Abstract
Objective
To examine the association between tibial pilon and calcaneal fracture classification and tendon entrapment or dislocation.
Materials and methods
After institutional review board approval, we retrospectively reviewed consecutive CT scans with calcaneal or pilon fractures from 5 years at a level 1 trauma center. We categorized calcaneal fractures according to the Sanders classification, and pilon fractures according to the Ruedi and Allgower and the Arbeitsgemeinschaft für Osteosynthesefragen-Orthopaedic Trauma Association (AO-OTA) classifications. Ankle tendons were assessed for dislocation or entrapment. Fisher’s exact test was used for statistical analysis with significance at p < 0.05.
Results
A total of 312 fractures (91 pilon only, 193 calcaneal only, and 14 ankles with ipsilateral pilon and calcaneal fractures) were identified in 273 patients. Twenty-two pilon, 42 calcaneal, and nine combination fractures were associated with 99 occurrences of tendon entrapment or superior peroneal retinacular injury. Such findings were associated with multiple fractures (p = 0.002). Multifragmentary pilon fractures were associated with posterior tibial and flexor digitorum longus tendon entrapment (p < 0.0001 and p = 0.0003 for Ruedi/Allgower and AO-OTA, respectively), and multifragmentary Sanders type 3 or 4 calcaneal fractures were associated with superior peroneal retinacular injury (p = 0.0473) compared to simple fracture patterns. Thirty-nine percent of tendon entrapments or retinacular injuries were prospectively identified, 85 % by musculoskeletal radiologists (p < 0.0001).
Conclusions
Approximately 25 % of calcaneal and pilon fractures were retrospectively identified to contain posteromedial tendon entrapment or superior peroneal retinacular injury. Radiologists should meticulously search for such injuries, particularly when analyzing multifragmentary and multiple fractures.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Fractures of the calcaneus and distal tibia are relatively common injuries that are often treated with open reduction and internal fixation to optimize functional recovery [1–5]. It has been established that subluxation or dislocation of the peroneal tendons may complicate calcaneal fractures and entrapment of the posteromedial soft tissue structures including the flexor tendons may complicate pilon fractures by preventing reduction or healing, or by causing chronic ankle pain or instability [1, 3–12]. CT scans are often obtained to evaluate fracture fragments in more detail and to guide surgical approach, and CT may reliably demonstrate soft tissue entrapment within fractures [3, 5, 8].
While peroneal tendon injuries including entrapment, impingement, or subluxation/dislocation have been documented in 28-70 % of intraarticular calcaneal fractures, radiologic and even operative detection of peroneal tendon injury has been reported to be poor [13, 14]. Toussaint et al. (2014) identified 118 cases of peroneal tendon subluxation or dislocation accompanying calcaneal fracture after repeat review of 421 CT scans. The authors reported that only 10.2 % of these cases with tendon subluxation/dislocation accompanying calcaneal fractures were identified radiologically in the original report. Only 10.8 % of tendon dislocations were treated operatively, and the authors concluded that the tendon dislocations were over six times more likely to have been treated if they were identified preoperatively by the radiologist [15]. Their data indicate the impact on treatment the radiologist may make if these injuries are correctly identified preoperatively.
Additionally, entrapment of the posterior tibial tendon or other posteromedial soft tissue structures may accompany pilon fractures. Crim et al. (2013) found flexor retinacular injury with flexor tendon abnormalities in 26 % of pilon fractures [14]. Irreducible fracture-dislocations of the ankle joint may be due to deltoid ligament or posterior tibial tendon interposition between fracture fragments, or from extensor tendons entrapped within the diastatic distal tibiofibular joint [16, 17]. While the most common soft tissue structure to become entrapped in pilon fractures is the posterior tibial tendon, any posteromedial structure including the flexor digitorum longus tendon or the tibial neurovascular bundle may become entrapped [1, 16, 18].
We present a retrospective analysis of 5 years of consecutive calcaneal and pilon fractures for concomitant tendon injuries including subluxation/dislocation or entrapment identified on CT scan. We hypothesized that multiple or more complex fractures would be associated with a higher incidence of associated tendon injuries. We also correlated with the clinical and surgical observations in an attempt to gauge our accuracy and sensitivity. Finally, we analyze the radiologists’ detection rates at our institution with comparison to the published data.
Methods
Subjects
After institutional review board approval, we performed a retrospective review of all CT scans with ICD-9 or CPT codes indicating calcaneal or pilon fractures from 1/1/2009 to 8/16/2014 at a level 1 trauma center.
A total of 431 records were identified, and 119 of these were excluded (see Table 1), leaving 312 fractures in 273 patients (298 ankles) available for inclusion. The most common reason a record was excluded was for a fracture that was incorrectly coded as a pilon or calcaneal fracture. The second most common reason for exclusion was unavailability of CT images on the Picture Archiving and Communication System (PACS) for review. Subjects were predominantly male (75.3 %), with a mean age of 40.2 years (range, 19–78 years). The first CT of the ankle or hindfoot from the time of injury was included in the analysis.
CT analysis
CT was performed on Siemens Definition and Sensation 64-slice scanners or Siemens Somatom Definition AS 128-slice scanner; 3-mm and 1.5-mm axial and 1.5-mm orthogonal sagittal and coronal reformats were provided for all CT scans, with bone and soft tissue multiplanar reconstruction kernels available for review for most CT scans.
All cases were retrospectively reviewed by a board-certified senior musculoskeletal attending radiologist with 29 years of experience and a post-graduate year 6 radiology resident with antecedent 2 years of orthopedic residency training. A consensus decision was used to identify the presence or absence of tendon entrapment or subluxation/dislocation to identify the presence or absence of avulsion fractures of the superior peroneal retinaculum causing a “fleck sign,” and to classify all pilon fractures according to both the Ruedi and Allgower classification (see Appendix 1) and the AO-OTA classification (see Appendix 2). Coronal oblique reformats through the widest portion of the posterior subtalar joint were created on the Philips PACS system for all calcaneal fractures in order to classify the calcaneal fractures according to the Sanders classification (see Appendix 3). For statistical analysis, fractures were categorized into simple or multifragmentary subgroups. The simple subgroup included Ruedi and Allgower types 1 or 2, AO-OTA types B1, B2, and C1, and Sanders types 1 and 2, and the multifragmentary subgroup included Ruedi and Allgower type 3, AO-OTA types B3, C2, and C3, and Sanders types 3 and 4 (see Appendices 1–4).
In our retrospective review, peroneal tendons were considered subluxated when the lateral tendon edge protruded from the margin of the lateral malleolus and dislocated when the peroneal tendons were located lateral or anterior to the lateral malleolus (Fig. 1). As subluxation and dislocation as well as a fleck sign imply injury to the superior peroneal retinaculum (Fig. 1), we refer to this simply as peroneal retinacular injury. All peroneal retinacular injuries were considered acute due to overlying soft tissue edema. Posteromedial tendons were considered entrapped when at least 50 % of the tendon cross-sectional area was located between major fracture fragments, which have been defined as anterior, posterior, medial, anterolateral, posterolateral, and die-punch fragments (see Appendix 4 and Fig. 2) [19].
Axial CT image (a) of a 55-year-old female who fell from 7 feet and sustained a Sanders type 3AC calcaneal fracture with dislocation of her peroneal tendons (solid arrow). A fleck sign is also seen (dotted arrow), indicating bony avulsion of the superior peroneal retinaculum. Coronal (b), sagittal (c), axial proton-density (d), and coronal STIR (e) MRI in a different patient demonstrate the subluxation of the peroneal tendons (solid arrow) with avulsion injury to the superior peroneal retinaculum (dotted arrow)
Axial CT scans of a 61-year-old female who fell from a curb, with entrapment of the posterior tibial tendon (arrow) within a Ruedi and Allgower type 3/AO-OTA type B3 pilon fracture (a). The patient was lost to follow-up, and axial (b) and coronal (c) CT scan 4 months later revealed persistent interposition of the posterior tibial tendon (dotted arrow) between fracture fragments without bony healing, with the flexor digitorum longus tendon (solid arrow) tracking into the region of entrapment
When available, findings at operative intervention were recorded, including whether the tendon subluxations/dislocations or entrapment had been identified or treated by the orthopedic surgeons.
Statistical analysis
Fisher’s exact test was used to perform univariate comparisons among fracture type and tendon injury. All statistics were calculated using Stata 13.1 (StataCorp, College Station, TX, USA); results were considered significant for p < 0.05.
Results
Tendon injury associations of the 312 fractures (91 pilon only, 193 calcaneus only, and 14 ankles with ipsilateral both pilon and calcaneal fractures) are summarized in Table 2. Seventy-three of the 207 calcaneus fractures were extraarticular, not involving the posterior subtalar facet, of which 68 extraarticular fractures were in ankles with only a calcaneus fracture. Fourteen CT scans revealed ipsilateral both calcaneus and pilon fractures, in which there were nine posteromedial tendon entrapments (four posterior tibial, two flexor digitorum longus, and one flexor hallucis longus) and seven peroneal tendon subluxation/dislocations, six of which occurred in combination fractures including an intraarticular calcaneus fracture and one of which occurred with an extraarticular calcaneus fracture. Overall, 73 of these fractures (23 %) revealed acute tendon subluxation/dislocation or entrapment: 22 of 91 (24 %) pilon only fractures, 42 of 193 (22 %) calcaneal only fractures, and nine of 14 (64 %) of ipsilateral both calcaneal and pilon fractures.
In 40 % of cases (n = 119/298), the CT was performed after closed reduction and splinting. Prior to reduction, peroneal retinacular injury was identified in 28 CT scans and posteromedial tendon entrapment was identified in 17 CT scans. After reduction, peroneal retinacular injury was identified in 18 CT scans and posteromedial tendon entrapment was identified in 17 CT scans, with no statistically significant difference between groups (p = 0.43).
Posterior tibial tendon dislocation without entrapment was also retrospectively identified in two additional patients, however there were no surrounding inflammatory changes or edema, and these were postulated to be chronic in etiology and not considered a positive finding for this analysis.
A total of 236 patients (86.4 %) sustained a single fracture, 53 of whom had injury to the peroneal retinaculum or entrapped posteromedial tendons. Thirty-seven patients (13.6 %), 18 of whom had such injury, sustained multiple fractures such as bilateral calcaneal fractures (n = 21), bilateral pilon fractures (n = 2), pilon fracture with ipsilateral or contralateral calcaneal fracture (n = 12), or bilateral calcaneal fractures with a single pilon fracture (n = 2). There was a statistically significant association between the incidence of tendon entrapment or subluxation/dislocation and the presence of multiple fractures in the same patient (p = 0.002).
Pilon fractures were more frequently associated with overall posteromedial tendon entrapment than calcaneal fractures (22.0 vs. 5 %, p < 0.0001). In particular, entrapments of the posterior tibial and flexor digitorum longus were more common in pilon fractures than in calcaneal fractures (21 vs. 0.1 % and 9 vs. 0.1 %, p < 0.0001 and p = 0.0006, respectively). Calcaneal fractures were more frequently associated with peroneal retinacular injury than pilon fractures (18 vs. 4 %, p = 0.0014). Additionally, entrapment of the flexor hallucis longus was more common in calcaneus fractures than in pilon fractures (4 vs. 2 %), and 82 % of the flexor hallucis longus entrapments retrospectively identified occurred in calcaneus fractures, however this did not reach statistical significance (p = 0.3). 3 (21 %) posterior tibial or flexor digitorum longus and 1 (7 %) flexor hallucis longus entrapments occurred in patients who sustained ipsilateral calcaneus and pilon fractures.
Pilon fractures classified in a multifragmentary subgroup, including Ruedi and Allgower type III or AO-OTA types B3, C2, and C3 were much more likely to be associated with posteromedial tendon entrapment compared to simple fracture patterns (p < 0.0001 and p = 0.0005, respectively) (Table 3). Only one patient with a Ruedi and Allgower type 1 and AO-OTA type C1 fracture had an entrapped posterior tibial tendon, and this patient also had an ipsilateral calcaneal fracture with peroneal tendon dislocation. Pilon fractures classified in a multifragmentary subgroup were not statistically significantly associated with peroneal retinacular injury (p = 0.24).
Intraarticular calcaneal fractures classified in a multifragmentary subgroup, including Sanders type III or IV, were more likely to be associated with peroneal retinacular injury (38 vs. 22 %, p = 0.0473), as seen in Table 3, but not with posteromedial tendon entrapment (10 vs. 5 %, p = 0.16). The vast majority of peroneal retinacular injuries were tendon subluxations and dislocations. However, one peroneal tendon was entrapped in a Sanders type 3AB fracture in a patient with a contralateral extraarticular calcaneal body fracture and Ruedi and Allgower type 2 and AO-OTA type B2 pilon fracture (Fig. 3). One of the Sanders type IV fractures was positive for entrapment of the posterior tibial, flexor digitorum longus, and flexor hallucis longus tendons.
There were 73 extraarticular calcaneal fractures not involving the posterior subtalar joint, involving only the anterior process, body, or posterior tubercle, five of which were in patients who sustained an ipsilateral pilon fracture. These were not included in the Sanders classification data analysis. Only four of these patients with extraarticular calcaneal fractures (5 %) were positive, indicating that tendon injury in extraarticular calcaneal fractures is unusual.
Avulsion fractures of the superior peroneal retinaculum, causing a “fleck sign,” (Fig. 1) were seen in eight calcaneal fractures. The fleck sign was present in four of 35 (11 %) calcaneal fractures with peroneal tendon subluxation/dislocation, and in four of 158 (3 %) calcaneal fractures without peroneal tendon subluxation/dislocation (p = 0.047, Fisher’s exact). One pilon fracture demonstrated a positive fleck sign without peroneal tendon subluxation/dislocation. Whether or not associated with peroneal tendon subluxation/dislocation, the fleck sign was considered a sign of injury to the peroneal retinaculum.
The tibial neurovascular bundle was entrapped in one multifragmentary pilon fracture with concomitant entrapment of the posterior tibial, flexor digitorum longus, and flexor hallucis longus tendons. The deep peroneal nerve was entrapped in one multifragmentary pilon fracture (Fig. 4). One multifragmentary pilon fracture lacerated both the posterior tibial tendon and the flexor digitorum longus tendon in a patient with a contralateral calcaneal fracture, and one multifragmentary pilon fracture lacerated only the posterior tibial tendon in a patient with an ipsilateral calcaneal fracture (Fig. 5).
Axial CT image of a 40-year-old male who was involved in a motorcycle collision who sustained a Ruedi and Allgower type 2/AO-OTA type C2 pilon fracture as well as ipsilateral extraarticular calcaneal fracture with laceration of the posterior tibial tendon. Superior image (a) reveals an intact posterior tibial tendon (arrow). Image at the level of the metaphyseal comminution (b) reveals a gap corresponding to the lacerated tendon (arrow). Image inferiorly at the tibial plafond (c) reveals the presence of the distal posterior tibial tendon (arrow). CT coronal reformat (d) depicts the lacerated tendon edges. Relatively low attenuation of the posterior tibial tendon likely correlates to intrasubstance edema
There were 121 of 312 fractures that underwent open reduction and internal fixation, all of which had available operative notes in the electronic medical record. Intra-operative findings of soft tissue entrapments or dislocations were documented in three patients, none of which were identified in the initial radiology CT report. One patient’s superficial peroneal nerve was entrapped in a multifragmentary pilon fracture, but this was not identifiable even on retrospective imaging review. In another patient, the tibial nerve and flexor hallucis longus were noted during surgery to be entrapped in a multifragmentary pilon fracture and were subsequently mobilized. Upon retrospective review of that CT scan, both the posterior tibial and flexor digitorum longus tendons were entrapped, but the tibial nerve and flexor hallucis longus did not appear entrapped. The multifragmentary pilon fracture of the third patient lacerated the posterior tibial and flexor digitorum tendons. The tendon lacerations were identified retrospectively on CT scan but were not repaired due to the extent of the patient’s soft tissue injuries.
A total of 99 posteromedial tendon entrapments or lacerations or injuries to the superior peroneal retinaculum were retrospectively identified. Among all radiologists at our institution, 39 (39 %) of these injuries were prospectively identified, 85 % of which were identified by musculoskeletal radiologists. Musculoskeletal radiologists originally identified 33 of 48 (69 %) tendon entrapments or retinacular injuries, and radiologists with alternative sub-specialization originally identified six of 51 (12 %)(p < 0.0001, Table 4). Seven patients with a total of eight fractures underwent repeat CT scans, which were interpreted by musculoskeletal radiologists. Nine of ten positive findings, including four peroneal tendon dislocations and five entrapped posteromedial tendons, were subsequently identified, however were not included in the statistical analysis, as only the patient’s first CT was considered in the statistical analysis.
Discussion
Peroneal retinacular injury has been reported in 28-92 % of calcaneal fractures, and includes lateral subluxation, dislocation, and entrapment [13, 15]. Although CT scan may be obtained for surgical planning, these soft tissue injuries may go undetected and potentially lead to chronic or stenosing tenosynovitis and subsequent pain and instability [3, 13, 15]. The peroneus longus and brevis muscles primarily pronate and evert the foot, contributing to stability during ambulation. Their tendons reside in the fibular groove posteriorly and course distally along the lateral wall of the calcaneus, held in place by the superior and inferior peroneal retinacula [13]. While the subluxated or dislocated tendons may reduce upon calcaneal fracture reduction, other times the retinaculum must be repaired to maintain the peroneal tendons in their anatomic location [6]. Historically, contrast-enhanced tenography was performed in patients who experienced persistent lateral ankle pain and instability after sustaining calcaneal fractures [20], however current CT techniques provide the necessary contrast and spatial resolution to prospectively identify peroneal retinacular injuries concomitantly with fracture description and classification [3, 13, 15].
Ho et al. (2001) described a method to determine whether the peroneal tendons are dislocated by finding their normal position within a triangle bounded by the lateral malleolus, the superior peroneal retinaculum, and the calcaneofibular ligament [3]. We refer to peroneal retinacular injury as disruption of the superior peroneal retinaculum causing subluxation/dislocation of the peroneal tendon, which we defined as the lateral margin of the peroneal tendons protruding from the lateral edge of the lateral malleolus. Additionally, we retrospectively found one case of peroneal tendon entrapment, which has been described in cases of lateral wall blowout which increases the calcaneal width, which we also combined into our peroneal retinacular injury category [5, 6, 10, 13, 15].
At our institution, 35 (18 %) peroneal retinacular injuries were retrospectively identified in 193 calcaneal fractures, 66 % of which were identified in the original radiology report, 87 % by musculoskeletal radiologists. This is significantly higher than that reported by Toussaint et al. (2014), who noted only 10.2 % of which were correctly prospectively identified [15].
A small fibular bony avulsion of the superior peroneal retinaculum, the “fleck sign,” has also been described to be associated with peroneal tendon pathology [8, 15]. We retrospectively identified eight positive fleck signs including seven in intraarticular calcaneal fractures and one in a type B extraarticular calcaneal fracture, out of a total of 207 calcaneal fractures. This rate is lower than Toussaint et al. (2014), who identified the fleck sign in 10.5 % of their calcaneal fractures. They also found that the “fleck sign” was strongly associated with peroneal retinacular injury (p < 0.001) [15]. Only four of the fleck signs identified in our study were associated with peroneal tendon subluxation or dislocation, however it is certainly possible that the peroneal tendons could subluxate or dislocate upon dynamic maneuvers in those patients with a positive fleck sign whose peroneal tendons are anatomically positioned at rest during the static CT scan.
Intraarticular fractures of the tibial plafond are typically high-energy injuries whose outcomes are directly related to anatomic joint reconstruction and stabilization, and Ruedi and Allgower type III fractures have been documented to have worse clinical outcomes than type I or type II [21]. Additionally, the inability to achieve an anatomic reduction may lead to chondral damage, and bony spicules may cause damage to the skin or tendons [22]. Many authors have described possible causes of the inability to reduce pilon fractures. Tendons including the posterior tibial may interpose between the medial edge of the Volkmann (posterolateral) major fracture fragment and the posterior edge of the medial malleolar fragment [1, 23]. The posterior tibial tendon has also been described to displace posterolaterally and then anteriorly through the disrupted syndesmosis, ultimately residing in the tibiotalar joint space (Fig. 6) [22].
A 32-year-old male who slipped and fell from standing, and was involved in a motor vehicle collision on the way to the hospital, sustained a Ruedi and Allgower type 3/AO-OTA type C3 pilon fracture. Axial CT images at the level of the fracture (a) reveal entrapment of the posterior tibial tendon (solid arrow) and the flexor digitorum longus tendon (dotted arrow) within bony fragments. Axial CT image inferiorly (b) reveals the posterior tibial tendon to reside within the tibiotalar joint (solid arrow). Coronal reformat (c) demonstrates the entrapped tendons (solid arrow), with better resolution on sagittal reformats (d, e, f) of the posterior tibial (solid arrow) and flexor digitorum longus tendons (dotted arrow)
At our institution, posteromedial tendon injuries were retrospectively identified in 20 of 91 (22 %) of pilon fractures. Twenty-seven percent of posteromedial tendon injuries were identified in the original radiology report, 81 % of which were identified by musculoskeletal radiologists. This is compatible with the retrospective review of 420 CT scans with pilon fractures by Eastman et al. (2013), who noted 20 % of posteromedial soft tissue entrapments were correctly prospectively identified [1].
We observed 14 patients with ipsilateral both calcaneal and pilon fractures. These patients were considered as a third group since it is unclear to which fracture a tendon entrapment or peroneal retinacular injury should be attributed. Seven of these patients had injury to the peroneal retinaculum, and four sustained entrapment or laceration of the posteromedial tendons. No association of a specific injury to ipsilateral calcaneal and pilon was identified, however these patients with multiple fractures were associated with overall tendon entrapment or peroneal retinacular injury.
We hypothesized that multifragmentary injuries tend to be of higher energy, which would be associated with a greater frequency of tendon entrapments. Accordingly, we combined Ruedi and Allgower types I and II into one category (n = 35) and type III into the multifragmentary category (n = 56). Likewise, we combined the AO-OTA types B1, B2, and C1 into one category (n = 26) and types B3, C2, and C3 into the multifragmentary category (n = 65). The subject number discrepancy between the Ruedi and Allgower and the AO-OTA categorizations arises since the AO-OTA type C2 (currently categorized as multifragmentary due to the characteristic metaphyseal comminution) shares the Ruedi and Allgower type 2 classification characteristic of a displaced articular surface without articular comminution. Multifragmentary classification was significantly associated with entrapment or laceration of the posteromedial tendons and neurovascular structures, for both the Ruedi and Allgower as well as the AO-OTA classifications (p < 0.0001 and p = 0.0003, respectively). Pilon fractures classified in a multifragmentary subgroup, including Ruedi and Allgower type III or AO-OTA types B3, C2, and C3 were not statistically significantly associated with peroneal retinacular injury. Similarly, multifragmentary intraarticular Sanders types III and IV were associated with injury to the superficial peroneal retinaculum with or without peroneal tendon subluxation/dislocation (p = 0.0473), however these fractures were not associated with posteromedial tendon injuries.
Only one patient with a Ruedi and Allgower type 1 and AO-OTA type C1 fracture had an entrapped posterior tibial tendon, and this patient also had an ipsilateral calcaneal fracture with a peroneal tendon dislocation. Despite the non-multifragmentary category, this remains compatible with our statistically significant association between the incidence of tendon injury and the presence of multiple fractures in the same patient (p = 0.002), which is presumably due to a higher energy injury.
We also identified a statistically significant trend among the three posteromedial tendons. Posterior tibial and flexor digitorum longus injuries were associated with pilon fractures. There was a trend of flexor hallucis longus injuries with calcaneal fractures. When the anatomic course of the flexor hallucis longus beneath the sustentaculum tali is considered, it is not surprising that this posteromedial tendon could be most associated with calcaneal fractures, although statistical significance was not achieved in our study. One patient with a calcaneal fracture and entrapment of the flexor hallucis longus tendon was treated non-operatively, and follow-up radiograph demonstrated lack of bony healing (Fig. 7).
A 58-year-old male sustained a Sanders type 2C calcaneal fracture from a fall into a shallow hole. Axial (a), sagittal (b), and coronal (c) CT images reveal entrapment of the flexor hallucis longus tendon (arrow) between bony fragments. One year later, lateral plain radiograph of the foot (d) reveals nonunion of the calcaneal fracture (arrow)
Entrapments of the posteromedial tendons and peroneal retinacular injuries may be clinically missed due to the presence of extensive soft tissue edema and inability to evaluate the integrity of the tendons on physical exam due to pain [15]. It is essential for the radiologist to pre-operatively identify such an injury, as it may require a modified surgical approach to treat both the fracture and a potential soft tissue injury [1]. Toussaint et al. (2014) commented that tendon injuries were more than six times more likely to have been treated if they were prospectively identified in the original CT report [15]. In our experience, only three patients were clinically documented to have tendon or neurovascular injuries intraoperatively, none of which were identified in the initial radiology CT report, and one of which was not retrospectively identified either. Unfortunately, this does introduce a significant limitation into our study. Ideally, we would consider surgical identification as the gold standard by which we would gauge our radiological accuracy. However, orthopedic surgical operative reports are not standardized and it is unclear if these retrospectively identified tendon entrapments and dislocations were truly not identified intraoperatively or if they were identified but not documented. We did not find a statistically significant association between the presence of tendon injuries and whether closed reduction and splinting had been performed prior to CT scan. Nevertheless, it is possible that the dislocated or entrapped tendons reduced after the CT scan and prior to operative intervention. Crim et al. (2013) speculated that their one tendon false negative CT interpretation was likely due to displacement of the tendon between the time of CT and surgery [14], and it is feasible that the contrary is true, that instead reduction may occur in the interim.
Other limitations of our study include a retrospective design, for which 8.1 % of records were excluded due to lack of available CT images. It is unknown how the distribution of fracture classification and presence of tendon injuries in these cases could have altered our results. Furthermore, while we standardized and quantified our definitions of tendon entrapment and subluxation/dislocation, these remain subjective findings. An analysis of interobserver variability was not performed, as the classification and identification of positive soft tissue findings was by consensus agreement. Although there is a large discrepancy in experience between readers, both expressed confidence in the data without the need for an arbitrator.
It is clear that multifragmentary calcaneal fractures are associated with peroneal retinacular injury and that multifragmentary pilon fractures are associated with posteromedial soft tissue injury, most of which remain prospectively undetected even at a high-volume level 1 trauma center. Further research is necessary to determine if awareness of these associated injuries increases detection pre-operatively and improves patient outcomes.
Conclusions
Multifragmentary pilon and calcaneal fractures are often associated with posteromedial tendon and peroneal retinacular injuries, respectively. While musculoskeletal sub-specialty was associated with increased recognition, all radiologists should be especially aware of the possibility for tendon injury in patients with ankle fractures sustained due to a high-energy axial load mechanism.
References
Eastman JG, Firoozabadi R, Benirschke SK, Barei DP, Dunbar RP. Entrapped posteromedial structures in pilon fractures. J Orthop Trauma. 2013.
Rak V, Ira D, Masek M. Operative treatment of intra-articular calcaneal fractures with calcaneal plates and its complications. Ind J Orthop. 2009;43(3):271–80.
Ho RT, Smith D, Escobedo E. Peroneal tendon dislocation: CT diagnosis and clinical importance. AJR Am J Roentgenol. 2001;177(5):1193.
Ehrlichman LK, Toussaint RJ, Kwon JY. Surgical relocation of peroneal tendon dislocation with calcaneal open reduction and internal fixation: technique tip. Foot Ankle Int. 2014.
Mak MF, Tay GT, Stern R, Assal M. Dual-incision approach for repair of peroneal tendon dislocation associated with fractures of the calcaneus. Orthopedics. 2014;37(2):96–100.
Ebraheim NA, Elgafy H, Sabry FF, Tao S. Calcaneus fractures with subluxation of the posterior facet. A surgical indication. Clin Orthop Relat Res. 2000;377:210–6.
Wright DG, Sangeorzan BJ. Calcaneal fracture with peroneal impingement and tendon dysfunction. Foot Ankle Int. 1996;17(10):650.
Ebraheim NA, Zeiss J, Skie MC, Jackson WT. Radiological evaluation of peroneal tendon pathology associated with calcaneal fractures. J Orthop Trauma. 1991;5(3):365–9.
Rosenberg ZS, Feldman F, Singson RD. Intra-articular calcaneal fractures: computed tomographic analysis. Skelet Radiol. 1987;16(2):105–13.
Guyer BH, Levinsohn EM, Fredrickson BE, Bailey GL, Formikell M. Computed tomography of calcaneal fractures: anatomy, pathology, dosimetry, and clinical relevance. AJR Am J Roentgenol. 1985;145(5):911–9.
Bradley SA, Davies AM. Computed tomographic assessment of old calcaneal fractures. Br J Radiol. 1990;63(756):926–33.
Jarvis HC, Cannada LK. Acute tibialis posterior tendon rupture associated with a distal tibial fracture. Orthopedics. 2012;35(4):e595–7.
Rosenberg ZS, Feldman F, Singson RD, Price GJ. Peroneal tendon injury associated with calcaneal fractures: CT findings. AJR Am J Roentgenol. 1987;149(1):125–9.
Crim J, Enslow M, Smith J. CT assessment of the prevalence of retinacular injuries associated with hindfoot fractures. Skelet Radiol. 2013;42(4):487–92.
Toussaint RJ, Lin D, Ehrlichman LK, Ellington JK, Strasser N, Kwon JY. Peroneal tendon displacement accompanying intra-articular calcaneal fractures. J Bone Joint Surg Am. 2014;96(4):310–5.
Coonrad RW, Bugg Jr EI. Trapping of the posterior tibial tendon and interposition of soft tissue in severe fractures about the ankle joint. J Bone Joint Surg Am. 1954;36-A(4):744–50.
Ermis MN, Yagmurlu MF, Kilinc AS, Karakas ES. Irreducible fracture dislocation of the ankle caused by tibialis posterior tendon interposition. J Foot Ankle Surg. 2010;49(2):166–71.
Pankovich AM. Fracture-dislocation of the ankle. Trapping of the postero-medical ankle tendons and neurovascular bundle in the tibiofibular interosseous space: a case report. J Trauma. 1976;16(11):927–9.
Topliss CJ, Jackson M, Atkins RM. Anatomy of pilon fractures of the distal tibia. J Bone Joint Surg Br Vol. 2005;87(5):692–7.
Resnick D, Goergen TG. Peroneal tenography in previous calcaneal fractures. Radiology. 1975;115(1):211–3.
Chen SH, Wu PH, Lee YS. Long-term results of pilon fractures. Arch Orthop Trauma Surg. 2007;127(1):55–60.
Henry PDG, McKee MD. Irreducible tibial pilon fracture secondary to posterior tibial tendon entrapment. J Bone Joint Surg Case Connect. 2012;2(4), e69.
Parrish TF. Fracture-dislocation of the ankle; an unusual cause of failure of reduction; a case report. J Bone Joint Surg Am. 1959;41-A(4):749–51.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
The authors declare that they have no conflicts of interest. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional review board. This research has been approved by the IRB.
Appendices
Appendix 1
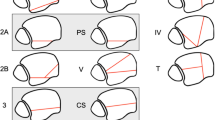
Ruedi and Allgower classification of pilon fractures. Type 1 (left) are cleavage fractures without displacement at the articular surface. Type 2 (middle) are fractures displaced at the articular surface without comminution. Type 3 (right) are impacted and comminuted fractures involving the articular surface. (Reproduced with permission from Ruedi, T.P., and Allgower, M. (1979). “The operative treatment of intra-articular fractures of the lower end of the tibia.” Clinical Orthpaedics and Related Research, 138, pg 105–110.)
Appendix 2
AO/OTA Fracture and Dislocation Classification. 43 is the anatomic category for the distal tibia. Type A (left) are extraarticular. Type B (middle) demonstrate continuity of the metaphysis with the articular surface with pure split (B1), split-depression (B2), and multifragmentary depression (B3). Type C (right) are characterized by fracture lines which completely separate the metaphysis from the articular surface, with simple articular and metaphyseal components (C1), simple articular component but multifragmentary metaphyseal component (C2), and multifragmentary articular components (C3). (Reproduced with permission, copyright by AO Foundation, Switzerland.)
Appendix 3
Sanders classification of intraarticular calcaneal fractures. The coronal oblique reconstruction through the widest portion of the posterior subtalar joint is utilized. Type 1 is nondisplaced. Type 2 has a single fracture line with at least 2 mm of displacement, with “2A,” “2B”, and “2C” subdivisions according to the fracture line position at the subtalar facet from lateral to medial. Type 3 has two fracture lines with at least 2 mm of displacement, with “3AB,” “3AC,” and “3BC” subdivisions according to the fracture line positions. Type 4 has three or more fracture lines displaced by at least 2 mm through the posterior subtalar facet. (Case courtesy of Dr. Matt Skalski, adapted with permission, Radiopaedia.org)
Appendix 4
Pilon major fracture fragments. CT scans of pilon fractures showing the major fracture fragments: anterior (A), posterior (P), medial (M), anterolateral (AL), posterolateral (PL), and die-punch (DP). (Reproduced with permission and copyright © of the British Editorial Society of Bone and Joint Surgery, Topliss, C.J., Jackson, M., and Atkins, R.M. (2005). “Anatomy of pilon fractures of the distal tibia.” Journal of Bone and Joint Surgery (Br), 87(5), pg 692–697.)
Rights and permissions
About this article
Cite this article
Tresley, J., Subhawong, T.K., Singer, A.D. et al. Incidence of tendon entrapment and dislocation with calcaneus and pilon fractures on CT examination. Skeletal Radiol 45, 977–988 (2016). https://doi.org/10.1007/s00256-016-2380-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00256-016-2380-0