Abstract
Purpose
To create a timetable for dating long bone fractures in infants aged less than 1 year using previously defined radiographic signs of fracture healing.
Materials and methods
A retrospective cross-sectional time series of long bone fractures in infants aged less than 1 year was conducted from 2006 to 2013. After exclusion criteria were applied 59 digital image series were available for review from 40 infants. Utilizing published criteria for dating fractures, the presence or absence of four pre-defined features of healing was scored: periosteal reaction, callus, bridging, and remodeling. Three radiologists independently scored radiographs with a 3-point scale, marking each feature as present, absent, or equivocal. The times in days when features were first seen, peaked (feature agreed present in >40% of images), and last seen were noted. Statistical analysis using free marginal kappa was conducted.
Results
The level of agreement among the three radiologists was high (0.64–0.85). The sequence in which the features were seen was: periosteal reaction range 7–130 (present in the majority of cases between 9 and 49 days); callus range 9–130 (present in the majority of cases between days 9–26); bridging range 15–130 (seen in the majority of cases between 15 and 67 days); remodeling range 51–247 days.
Conclusion
This study provides a timetable of radiological features of long bone healing among young infants for the first time. Dating of incomplete long bone fractures is challenging, beyond the presence of periosteal reaction, but a consistent sequence of changes is present in complete fractures.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
According to the 4th National Incidence Study of Childhood Abuse and Neglect, 1 child in every 58 in the USA experiences maltreatment each year, with nearly half of child abuse-related fatalities occurring in children younger than 1 year of age [1]. Fractures are common and occur most frequently in children less than 3 years of age, with at least half occurring in children less than 1 year of age [1, 2]. Consequently, estimating the timing of skeletal injury appropriately can be of great importance in forensic cases and can have a significant bearing on the judicial process [3].
Dating of fractures for many years was based on a timetable initially published by O’Connor and Cohen in 1998 [4], which was based on clinical experience rather than scientific evidence. This timetable, following the publication of the Walters’ manuscript on the healing of clavicle fractures written in conjunction with Kleinman [5], has been recently updated in the third edition of Diagnostic Imaging of Child Abuse [6], with only modest changes from the original. Other studies published to date are predominantly based on long bone fracture healing in older children [7, 8], although the majority of abusive fractures occur in infants less than 18 months of age.
Skeletal fractures are known to follow an expected course of healing histologically. Following the initial trauma resulting in a fracture, the periosteum is stripped away from the underlying cortical bone, and the contained hemorrhage dissects between the periosteum and cortex. The hematoma is gradually replaced by vascular fibrous tissue along with new bone [4]. Callus develops at the ends of the fracture by cellular organization within the subperiosteal hematoma and ultimately unites the fracture fragments. Fibrovascular tissue replaces the hematoma with collagen fibers, and the bone matrix is mineralized, resulting in the formation of woven bone that eventually forms an osseous union across the fracture site. These occurrences manifest radiographically as periosteal reaction/elevation (reparative), callus formation (reparative), bridging, and remodeling.
As the timing of skeletal injury can be of great importance in cases of suspected abuse, with a lack of published evidence related to radiological features of fracture healing in relation to young infants, we set out to develop a timetable of long bone fracture healing in infants less than 1 year of age, using previously defined radiographic signs of fracture healing.
Methods
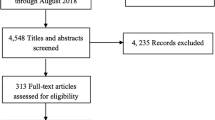
We completed a retrospective cross-sectional time-series study of digital radiographs (5 different lower extremity radiographic examination series, i.e., 2 views of the femur, and 4 different upper extremity radiographic examination series, i.e., 3 views of the humerus) at our free-standing tertiary care children’s hospital from 2006 to 2013. The diagnostic radiography during this period was performed on x-ray units manufactured by Swissray Global Healthcare Holding Ltd. with two unit models utilized (ddR Formula and Combitrauma). The study was approved by the Institutional Review Board and deemed exempt from requiring informed consent. Cases were identified from the hospital electronic medical record. Each positive result obtained from the database query was reviewed to confirm the fracture was visible radiographically. The exclusion criteria included confirmed or suspected physical abuse, fractures in which date of injury could not reliably be confirmed, metabolic bone disorders, and poorly visualized fractures such as those in which a cast was present. In individual long bones with more than one fracture per case, the most apparent fracture was scored. No fractures were treated with internal fixation. All radiographs were anonymized prior to scoring within the study.
The initial search resulted in 69 patients with 209 radiographs. After the initial exclusion criteria had been applied, 51 patients remained with a total of 100 examinations. An additional 41 images were excluded, all of which were 7 days or less from the time of documented injury, given there was unanimous agreement by the raters that there was no evidence of healing, leaving 40 patients with a total of 59 radiographic series for analysis. Fractures were then further subdivided into two categories: complete (41) or incomplete (18). A complete fracture was defined as a fracture with both cortices disrupted, while an incomplete fracture was defined as having only a single cortex disrupted.
The timing of the radiographs in days represented an unbalanced panel data set because the number of radiographic series obtained for each fracture was determined clinically. Images were obtained varying between 1 and 4 points in time per patient. Three pediatric radiologists, with experience ranging from 6 to 25 years, independently assessed each radiograph. Each radiologist was blinded to the age, gender, and timing of the original injury. The radiographs were presented in a random order unique to each radiologist to minimize memory bias and fatigue.
The presence or absence of four radiographic features of fracture healing (periosteal reaction, callus, bridging, and remodeling) were scored for all radiographs. Each radiologist was provided with training as to the application of the definitions at each stage of healing, including written and pictorial content (Figs. 1, 2, 3, and 4). The following were the explicit definitions for the stages of fracture healing utilized in the study: (1) periosteal reaction: linear (not rounded) elevation and/or calcification of the periosteum along the shaft of the bone at or near the fracture site; (2) callus: evidence of healing as new bone is laid down, which gradually calcifies and ossifies, eventually enveloping the fracture site in a noncontiguous fashion with continued visualization of the fracture line. This initially has a “fluffy” edge followed by a more well demarcated dense edge that is nearly as dense as cortex; (3) bridging: fracture site has been completely crossed by intact callus on both sides of the bone, regardless of whether the fracture line still remains visible centrally; (4) bony remodeling: loss of fracture line definition with complete bridging of the fracture gap by continuity of cortical bone with the callus no longer being distinguishable from underlying cortex.
Callus. Two examples of callus (yellow arrows in a and b). Callus develops at a fracture site as new bone is laid down, which gradually calcifies and ossifies to eventually envelop the fracture site. This occurs in a noncontiguous fashion with continued visualization of the fracture line at this stage of healing. The callus in (b) is incomplete laterally with continued visualization of the fracture line (blue arrow)
Remodeling. Loss of fracture line definition with complete bridging of the fracture gap secondary to continuity of cortical bone with callus indistinguishable from underlying cortex. This progression is apparent when comparing the presence of callus at 24 days post injury in (a) to changes of remodeling present at 120 days post injury in (b)
Radiologists scored radiographs with a 3-point scale as either present, indeterminate (including images that the radiologist could not score because of technical flaws) or absent. In the absence of a gold standard, features were defined to be ‘agreed present’ when two or more radiologists stated that the feature was present. For the purposes of analysis, all radiographs were dichotomized for each of the four features of fracture healing into ‘agreed present’ and ‘not agreed present.’ Note that the ‘not agreed present’ group included all other alternatives to ‘agreed present.’ Thus, for each of the four features of fracture healing, the proportion of radiographs with that feature ‘agreed present’ was calculated.
Statistical analysis
The scores were entered into a Microsoft Excel spread sheet database. The 3-point scale results provided by the radiologists included 1 absent, 2 indeterminate, and 3 present. This allowed assessment of agreement between radiologists based on stated feature presence, reducing ambiguity between overlapping definitions and moving toward the development of a broader “agreed present” definition [9]. Interobserver agreement was assessed using free marginal multirater kappa for the aggregated score.
Results
A total of 40 patients with 59 radiographic series underwent analysis. There were 41 complete fractures and 18 incomplete fractures in total. Each image series was reviewed by 3 pediatric radiologists resulting in 177 interpretations. The infants ranged in age from 9 days to 12 months at the time of initial imaging. The infants’ fracture ages ranged from 0 to 247 days, with a mean fractures age of 31.97 days (SD ±38.84 days). There were a total of 8 imaging series evaluated from day 0–6, 12 image series from day 7–21, 31 image series from day 22–51 and 8 image series from 52 days or greater (Table 1).
The level of agreement among the three radiologists overall was 0.64–0.85 (Table 2). The level of agreement for complete fractures was 0.56–0.90 and for buckle/incomplete fractures was 0.47–0.75 (Table 2). Periosteal reaction was first seen at day 7, last seen on day 130, and present in the majority of cases between 9 and 49 days. When incomplete fractures were removed from the analysis, the first sign of periosteal reaction was seen at day 9. Callus was also first seen at day 9, last seen at day 130, and present in the majority of cases between days 9–26 when all fractures were included. When only complete fractures were included, callus was present in the majority of the cases between days 9–36. Bridging was first seen at day 15, seen in the majority of cases between 15 and 67 days, and last seen at day 130. Remodeling was seen from days 51–247.
Periosteal reaction initially appears at a comparable time in both incomplete and complete fractures, although the peak occurs more rapidly with incomplete fractures at 7–28 days. Regarding the other radiographic features of healing, there was no agreement as to the presence of callus, bridging, or remodeling in 15 of the 18 cases with incomplete fractures (Table 3).
Discussion
This study of infants aged less than 1 year, the age at which abusive fractures are most common, is the largest study to date addressing the topic of fracture healing of long bones among infants. The previous studies of this age group predominantly dealt with healing rib or clavicle fractures. The results show that it is possible to define a broad timetable of healing for fractures based on the ordered progression of radiological features of fracture healing, thus facilitating the dating of fractures with an unknown time of injury in this vulnerable age group. It is reassuring to note the high level of agreement among radiologists when defining the presence or absence of specific radiological features of healing. This has the important implication that if radiologists with varying levels of experience are involved in the dating of infant fractures, they can apply criteria that are unambiguous and consistent.
Given the above data, if periosteal reaction and callus formation are absent in a complete fracture then it is consistent with being <9 days old. If periosteal reaction and callus formation are present without evidence of bridging, the fracture is at least 9–14 days old. If there is evidence of bridging without remodeling then the fracture is at least 15–51 days old. Once remodeling is present, regardless of whether the fracture is complete or incomplete, then the fracture is >51 days old (Table 4). Caution should be taken when attempting to date incomplete fractures given the limited data (Appendix Tables 5 and 6).
It appears that radiographic healing of incomplete fractures may differ somewhat in comparison to complete fractures in the later stages. Periosteal reaction appears essentially at the same time in both incomplete and complete fractures. Regarding the other radiographic features of healing, there was no clarity as to the presence of callus, bridging, or remodeling in the majority of cases. It is possible that this is due to decreased disruption and/or stripping of the periosteum away from the parent bone in incomplete fractures, and therefore there is less potential space for a subperiosteal hematoma to collect. This makes the previously described early radiographic stages of fracture healing less apparent and the later stages of fracture healing often not visualized. The lesser degree of injury to the periosteum seen in incomplete fractures could therefore result in an increase in the rate of healing for this specific type of fracture. However, a clear conclusion of this study would be that caution should be exercised in dating incomplete fractures radiologically, beyond the observation that if a periosteal reaction is present, the fracture may be between 1 and 4 weeks old.
There is scant scientific evidence pertaining to fracture healing in this age group, with only a few relevant studies. The first study, published in 1979, looked at birth-related fractures in 23 newborns that occurred at three different sites (clavicle, humerus, and femur) assessing only for the initial appearance of calcification at the fracture site [10]. A subsequent small study assessing callus formation in fractures of the femoral diaphysis in 25 patients, ages birth to 14 years of age, included 10 patients less than 4 years of age. However, the authors did not provide the specific ages of each patient; consequently, it is unknown whether any of the patients were less than 1 year of age [11]. Likewise, Islam et al. [8], studying forearm fractures in those aged 0–17 years of age, only included 23 children aged 0–4, with no information as to whether any were aged less than 1 year. Prosser et al. studied 53 children aged less than 5 years with long bone fractures, but the mean age was 4.8 years [9].
Malone’s paper from 2011 looked at healing fractures of the tibia and radius in 107 patients, 31 of whom were less than 1 year of age [3]. Unfortunately, this study did not exclude children who had been abused, potentially influencing the true timing of the injury. The authors did not comment on subperiosteal new bone formation, but rather differentiated soft from hard callus, assessed bridging, as well as completion, which would correspond with our definition of remodeling, and performed a clinical assessment. Many of their patients were assessed while casted, which has been shown to limit the ability to evaluate specific radiographic features [8, 9].
Halliday’s 2011 article looked at 31 patients with a total of 161 conventional radiographs obtained to evaluate long bone fractures as the result of suspected abuse [12]. The majority of patients were less than 1 year of age, and soft-tissue swelling, periosteal reaction, fracture line definition, callus formation, and callus and endosteal callus were quantified radiographically. However, determining the timing of injury or injuries with certainty in cases of suspected abuse such as these can only be an estimate, thus calling into question the validity of some of their findings.
The data in our study are broadly consistent with O’Connor and Cohen [4], Kleinman and Walters [5, 6], and Cumming [10] in noting the initial appearance of a periosteal reaction around 7–9 days. We also looked at the duration of the periosteal reaction with a second peak at 49 days and last seen at 130 days. This long duration however is not surprising as resorbing callus can result in persistent elevation of the periosteum. This observation requires emphasis, as a persistent periosteal reaction late in the healing process could potentially be a confounding factor when attempting to date a healing fracture; consequently, radiographs from at least two separate points in time should be evaluated to allow differentiation of fractures at the early stages of healing from fractures at the late stages of healing.
In our study, callus was initially seen at 9 days, peaking between 9 and 26 days and last seen at day 130. This is broadly similar to Walters [5] summed data relating to newborn clavicle fractures as they separated out soft and hard callus while we did not. Callus did appear to last longer in the current study of long bone fractures than in the Walters study of healing clavicle fractures, although they [5] did not specifically comment on the duration of callus, and there is also the potential for some variation in the healing of the clavicle, as ossification of the clavicle differs from that in other tubular bones, undergoing both endochondral and intramembranous ossification, with the potential for it to heal slightly differently from other long bones. Consequently, healing patterns of the clavicle may not be generalizable to other long bone fractures.
The long duration of remodeling in our data set without the presence of a significant peak was comparable to that suggested by O’Connor and Cohen [4] who indicated that remodeling can take up to 2 years to resolve, though contradictory to some previous studies [8, 11] that suggested that remodeling resolves around 8 or 9 weeks. A likely consideration as to why remodeling resolved more quickly in forearm fractures in Islam’s study and femoral fractures in Yeo’s study is the significantly varied definition of remodeling used in each study. We defined remodeling as loss of fracture line definition with complete bridging of the fracture gap by continuity of cortical bone while Yeo referred to the maturity of callus and Islam defined remodeling as the loss of a focal cortical bump or an increase in the obtuse angle of new bone with cortex.
The strengths of the current study include the inclusion of the patient population most frequently abused, i.e., infants less than 1 year of age, and in whom the dating of fractures of unknown timing is most frequently required. The decision to restrict the study to digital radiography and non-casted fractures and to only evaluate long bones, as they ossify exclusively by enchondral ossification, maximized consistency across the data set. The data provided can thus inform an evidence-based estimate of the age of a fracture within the population of interest, utilizing easily measurable and reproducible characteristics that can be applied by a wide range of professionals.
The limitations of this work include its retrospective observational methodology, whereby the timing of images was dictated by clinical need and led to an unbalanced data set. However, it would be unethical to impose a timetable of imaging of infants purely for research purposes because of the potential radiation risk. Though every effort was made to document a known mechanism and timing for the injuries, we cannot 100% exclude that there were no cases of abuse. As no metaphyseal corner fractures were included in this data set, the time of radiological features of healing cannot be generalized to the classic metaphyseal lesion.
There is a clear need for radiologists who are estimating the timing of fractures to use a standardized approach, thus minimizing inconsistencies between reports and improving the quality of evidence given to investigating teams and provided to courts, thus providing a higher standard of medical evidence available for decision making by other professionals involved. Future research into the application of the proposed timetable on a novel data set would further strengthen the evidence base in this important field.
Conclusion
This study provides a clear and reproducible set of radiological features that can be applied when determining whether a given fracture is consistent with a proposed time frame, especially in assessing cases in which non-accidental trauma is a consideration. These features of fracture healing develop in a logical progression, and the specific combinations of features present at any one time period offer a timetable of healing: a fracture with no evidence of periosteal reaction is likely to be less than 1 week old, the presence of periosteal reaction and callus formation alone indicates the fracture is at least 9–14 days old, the presence of bridging indicates the fracture is at least 2 weeks old, and once remodeling is seen, regardless of other features, the fracture is likely to be at least 51 days old.
References
Skellern CY, Wood DO, Murphy A, Crawford M. Non-accidental fractures in infants: risk of further abuse. J Paediatr Child Health. 2000;36:590–2.
Hoskote A, Martin K, Hormbrey P, Burns E. Fractures in infants: one in four is non-accidental. Child Abuse Rev. 2003;12:384–91.
Malone CA, Sauer NJ, Fenton TW. A radiographic assessment of pediatric fracture healing and time since injury. J Forensic Sci. 2011;56:1123–30.
O’Connor JF, Cohen J. Dating fractures. In: Kleinman P, editor. Diagnostic imaging of child abuse. St. Louis: Mosby; 1998.
Walters MM, Forbes PW, Buonomo C, Kleinman PK. Healing patterns of clavicular birth injuries as a guide to fracture dating in cases of possible infant abuse. Pediatr Radiol. 2014;44:1224–9.
Kleinman P, Walters MM. Dating Fractures. In: Kleinman P, editor. Diagnostic Imaging of Child Abuse. UK: Cambridge University Press; 2015.
Prosser I, Maguire S, Harrison SK, Mann M, Sibert JR, Kemp AM. How old is this fracture? Radiologic dating of fractures in children: a systematic review. AJR Am J Roentgenol. 2005;184:1282–6.
Islam O, Soboleski D, Symons S, Davidson LK, Ashworth MA, Babyn P. Development and duration of radiographic signs of bone healing in children. AJR Am J Roentgenol. 2000;175:75–8.
Prosser I, Lawson Z, Evans A, Harrison S, Morris S, Maguire S, et al. A timetable for the radiologic features of fracture healing in young children. AJR Am J Roentgenol. 2012;198:1014–20.
Cumming WA. Neonatal skeletal fractures. Birth trauma or child abuse. J Assoc Can Radiol. 1979;30:30–3.
Yeo LI, Reed MH. Staging of healing of femoral fractures in children. Can Assoc Radiol J. 1994;45:16–9.
Halliday KE, Broderick NJ, Somers JM, Hawkes R. Dating fractures in infants. Clin Radiol. 2011;66:1049–54.
Acknowledgements
Elizabeth Caroll, Research Assistant.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
This article does not contain identifiable patient data.
Appendix
Appendix
Rights and permissions
About this article
Cite this article
Warner, C., Maguire, S., Trefan, L. et al. A study of radiological features of healing in long bone fractures among infants less than a year. Skeletal Radiol 46, 333–341 (2017). https://doi.org/10.1007/s00256-016-2563-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00256-016-2563-8