted images on sagittal plane, with slice thickness: 3 mm, TR: 3748 ms/echo time, TE: 120 ms/echo time, echo train 50, matrix: 264 × 175, FOV: 24, Nex 6, flip angle 90°; (5) Short Tau Inversion Recovery (STIR) images on sagittal plane, with slice thickness: 3 mm, TR: 2500 ms/echo time, TE: 60 ms/echo time, echo train 19, matrix: 232 × 171, FOV: 24, Nex: 4, flip angle: 90°; (6) turbo spin-echo T2-weighted images on axial plane, with slice thickness: 3 mm, TR: 3000 ms/echo time, TE: 120 ms/echo time, echo train: 44, matrix 248 × 176, FOV: 22, Nex: 4, flip angle: 90; (7) turbo spin-echo T2-weighted images spectral presaturation inversion recovery (SPIR) on coronal plane, with slice thickness: 3 mm, TR: 3750 ms/echo time, TE: 120 ms/echo time, echo train 17, matrix 184 × 170, FOV: 13, Nex: 6, flip angle: 90°, Nex: 6, flip angle: 90°. MR images were reviewed with particular attention to the presence of atlantoaxial and subaxial spinal levels. The atlantoaxial joint (C1-C2) was assessed for the presence of synovitis, bone marrow edema (BME), odontoid erosions, anterior, posterior or superior vertebral subluxation, and alterations of the cervicomedullary angle. BME was identified as a poorly defined area of low signal within bone on T1-weighted images that had signal intensity on STIR images. Synovitis was defined by a thickening of the synovial membrane at the atlantoaxial joint (C1-C2), showing increased water content in fat-suppressed T2-weighted and STIR sequences: the amount of pannus was classified as absent, little, moderate, or marked (four-point scale). BME was identified as a poorly defined area of low signal within bone on T1-weighted images that had signal intensity on STIR images. Erosion of the odontoid process was defined as a bone defect with sharp margins, visible in two planes. AAS was defined when the anterior atlantodental interval, measured from the posterior aspect of the anterior ring of C1 to the anterior aspect of the dens, was greater than 3 mm. Posterior AAS was defined when the anterior arch of the atlas moved over the odontoid process. Vertical subluxation at C1-C2 was defined as migration of the odontoid tip by more than 4.5 mm above the palat-occipital line or McGregor’s line [20]. The cervicomedullary angle was measured in degrees by drawing lines along the ventral side of the medulla oblongata or brainstem and the cervical cord. Normal angles range from between 135° and 175° [21].
Statistical analysis
Data were inserted into a Microsoft Excel database and analyzed using MedCalc® version 17.0 (MedCalc Software, Ostend, Belgium). Qualitative data were described as absolute frequencies and percentages. Descriptive statistics were used to describe the sample, and are given as mean values ± standard deviation and median values and interquartile range depending on the distribution (skewness) of the continuous data. The normal distribution was investigated by Kolmogorov–Smirnov test. Chi-squared and Fisher’s test were used for qualitative data and Student’s parametric t tests or Mann–Whitney non-parametric U tests were used to determine between-group differences.
The reliability of the radiographic scores was assessed using the intraclass correlation coefficient (ICC). The ICC measures the repeatability of the measures from each reader and the repeatability of the averages of the two readers’ scores. A multiple regression model was performed to determine which variables were independently associated with upper cervical spine involvement (defined by the presence of atlantoaxial joint synovitis) on MRI. Age, gender, disease duration, autoantibodies titers, RAI, SJC, GH, DAS44, HAQ-DI, and SENS were examined as potential confounders based on the significant associations with MRI findings. All statistical analyses were performed at p < 0.05.
Results
Fifty patients, 13 men (26% of the sample) and 37 women (74% of the sample) with a mean age of 58.2 years (range, 36–79 years), and with a mean disease duration of 9.7 months (range, 5–12 months), have been included in the study.
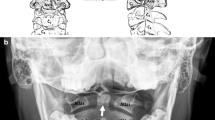
No obvious radiological lesions at the craniovertebral junction were evident on the conventional radiographs in none of the 50 patients of the sample (a representative example of a negative X-ray is provided in Fig. 1).
Anteroposterior (a), laterolateral (b), and transoral (c) X-ray images of the cervical spine of the same patient shown in Fig. 2 (magnetic resonance images). The X-ray does not demonstrate the presence of odontoid process damage (erosions) or signs of atlantoaxial subluxation
Twelve patients (24%) revealed MRI findings suggestive of the craniovertebral junction involvement. In all cases, the MRI showed pannus (synovitis) surrounding the odontoid process, with additional odontoid process erosions in eight patients, and BME at atlantoaxial joint in nine subjects (Fig. 2). The amount of pannus was divided as follows: little in six patients (50%), moderate in four patients (33.3%), and marked in two patients (16.7%). BME was usually observed involving the odontoid process (six subjects) whereas subaxially BME was limited to the vertebral plates and the interapophyseal joints (two subjects). AAS was observed in two of the 12 patients. No posterior or vertical subluxation were detected.
Turbo spin-echo T1-weighted (a), turbo spin-echo T2-weighted (b), and short tau inversion recovery (STIR) images (c) of sagittal planes. The images show bone marrow edema (double arrowhead) with erosions of the odontoid process (point arrow). Synovial pannus presence around the odontoid process (arrow), demonstrating increased water content on STIR sequence, related to inflamed synovium. The spinal cord is slightly compressed between the pannus anteriorly and the posterior arch of the atlas. Note the anterior atlantoaxial subluxation with an increase in the atlas-dens interval (more than 3 mm) (asterisk)
In one patient, the spinal cord was compressed between the pannus anteriorly and the posterior arch of the atlas. An abnormal cervico-medullary angle (< 135°) was detectable in two subjects (Fig. 3), respectively 118° and 129° (mean value of 12 patients with positive MRI findings 150.2°, range, 118-177°).
Turbo spin T1-weighted (a) and turbo spin-echo T2-weighted spectral presaturation inversion recovery (SPIR) (b) images on coronal plane, turbo spin-echo T2-weighted images on axial plane (c). The images show periodontoid synovitis, with a reduction of the joint space between the right lateral mass of C1 and the odontoid process (short arrow). Combination of rotational deformities— unilateral or asymmetric involvement of the lateral atlantoaxial joint with narrowing joint space between the lateral mass C1 and articular process C2, with increased signal intensity of the bone marrow of the vertebral bodies of C1 and C2, corresponding to bone marrow edema changes (double arrowhead). The presence of synovitis at the left atlantoaxial joint (C1-C2) can also be observed (long arrow). The axial image confirms atlantoaxial synovitis (long arrow), and reveals the thinning of the transverse ligamentous (arrowhead), especially in the central portion
Regarding the clinical symptoms complained by the 12 patients with atlantoaxial synovitis, five patients (41.7%) did not describe symptoms suggestive of cervical spine involvement, while six reported neck pain located mostly at the craniocervical junction, and one both headaches and dizziness. Other clinical manifestations could include amnestic episodes, brain stem signs, and lower cranial nerve palsies, urinary retention, and later incontinence or rectal disturbances: none of these symptoms was found in our patients.
The majority of the subjects (8/12) with craniovertebral involvement were positive for RF or ACPA, and in three a single ACPA presence was detectable.
Compared with patients without craniovertebral involvement, the 12 patients showed significantly higher ACPA titers, greater SJC, higher RAI, higher GH, higher DAS44, worse HAQ-DI, and greater SENS (Table 1). Considering the MRI findings and the demographic characteristics, there was no significant association between age, gender, or disease duration.
In the multivariate analysis (this model had an acceptable coefficient of determination, with the R2 adjusted of 0.66), the results showed that the presence of a high ACPA titer (p = 0.017), a worse DAS44 (p = 0.005), and the presence of a peripheral erosive disease (SENS) (p = 0.006), were predictors of atlantoaxial joint synovitis in MRI (Table 2). The single presence of RF was not significant for atlantoaxial involvement (p = 0.139).
Discussion
This study confirms that the atlantoaxial joint is an early target of the inflammatory process in RA. After synovitis of hands and wrists, some series describe the cervical spine involvement as the second more frequent in RA [3, 6]. The damage at the craniovertebral junction can be severe, even in subjects without neurologic signs [22].
Atlantoaxial synovitis can lead to C1-C2 instability. The hypertrophic synovial tissue results in a laxity and/or destruction of the ligamentous structures, in particular at level of the alar and transverse ligaments. The AAS is secondary to this destructive process. Considering the atlantoaxial instability, different subtypes can be differentiated. The anterior AAS is the more frequent lesion, followed by lateral AAS, which represents about 20% of cases, and posterior AAS, which concerns about 7% in association with RA [23]. Posterior AAS usually occurs in the setting of an odontoid base erosion or fracture. Posterior subluxation is associated the highest rate of neurological deficits of all forms of AAS [24].
In some cases, atlantoaxial instability can evolve in a vertical migration of the odontoid process into the cranial cavity, also known as basilar impression or invagination, or in a vertical subluxation [5, 25,26,27].
MRI is a formidable technique to evaluate soft tissues such as ligaments, joint capsules, and the retrodental synovial hypertrophy. Furthermore, MRI of the cervical spine can show the level and the degree of narrowing of the spinal canal caused by dislocation and/or the presence of extra-dural pannus tissue that can in some cases compress the spinal cord.
In the peripheral joints (fundamentally hands and feet), it is well demonstrated that the presence of BME is closely linked to the degree of synovitis and is a predictor of the radiographic erosive progression [20]. It is believed that the same process, which is well documented in the peripheral joints, also affects the atlantoaxial joint [28].
Reijnierse and coworkers observed a fivefold increased risk of neurologic dysfunction when MRI revealed atlas erosion and cranial settling, as evidenced by a decreased distance of the dens to McRae’s line [22].
In two subjects, an abnormal cervico-medullary angle (< 135°) was also found. On the sagittal MRI scan, the normal cervicomedullary angle is between 135° and 175°. Patients with a cervicomedullary angle of less than 135° had cranial settling and clinical signs of C2 root pain, neural compression, or myelopathy [21, 29, 30].
Recognizing the predictive factors of the cervical spine involvement may allow the identification of those subjects who need a more aggressive therapy and a tighter control. Our patients with atlantoaxial synovitis showed significantly higher DAS44 score than patients without craniovertebral junction involvement. Moreover, the results of our research revealed that ACPA and peripheral erosive disease are indicators of a high risk of early involvement of the atlantoaxial joint in terms of synovitis.
Various studies tried to identify prognostic factors of radiographic damage in patients with ERA. ACPA and radiographic joint damage are believed to be the most important outcome measure in ERA populations in the majority of the research [31,32,33]. The finding that cervical arthritis is linked to peripheral erosive disease is not a surprise [34, 35]. The correlation between arthritis of the atlantoaxial joint and peripheral radiographic damage could reinforce the theory of the primary influence of synovitis over that of bone destruction, as already demonstrated during the initial phases of the disease in the hands and feet [36, 37].
Magarelli and colleagues pointed to the early beginning of the cervical spine synovitis in patients with active and evolving RA. In their study, the ESR had a significantly higher mean value in patients with atlantoaxial instability compared to patients who did not have this kind of involvement. A higher mean value of DAS28 was revealed in the first group compared to the second one. Moreover, in 80% of the patients with atlantoaxial instability ACPA and RF were present, and all the patients of the first group had radiographic erosive changes [38]. Chellapandian et al. found a correlation between the involvement of cervical spine with disease duration, tender joint count, SJC, joint deformities, extra-articular features such as rheumatoid nodules, RF positivity, and erosions in X-rays of hands and feet [39]. Paimela and colleagues evaluated prospectively 67 RA patients. They revealed the early presence of spinal damage in those patients with a higher disease activity and with a peripheral erosive disease [40].
Bouchaud-Chabot et al., in a review of the literature, highlighted the presence of a severe peripheral erosive disease among the risk factors of the cervical spine arthritis [41].
The results coming from our study corroborate those from the works previously cited. The positivity of biological markers such as ACPA, high disease activity, as well the peripheral erosive disease, are predictive factors for the development of the atlantoaxial involvement in patients with RA, even in the subjects with early disease.
The major limitations of this study have to be mentioned. First of all, the results of could be somewhat limited by the small sample size, which makes it difficult to extrapolate the findings in this cohort to other settings. For this reason, our findings are only applicable to ERA patients. Secondly, synovitis was evaluated without the administration of intravenous contrast. The contrast medium utilization allows a good distinction between a hypervascularized synovium, a fibrous pannus, or a synovial effusion [4]. However, fat-suppressed T2-weighted and STIR sequences, which can reveal increased water content, can be considered a good alternative to contrast-enhanced sequences to identify synovitis in RA patients [27, 42]. In our opinion, and in that of other researchers, MRI without contrast is likely to be sufficient for some purposes [42, 43].
Finally, from a practical point of view, in daily practice, the indication for a cervical spine MRI in subjects with early disease in absence of symptoms seems difficult to justify.
However, taking into account the significant prevalence of the atlantoaxial joint synovitis, even in the absence of symptoms, we believe that a baseline cervical spine MRI in patients with active and erosive ERA, who are seropositive for ACPA, could be strongly considered [44].
In conclusion, MRI identification of atlantoaxial synovitis provides additional information regarding disease activity in patients with ERA, and may be a possible marker of disease progression. Further studies in larger populations with ERA are needed to provide information for comparison with our results. Predicting which ERA patients with asymptomatic atlantoaxial synovitis will progress to being symptomatic and could benefit from therapeutic intervention will be an important area of future research.
References
Salaffi F, De Angelis R, Grassi W. Prevalence of musculoskeletal conditions in an Italian population sample: results of a regional community-based study. The MAPPING study. Clin Exp Rheumatol. 2005;23(6):819–28.
Cross M, Smith E, Hoy D, Carmona L, Wolfe F, Vos T, et al. The global burden of rheumatoid arthritis: estimates from the global burden of disease 2010 study. Ann Rheum Dis. 2014;73(7):1316–22.
Zikou AK, Alamanos Y, Argyropoulou MI, Tsifetaki N, Tsampoulas C, Voulgari PV, et al. Radiological cervical spine involvement in patients with rheumatoid arthritis: a cross sectional study. J Rheumatol. 2005;32(5):801–6.
Zoli A, Priolo F, Galossi A, Altomonte L, Di Gregorio F, Cerase A, et al. Craniocervical junction involvement in rheumatoid arthritis: a clinical and radiological study. J Rheumatol. 2000;27(5):1178–82.
Joaquim AF, Appenzeller S. Cervical spine involvement in rheumatoid arthritis—a systematic review. Autoimmun Rev. 2014;13(12):1195–202.
Aggarwal A, Kulshreshtha A, Chaturvedi V, Misra R. Cervical spine involvement in rheumatoid arthritis: prevalence and relationship with overall disease severity. J Assoc Physicians India. 1996;44(7):468–71.
Blom M, Creemers MC, Kievit W, Lemmens JA, van Riel PL. Long-term follow-up of the cervical spine with conventional radiographs in patients with rheumatoid arthritis. Scand J Rheumatol. 2013;42(4):281–9.
Younes M, Belghali S, Kriâa S, Zrour S, Bejia I, Touzi M, et al. Compared imaging of the rheumatoid cervical spine: prevalence study and associated factors. Joint Bone Spine. 2009;76(4):361–8.
Suppiah R, Doyle A, Rai R, Dalbeth N, Lobo M, Braun J, et al. Quantifying bone marrow edema in the rheumatoid cervical spine using magnetic resonance imaging. J Rheumatol. 2010;37(8):1626–32.
Joaquim AF, Ghizoni E, Tedeschi H, Appenzeller S, Riew KD. Radiological evaluation of cervical spine involvement in rheumatoid arthritis. Neurosurg Focus. 2015;38(4):E4.
Aletaha D, Neogi T, Silman AJ, Funovits J, Felson DT, Bingham CO III, et al. Rheumatoid arthritis classification criteria: an American College of Rheumatology/European League Against Rheumatism collaborative initiative. Ann Rheum Dis. 2010;69(9):1580–8.
Anderson JK, Zimmerman L, Caplan L, Michaud K. Measures of rheumatoid arthritis disease activity: patient (PtGA) and provider (PrGA) global assessment of disease activity, disease activity score (DAS) and disease activity score with 28-joint counts (DAS28), simplified disease activity index (SDAI), clinical disease activity index (CDAI), patient activity score (PAS) and patient activity score-II (PASII), routine assessment of patient index data (RAPID), rheumatoid arthritis disease activity index (RADAI) and rheumatoid arthritis disease activity Index-5 (RADAI-5), chronic arthritis systemic index (CASI), patient-based disease activity score with ESR (PDAS1) and patient-based disease activity score without ESR (PDAS2), and mean overall index for rheumatoid arthritis (MOI-RA). Arthritis Care Res. 2011;63(Suppl 11):S14–36.
Caporali R, Conti F, Covelli M, Govoni M, Salaffi F, Ventriglia G, et al. Treating rheumatoid arthritis to target: an Italian rheumatologists' survey on the acceptance of the treat-to-target recommendations. Clin Exp Rheumatol. 2014;32(4):471–6.
Fries JF, Spitz P, Kraines RG, Holman HR. Measurement of patient outcome in arthritis. Arthritis Rheum. 1980;23(2):137–45.
Ranza R, Marchesoni A, Calori G, Bianchi G, Braga M, Canazza S, et al. The Italian version of the functional disability index of the health assessment questionnaire. A reliable instrument for multi center studies on rheumatoid arthritis. Clin Exp Rheumatol. 1993;11(2):123–8.
Dias EM, Lukas C, Landewe R, Fatenejad S, van der Heijde D. Reliability and sensitivity to change of the simple erosion narrowing score compared with the Sharp-van der Heijde method for scoring radiographs in rheumatoid arthritis. Ann Rheum Dis. 2008;67(3):375–9.
van der Heijde DM, van Riel PL, Nuver-Zwart IH, Gribnau FW, van de Putte LB. Effects of hydroxychloroquine and sulphasalazine on progression of joint damage in rheumatoid arthritis. Lancet. 1989;1(8646):1036–8.
Barnabe C, Hazlewood G, Barr S, Martin L. Comparison of radiographic scoring methods in a cohort of RA patients treated with anti-TNF therapy. Rheumatology (Oxford). 2012;51(5):878–81.
Kwong Y, Rao N, Latief K. Craniometric measurements in the assessment of craniovertebral settling: are they still relevant in the age of cross-sectional imaging? AJR Am J Roentgenol. 2011;196(4):W421–5.
Narváez JA, Narváez J, de Albert M, De Lama E, Serrallonga M, Nolla JM. Bone marrow edema in the cervical spine of symptomatic rheumatoid arthritis patients. Semin Arthritis Rheum. 2009;38(4):281–8.
Bundschuh C, Modic MT, Kearney F, Morris R, Deal C. Rheumatoid arthritis of the cervical spine: surface-coil MR imaging. AJR Am J Roentgenol. 1988;151(1):181–7.
Reijnierse M, Bloem JL, Dijkmans BA, Kroon HM, Holscher HC, Hansen B, et al. The cervical spine in rheumatoid arthritis: relationship between neurologic signs and morphology of MR imaging and radiographs. Skelet Radiol. 1996;25(2):113–8.
Bogduk N, Major GA, Carter J. Lateral subluxation of the atlas in rheumatoid arthritis: a case report and post-mortem study. Ann Rheum Dis. 1984;43(2):341–6.
Nguyen HV, Ludwig SC, Silber J, Gelb DE, Anderson PA, Frank L, et al. Rheumatoid arthritis of the cervical spine. Spine J. 2004;4(3):329–34.
Matthews JA. Atlanto-axial subluxation in rheumatoid arthritis. A 5-year follow-up study. Ann Rheum Dis. 1974;33(6):526–31.
Pellici PM, Ranawat CS, Tsairis P, Bryan WJ. A prospective study of the progression of rheumatoid arthritis of the cervical spine. J Bone Joint Surg Am. 1981;63(3):342–50.
Rana NA. Natural history of atlanto-axial subluxation in rheumatoid arthritis. Spine (Phila Pa 1976). 1989;14(10):1054–6.
Dreyer SJ, Boden SD. Natural history of rheumatoid arthritis of the cervical spine. Clin Orthop Relat Res. 1999;366:98–106.
Cha TD, An HS. Cervical spine manifestations in patients with inflammatory arthritides. Nat Rev Rheumatol. 2013;9(7):423–32.
Kosta PE, Voulgari PV, Zikou AK, Drosos AA, Argyropoulou MI. The usefulness of magnetic resonance imaging of the hand and wrist in very early rheumatoid arthritis. Arthritis Res Ther. 2011;13(3):R84.
Salaffi F, Ferracioli G, Peroni M, Carotti M, Bartoli E, Cervini C. Progression of erosion and joint space narrowing scores in rheumatoid arthritis assessed by nonlinear models. J Rheumatol. 1994;21(9):1626–30.
Scott DL, Pugner K, Kaarela K, Doyle DV, Woolf A, Holmes J, et al. The links between joint damage and disability in rheumatoid arthritis. Rheumatology (Oxford). 2000;39(2):122–32.
Lindqvist E, Saxne T, Geborek P, Eberhardt K. Ten year outcome in a cohort of patients with early rheumatoid arthritis: health status, disease process, and damage. Ann Rheum Dis. 2002;61(12):1055–9.
Ahn JK, Hwang JW, Oh JM, Lee J, Lee YS, Jeon CH, et al. Risk factors for development and progression of atlantoaxial subluxation in Korean patients with rheumatoid arthritis. Rheumatol Int. 2011;31(10):1363–8.
Neva MH, Isomaki P, Hannonen P, Kauppi M, Krishnan E, Sokka T. Early and extensive erosiveness in peripheral joints predicts atlantoaxial subluxations in patients with rheumatoid arthritis. Arthritis Rheum. 2003;48(7):1808–13.
Conaghan PG, O’Connor P, McGonagle D, Astin P, Wakefield RJ, Gibbon WW, et al. Elucidation of the relationship between synovitis and bone damage: a randomized magnetic resonance imaging study of individual joints in patients with early rheumatoid arthritis. Arthritis Rheum. 2003;48(1):64–71.
McQueen FM, Benton N, Perry D, Crabbe J, Robinson E, Yeoman S, et al. Bone edema scored on magnetic resonance imaging scans of the dominant carpus at presentation predicts radiographic joint damage of the hands and feet six years later in patients with rheumatoid arthritis. Arthritis Rheum. 2003;48(7):1814–27.
Magarelli N, Simone F, Amelia R, Leone A, Bosello S, D’Antona G, et al. MR imaging of atlantoaxial joint in early RA. Radiol Med. 2010;115(7):1111–20.
Chellapandian D, Panchapekesa RC, Rukmangatha S, et al. Cervical spine involvement in rheumatoid arthritis and its correlation with disease severity. J Indian Rheumatol Assoc. 2004;12:2–5.
Paimela L, Laasonen L, Kankaanpää E, Leirisalo-Repo M. Progression of cervical spine changes in patients with early rheumatoid arthritis. J Rheumatol. 1997;24(7):1280–4.
Bouchaud-Chabot A, Liotè F. Cervical spine involvement in rheumatoid arthritis. A review. Joint Bone Spine. 2002;69(2):141–54.
Ostergaard M, Ejbjerg B, Szkudlarek M. Imaging in early rheumatoid arthritis: roles of magnetic resonance imaging, ultrasonography, conventional radiography and computed tomography. Best Pract Res Clin Rheumatol. 2005;19(1):91–116.
Ostergaard M, Ejbjerg B. Magnetic resonance imaging of the synovium in rheumatoid arthritis. Semin Musculoskelet Radiol. 2004;8(4):287–99.
Del Grande M, Del Grande F, Carrino J, Bingham CO III, Louie GH. Cervical spine involvement early in the course of rheumatoid arthritis. Semin Arthritis Rheum. 2014;43(6):738–44.
Author information
Authors and Affiliations
Contributions
MC has been the principal investigator, responsible for the coordination and management of the study, and scored the radiographic examinations. FaS participated in the conception of the study, in the acquisition of clinical data, scored the radiographic examinations, drafted the manuscript, and was the more experienced reader of data analysis. MDC participated in the acquisition of data and has been involved in revising the paper for intellectual content. FrS performed the MRI examinations, took part in study planning, and in the analysis of data. AG was the critical and final editor, study design planner, and supervisor. All authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethical approval
All procedures performed in this study were in accordance with the ethical standards of our institutional research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. Written informed consent was obtained from all individual participants included in the study.
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Carotti, M., Salaffi, F., Di Carlo, M. et al. Magnetic resonance imaging of the craniovertebral junction in early rheumatoid arthritis. Skeletal Radiol 48, 553–561 (2019). https://doi.org/10.1007/s00256-018-3055-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00256-018-3055-9