Abstract
Objectives
The objective of this study was to investigate the common sites of subchondral insufficiency fractures of the femoral head (SIF) based on three-dimensional (3-D) reconstruction of MR images.
Materials and methods
In 33 hips of 31 consecutive patients diagnosed with SIF, 3-D reconstruction of the bone, fracture, and acetabular edge was performed using MR images. These 3-D images were used to measure the fractured areas and clarify the positional relationship between the fracture and degree of acetabular coverage.
Results
The fractured area in the anterior portion was significantly larger than in the posterior area. In 11 cases, the fractures contacted the acetabular edge and were distributed on the lateral portion. The indices of acetabular coverage (center-edge angle and acetabular head index) in these cases were less than the normal range. In the remaining 22 cases, the fractures were apart from the acetabular edge and distributed on the mediolateral centerline of the femoral head. The majority of these cases had normal acetabular coverage.
Conclusions
The common site of SIF is the anterior portion. In addition, two types of SIF are proposed: (1) Lateral type: the contact stress between the acetabular edge and lateral portion of the femoral head causes SIF based on the insufficient acetabular coverage, and (2) Central type: the contact stress between the acetabular surface and the mediolateral center of the femoral head causes SIF independent from the insufficiency of acetabular coverage. These findings may be useful for considering the treatment and prevention of SIF.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Subchondral insufficiency fracture of the femoral head (SIF) has been observed in elderly females with osteoporosis [1–3]. In general, most patients tend to show unilateral involvement [1, 4–6], and affected patients typically complain of acute hip pain without any obvious antecedent trauma.
Radiologically, subchondral fractures are primarily observed in the superior portion of the femoral head [4, 5, 7]. T1-weighted magnetic resonance (MR) images reveal low-intensity bands in the subchondral area of the femoral head, which tend to be irregular, disconnected, and convex to the articular surface [3, 5, 8]. These low-intensity bands in SIF have been histologically proven to correspond with the fracture line of the associated repair tissue [4, 9]. The low-intensity band is surrounded by a bone marrow edema pattern (BME), and BME is observed as a homogenous and ill-delimited low signal intensity area on T1-weighted MR images and high signal intensity on T2-weighted MR images [10].
Previous reports have focused on the characteristics of imaging findings, prognostic factors, and treatments for SIF. However, some important issues remain poorly understood. First, the mechanism of SIF is not clear. Ishihara et al. reported that the occurrence of SIF is associated with insufficient acetabular coverage [11]. However, in our experience, many patients who have no findings of insufficient acetabular coverage develop SIF. Second, there are no previous reports clarifying the common site of SIF, which may be useful for determining the mechanism as well as the treatment and prevention of SIF. The current study investigated common sites for SIF based on three-dimensional (3-D) reconstruction of MR images and evaluated the mechanism of SIF.
Materials and methods
Patients
The present retrospective study was approved by the institutional review board. We retrospectively reviewed 31 consecutive patients in whom DICOM formatted MR images were available, with 33 hips diagnosed with SIF between June 2007 and April 2014 at our institution. There were 11 male and 20 female patients, ranging from 23 to 88 years of age (mean age, 59.1 ± 17.4 years old). Patients with a history of surgery, trauma, infection of the hip joint, osteonecrosis of the femoral head or Perthes disease were excluded. Of the 31 patients, two had a known diagnosis of osteoporosis, four had a history of treatment with corticosteroid therapy (systemic lupus erythematosus, liver transplantation, asthma, and urticaria) and two had colon cancer.
The diagnosis of SIF was made based on the following published criteria [5, 7, 9]: (1) hip pain that began without any apparent history of trauma; (2) radiograph findings that were normal or showed collapse of the femoral head, joint space narrowing and/or linear patchy sclerotic areas in the superior portion of the femoral head; (3) a bone marrow edema pattern in the femoral head and/or neck on MR images; and (4) a subchondral low signal intensity band on T1-weighted MR images that was serpiginous, or paralleled the articular surface. In five cases, gadolinium-enhanced MR imaging was performed to differentiate SIF from osteonecrosis of the femoral head. On enhanced MRI, both the low signal intensity band and the proximal portion tended to show a high intensity in SIF, while this portion was not enhanced in osteonecrosis [7, 12].
All patients were initially managed by conservative treatment, which consisted of rest and the avoidance of weight-bearing activities for 6–8 weeks. Both a clinical assessment and follow-up radiographs were obtained at 1, 2, 4, 6, and 12 months in all patients, at which time the progression of collapse was evaluated. If the progression of collapse was noted, then surgical treatment was indicated. In the patients who did not receive surgery, follow-up MR images were obtained at approximately 6 or 12 months following the first visit.
MR image findings
The patients underwent examinations using a 1.5-T MR system or 3.0-T MR system. The T1-weighted MR images (repetition time/echo time [TR/TE] = 400-675/8-19 ms, field of view = 35–68 cm, matrix = 220–512 × 256–512, slice thickness = 3–5 mm) in the coronal planes were available for all patients. The hip position was neutral during the MRI scan, namely flexion, extension, abduction, adduction, internal rotation, and external rotation were each zero degrees. All hips showed a low-intensity band in T1-weighted MR images, which tended to be irregular, disconnected, and convex to the articular surface.
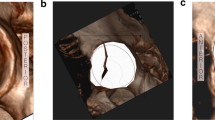
Visualization of the fracture distribution
To visualize the fractured area, three-dimensional (3-D) reconstruction of MR images was performed. MR image data formatted in the DICOM format were necessary for the following 3-D reconstruction. Two subspecialized hip orthopedic surgeons with seven and 13 years of experience reviewed the MR images and arrived at a consensus regarding the fractured area. T1-weighted MR images on coronal slices were selected to reconstruct 3-D images of the proximal portion of the femur and fracture using the methods described below. To clarify the positional relationship between the fracture and acetabular edge, the three-dimensionally reconstructed acetabular edge was superimposed on the bone and fracture (Fig. 1).
a T1-weighted MR image of the right hip of a 47-year-old male patient shows a low signal intensity band (arrows). b An outline of the proximal portion of the femur is traced (green line). These tracings are performed in all slices. c An outline of the fracture is traced (red line). These tracings are performed in all slices in which the fracture lines are obvious. The acetabular edge was marked with a dot (yellow circle). d The proximal portion of the femur (green) and fracture (red) are three-dimensionally reconstructed (anterior view). e The superior view was obtained from the anterior view with 90 degrees of rotation. f The acetabular edge is superimposed
-
1.
All T1-weighted MR images on coronal slice were opened using an image analysis software program, Amira version 5.4.1 (Visage imaging Inc. Melbourne, Australia)
-
2.
Outlines of the proximal portion of the femur were traced on all slices.
-
3.
Outlines of the subchondral fracture were traced on the slices that showed the fracture.
-
4.
The acetabular edge was marked with a dot.
-
5.
The proximal portion of the femur and fracture were three-dimensionally reconstructed.
-
6.
The three-dimensionally reconstructed acetabular edge was superimposed.
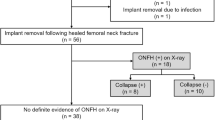
Measurement of the fractured area
To measure the fractured area, the superior view of the three-dimensionally reconstructed images was used. In this view, the femoral head was assumed to be a circle. The circle was divided into four regions: anteromedial (AM), anterolateral (AL), posteromedial (PM) and posterolateral (PL). The method considered the whole fractured area to be 100 %, and the fractured area in each region (AM, AL, PM, and PM) was calculated as a percentage of the whole fractured area (Fig. 2a). The above measurement of the fractured area was performed using the ImageJ 1.45S software package (National Institutes of Health, USA).
a Method for measuring the fractured area: A circle, which indicates the femoral head on the superior view, is divided into four regions and the fracture is traced. The whole fractured area is considered to be 100 %. In this case, the fractured area in the anteromedial (AM) region was 23.0 %, while that in the anterolateral (AL) region was 39.3 %, that in the posteromedial (PM) region was 26.2 % and that in the posterolateral (PL) region was 11.5 %. b Method for measuring the coverage rate: A circle, which indicates the femoral head in the superior view. The area covered by the acetabulum is measured (portion shaded by blue line). The area of the circle is considered to be 100 %. In this case, the coverage rate is 82.6 %. c The measurements of acetabular coverage. (1) = A horizontal line between the pelvis teardrops, (2) = A line between the lateral edge of the acetabular roof and the femoral head center. CEA Center edge angle, AHI Acetabular head index
Measurements of acetabular coverage
Before the measurements, we confirmed that there was no femoro-acetabular impingement. The percentage of acetabular coverage was measured using the three-dimensionally reconstructed images. In the superior view, the femoral head was assumed to be a circle, considered to be 100 %. The femoral head area covered by the acetabular region was calculated as a percentage of the circle (Fig. 2b) [13].
The following radiographic measurements of acetabular coverage were obtained: the center edge angle (CEA) [14] and acetabular head index (AHI) [15]. The original measurements were obtained using AP radiographs; however, we performed these assessments on coronal slice MR images (Fig. 2c) since MR image measurements are considered to be more accurate than radiograph measurements. According to the published criteria, a CEA of more than 27° was classified as normal, a CEA between 20 and 27° was classified as insufficient coverage and a CEA less than 20° was classified as dysplasia. An AHI more than 80 % was classified as normal, an AHI between 70 and 80 % was classified as insufficient coverage and an AHI less than 70 % was classified as dysplasia.
Positional relationship between the fracture, acetabular edge, and site of SIF occurrence
To clarify the positional relationship between the fracture and degree of acetabular coverage, whether the acetabular edge contacts the fractured area was evaluated using the superior view of the three-dimensionally reconstructed images. In addition, the site of SIF occurrence was classified as being in the lateral, central, or medial portion of the femoral head.
Statistical analysis
The statistical analyses of the fractured area were performed using the Student’s paired t test. The age, CEA, AHI, and coverage rates were analyzed using Student’s unpaired t test. Gender and the prognosis were analyzed using the Chi-square test. Differences with p values of less than 0.05 were considered to be statistically significant. The cut-off points for these radiographic variables were calculated using receiver operating characteristic (ROC) curves. In the ROC curves, the area under the curve (AUC) was used to test useful prognostic factors, in which an area of 1 represented a perfect test and an area of 0.5 represented a worthless test. A Kaplan–Meier analysis was performed and survival curves were created using the log-rank test. Spearman’s rank correlation coefficient was performed to assess correlations among the values of acetabular coverage. All of the statistical analyses were performed using the JMP software program, version 9.0.1 (SAS Institute Inc. Cary, NC, USA).
Results
Patients
Twenty-three hips resolved after the conservative treatment consisting of rest and the avoidance of weight-bearing activities (6–8 weeks), while ten hips required surgical treatment due to progression of femoral head collapse (hip arthroplasty: seven cases and transtrochanteric anterior rotational osteotomy: three cases). Two patients with bilateral SIF were included. They were relatively young male patients (23 and 47 years of age) without any appreciable past history.
Fractured area
The fractured areas were three-dimensionally reconstructed for 33 hips in 31 patients. The results of the measurements of the fractured areas are shown in Fig. 3. The fractured area in the AM region (mean ± standard deviation: 32.5 ± 27.6 %, ranging from 0 to 100 %) was significantly larger than that in the PM region (12.1 ± 12.0 %, ranging from 0 to 48.9 %), and the measurements of the fractured area in the AL region (36.8 ± 21.9 %, ranging from 0 to 93.5 %) was significantly larger than that in the PL region (18.6 ± 19.3 %, ranging from 0 to 64.8 %). The mean fractured areas in the AL and PL regions were larger than those in the AM and PM regions, respectively; however, the differences were not significant. In five hips, the fractures were distributed to only the anterior portion of the femoral head. In 22 hips, the fractures were distributed more widely to the anterior portion than the posterior portion. In six hips, the fracture areas were slightly wider in the posterior portion than in the anterior portion (Fig. 4).
Visualization of the fracture distribution. a The right hip of a 53-year-old male patient: The fractured area distributes to only the anterior portion of the right femoral head. b A 47-year-old male patient (a bilateral case): In both femoral heads, the fractured areas distribute more widely to the anterior portion than the posterior portion. c The right hip of a 77-year-old female patient: The fractured area is slightly wider to the posterior portion than the anterior portion
Acetabular coverage
The mean CEA was 29.3 ± 7.9°, ranging from 12.5 to 45.0° and the mean AHI was 79.9 ± 6.9 %, ranging from 63.8 to 93.6 %. Approximately half of the hips (CEA: 17 and AHI: 14) were in the normal range, while some hips (CEA: 5 and AHI: 4) were diagnosed as exhibiting dysplasia. Four hips of these hips with dysplasia required surgical treatment due to the progression of femoral head collapse. The mean coverage rate obtained using the 3D MR images was 74.7 ± 11.6 % (ranging from 47.0 to 94.5 %), which had a high correlation with CEA (r = 0.6539, p < 0.0001) and AHI (r = 0.6692, p < 0.0001).
Site of SIF
As to the positional relationship between the acetabular edge and the fracture, the acetabular edges contacted the fracture in 11 hips and were apart from the fracture in 22 hips (Fig. 5). The site of SIF occurrence in these 11 hips was the lateral portion of the femoral head, while the site of SIF occurrence in all 22 hips was the central portion of the femoral head. The results for the acetabular coverage indices (CEA and AHI), site of SIF occurrence and contact of the acetabular edge are shown in Tables 1 and 2. All 11 hips in which the fractured areas contacted the acetabular edge had lower indices of acetabular coverage (CEA and AHI) than the normal limits. The majority of the 22 hips in which the fractured areas were apart from the acetabular edge had normal indices of acetabular coverage (CEA: 17 hips and AHI: 14 hips).
a The left hip of a 62-year-old female patient: T1-weighted MR image (TR = 413 ms, TE = 11 ms) shows a low signal intensity band (arrows). The band contacts the acetabular edge (arrowhead). This patient has dysplasia (CEA = 12.5° and AHI = 66.3 %). b The three-dimensionally reconstructed image in the same patient shows clearly that the acetabular edge (yellow) contacts the fracture (red). The site of SIF occurrence is in the lateral portion of the femoral head. c The right hip of a 64-year-old female patient: T1-weighted MR image (TR = 500 ms, TE = 15 ms) shows a low signal intensity band (arrows). The band is apart from the acetabular edge (arrowhead). The acetabular indices of this case are in the normal range (CEA = 30.0° and AHI = 81.4 %). d The three-dimensionally reconstructed image in the same patient shows clearly that the acetabular edge (yellow) is apart from the fracture (red). The site of SIF occurrence is in the central portion of the femoral head
Type classification
From the results of the three-dimensionally reconstructed fractures and acetabular edges, we classified SIF into two types (Fig. 5): (1) Lateral type: The fracture contacts the acetabular edge. The fractured area is distributed on the lateral portion of the femoral head; (2) Central type: The fracture is apart from the acetabular edge. The fractured area is distributed on the central portion of the femoral head. The characteristics of both types are shown in Table 3. The differences of gender and the mean age were not significant. The lateral type was more likely to need surgical treatment due to progression of femoral head collapse. Both hips in one of the two bilateral patients (23 years of age) were classified as the lateral type, while both hips in the other bilateral patient (47 years of age) were classified as the central type.
The receiver operating characteristic (ROC) curves established the cut-off points for the CEA, AHI, and 3-D acetabular coverage (Table 4). In the ROC curve tests, all areas under the curves (AUCs) for CEA, AHI, and the coverage rate showed good results (>0.8). The Kaplan–Meier survivorship analysis using the log-rank test demonstrated significant differences between the two types (Fig. 6).
Discussion
In the present study, the 3-D reconstruction analysis demonstrated that SIF was distributed widely to the anterior portion of the femoral head rather than the posterior portion. Possible reasons for this characteristic location of SIF may include differences in the subchondral bone density of the femoral head and/or degree of mechanical stress between the anterosuperior portion and posterosuperior portion. Regarding the subchondral bone density, Wright et al. quantitatively characterized the distribution of subchondral bone density across the human femoral head using 3-D computed tomography [16]. In that report, the subchondral bone density was not significantly different between the anterosuperior and posterosuperior portion. That report indicates that the difference in the subchondral bone density is not the reason for the characteristic location of SIF. On the other hand, there are several reports describing that the extent of mechanical stress is higher in the anterosuperior portion than in the posterosuperior portion. Bachtar et al. reported that high stress sensitivity is concentrated in the anterosuperior portion when standing and walking, using a finite element analysis [17]. The anterosuperior portion of the femoral head suffers from a higher degree of contact stress than the posterior portion, especially in the hip flexed position. The reason why SIF generally localizes in the anterior portion may be related to the higher amount of contact stress on the anterior portion of the femoral head compared with the posterior portion.
Two kinds of mechanisms of SIF were inferred in this study. The first mechanism is that the contact between the acetabular edge and lateral portion of the femoral head causes SIF based on insufficient acetabular coverage, including cases of developmental dysplasia of the hip (DDH). Such cases accounted for 11 of the 33 SIF cases in the present study. Ishihara et al. reported that the occurrence of SIF is associated with insufficient acetabular coverage [11]. In patients with insufficient acetabular coverage, an excessive amount of stress is placed between the acetabular edge and superolateral portion of the femoral head, causing SIF. We classified such cases as the “lateral type.” Recently, insufficiency of the acetabular coverage was reported to be a poor prognostic factor for SIF [18]; thus, the lateral type of SIF is considered to have a worse prognosis than the other type. In the present study, the lateral type was likely to need surgical treatment due to progression of femoral head collapse after conservative treatment, compared with the central type.
The second mechanism is that the contact between the acetabular surface and mediolateral center of the femoral head causes SIF independently from the degree of insufficiency of acetabular coverage. Such cases accounted for 22 of our 33 SIF cases. The fractures in these cases were apart from the acetabular edge. The majority of such cases had normal acetabular coverage, although some cases may have slight insufficiency of acetabular coverage. We classified such cases as the “central type.” The central type has a better prognosis than the lateral type. In the current study, many cases of this type resolved after conservative treatment, which consisted of rest and the avoidance of weight-bearing activities for 6 to 8 weeks.
It is considered that SIF rarely develops from the medial portion of the femoral head since the contact stress on this area is much lower than that on the central and lateral portions [19]. In the present measurements, the mean fractured area in the lateral portion of the femoral head was larger than that in the medial part of the femoral head. However, the difference was not significant. This is because, as described earlier, the lateral type of SIF accounted for only 11 of the 33 cases. The majority of SIF cases were the central type, in which the medial and lateral fractured areas were not different.
Regarding treatments for SIF, conservative therapy, consisting of rest and the avoidance of weight-bearing activities, is the first choice of treatment for SIF. However, some SIF patients require surgical treatment due to progression of femoral head collapse in spite of conservative treatment [18]. Reported surgical treatments for SIF include hip arthroplasty and transtrochanteric anterior rotational osteotomy [18, 20]. Yamamoto et al. reported that transtrochanteric anterior rotational osteotomy was a good indication in five young SIF patients since the anterosuperior portion of the femoral head was mainly involved [20]. In both the lateral and central types in the present study, the majority of cases of SIF developed from the anterior or central portion of the femoral head and had a large intact area in the posterior portion of the femoral head. Therefore, ARO, which transposes the posterior intact area to a weight-bearing portion of the joint, seems to be a useful procedure in young patients with SIF who need surgical treatment.
In previous reports, the period of weight-bearing avoidance was 6–8 weeks regarding conservative therapy for SIF [1, 20]. We first applied such conservative therapy to all patients, and if the degree of collapse of the femoral head became severe (more than 2 mm), we considered operative treatment. However, the therapy may be possibly be changed according to the results of the present study. Regarding the central type, the period of weight-bearing avoidance should be shorter than 6–8 weeks. As to the lateral type, operative treatment should be considered earlier if the degree of femoral head collapse progresses.
The main limitation of this study is the small sample size. Because SIF is a rare fracture, in addition to the fact that MR images in DICOM format were necessary for the present study, further studies in large number of cases are needed. Second, in the present study, the fractured area was measured using the superior view of the three-dimensionally reconstructed images. Measurements of the fractured volume may be better than those of the fractured area. However, SIF is usually distributed to only the subchondral bone parallel to the articular surface. Therefore, the measurements of the fractured area in the present study are considered to be reasonable for evaluating the common site and mechanism of SIF.
Conclusions
In the present study, 3-D reconstruction of SIF using MR images demonstrated that common site of SIF is the anterior portion of the femoral head. In addition, two types of SIF were proposed based on the mechanism: (1) Lateral type: The contact between the acetabular edge and lateral portion of the femoral head causes SIF as a result of insufficient acetabular coverage; (2) Central type: The contact between the acetabular surface and mediolateral center of the femoral head causes SIF independently from the degree of insufficiency of acetabular coverage. The lateral type has a significantly poorer prognosis than the central type. These facts may be useful for considering the treatment as well as prevention of SIF.
References
Vande Berg BC, Malghem J, Goffin EJ, Duprez TP, Maldague BE. Transient epiphyseal lesions in renal transplant recipients: presumed insufficiency stress fractures. Radiology. 1994;191(2):403–7.
Bangil M, Soubrier M, Dubost JJ, Rami S, Carcanagues Y, Ristori JM, et al. Subchondral insufficiency fracture of the femoral head. Rev Rhum Engl Ed. 1996;63(11):859–61.
Rafii M, Mitnick H, Klug J, Firooznia H. Insufficiency fracture of the femoral head: MR imaging in three patients. AJR Am J Roentgenol. 1997;168(1):159–63.
Yamamoto T, Schneider R, Bullough PG. Subchondral insufficiency fracture of the femoral head: histopathologic correlation with MRI. Skelet Radiol. 2001;30(5):247–54.
Yamamoto T, Bullough PG. Subchondral insufficiency fracture of the femoral head: a differential diagnosis in acute onset of coxarthrosis in the elderly. Arthritis Rheum. 1999;42(12):2719–23.
Hagino H, Okano T, Teshima R, Nishi T, Yamamoto K. Insufficiency fracture of the femoral head in patients with severe osteoporosis--report of 2 cases. Acta Orthop Scand. 1999;70(1):87–9.
Miyanishi K, Hara T, Kaminomachi S, Maeda H, Watanabe H, Torisu T. Contrast-enhanced MR imaging of subchondral insufficiency fracture of the femoral head: a preliminary comparison with that of osteonecrosis of the femoral head. Arch Orthop Trauma Surg. 2009;129(5):583–9.
Vande Berg BC, Malghem JJ, Lecouvet FE, Jamart J, Maldague BE. Idiopathic bone marrow edema lesions of the femoral head: predictive value of MR imaging findings. Radiology. 1999;212(2):527–35.
Yamamoto T, Schneider R, Bullough PG. Insufficiency subchondral fracture of the femoral head. Am J Surg Pathol. 2000;24(3):464–8.
Vande Berg BC, Lecouvet FE, Koutaissoff S, Simoni P, Malghem J. Bone marrow edema of the femoral head and transient osteoporosis of the hip. Eur J Radiol. 2008;67(1):68–77.
Ishihara K, Miyanishi K, Ihara H, Jingushi S, Torisu T. Subchondral insufficiency fracture of the femoral head may be associated with hip dysplasia: a pilot study. Clin Orthop. 2010;468(5):1331–5.
Yamamoto T. Subchondral insufficiency fractures of the femoral head. Clin Orthop Surg. 2012;4(3):173–80.
Ito H, Matsuno T, Hirayama T, Tanino H, Yamanaka Y, Minami A. Three-dimensional computed tomography analysis of non-osteoarthritic adult acetabular dysplasia. Skelet Radiol. 2009;38(2):131–9.
Massie WK, Howorth MB. Congenital dislocation of the hip. Part I. Method of grading results. J Bone Joint Surg Am. 1950;32-A(3):519–31.
Heyman CH, Herndon CH. Legg–Perthes disease; a method for the measurement of the roentgenographic result. J Bone Joint Surg Am. 1950;32 A(4):767–78.
Wright DA, Meguid M, Lubovsky O, Whyne CM. Subchondral bone density distribution in the human femoral head. Skelet Radiol. 2012;41(6):677–83.
Bachtar F, Chen X, Hisada T. Finite element contact analysis of the hip joint. Med Biol Eng Comput. 2006;44(8):643–51.
Iwasaki K, Yamamoto T, Motomura G, Ikemura S, Yamaguchi R, Iwamoto Y. Radiologic measurements associated with the prognosis and need for surgery in patients with subchondral insufficiency fractures of the femoral head. AJR Am J Roentgenol. 2013;201(1):W97–103.
Ipavec M, Brand RA, Pedersen DR, Mavcic B, Kralj-Iglic V, Iglic A. Mathematical modelling of stress in the hip during gait. J Biomech. 1999;32(11):1229–35.
Yamamoto T, Iwasaki K, Iwamoto Y. Transtrochanteric rotational osteotomy for a subchondral insufficiency fracture of the femoral head in young adults. Clin Orthop Relat Res. 2010;468(12):3181–5.
Acknowledgments
This work was supported in part by a research grant from Japan Society for the Promotion of Science (15 K10479), and a Research Grant for Intractable Diseases from the Japan Agency for Medical Research and Development (H26-Itaku(Nan)-Ippan-031).
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Iwasaki, K., Yamamoto, T., Motomura, G. et al. Common site of subchondral insufficiency fractures of the femoral head based on three-dimensional magnetic resonance imaging. Skeletal Radiol 45, 105–113 (2016). https://doi.org/10.1007/s00256-015-2258-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00256-015-2258-6